Perspectives for Generative AI-Assisted Art Therapy for Melanoma Patients
Abstract
:1. Introduction
2. Methods
2.1. Study Design
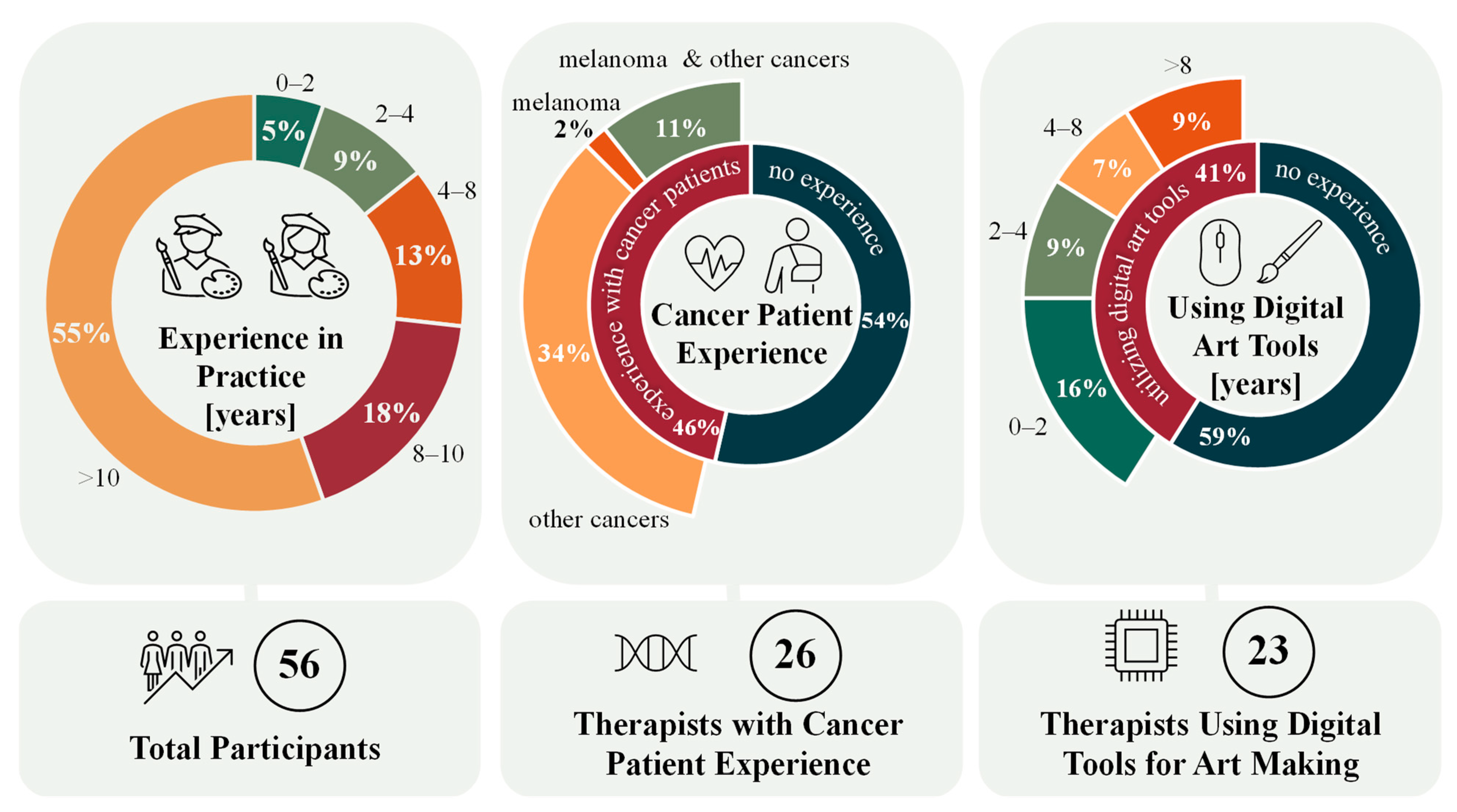
2.2. Participants
2.3. Procedures and Ethics
2.4. Data Analysis and Reflexivity
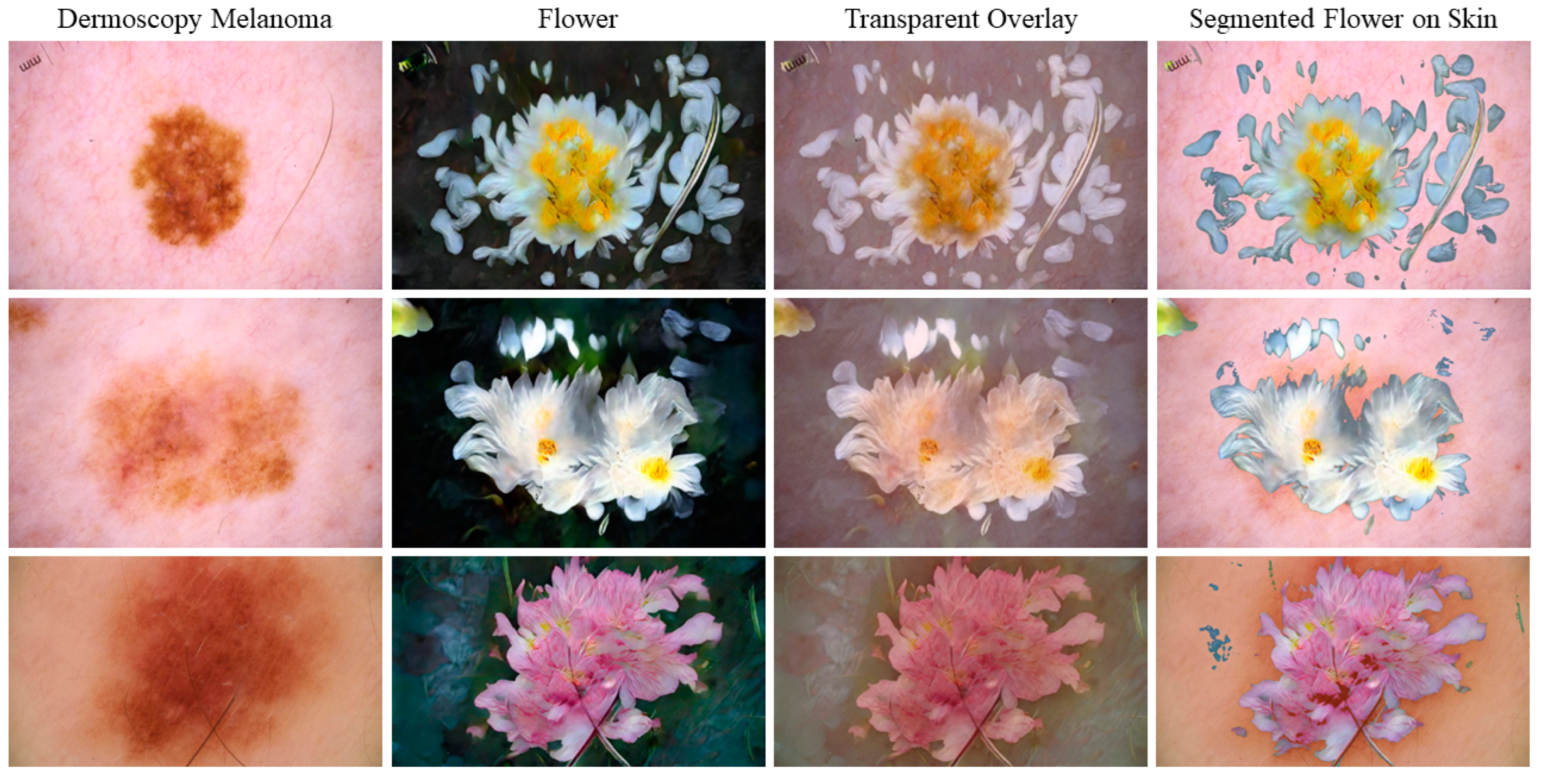
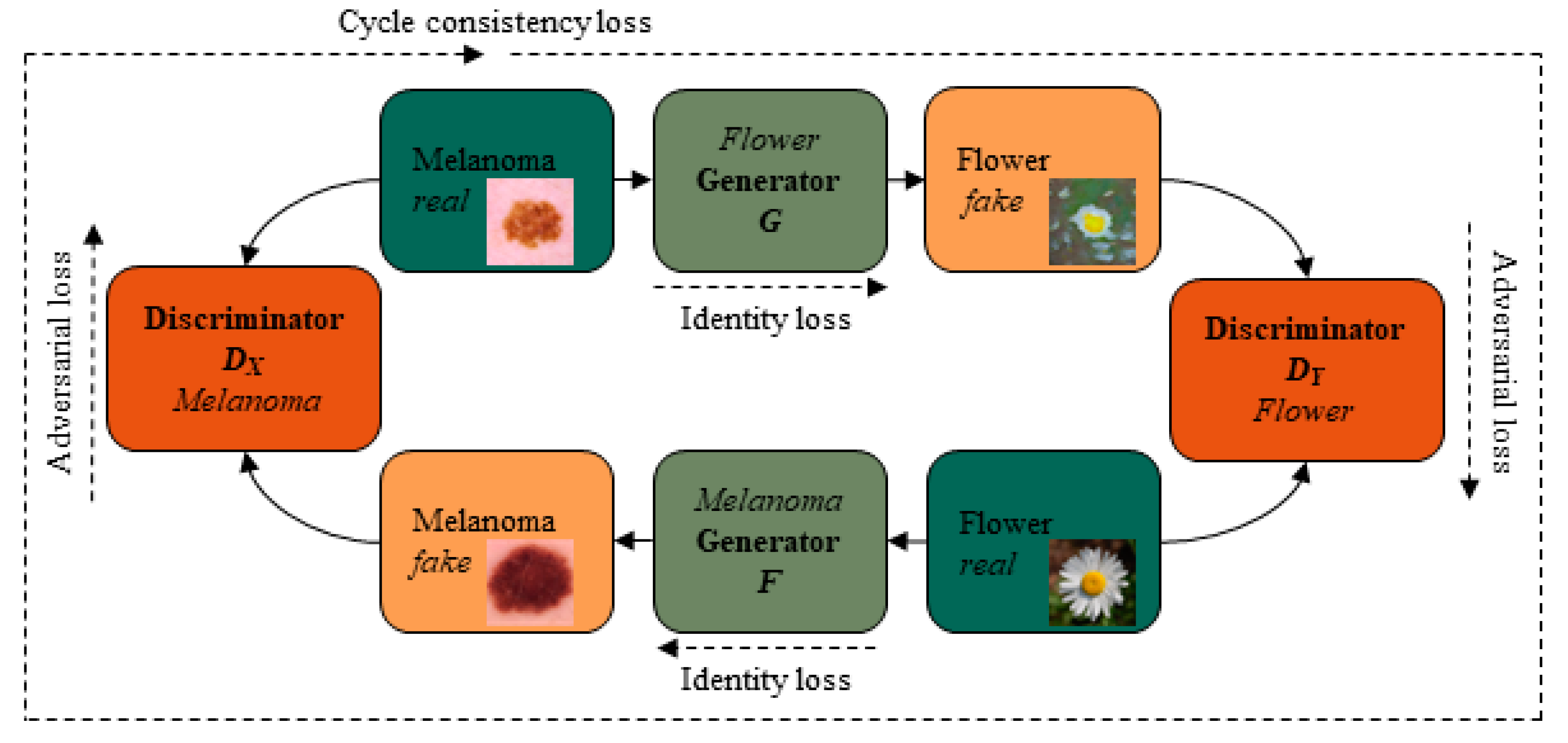
2.5. Basic Cycle-Consistent Generative Adversarial Network (GAN) Principle
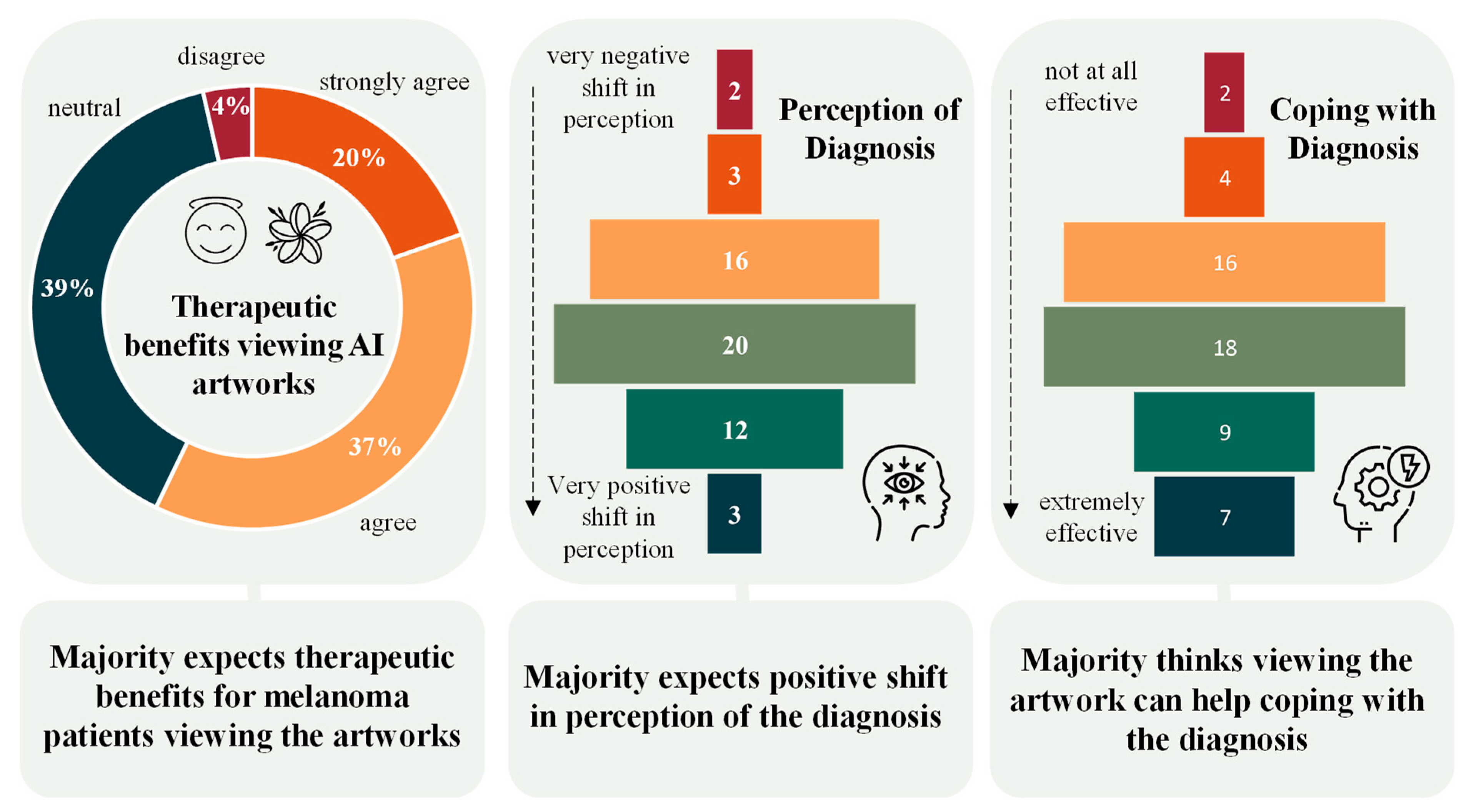
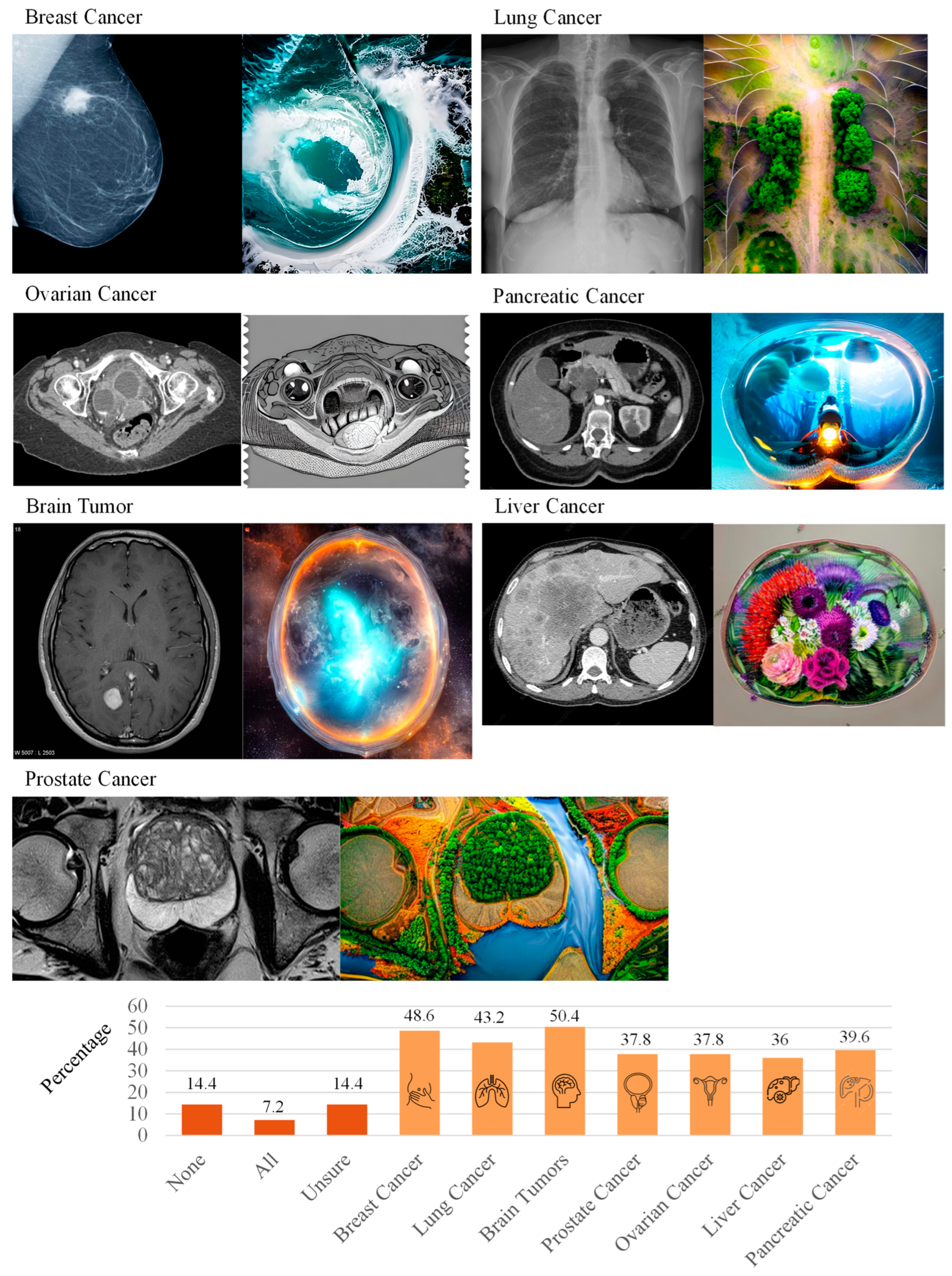
3. Results
4. Discussion
5. Limitations of the Study
6. Implications for Policy, Practice, and Further Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Questionnaire
References
- Miller, G.; McDonald, A. Online art therapy during the COVID-19 pandemic. Int. J. Art Ther. 2020, 25, 159–160. [Google Scholar] [CrossRef]
- Gao, T.; Zhang, D.; Hua, G.; Qiao, Y.; Zhou, H. Artificial Intelligence Painting Interactive Experience Discovers Possibilities for Emotional Healing in the Post-pandemic Era. In HCI International 2023 Posters; Stephanidis, C., Antona, M., Ntoa, S., Salvendy, G., Eds.; Springer Nature: Cham, Switzerland, 2023; pp. 415–425. ISBN 978-3-031-35997-2. [Google Scholar]
- Hadjipanayi, C.; Banakou, D.; Michael-Grigoriou, D. Art as therapy in virtual reality: A scoping review. Front. Virtual Real. 2023, 4, 1065863. [Google Scholar] [CrossRef]
- Ragot, M.; Martin, N.; Cojean, S. AI-generated vs. Human Artworks. A Perception Bias Towards Artificial Intelligence? In Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems, Proceedings of the CHI‘20: CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; Bernhaupt, R., Mueller, F., Verweij, D., Andres, J., McGrenere, J., Cockburn, A., Avellino, I., Goguey, A., Bjørn, P., Zhao, S., et al., Eds.; ACM: New York, NY, USA, 2020; pp. 1–10. ISBN 9781450368193. [Google Scholar]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Uong, A.; Zon, L.I. Melanocytes in development and cancer. J. Cell. Physiol. 2010, 222, 38–41. [Google Scholar] [CrossRef]
- Guy, G.P.; Thomas, C.C.; Thompson, T.; Watson, M.; Massetti, G.M.; Richardson, L.C. Vital signs: Melanoma incidence and mortality trends and projections—United States, 1982–2030. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 591–596. [Google Scholar]
- Kasparian, N.A. Psychological care for people with melanoma: What, when, why and how? Semin. Oncol. Nurs. 2013, 29, 214–222. [Google Scholar] [CrossRef]
- Yang, H.; Xia, L.; Chen, J.; Zhang, S.; Martin, V.; Li, Q.; Lin, S.; Chen, J.; Calmette, J.; Lu, M.; et al. Stress-glucocorticoid-TSC22D3 axis compromises therapy-induced antitumor immunity. Nat. Med. 2019, 25, 1428–1441. [Google Scholar] [CrossRef] [PubMed]
- Schoemaker, M.J.; Jones, M.E.; Wright, L.B.; Griffin, J.; McFadden, E.; Ashworth, A.; Swerdlow, A.J. Psychological stress, adverse life events and breast cancer incidence: A cohort investigation in 106,000 women in the United Kingdom. Breast Cancer Res. 2016, 18, 72. [Google Scholar] [CrossRef]
- Blum, A.; Blum, D.; Stroebel, W.; Rassner, G.; Garbe, C.; Hautzinger, M. Psychosoziale Belastung und subjektives Erleben von Melanompatienten in der ambulanten Nachsorge. Psychother. Psychosom. Med. Psychol. 2003, 53, 258–266. [Google Scholar] [CrossRef]
- Kim, K.S.; Loring, S.; Kwekkeboom, K. Use of Art-Making Intervention for Pain and Quality of Life Among Cancer Patients: A Systematic Review. J. Holist. Nurs. 2018, 36, 341–353. [Google Scholar] [CrossRef]
- Tang, Y.; Fu, F.; Gao, H.; Shen, L.; Chi, I.; Bai, Z. Art therapy for anxiety, depression, and fatigue in females with breast cancer: A systematic review. J. Psychosoc. Oncol. 2019, 37, 79–95. [Google Scholar] [CrossRef]
- Boehm, K.; Cramer, H.; Staroszynski, T.; Ostermann, T. Arts therapies for anxiety, depression, and quality of life in breast cancer patients: A systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2014, 2014, 103297. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.-H.; Moh, S.-L.; Kuo, Y.-C.; Wu, P.-Y.; Lin, C.-L.; Tsai, M.-H.; Chen, T.-J.; Hwang, S.-J. Art therapy for terminal cancer patients in a hospice palliative care unit in Taiwan. Palliat. Support. Care 2012, 10, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Choi, M.Y.; Kim, Y.B.; Sun, J.; Park, E.J.; Kim, J.H.; Kang, M.; Koom, W.S. Art therapy based on appreciation of famous paintings and its effect on distress among cancer patients. Qual. Life Res. 2017, 26, 707–715. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, I.; Pouget-Abadie, J.; Mirza, M.; Xu, B.; Warde-Farley, D.; Ozair, S.; Courville, A.; Bengio, Y. Generative adversarial networks. Commun. ACM 2020, 63, 139–144. [Google Scholar] [CrossRef]
- Zhu, J.-Y.; Park, T.; Isola, P.; Efros, A.A. Unpaired Image-to-Image Translation Using Cycle-Consistent Adversarial Networks. In Proceedings of the 2017 IEEE International Conference on Computer Vision (ICCV), Venice, France, 22–29 October 2017; pp. 2242–2251, ISBN 978-1-5386-1032-9. [Google Scholar]
- Chen, Y.; Lin, H.; Zhang, W.; Chen, W.; Zhou, Z.; Heidari, A.A.; Chen, H.; Xu, G. ICycle-GAN: Improved cycle generative adversarial networks for liver medical image generation. Biomed. Signal Process. Control. 2024, 92, 106100. [Google Scholar] [CrossRef]
- Lei, Y.; Harms, J.; Wang, T.; Liu, Y.; Shu, H.-K.; Jani, A.B.; Curran, W.J.; Mao, H.; Liu, T.; Yang, X. MRI-only based synthetic CT generation using dense cycle consistent generative adversarial networks. Med. Phys. 2019, 46, 3565–3581. [Google Scholar] [CrossRef]
- Rajagopal, B.G.; Kumar, M.; Alshehri, A.H.; Alanazi, F.; Deifalla, A.F.; Yosri, A.M.; Azam, A. A hybrid Cycle GAN-based lightweight road perception pipeline for road dataset generation for Urban mobility. PLoS ONE 2023, 18, e0293978. [Google Scholar] [CrossRef]
- Liu, S.; Li, X.; Zheng, A.; Yang, F.; Liu, Y.; Guan, T.; He, Y. The Generation of Virtual Immunohistochemical Staining Images Based on an Improved Cycle-GAN. In Proceedings of the Machine Learning and Intelligent Communications; Guan, M., Na, Z., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 137–147, ISBN 978-3-030-66784-9. [Google Scholar]
- Liu, Y.; Chen, A.; Shi, H.; Huang, S.; Zheng, W.; Liu, Z.; Zhang, Q.; Yang, X. CT synthesis from MRI using multi-cycle GAN for head-and-neck radiation therapy. Comput. Med. Imaging Graph. 2021, 91, 101953. [Google Scholar] [CrossRef]
- Zubala, A.; Kennell, N.; Hackett, S. Art Therapy in the Digital World: An Integrative Review of Current Practice and Future Directions. Front. Psychol. 2021, 12, 595536. [Google Scholar] [CrossRef]
- He, K.; Zhang, X.; Ren, S.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778, ISBN 978-1-4673-8851-1. [Google Scholar]
- Isola, P.; Zhu, J.-Y.; Zhou, T.; Efros, A.A. Image-to-Image Translation with Conditional Adversarial Networks. In Proceedings of the 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July 2017; pp. 5967–5976, ISBN 978-1-5386-0457-1. [Google Scholar]
- Lin, M.; Chen, Q.; Yan, S. Network in Network. arXiv 2013, arXiv:1312.4400v3. [Google Scholar]
- Hammad, M.M. Deep Learning Activation Functions: Fixed-Shape, Parametric, Adaptive, Stochastic, Miscellaneous, Non-Standard, Ensemble. arXiv 2024, arXiv:2407.11090. [Google Scholar]
- Jütte, L.; Wang, N.; Roth, B. Generative Adversarial Network for Personalized Art Therapy in Melanoma Disease Management. arXiv 2023, arXiv:2303.09232. [Google Scholar]
- Shi, W.; Caballero, J.; Huszár, F.; Totz, J.; Aitken, A.P.; Bishop, R.; Rueckert, D.; Wang, Z. Real-Time Single Image and Video Super-Resolution Using an Efficient Sub-Pixel Convolutional Neural Network. arXiv 2016, arXiv:1609.05158. [Google Scholar]
- Sun, Y.; Chen, Y.; Liu, Q.; Liu, G. Learning image compressed sensing with sub-pixel convolutional generative adversarial network. Pattern Recognit. 2020, 98, 12. [Google Scholar] [CrossRef]
- Vaswani, A.; Shazeer, N.; Parmar, N.; Uszkoreit, J.; Jones, L.; Gomez, A.N.; Kaiser, L.; Polosukhin, I. Attention Is All You Need. arXiv 2017, arXiv:1706.03762. [Google Scholar]
- Wang, X.; Girshick, R.; Gupta, A.; He, K. Non-local Neural Networks. arXiv 2017, arXiv:1711.07971. [Google Scholar]
- Miyato, T.; Kataoka, T.; Koyama, M.; Yoshida, Y. Spectral Normalization for Generative Adversarial Networks. arXiv 2018, arXiv:1802.05957. [Google Scholar]
- Mao, X.; Li, Q.; Xie, H.; Lau, R.Y.K.; Wang, Z.; Smolley, S.P. Least Squares Generative Adversarial Networks. arXiv 2016, arXiv:1611.04076. [Google Scholar]
- Rotemberg, V.; Kurtansky, N.; Betz-Stablein, B.; Caffery, L.; Chousakos, E.; Codella, N.; Combalia, M.; Dusza, S.; Guitera, P.; Gutman, D.; et al. A patient-centric dataset of images and metadata for identifying melanomas using clinical context. Sci. Data 2021, 8, 34. [Google Scholar] [CrossRef]
- Nilsback, M.-E.; Zisserman, A. Automated Flower Classification over a Large Number of Classes. In Proceedings of the 2008 Sixth Indian Conference on Computer Vision, Graphics & Image Processing. Image Processing (ICVGIP), Bhubaneswar, India, 16–19 December 2008; pp. 722–729. [Google Scholar]
- Lee, Y.K.; Park, Y.-H.; Hahn, S. A Portrait of Emotion: Empowering Self-Expression through AI-Generated Art. arXiv 2023, arXiv:2304.13324. [Google Scholar]
- Yoo, D.; Kim, D.Y.; Lopes, E. Digital Art Therapy with Gen AI: Mind Palette. In Proceedings of the 2023 11th International Conference on Affective Computing and Intelligent Interaction Workshops and Demos (ACIIW), Cambridge, MA, USA, 10–13 September 2023; pp. 1–3, ISBN 979-8-3503-2745-8. [Google Scholar]
- Du, X.; An, P.; Leung, J.; Li, A.; Chapman, L.E.; Zhao, J. DeepThInk: Designing and probing human-AI co-creation in digital art therapy. Int. J. Hum.-Comput. Stud. 2024, 181, 103139. [Google Scholar] [CrossRef]
- Liu, D.; Zhou, H.; An, P. “When He Feels Cold, He Goes to the Seahorse”—Blending Generative AI into Multimaterial Storymaking for Family Expressive Arts Therapy. In Proceedings of the CHI Conference on Human Factors in Computing Systems. CHI‘24: CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 11–16 May 2024; Mueller, F.F., Kyburz, P., Williamson, J.R., Sas, C., Wilson, M.L., Dugas, P.T., Shklovski, I., Eds.; ACM: New York, NY, USA, 2024; pp. 1–21. [Google Scholar]
- Choe, N.S.; Hinz, L.D. The Role of the Expressive Therapies Continuum in Human Creativity in the Age of AI. Art Ther. 2024, 1–9. [Google Scholar] [CrossRef]
- Hu, C.; Lin, Z.; Zhang, N.; Ji, L.-J. AI-empowered imagery writing: Integrating AI-generated imagery into digital mental health service. Front. Psychiatry 2024, 15, 1434172. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W.F. Comparison of Beck Depression Inventories-IA and-II in Psychiatric Outpatients. J. Personal. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef]
- Spielberger, C.D. PsycTESTS Dataset; APA PsycTests: Washington, DC, USA, 1983. [Google Scholar]
- Tulyakov, S.; Liu, M.-Y.; Yang, X.; Kautz, J. MoCoGAN: Decomposing Motion and Content for Video Generation. arXiv 2017, arXiv:1707.04993. [Google Scholar]
- Yan, W.; Zhang, Y.; Abbeel, P.; Srinivas, A. VideoGPT: Video Generation using VQ-VAE and Transformers. arXiv 2021, arXiv:2104.10157. [Google Scholar]
- Karras, T.; Laine, S.; Aila, T. A Style-Based Generator Architecture for Generative Adversarial Networks. arXiv 2018, arXiv:1812.04948. [Google Scholar]
- Ramesh, A.; Dhariwal, P.; Nichol, A.; Chu, C.; Chen, M. Hierarchical Text-Conditional Image Generation with CLIP Latents. arXiv 2022, arXiv:2204.06125. [Google Scholar]
- Radford, A.; Kim, J.W.; Hallacy, C.; Ramesh, A.; Goh, G.; Agarwal, S.; Sastry, G.; Askell, A.; Mishkin, P.; Clark, J.; et al. Learning Transferable Visual Models from Natural Language Supervision. arXiv 2021, arXiv:2103.00020. [Google Scholar]

| Integration into Art Therapy Session | Counts | Percentage [%] |
|---|---|---|
| Introduction & Contextualization | 23 | 41.1 |
| Physical Art Creation | 34 | 60.7 |
| Storytelling & Symbolism | 39 | 69.6 |
| Group Discussions | 34 | 60.7 |
| Projection & Reflection | 33 | 58.9 |
| Journaling | 36 | 64.3 |
| Digital-Physical Fusion | 28 | 50 |
| Feedback & Evolution | 27 | 48.2 |
| Closing Reflection | 23 | 41.1 |
| Impact on Patients’ Perception of Their Diagnosis | Counts | Percentage [%] |
|---|---|---|
| Empowerment | 31 | 55.4 |
| Distress | 25 | 44.6 |
| Cathartic Release | 25 | 44.6 |
| Increased Connection | 25 | 44.6 |
| Aestheticizing Illness | 20 | 35.7 |
| Educational Tool | 20 | 35.7 |
| Therapeutic Potential | 35 | 62.5 |
| Increased Anxiety | 14 | 25 |
| Reframing Perspective | 34 | 60.7 |
| Mixed Emotions | 31 | 55.4 |
| Sense of Ownership | 27 | 48.2 |
| Potential for Misunderstanding | 25 | 44.6 |
| Potential Challenges Introducing Artworks to Patients | Counts | Percentage [%] |
|---|---|---|
| None | 1 | 1.8 |
| Emotional Triggers | 32 | 57.1 |
| Misunderstanding | 21 | 37.5 |
| Digital Art Acceptance | 36 | 64.3 |
| Technical Barriers | 42 | 75 |
| Integration with Traditional Therapy | 24 | 42.9 |
| Overemphasis on Aesthetics | 24 | 42.9 |
| Differing Cultural Perceptions | 34 | 60.7 |
| Identity and Personal Connection | 24 | 42.9 |
| Ambiguity in Therapeutic Outcomes | 27 | 48.2 |
| Possible Accompanying Therapeutic Interventions | Counts | Percentage [%] |
|---|---|---|
| Art History Introduction | 6 | 10.3 |
| Art Interpretation Session | 34 | 58.6 |
| Narrative Therapy Integration | 36 | 62.1 |
| Guided Imagery Meditation | 33 | 56.9 |
| Comparative Analysis | 22 | 37.9 |
| Digital Art Creation Session | 35 | 60.4 |
| Group Sharing Sessions | 33 | 56.9 |
| Feedback Loop | 26 | 44.8 |
| Art and Emotional Journaling | 33 | 56.9 |
| Integrating Traditional Art | 37 | 63.8 |
| Advancements in Digital Art Therapy Tools (Next Five Years) | Counts | Percentage [%] |
|---|---|---|
| None | 1 | 1.8 |
| Virtual Reality Integration | 20 | 35.7 |
| AI-guided Sessions | 6 | 10.7 |
| Digital Art Toolkits | 34 | 60.7 |
| Remote Art Therapy Platforms | 39 | 69.6 |
| Augmented Reality in Art Therapy | 11 | 19.6 |
| Therapeutic Gaming | 17 | 30.4 |
| Digital Art Display and Storage | 28 | 50 |
| Wearable Biofeedback Devices | 21 | 37.5 |
| Multimedia Integration | 25 | 44.6 |
| Online Art Therapy Communities | 25 | 44.6 |
| Training and Workshops | 44 | 78.6 |
| Accessibility Features | 33 | 58.9 |
| Interactive Digital Installations | 19 | 33.9 |
| Digital Storytelling | 30 | 53.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jütte, L.; Wang, N.; Steven, M.; Roth, B. Perspectives for Generative AI-Assisted Art Therapy for Melanoma Patients. AI 2024, 5, 1648-1669. https://doi.org/10.3390/ai5030080
Jütte L, Wang N, Steven M, Roth B. Perspectives for Generative AI-Assisted Art Therapy for Melanoma Patients. AI. 2024; 5(3):1648-1669. https://doi.org/10.3390/ai5030080
Chicago/Turabian StyleJütte, Lennart, Ning Wang, Martin Steven, and Bernhard Roth. 2024. "Perspectives for Generative AI-Assisted Art Therapy for Melanoma Patients" AI 5, no. 3: 1648-1669. https://doi.org/10.3390/ai5030080







