C5 Palsy after Cervical Disc Arthroplasty: Two Case Reports and Literature Review
Abstract
1. Introduction
2. Case Presentation
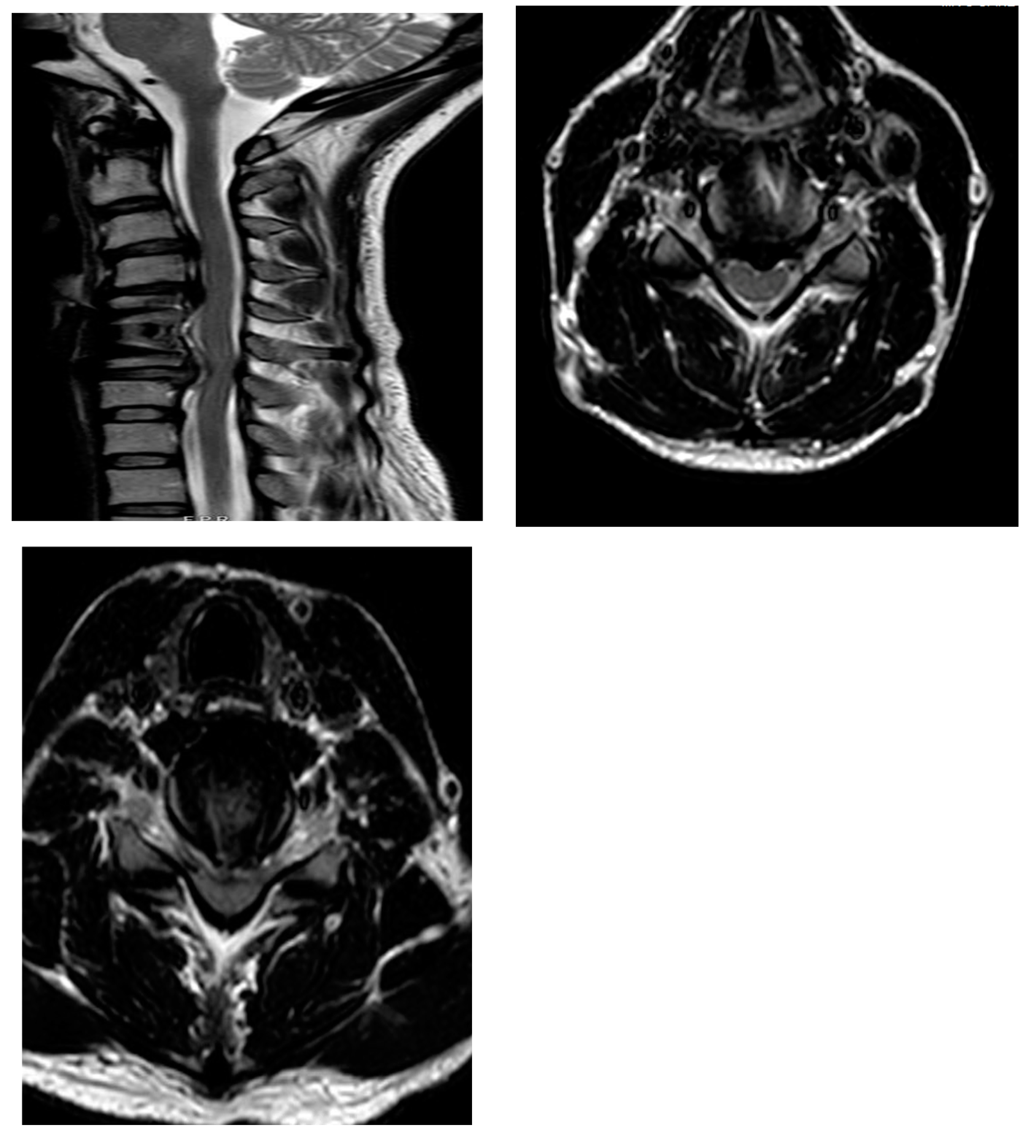
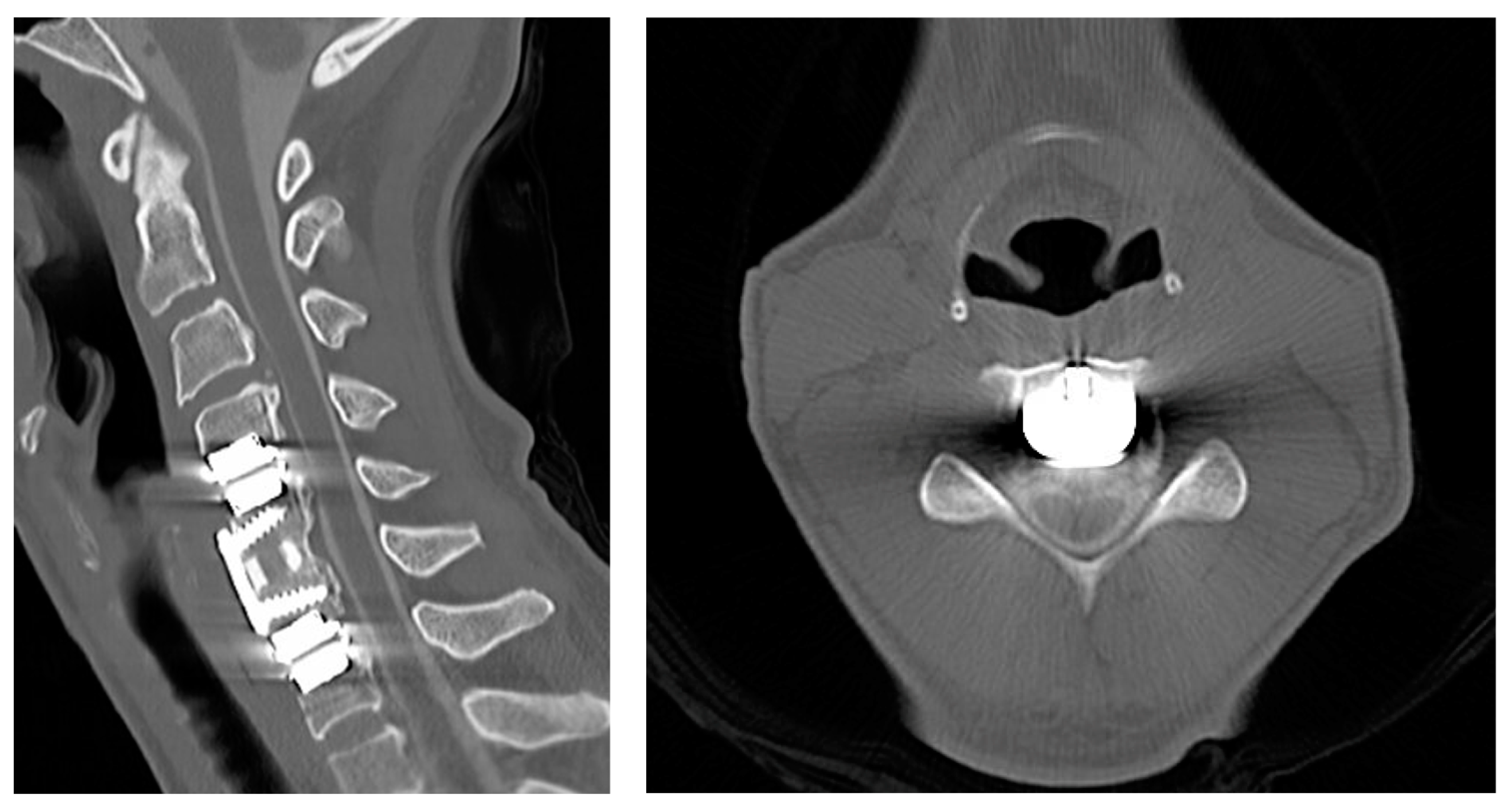
2.1. Case 1
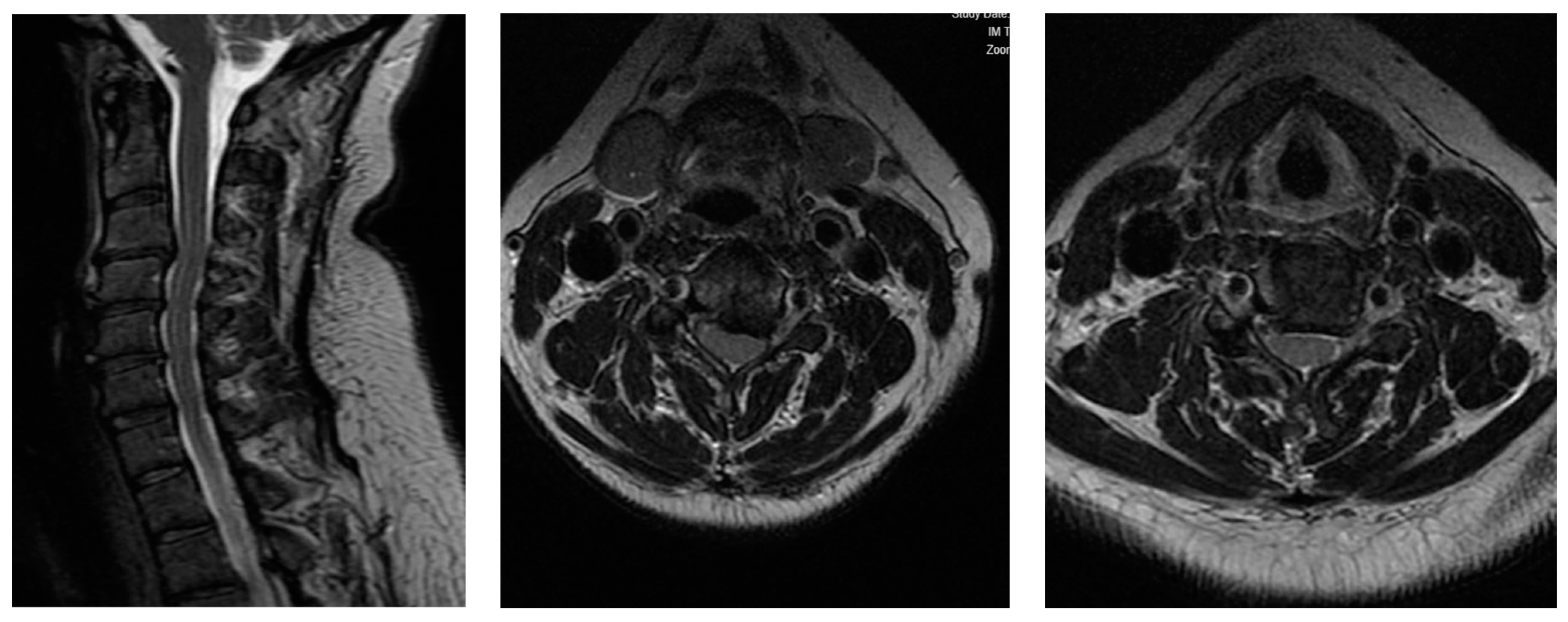
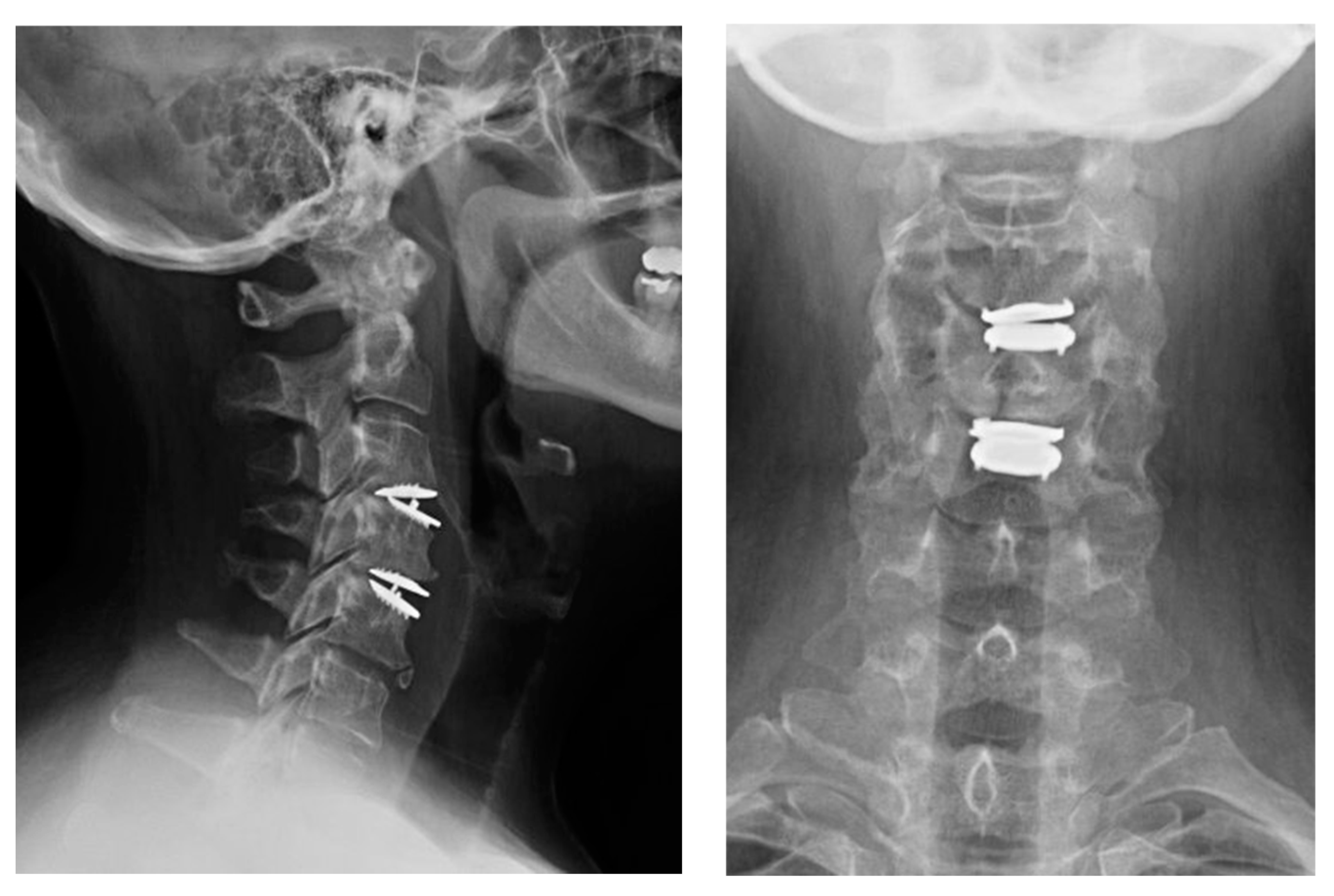
2.2. Case 2
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bydon, M.; Michalopoulos, G.D.; Spinner, R.J. Postoperative C5 Palsy: Apples, Oranges, and Rotten Tomatoes. World Neurosurg. 2021, 151, 145–146. [Google Scholar] [CrossRef] [PubMed]
- Shou, F.; Li, Z.; Wang, H.; Yan, C.; Liu, Q.; Xiao, C. Prevalence of C5 nerve root palsy after cervical decompressive surgery: A meta-analysis. Eur. Spine J. 2015, 24, 2724–2734. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Wang, H.; Liu, S.; Ding, W.Y. Incidence of C5 nerve root palsy after cervical surgery: A meta-analysis for last decade. Medicine 2017, 96, e8560. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.A.; Matz, P.G.; Groff, M.W.; Heary, R.F.; Holly, L.T.; Kaiser, M.G.; Mummaneni, P.V.; Ryken, T.C.; Choudhri, T.F.; Vresilovic, E.J.; et al. Laminectomy and fusion for the treatment of cervical degenerative myelopathy. J. Neurosurg. Spine 2009, 11, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, N.; Nakanishi, K.; Fujiwara, Y.; Kamei, N.; Ochi, M. Postoperative segmental C5 palsy after cervical laminoplasty may occur without intraoperative nerve injury: A prospective study with transcranial electric motor-evoked potentials. Spine 2006, 31, 3013–3017. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, N.; Stino, A.M.; Smith, B.W.; Little, A.A.; Yang, L.J.S.; Park, P.; Saadeh, Y.S. Defining postoperative C5 palsy and recovery: A systematic review. J. Neurosurg. Spine 2023, 38, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Traynelis, V.C.; Fontes, R.B.V.; Kasliwal, M.K.; Ryu, W.H.A.; Tan, L.A.; Witiw, C.D.; Dettori, J.R.; Brodt, E.D.; Skelly, A.C. Risk factors for C5 palsy: A systematic review and multivariate analysis. J. Neurosurg. Spine 2024, 40, 216–228. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.J.; Kim, K.R.; Son, D.W.; Shin, D.A.; Yi, S.; Kim, K.N.; Yoon, D.H.; Ha, Y.; Riew, K.D. Cervical disc arthroplasty: What we know in 2020 and a literature review. J. Orthop. Surg. 2021, 29, 23094990211006934. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, N.; Abe, R.; Saiki, K.; Okai, K. Paralysis of the arm after posterior decompression of the cervical spinal cord. II. Analyses of clinical findings. Eur. Spine J. 1993, 2, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Uematsu, Y.; Tokuhashi, Y.; Matsuzaki, H. Radiculopathy after laminoplasty of the cervical spine. Spine 1998, 23, 2057–2062. [Google Scholar] [CrossRef] [PubMed]
- Aiba, A.; Mochizuki, M.; Kadota, R.; Hashimoto, M.; Maki, S.; Furuya, T.; Koda, M.; Yamazaki, M.; Takahashi, H. Characteristics of Postoperative C5 Palsy Following Anterior Decompression and Fusion Surgery for Cervical Degenerative Disorders: Trends Associated with Advancements in Surgical Technique. World Neurosurg. 2023, 176, e232–e239. [Google Scholar] [CrossRef] [PubMed]
- Jack, A.; Ramey, W.L.; Dettori, J.R.; Tymchak, Z.A.; Oskouian, R.J.; Hart, R.A.; Chapman, J.R.; Riew, D. Factors Associated With C5 Palsy Following Cervical Spine Surgery: A Systematic Review. Global Spine J. 2019, 9, 881–894. [Google Scholar] [CrossRef] [PubMed]
- Bydon, M.; Macki, M.; Kaloostian, P.; Sciubba, D.M.; Wolinsky, J.P.; Gokaslan, Z.L.; Belzberg, A.J.; Bydon, A.; Witham, T.F. Incidence and prognostic factors of c5 palsy: A clinical study of 1001 cases and review of the literature. Neurosurgery 2014, 74, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.G.; Havey, R.M. Biomechanics of Cervical Disc Arthroplasty-A Review of Concepts and Current Technology. Int. J. Spine Surg. 2020, 14, S14–S28. [Google Scholar] [CrossRef] [PubMed]
- Pennington, Z.; Lubelski, D.; Westbroek, E.M.; Ahmed, A.K.; Ehresman, J.; Goodwin, M.L.; Lo, S.F.; Witham, T.F.; Bydon, A.; Theodore, N.; et al. Time to recovery predicted by the severity of postoperative C5 palsy. J. Neurosurg. Spine 2019, 32, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Staudt, M.D.; Rabin, D.; Baaj, A.A.; Crawford, N.R.; Duggal, N. Biomechanical evaluation of the ProDisc-C stability following graded posterior cervical injury. J. Neurosurg. Spine 2018, 29, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Srikantha, U.; Hari, A.; Lokanath, Y.K.; Somasundar, D.; Rao, S. Delayed C5 palsy following anterior cervical discectomy and arthroplasty—Rare presentation of two cases by an unusual phenomenon of “flosealoma”. J. Spinal Surg. 2022, 9, 128–133. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carballo Cuello, C.; Flores Milan, G.; Baerga, N.; Greenberg, M.; Alikhani, P.; Hayman, E. C5 Palsy after Cervical Disc Arthroplasty: Two Case Reports and Literature Review. Surgeries 2024, 5, 719-725. https://doi.org/10.3390/surgeries5030056
Carballo Cuello C, Flores Milan G, Baerga N, Greenberg M, Alikhani P, Hayman E. C5 Palsy after Cervical Disc Arthroplasty: Two Case Reports and Literature Review. Surgeries. 2024; 5(3):719-725. https://doi.org/10.3390/surgeries5030056
Chicago/Turabian StyleCarballo Cuello, César, Gabriel Flores Milan, Nicolas Baerga, Mark Greenberg, Puya Alikhani, and Erik Hayman. 2024. "C5 Palsy after Cervical Disc Arthroplasty: Two Case Reports and Literature Review" Surgeries 5, no. 3: 719-725. https://doi.org/10.3390/surgeries5030056
APA StyleCarballo Cuello, C., Flores Milan, G., Baerga, N., Greenberg, M., Alikhani, P., & Hayman, E. (2024). C5 Palsy after Cervical Disc Arthroplasty: Two Case Reports and Literature Review. Surgeries, 5(3), 719-725. https://doi.org/10.3390/surgeries5030056





