Mitigating Weight Stigma: A Randomized Controlled Trial Addressing Obesity Prejudice through Education among Healthcare Undergraduates
Abstract
1. Introduction
2. Materials and Methods
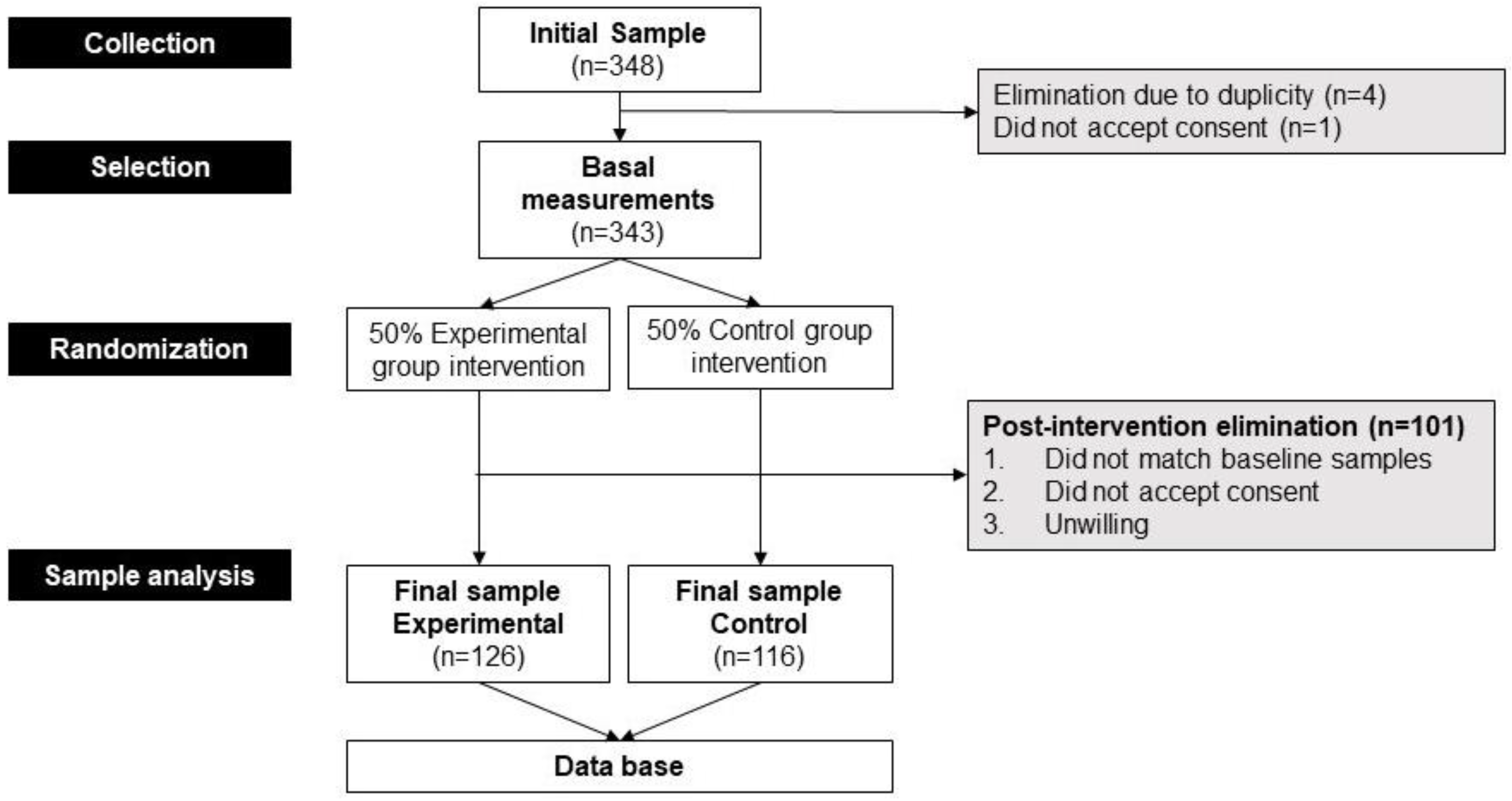
2.1. Participants and Design
2.2. Variables Analyzed and Intervention Procedures
2.3. Natural Semantic Network
2.4. Belief about Persons Living with Obesity
2.5. Fat Phobia Scale
2.6. Statistics
2.7. Ethical Considerations
3. Results
3.1. Intervention Design
3.2. Participant Characteristics
3.3. Beliefs and Conceptions of Future Health Professionals towards People Living with Obesity
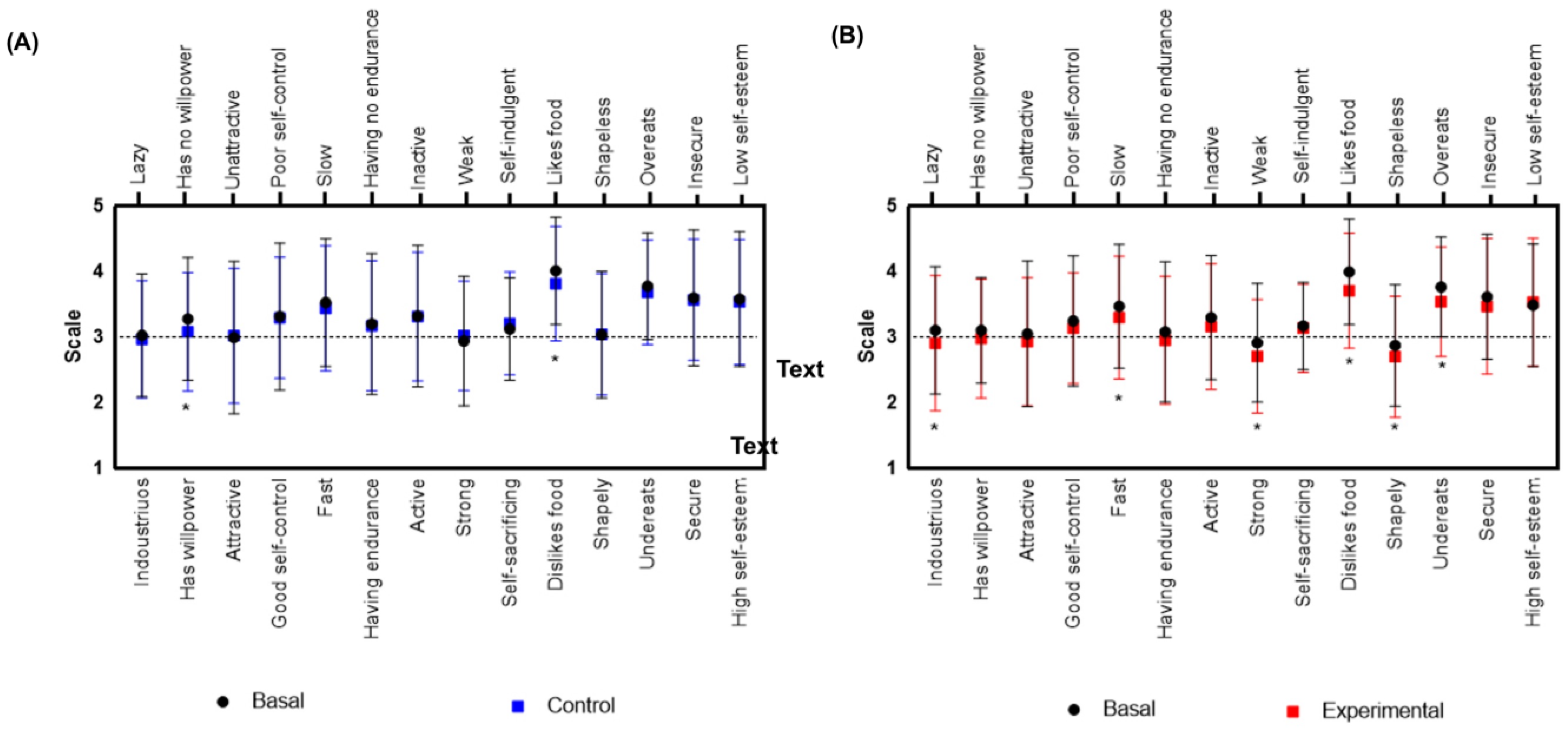
3.4. Post-Intervention Beliefs, Conceptions, and Prejudices towards People Living with Obesity
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Control Group | Experimental Group |
|---|---|
Participants in this group underwent a 60 min lecture centered on the traditional etiology and consequences of obesity. The content of this lecture was drawn from the standard obesity curriculum, encompassing several crucial topics, which are outlined below:
| Participants in this group received a 60 min lecture focusing on the ecological model of obesity and its stigmatizing consequences. The educational session aimed to equip future healthcare professionals with the knowledge and strategies necessary to cultivate a weight-inclusive healthcare environment. The lesson provided a succinct overview of the subject and presented key strategies to mitigate weight stigma. The following topics were addressed during the session:
|
References
- Nagi, M.A.; Ahmed, H.; Rezq, M.A.A.; Sangroongruangsri, S.; Chaikledkaew, U.; Almalki, Z.; Thavorncharoensap, M. Economic Costs of Obesity: A Systematic Review. Int. J. Obes. 2024, 48, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Tyszkowski, R.; Mehrzad, R. The Obesity Pandemic: How We Are Failing Our Patients. In Inflammation and Obesity: A New and Novel Approach to Manage Obesity and Its Consequences; Academic Press: Cambridge, MA, USA, 2022; pp. 5–17. [Google Scholar] [CrossRef]
- Nutter, S.; Eggerichs, L.A.; Nagpal, T.S.; Ramos Salas, X.; Chin Chea, C.; Saiful, S.; Ralston, J.; Barata-Cavalcanti, O.; Batz, C.; Baur, L.A.; et al. Changing the Global Obesity Narrative to Recognize and Reduce Weight Stigma: A Position Statement from the World Obesity Federation. Obes. Rev. 2024, 25, e13642. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.K.; Berry, D.C. Impact of Weight Stigma on Physiological and Psychological Health Outcomes for Overweight and Obese Adults: A Systematic Review. J. Adv. Nurs. 2018, 74, 1030–1042. [Google Scholar] [CrossRef] [PubMed]
- Jayawickrama, R.S.; Hill, B.; O’Connor, M.; Flint, S.W.; Hemmingsson, E.; Lawrence, B.J. Assessing Explicit Weight Bias Among Australian Health Care Students: Suitability of the Beliefs About Obese Persons Scale (BAOP) and the Antifat Attitudes Questionnaire (AFA). Stigma Health 2023. [Google Scholar] [CrossRef]
- Collipal, E.; Godoy, M.P. Social Representation of Obesity: An Analysis with Students of middle and University Education. Int. J. Morphol. 2015, 33, 877–882. [Google Scholar] [CrossRef][Green Version]
- Spahlholz, J.; Baer, N.; König, H.H.; Riedel-Heller, S.G.; Luck-Sikorski, C. Obesity and Discrimination—A Systematic Review and Meta-Analysis of Observational Studies. Obes. Rev. 2016, 17, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Cardel, M.I.; Newsome, F.A.; Pearl, R.L.; Ross, K.M.; Dillard, J.R.; Miller, D.R.; Hayes, J.F.; Wilfley, D.; Keel, P.K.; Dhurandhar, E.J.; et al. Patient-Centered Care for Obesity: How We Can Treat Obesity While Actively Fighting Weight Stigma and Eating Disorder Risk. J. Acad. Nutr. Diet. 2022, 122, 1089. [Google Scholar] [CrossRef] [PubMed]
- Westbury, S.; Oyebode, O.; van Rens, T.; Barber, T.M. Obesity Stigma: Causes, Consequences, and Potential Solutions. Curr. Obes. Rep. 2023, 12, 10–23. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, B.J.; Kerr, D.; Pollard, C.M.; Theophilus, M.; Alexander, E.; Haywood, D.; O’Connor, M. Weight Bias among Health Care Professionals: A Systematic Review and Meta-Analysis. Obesity 2021, 29, 1802–1812. [Google Scholar] [CrossRef] [PubMed]
- Ryan, L.; Coyne, R.; Heary, C.; Birney, S.; Crotty, M.; Dunne, R.; Conlan, O.; Walsh, J.C. Weight Stigma Experienced by Patients with Obesity in Healthcare Settings: A Qualitative Evidence Synthesis. Obes. Rev. 2023, 24, e13606. [Google Scholar] [CrossRef]
- O’Hara, L.; Taylor, J. What’s Wrong With the ‘War on Obesity?’ A Narrative Review of the Weight-Centered Health Paradigm and Development of the 3C Framework to Build Critical Competency for a Paradigm Shift. Sage Open 2018, 8, 2158244018772888. [Google Scholar] [CrossRef]
- Varkevisser, R.D.M.; van Stralen, M.M.; Kroeze, W.; Ket, J.C.F.; Steenhuis, I.H.M. Determinants of Weight Loss Maintenance: A Systematic Review. Obes. Rev. 2019, 20, 171–211. [Google Scholar] [CrossRef] [PubMed]
- Tesfay, F.; Javanparast, S.; Mwanri, L.; Ziersch, A. Stigma and Discrimination: Barriers to the Utilisation of a Nutritional Program in HIV Care Services in the Tigray Region, Ethiopia. BMC Public Health 2020, 20, 904. [Google Scholar] [CrossRef]
- Armoon, B.; Higgs, P.; Fleury, M.J.; Bayat, A.H.; Moghaddam, L.F.; Bayani, A.; Fakhri, Y. Socio-Demographic, Clinical and Service Use Determinants Associated with HIV Related Stigma among People Living with HIV/AIDS: A Systematic Review and Meta-Analysis. BMC Health Serv. Res. 2021, 21, 1004. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Puhl, R.M.; Cummings, D.E.; Eckel, R.H.; Ryan, D.H.; Mechanick, J.I.; Nadglowski, J.; Ramos Salas, X.; Schauer, P.R.; Twenefour, D.; et al. Joint International Consensus Statement for Ending Stigma of Obesity. Nat. Med. 2020, 26, 485. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M. Weight Bias Internalization and Health: A Systematic Review. Obes. Rev. 2018, 19, 1141–1163. [Google Scholar] [CrossRef] [PubMed]
- Thedinga, H.K.; Zehl, R.; Thiel, A. Weight Stigma Experiences and Self-Exclusion from Sport and Exercise Settings among People with Obesity. BMC Public Health 2021, 21, 565. [Google Scholar] [CrossRef]
- Puhl, R.M.; Lessard, L.M.; Himmelstein, M.S.; Foster, G.D. The Roles of Experienced and Internalized Weight Stigma in Healthcare Experiences: Perspectives of Adults Engaged in Weight Management across Six Countries. PLoS ONE 2021, 16, e0251566. [Google Scholar] [CrossRef]
- Talumaa, B.; Brown, A.; Batterham, R.L.; Kalea, A.Z. Effective Strategies in Ending Weight Stigma in Healthcare. Obes. Rev. 2022, 23, e13494. [Google Scholar] [CrossRef] [PubMed]
- Gayer, G.G.; Weiss, J.; Clearfield, M. Fundamentals for an Osteopathic Obesity Designed Study: The Effects of Education on Osteopathic Medical Students’ Attitudes Regarding Obesity. J. Am. Osteopath. Assoc. 2017, 117, 495–502. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vargas-Garduño, M.d.L.; Méndez Puga, A.M.; Vargas Silva, A.D. La Técnica de Las Redes Semánticas Naturales Modificadas y Su Utilidad En La Investigación Cualitativa 2014. Available online: https://www.memoria.fahce.unlp.edu.ar/trab_eventos/ev.8204/ev.8204.pdf (accessed on 10 March 2024).
- Allison, D.B.; Basile, V.C.; Yuker, H.E. The Measurement of Attitudes toward and Beliefs about Obese Persons. Int. J. Eat. Disord. 1991, 10, 599–607. [Google Scholar] [CrossRef]
- Lewitan, D.; Katz, M.; Formoso, J.; Anger, V. Estigma En Obesidad: Validación al Español de La Escala de Creencias Sobre Las Personas Con Obesidad (Beliefs about Obese Persons Scale- Baop). Actual. Nutr. 2022, 23, 195–203. [Google Scholar] [CrossRef]
- Robinson, B.B.E.; Bacon, L.C.; O’reilly, J. Fat Phobia: Measuring, Understanding, and Changing Anti-fat Attitudes. Int. J. Eat. Disord. 1993, 14, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Bacon, J.G.; Scheltema, K.E.; Robinson, B.E. Fat Phobia Scale Revisited: The Short Form. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Soto, L.; Jiménez-Cruz, A.; Armendariz-Anguiano, A.L.; Bacardí-Gascón, M. Fobia a La Grasa Entre Los Estudiantes de Primer y Quinto Año de Medicina En Tijuana, México. Gac. Sanit. 2015, 29, 153. [Google Scholar] [CrossRef] [PubMed]
- Bacardí-Gascón, M.; Jimenéz-Cruz, A.; Castillo-Ruiz, O.; Bezares-Sarmiento, V.; León-González, J.M. Fat phobia in mexican nutrition students. Nutr. Hosp. 2015, 32, 2956–2957. [Google Scholar] [CrossRef]
- World Health Organization Obesity. Available online: https://www.who.int/health-topics/obesity (accessed on 8 January 2024).
- Márquez Solís, R. Redes Semánticas Naturales en Obesidad; Universidad Autónoma de Nuevo León: San Nicolás de los Garza, Mexico, 2015. [Google Scholar]
- Rathbone, J.A.; Cruwys, T.; Jetten, J.; Banas, K.; Smyth, L.; Murray, K. How Conceptualizing Obesity as a Disease Affects Beliefs about Weight, and Associated Weight Stigma and Clinical Decision-Making in Health Care. Br. J. Health Psychol. 2023, 28, 291–305. [Google Scholar] [CrossRef] [PubMed]
- Phelan, S.M.; Burgess, D.J.; Yeazel, M.W.; Hellerstedt, W.L.; Griffin, J.M.; van Ryn, M. Impact of Weight Bias and Stigma on Quality of Care and Outcomes for Patients with Obesity. Obes. Rev. 2015, 16, 319–326. [Google Scholar] [CrossRef] [PubMed]
| Variable | Frequency (%) | |
|---|---|---|
| Sex | Feminine | 71.9% |
| Masculine | 28.1% | |
| Educational program | Dietetics | 28.1% |
| Nursing | 26.9% | |
| Medicine | 26.5% | |
| Psychology | 18.6% | |
| Semesters attended | One Three Five | 32.6% 28.1% 39.3% |
| Age range * | 18–54 |
| Premeasurements | Post Educational Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (n = 116) | Experimental (n = 126) | ||||||||
| Network Breadth = 189 | Network Breadth = 138 | Network Breadth = 117 | |||||||
| Appearance | Concepts | M Value | FMG Value | Concepts | M Value | FMG Value | Concepts | M Value | FMG Value |
| 1 | Disease | 746 | 100.0 | Disease | 396 | 100 | Disease | 383 | 100.0 |
| 2 | Fat | 524 | 70.2 | Fat | 237 | 59.8 | Stigma | 269 | 70.2 |
| 3 | Food | 480 | 64.3 | Sedentary | 200 | 50.5 | Fat | 265 | 69.2 |
| 4 | Sedentary | 422 | 56.6 | Diet | 187 | 47.2 | Diet | 208 | 54.3 |
| 5 | Overweight | 406 | 54.4 | Food | 181 | 45.7 | Sedentary | 194 | 50.7 |
| 6 | Weight | 401 | 53.8 | Problem | 160 | 40.4 | Food | 188 | 49.1 |
| 7 | Fatty | 384 | 51.5 | Habits | 152 | 38.4 | Weight | 188 | 49.1 |
| 8 | Diet | 353 | 47.3 | Health | 148 | 37.4 | Self-esteem | 175 | 45.7 |
| 9 | Diabetes | 257 | 34.5 | Excess | 121 | 30.6 | Fatty | 172 | 44.9 |
| 10 | Big | 256 | 34.3 | Weight | 109 | 27.5 | Health | 144 | 37.6 |
| 11 | Health | 237 | 31.8 | Fatty | 107 | 27.0 | Overweight | 135 | 35.2 |
| 12 | Problem | 235 | 31.5 | Self-esteem | 102 | 25.8 | Habits | 128 | 33.4 |
| 13 | Habits | 224 | 30.0 | Overweight | 99 | 25.0 | Problem | 119 | 31.1 |
| 14 | Excess | 213 | 28.6 | Junk food | 76 | 19.2 | Big | 110 | 28.7 |
| 15 | Self-esteem | 180 | 24.1 | Diabetes | 66 | 16.7 | Excess | 108 | 28.2 |
| Items | Control (n = 116) Mean ± SD | Experimental (n = 126) Mean ± SD | ||||
|---|---|---|---|---|---|---|
| Pre | Post | p Value | Pre | Post | p Value | |
| 1. Obesity often occurs when eating is used as a form of compensation for lack of love or attention. | 0.1 ± 1.8 | 0.0 ± 1.8 | 0.23654 | 0.2 ± 1.9 | −0.6 ± 1.7 | 0.00008 |
| 2. In many cases, obesity is the result of a biological disorder. | 0.8 ± 1.8 | 0.9 ± 1.7 | 0.76181 | 0.9 ± 1.6 | 0.9 ± 1.6 | 0.58211 |
| 3. Obesity is usually caused by overeating. | 0.6 ± 1.7 | 0.7 ± 1.6 | 0.62203 | 0.6 ± 1.7 | 0.0 ± 1.7 | 0.00142 |
| 4. Most obese people cause their problem by not getting enough exercise. | 0.7 ± 1.9 | 0.8 ± 1.7 | 0.62546 | 0.9 ± 1.7 | 0.0 ± 1.6 | 0.00000 |
| 5. Most obese people eat more than nonobese people. | −0.1 ± 1.8 | 0.3 ± 1.8 | 0.97613 | 0.2 ± 1.9 | −0.5 ± 1.8 | 0.00039 |
| 6. Most obese people have poor eating habits that lead to their obesity. | 1.2 ± 1.8 | 1.1 ± 1.7 | 0.19636 | 1.2 ± 1.6 | 0.5 ± 1.6 | 0.00031 |
| 7. Obesity is rarely caused by a lack of willpower. | −0.1 ± 1.9 | 0.2 ± 1.7 | 0.28621 | −0.3 ± 1.7 | −0.5 ± 1.6 | 0.08110 |
| 8. People can be addicted to food, just as others are addicted to drugs, and these people usually become obese. | 1.5 ± 1.7 | 1.3 ± 1.7 | 0.18174 | 1.5 ± 1.6 | 0.9 ± 1.7 | 0.00018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Lara, K.M.; Cruz-Millán, A.C.; Barrera-Hernandez, L.F.; Valbuena-Gregorio, E.; Ayala-Burboa, M.O.; Hernández-Lepe, M.A.; Olivas-Aguirre, F.J. Mitigating Weight Stigma: A Randomized Controlled Trial Addressing Obesity Prejudice through Education among Healthcare Undergraduates. Obesities 2024, 4, 73-84. https://doi.org/10.3390/obesities4020008
López-Lara KM, Cruz-Millán AC, Barrera-Hernandez LF, Valbuena-Gregorio E, Ayala-Burboa MO, Hernández-Lepe MA, Olivas-Aguirre FJ. Mitigating Weight Stigma: A Randomized Controlled Trial Addressing Obesity Prejudice through Education among Healthcare Undergraduates. Obesities. 2024; 4(2):73-84. https://doi.org/10.3390/obesities4020008
Chicago/Turabian StyleLópez-Lara, Karen Marina, Ana Carolina Cruz-Millán, Laura Fernanda Barrera-Hernandez, Edith Valbuena-Gregorio, Moisés Omar Ayala-Burboa, Marco Antonio Hernández-Lepe, and Francisco Javier Olivas-Aguirre. 2024. "Mitigating Weight Stigma: A Randomized Controlled Trial Addressing Obesity Prejudice through Education among Healthcare Undergraduates" Obesities 4, no. 2: 73-84. https://doi.org/10.3390/obesities4020008
APA StyleLópez-Lara, K. M., Cruz-Millán, A. C., Barrera-Hernandez, L. F., Valbuena-Gregorio, E., Ayala-Burboa, M. O., Hernández-Lepe, M. A., & Olivas-Aguirre, F. J. (2024). Mitigating Weight Stigma: A Randomized Controlled Trial Addressing Obesity Prejudice through Education among Healthcare Undergraduates. Obesities, 4(2), 73-84. https://doi.org/10.3390/obesities4020008







