Infection-Related Readmissions Are Rising among Patients with Hepatorenal Syndrome: A Nationwide Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Population
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
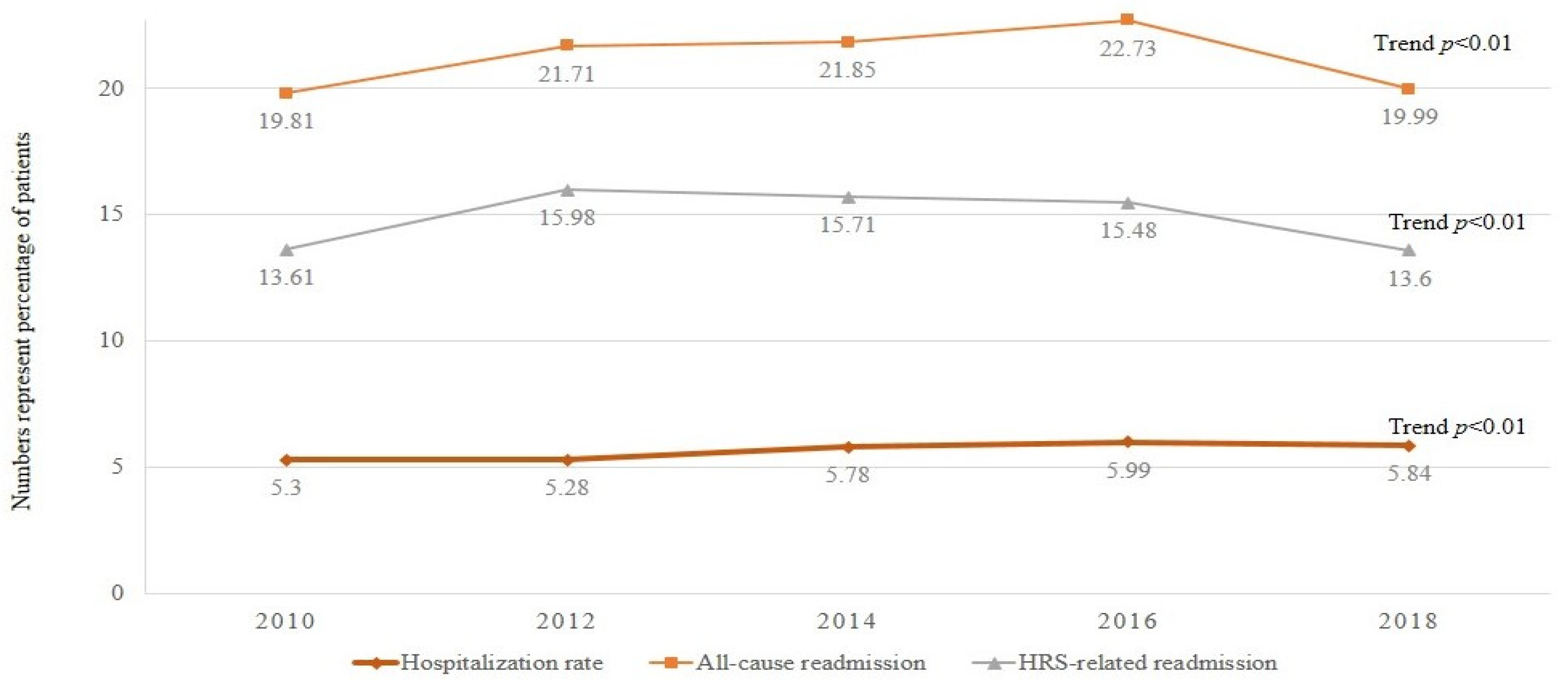
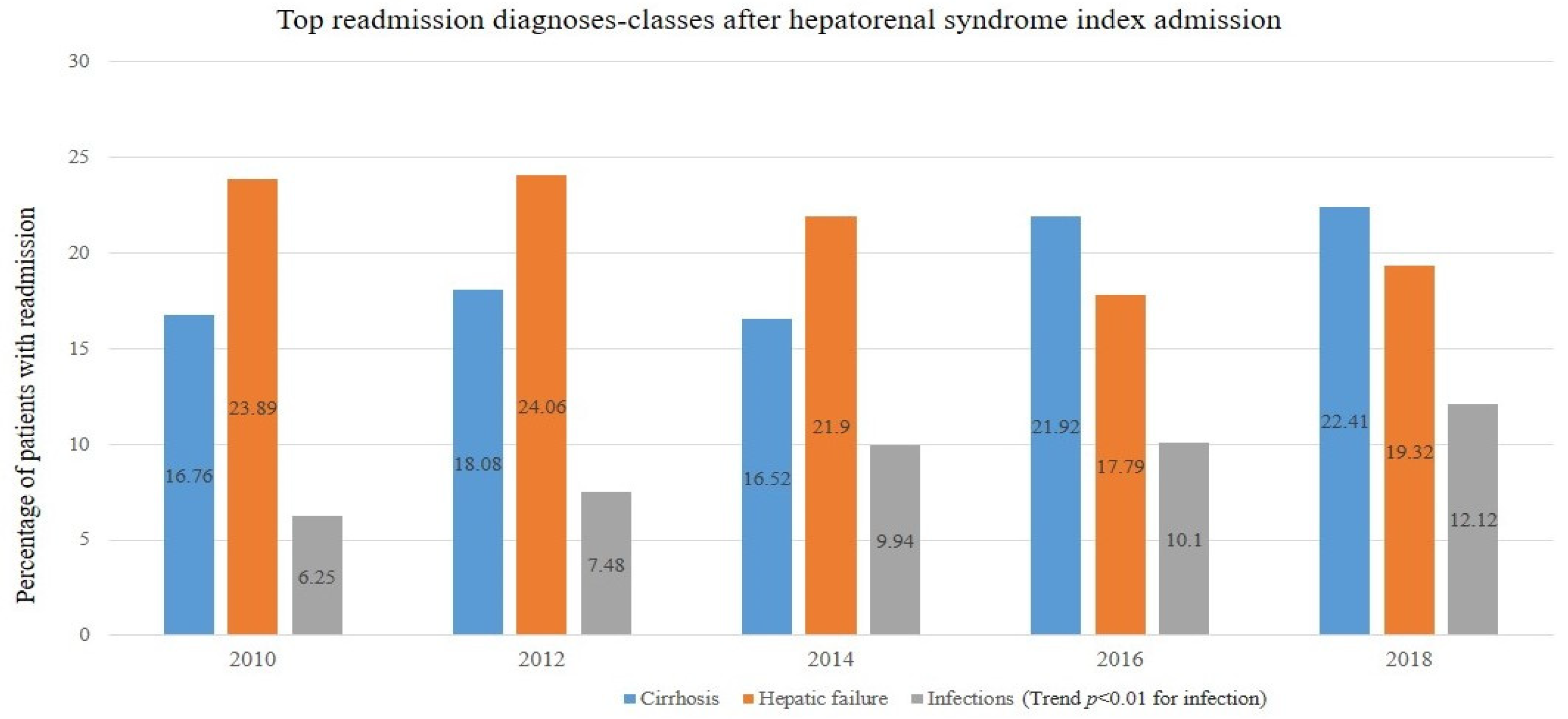
3.2. Hospitalization and 30-Day Readmission
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Angeli, P.; Garcia-Tsao, G.; Nadim, M.K.; Parikh, C.R. News in pathophysiology, definition and classification of hepatorenal syndrome: A step beyond the International Club of Ascites (ICA) consensus document. J. Hepatol. 2019, 71, 811–822. [Google Scholar] [CrossRef] [PubMed]
- Flamm, S.L.; Brown, K.; Wadei, H.M.; Brown, R.S., Jr.; Kugelmas, M.; Samaniego-Picota, M.; Burra, P.; Poordad, F.; Saab, S. The Current Management of Hepatorenal Syndrome-Acute Kidney Injury in the United States and the Potential of Terlipressin. Liver Transpl. 2021, 27, 1191–1202. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.Y.; Chang, J.W. Hepatorenal Syndrome: Current Concepts and Future Perspectives. Clin. Mol. Hepatol. 2023, 29, 891–908. [Google Scholar] [CrossRef] [PubMed]
- Ginès, A.; Escorsell, A.; Ginès, P.; Saló, J.; Jiménez, W.; Inglada, L.; Navasa, M.; Clària, J.; Rimola, A.; Arroyo, V.; et al. Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites. Gastroenterology 1993, 105, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Kaewput, W.; Thongprayoon, C.; Dumancas, C.Y.; Kanduri, S.R.; Kovvuru, K.; Kaewput, C.; Pattharanitima, P.; Petnak, T.; Lertjitbanjong, P.; Boonpheng, B.; et al. In-hospital mortality of hepatorenal syndrome in the United States: Nationwide inpatient sample. World J. Gastroenterol. 2021, 27, 7831–7843. [Google Scholar] [CrossRef] [PubMed]
- Albillos, A.; Lario, M.; Álvarez-Mon, M. Cirrhosis-associated immune dysfunction: Distinctive features and clinical relevance. J. Hepatol. 2014, 61, 1385–1396. [Google Scholar] [CrossRef] [PubMed]
- Chirapongsathorn, S.; Poovorawan, K.; Soonthornworasiri, N.; Pan-Ngum, W.; Phaosawasdi, K.; Treeprasertsuk, S. Thirty-Day Readmission and Cost Analysis in Patients with Cirrhosis: A Nationwide Population-Based Data. Hepatol. Commun. 2020, 4, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Dahiya, D.S.; Kichloo, A.; Singh, G.; Khoshbin, K.; Shaka, H. Hepatorenal syndrome: A Nationwide Trend Analysis from 2008 to 2018. Ann. Med. 2021, 53, 2018–2024. [Google Scholar] [CrossRef] [PubMed]
- Healthcare Cost & Utilization Project. HCUP Databases. Rockville, MD. September 2022. Available online: https://hcup-us.ahrq.gov/nisoverview.jsp (accessed on 29 May 2023).
- The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 245–266. [CrossRef] [PubMed]
- Keller, J.J.; Offerhaus, G.J.; Hylind, L.M.; Giardiello, F.M. Rectal epithelial apoptosis does not predict response to sulindac treatment or polyp development in presymptomatic familial adenomatous polyposis patients. Cancer Epidemiol. Biomarkers Prev. 2002, 11, 670–671. [Google Scholar] [PubMed]
- Garg, S.K.; Goyal, H.; Obaitan, I.; Shah, P.A.; Sarvepalli, S.; Jophlin, L.L.; Singh, D.; Asrani, S.; Kamath, P.S.; Leise, M.D. Incidence and predictors of 30-day hospital readmissions for liver cirrhosis: Insights from the United States National Readmissions Database. Ann. Transl. Med. 2021, 9, 1052. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, S.J.; Metcalfe, L.; Kliethermes, S.; Vasilyev, I.; Tsang, R.; Caines, A.; Mumtaz, S.; Goyal, V.; Khalid, A.; Shoham, D.; et al. Early Hospital Readmissions and Mortality in Patients with Decompensated Cirrhosis Enrolled in a Large National Health Insurance Administrative Database. J. Clin. Gastroenterol. 2017, 51, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Barreto, R.; Fagundes, C.; Guevara, M.; Solà, E.; Pereira, G.; Rodríguez, E.; Graupera, I.; Martín-Llahí, M.; Ariza, X.; Cárdenas, A.; et al. Type-1 hepatorenal syndrome associated with infections in cirrhosis: Natural history, outcome of kidney function, and survival. Hepatology 2014, 59, 1505–1513. [Google Scholar] [CrossRef] [PubMed]
- Umapathy, C.; Loganathan, P.; Dodoo, C.; Gajendran, M. Predictors for Early Readmission in Cirrhosis in the United States—A Nationwide Population-based Study. Am. J. Gastroenterol. 2018, 113, S460–S461. [Google Scholar] [CrossRef]
- Saab, S.; Hernandez, J.C.; Chi, A.C.; Tong, M.J. Oral antibiotic prophylaxis reduces spontaneous bacterial peritonitis occurrence and improves short-term survival in cirrhosis: A meta-analysis. Am. J. Gastroenterol. 2009, 104, 993–1001, quiz 1002. [Google Scholar] [CrossRef] [PubMed]
- Komolafe, O.; Roberts, D.; Freeman, S.C.; Wilson, P.; Sutton, A.J.; Cooper, N.J.; Pavlov, C.S.; Milne, E.J.; Hawkins, N.; Cowlin, M.; et al. Antibiotic prophylaxis to prevent spontaneous bacterial peritonitis in people with liver cirrhosis: A network meta-analysis. Cochrane Database Syst. Rev. 2020, 1, Cd013125. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Tandon, P.; O’Leary, J.G.; Wong, F.; Biggins, S.W.; Garcia-Tsao, G.; Kamath, P.S.; Maliakkal, B.; Fallon, M.B.; Lai, J.C.; et al. Outcomes in Patients with Cirrhosis on Primary Compared to Secondary Prophylaxis for Spontaneous Bacterial Peritonitis. Am. J. Gastroenterol. 2019, 114, 599–606. [Google Scholar] [CrossRef]
- Biggins, S.W.; Angeli, P.; Garcia-Tsao, G.; Ginès, P.; Ling, S.C.; Nadim, M.K.; Wong, F.; Kim, W.R. Diagnosis, Evaluation, and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021, 74, 1014–1048. [Google Scholar] [CrossRef] [PubMed]
- Tapper, E.B.; Halbert, B.; Mellinger, J. Rates of and Reasons for Hospital Readmissions in Patients with Cirrhosis: A Multistate Population-based Cohort Study. Clin. Gastroenterol. Hepatol. 2016, 14, 1181–1188.e2. [Google Scholar] [CrossRef] [PubMed]
| Variables | Year | |||||
|---|---|---|---|---|---|---|
| 2010 | 2012 | 2014 | 2016 | 2018 | p-Value | |
| No. of hospitalization | 25,291 | 28,294 | 34,262 | 39,414 | 42,261 | |
| Sex, % | <0.001 | |||||
| Male | 63.08 | 64.40 | 63.03 | 61.43 | 61.85 | |
| Female | 36.92 | 35.60 | 36.97 | 38.57 | 38.15 | |
| Age, mean, y | 58.09 | 58.39 | 59.01 | 59.09 | 59.16 | <0.001 |
| Insurance type, % | <0.001 | |||||
| Medicare | 40.71 | 41.66 | 44.43 | 44.84 | 46.11 | |
| Medicaid | 22.12 | 23.69 | 23.74 | 25.50 | 24.51 | |
| Private | 31.22 | 29.48 | 27.96 | 27.38 | 25.42 | |
| Uninsured | 5.95 | 5.17 | 4.18 | 3.28 | 3.97 | |
| Household income quartile, % | 0.001 | |||||
| 1st | 30.66 | 31.13 | 27.65 | 30.81 | 29.49 | |
| 2nd | 25.22 | 25.13 | 28.56 | 26.89 | 29.72 | |
| 3rd | 24.08 | 23.54 | 24.12 | 24.80 | 23.80 | |
| 4th | 20.04 | 20.20 | 19.67 | 17.50 | 16.99 | |
| Charlson comorbidity index score, % | <0.001 | |||||
| <4 | 30.46 | 29.19 | 25.83 | 21.19 | 20.53 | |
| ≥4 | 69.54 | 70.81 | 74.17 | 78.81 | 79.47 | |
| Hospital size, % | <0.001 | |||||
| Small | 8.22 | 8.63 | 11.70 | 11.33 | 13.26 | |
| Medium | 18.55 | 20.73 | 23.54 | 25.23 | 23.77 | |
| Large | 73.23 | 70.64 | 64.76 | 63.45 | 62.97 | |
| Hospital teaching status, % | <0.001 | |||||
| Metropolitan non-teaching | 33.97 | 31.47 | 20.87 | 21.39 | 16.73 | |
| Metropolitan teaching | 58.40 | 60.16 | 73.17 | 73.12 | 77.79 | |
| Non-metropolitan | 7.63 | 8.37 | 5.97 | 5.48 | 5.48 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farooq, U.; Tarar, Z.I.; Chaudhary, A.J.; Alayli, A.E.; Kamal, F.; Niu, C.; Qureshi, K. Infection-Related Readmissions Are Rising among Patients with Hepatorenal Syndrome: A Nationwide Analysis. Livers 2024, 4, 268-274. https://doi.org/10.3390/livers4020019
Farooq U, Tarar ZI, Chaudhary AJ, Alayli AE, Kamal F, Niu C, Qureshi K. Infection-Related Readmissions Are Rising among Patients with Hepatorenal Syndrome: A Nationwide Analysis. Livers. 2024; 4(2):268-274. https://doi.org/10.3390/livers4020019
Chicago/Turabian StyleFarooq, Umer, Zahid I. Tarar, Ammad J. Chaudhary, Abdallah E. Alayli, Faisal Kamal, Chengdu Niu, and Kamran Qureshi. 2024. "Infection-Related Readmissions Are Rising among Patients with Hepatorenal Syndrome: A Nationwide Analysis" Livers 4, no. 2: 268-274. https://doi.org/10.3390/livers4020019
APA StyleFarooq, U., Tarar, Z. I., Chaudhary, A. J., Alayli, A. E., Kamal, F., Niu, C., & Qureshi, K. (2024). Infection-Related Readmissions Are Rising among Patients with Hepatorenal Syndrome: A Nationwide Analysis. Livers, 4(2), 268-274. https://doi.org/10.3390/livers4020019







