Journal Description
Livers
Livers
is an international, peer-reviewed, open access journal on liver science published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- High Visibility: indexed within ESCI (Web of Science), Scopus, EBSCO, and other databases.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 27.8 days after submission; acceptance to publication is undertaken in 6.7 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
Impact Factor:
2.4 (2024);
5-Year Impact Factor:
2.3 (2024)
Latest Articles
Comparison of Liver Venous Deprivation Versus Portal Vein Embolization in Patients with Liver Malignancies: A Systematic Review
Livers 2025, 5(4), 48; https://doi.org/10.3390/livers5040048 - 2 Oct 2025
Abstract
►
Show Figures
Background: Liver cancer, either primary or metastatic, is a leading cause of cancer-related deaths and in many cases is presented in stages requiring major hepatectomy. Adequate future liver remnant (FLR) volume is essential before any major hepatectomy. Portal vein embolization (PVE) has long
[...] Read more.
Background: Liver cancer, either primary or metastatic, is a leading cause of cancer-related deaths and in many cases is presented in stages requiring major hepatectomy. Adequate future liver remnant (FLR) volume is essential before any major hepatectomy. Portal vein embolization (PVE) has long been the standard technique for preoperative liver hypertrophy, but liver venous deprivation (LVD) has emerged as a novel method, potentially offering faster and superior results. The aim of this study is to compare FLR hypertrophy outcomes between LVD and PVE in patients undergoing major hepatectomy for liver malignancy. Methods: A systematic literature search was conducted across PubMed, Cochrane library, and clinicaltrials.gov for studies assessing FLR volume changes after LVD or PVE in patients with primary or secondary liver tumors undergoing liver resection. Data extraction was performed independently by two reviewers. The study protocol was registered in PROSPERO and was prepared according to the PRISMA guidelines. Results: Twelve retrospective cohort studies were included in this systematic review. Liver venous deprivation consistently demonstrated superior FLR hypertrophy, with a faster and higher percentage increase compared to PVE. Time to resection was also shorter in the LVD groups in most studies. Safety outcomes were comparable, with no consistent difference in post-procedural complications or mortality. Conclusions: Liver venous deprivation may potentially be a safe and effective alternative to PVE, offering more robust and rapid FLR hypertrophy with similar morbidity and mortality rates. While current evidence supports its superiority in selected patients, future validation with larger prospective clinical trials is essential before it can be adopted as standard management of patients with insufficient FLR volume.
Full article
Open AccessEditorial
Special Issue “Liver Fibrosis: Mechanisms, Targets, Assessment and Treatment”
by
Ralf Weiskirchen and Tilman Sauerbruch
Livers 2025, 5(3), 47; https://doi.org/10.3390/livers5030047 - 22 Sep 2025
Abstract
Liver fibrosis is a significant challenge in hepatology, as it represents the common pathway of chronic liver injury due to various causes such as viral hepatitis, metabolic dysfunction-associated steatotic liver disease (MASLD), intoxication, alcohol-related liver disease, autoimmune conditions, and genetic disorders [...]
Full article
(This article belongs to the Special Issue Liver Fibrosis: Mechanisms, Targets, Assessment and Treatment)
Open AccessReview
Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach
by
Mario Romeo, Carmine Napolitano, Paolo Vaia, Fiammetta Di Nardo, Silvio Borrelli, Carlo Garofalo, Luca De Nicola, Alessandro Federico and Marcello Dallio
Livers 2025, 5(3), 46; https://doi.org/10.3390/livers5030046 - 22 Sep 2025
Abstract
►▼
Show Figures
Ascites and renal dysfunction are among the most frequent and severe complications of decompensated advanced chronic liver disease (dACLD), often representing two interrelated manifestations of a shared pathophysiological continuum. Recurrent ascites and refractory ascites pose significant therapeutic challenges and are frequently associated with
[...] Read more.
Ascites and renal dysfunction are among the most frequent and severe complications of decompensated advanced chronic liver disease (dACLD), often representing two interrelated manifestations of a shared pathophysiological continuum. Recurrent ascites and refractory ascites pose significant therapeutic challenges and are frequently associated with kidney impairment, particularly hepatorenal syndrome. Recent advances have reshaped the understanding of the underlying mechanisms, moving beyond the classical paradigm of peripheral arterial vasodilation to encompass systemic inflammation, gut dysbiosis, and cirrhosis-associated immune dysfunction (CAID). These insights have prompted a shift from uniform treatment protocols toward personalized, multidisciplinary strategies. Therapeutic innovations such as long-term albumin infusion, a transjugular intrahepatic portosystemic shunt, and the Alfapump® system offer promising options, though each requires careful patient selection. Emerging approaches—including fecal microbiota transplantation and peritoneal dialysis—further expand the therapeutic landscape. Ultimately, early risk stratification, the integration of non-invasive tools, and individualized care models are essential to improving outcomes in this high-risk population. This review synthesizes current evidence and highlights future directions for the tailored management of dACLD patients with ascites and renal dysfunction.
Full article

Figure 1
Open AccessArticle
Effects of Chronic Elevation in Plasma Membrane Cholesterol on the Function of Human Na+/Taurocholate Cotransporting Polypeptide (NTCP) and Organic Cation Transporter 1 (OCT1)
by
Jessica Y. Idowu, Caylie McKimens and Bruno Hagenbuch
Livers 2025, 5(3), 45; https://doi.org/10.3390/livers5030045 - 12 Sep 2025
Abstract
►▼
Show Figures
Background: We have previously demonstrated that the function and expression of the Na+/taurocholate cotransporting polypeptide (NTCP) and the organic cation transporter 1 (OCT1) are affected by increasing free or unesterified cholesterol in the plasma membrane by an acute incubation with cholesterol
[...] Read more.
Background: We have previously demonstrated that the function and expression of the Na+/taurocholate cotransporting polypeptide (NTCP) and the organic cation transporter 1 (OCT1) are affected by increasing free or unesterified cholesterol in the plasma membrane by an acute incubation with cholesterol for 30 min. In the current study we wanted to extend these findings to a more chronic condition to mimic what would be seen in obese patients. Methods: We incubated HEK293 cells that stably express NTCP or OCT1 for 24 h with 0.05 mM cholesterol and determined their function by measuring uptake of radioactive taurocholate or MPP+. Expression at the plasma membrane was quantified with a biotinylation assay combined with Western blots. Results: Incubation with cholesterol increased the cholesterol content of the cells by about 2-fold. Transport mediated by NTCP and OCT1 was decreased. Membrane expression for both transporters showed a slight decrease, and when kinetics were normalized for the membrane expression, the Vmax for NTCP-mediated taurocholate uptake slightly decreased, but the Vmax and the capacity (Vmax/Km) for OCT1-mediated MPP+ uptake increased by 2.5-fold and 3-fold, respectively. Acyl-Coenzyme A acyltransferase inhibitors enhanced the decrease in transport function, potentially due to retention of more free cholesterol in the plasma membrane. Conclusions: Chronic increases in free cholesterol in the plasma membrane can result in increased or decreased transporter function and expression. In the case of OCT1, which is involved in the uptake of the anti-diabetic drug metformin into hepatocytes, the 3-fold increase in transport capacity might affect drug therapy.
Full article

Figure 1
Open AccessReview
Liver Transplantation for Colorectal Liver Metastasis: A Comprehensive Review of Current Practices and Future Trends
by
Zain Tariq, Affan Faisal, Sreevani Maheswaran, Narendra R. Battula, Paulo N. Martins and Maheswaran Pitchaimuthu
Livers 2025, 5(3), 44; https://doi.org/10.3390/livers5030044 - 10 Sep 2025
Abstract
Colorectal cancer (CRC) remains a leading cause of cancer-related mortality worldwide, with liver metastases (CRLM) representing a common and often incurable manifestation. While surgical resection combined with chemotherapy remains the standard for resectable disease, a significant subset of patients presents with unresectable CRLM.
[...] Read more.
Colorectal cancer (CRC) remains a leading cause of cancer-related mortality worldwide, with liver metastases (CRLM) representing a common and often incurable manifestation. While surgical resection combined with chemotherapy remains the standard for resectable disease, a significant subset of patients presents with unresectable CRLM. Recent advances have positioned liver transplantation (LT) as a promising therapeutic option for select patients with unresectable CRLM. This review synthesizes current evidence from landmark studies—including the SECA and TRANSMET trials—and emerging data from North American cohorts, highlighting the evolution of patient selection criteria, prognostic indicators such as the Oslo score and metabolic tumor volume, and the role of living-donor and extended-criteria grafts. Outcomes from recent studies demonstrate that LT can achieve 5-year overall survival rates exceeding 70% in well-selected patients, rivaling those of traditional transplant indications. Ongoing trials such as SECA-III and SOULMATE aim to refine indications and address organ allocation challenges. Collectively, these findings suggest that LT can offer long-term survival benefits comparable to traditional transplant indications, marking a paradigm shift in the management of metastatic CRC.
Full article
Open AccessReview
Linking Psychological Stress to Epigenetic Regulation via the Gut–Liver–Brain Axis in Irritable Bowel Syndrome and Metabolic Dysfunction-Associated Fatty Liver Disease
by
Annachiara Crocetta, Maria-Anna Giannelou, Agata Benfante, Lorys Castelli and Lemonica Koumbi
Livers 2025, 5(3), 43; https://doi.org/10.3390/livers5030043 - 5 Sep 2025
Abstract
►▼
Show Figures
Irritable Bowel Syndrome (IBS) and Metabolic dysfunction-associated fatty liver disease (MAFLD) have traditionally been viewed as disorders of distinct organ systems. IBS is a gut–brain axis disorder characterized by abdominal pain, altered bowel habits, and psychological comorbidities. MAFLD, recently redefined to emphasize its
[...] Read more.
Irritable Bowel Syndrome (IBS) and Metabolic dysfunction-associated fatty liver disease (MAFLD) have traditionally been viewed as disorders of distinct organ systems. IBS is a gut–brain axis disorder characterized by abdominal pain, altered bowel habits, and psychological comorbidities. MAFLD, recently redefined to emphasize its metabolic underpinnings, is the hepatic manifestation of systemic metabolic dysfunction. Growing evidence suggests that these conditions share overlapping pathophysiological mechanisms linked through disruption of the gut–liver–brain axis (GLBA), including psychological stress, gut dysbiosis, impaired intestinal permeability, systemic inflammation, and altered neuroendocrine signaling. Neuroimaging studies further reveal functional alterations in brain regions responsible for interoception, emotional regulation, and stress responsiveness in both disorders. This narrative review explores how psychological distress influences the onset and progression of IBS and MAFLD via GLBA dysfunction and stress-induced epigenetic reprogramming. A targeted literature search of major biomedical databases, supplemented by manual screening, identified relevant observational, clinical, neuroimaging, and molecular studies. Findings indicate that chronic psychological distress activates the hypothalamic–pituitary–adrenal (HPA) axis, elevates cortisol, disrupts gut microbiota, and reduces vagal tone; amplifying intestinal permeability and microbial translocation. These changes promote hepatic inflammation and gastrointestinal symptoms. Stress-related epigenetic modifications further impair GLBA communication, while psychological and lifestyle interventions may reverse some of these molecular imprints. Recognizing the shared neuromodulation and epigenetic mechanisms that link IBS and MAFLD opens promising avenues for integrated therapeutic strategies targeting the GLBA to improve outcomes across both conditions.
Full article

Graphical abstract
Open AccessReview
Hepatotoxicity of Herbal and Dietary Supplements a Review of Diagnosis, Histologic Features, and Common Culprits: Bodybuilding and Weight Loss Supplements
by
Esmeralda Celia Marginean
Livers 2025, 5(3), 42; https://doi.org/10.3390/livers5030042 - 2 Sep 2025
Abstract
►▼
Show Figures
Herbal and dietary supplements (HDS) are used by over half of American adults and represent a multi-billion-dollar industry. More recently, they have gained popularity, in part due to promotion on multiple social media platforms. However, the Food and Drug Administration (FDA) does not
[...] Read more.
Herbal and dietary supplements (HDS) are used by over half of American adults and represent a multi-billion-dollar industry. More recently, they have gained popularity, in part due to promotion on multiple social media platforms. However, the Food and Drug Administration (FDA) does not regulate these products rigorously, and up to 20% of acute liver injuries are attributed to HDS. The true incidence of HDS hepatotoxicity is unknown but thought to be underreported. According to the World Health Organization (WHO), HDS-induced liver injuries are now the fifth most common cause of liver disease–associated death. The most common type of supplements associated with liver injury are bodybuilding and weight loss supplements. This study represents a comprehensive literature review of HDS-induced liver injury with a focus on the two most common culprits: bodybuilding supplements and weight loss supplements. Future strategies recommended to mitigate hepatotoxicity include strengthening regulatory oversight through mandatory product listing, enhancing post-market surveillance with standardized reporting and registries, improving product quality via ingredient verification and contaminant testing and, possibly, implementing standardized risk labeling.
Full article
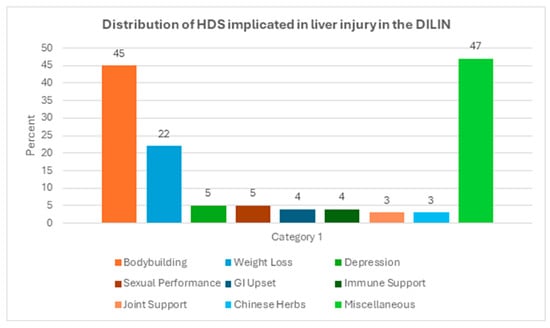
Figure 1
Open AccessFeature PaperArticle
Ketosis Suppression and Ageing (KetoSAge): The Effect of Suppressing Ketosis on GKI and Liver Biomarkers in Healthy Females
by
Isabella D. Cooper, Lucy Petagine, Adrian Soto-Mota, Tomás Duraj, Andrew Scarborough, Nicolas G. Norwitz, Thomas N. Seyfried, Maricel A. Furoni and Yvoni Kyriakidou
Livers 2025, 5(3), 41; https://doi.org/10.3390/livers5030041 - 2 Sep 2025
Abstract
►▼
Show Figures
Background: As the growing global population continues to age, the risk of chronic metabolic diseases, including cardiovascular disease, neurodegenerative disorders, type 2 diabetes mellitus, and fatty liver disease, increases considerably. Driven largely by lifestyle factors and metabolic dysfunction, this escalating health crisis is
[...] Read more.
Background: As the growing global population continues to age, the risk of chronic metabolic diseases, including cardiovascular disease, neurodegenerative disorders, type 2 diabetes mellitus, and fatty liver disease, increases considerably. Driven largely by lifestyle factors and metabolic dysfunction, this escalating health crisis is placing mounting pressure on healthcare systems and contributing to significant economic costs. Insulin resistance and hyperinsulinaemia are major drivers of these disorders, emphasising the need for early detection and intervention. Changes in liver enzymes, such as alanine aminotransferase (ALT) and gamma-glutamyl transferase (GGT), commonly assessed in routine laboratory testing, can serve as biomarkers of early-stage insulin resistance, offering a potentially underutilised window for intervention and disease prevention. Correspondingly, low-carbohydrate ketogenic diets have shown to be effective in reversing insulin resistance, metabolic disease, and liver disease. Objectives: We chose to explore the relationship between suppressing ketosis and changes in liver enzymes in the Ketosis Suppression and Ageing cohort. Methods: Ten lean (BMI 20.5 kg/m2 ± 1.4), healthy young women (age 32.3 ± 8.9 years) who habitually followed a ketogenic diet maintaining nutritional ketosis (NK) for an average of 3.9 years (±2.3) were exposed to a higher carbohydrate diet, in line with standard healthy eating guidelines for a 21-day phase and then transitioned back to a ketogenic diet. Results: Carbohydrate challenge and suppression of ketosis increased insulin resistance score HOMA-IR by 2.13-fold (p = 0.0008), GKI by 22.28-fold (p = 0.0024), and liver markers ALT by 1.85-fold (p = 0.0010), GGT, 1.29-fold (p = 0.0087) and the ALT/AST, 1.30-fold (p = 0.0266), reflecting an adverse pattern suggestive of hepatic insulin resistance. Conclusions: These results support the clinical utility of liver markers as early and directional signs of hyperinsulinaemia.
Full article

Graphical abstract
Open AccessCase Report
Shades of Gray: Diagnostic Challenges and Fatal Tumor Thromboembolism in Periductal-Infiltrating Perihilar Cholangiocarcinoma—Case Report with Autopsy Findings
by
Mihnea Horia Strain, Maike Koch, Basem Salayma, Lkhagvadorj Byambaa, Sven Wylenga, Sven Müller, Christopher D. Intemann and Johannes König
Livers 2025, 5(3), 40; https://doi.org/10.3390/livers5030040 - 27 Aug 2025
Abstract
►▼
Show Figures
Background: Perihilar cholangiocarcinoma (pCCA), especially the periductal-infiltrating subtype, is notoriously difficult to diagnose due to subtle imaging findings and the absence of a mass. Case Presentation: We describe a 56-year-old man with morbid obesity and deep vein thrombosis (DVT), admitted for severe cholestatic
[...] Read more.
Background: Perihilar cholangiocarcinoma (pCCA), especially the periductal-infiltrating subtype, is notoriously difficult to diagnose due to subtle imaging findings and the absence of a mass. Case Presentation: We describe a 56-year-old man with morbid obesity and deep vein thrombosis (DVT), admitted for severe cholestatic jaundice. Initial ultrasound and two ERCPs were inconclusive, with only mild hilar duct dilation on CT. MRI was not possible due to the severe weight of the patient. Only at the 3rd ERCP with digital cholangioscopy were irregular mucosa and tumor infiltration observed, and a biopsy confirmed moderately to poorly differentiated adenocarcinoma. The patient deteriorated rapidly after discharge, returning in septic shock. Despite laparoscopy excluding cholecystitis and cirrhosis, he died from multiorgan failure. Autopsy revealed diffuse hilar tumor infiltration, nodal metastases, and fatal pulmonary tumor embolism (Bismuth IV). Conclusions: This case highlights the necessity of early escalation to cholangioscopy in unresolved cholestasis, the importance of recognizing paraneoplastic thrombosis, and the value of autopsy in clarifying cause of death.
Full article

Figure 1
Open AccessReview
Palliative Care in End-Stage Liver Disease
by
Luisa Sousa, Sofia Marques Silva, Francisca Rego, Rui Nunes and Hugo M. Oliveira
Livers 2025, 5(3), 39; https://doi.org/10.3390/livers5030039 - 22 Aug 2025
Abstract
►▼
Show Figures
Chronic liver disease is a significant global cause of morbidity and mortality. While early-stage liver cirrhosis is often asymptomatic, it can progress to a decompensated phase known as end-stage liver disease (ESLD), resulting in a high symptom burden, diminished quality of life, and
[...] Read more.
Chronic liver disease is a significant global cause of morbidity and mortality. While early-stage liver cirrhosis is often asymptomatic, it can progress to a decompensated phase known as end-stage liver disease (ESLD), resulting in a high symptom burden, diminished quality of life, and frequent hospitalizations. Palliative care is a form of specialized care aimed at addressing the needs of patients; however, it remains underutilized in ESLD patients. Globally, the integration of palliative care into ESLD is impeded by several barriers. Certain factors—such as advanced age, the presence of hepatocellular carcinoma (HCC), and transplant listing status—have been associated with higher rates of palliative care referral. This review provides a comprehensive analysis of the current literature, emphasizing the benefits of palliative care interventions in ESLD, including improved symptom control and enhanced quality of life. It also underscores the impact on caregivers and healthcare systems, notably in reducing hospital readmissions. We advocate for a paradigm shift toward proactive, patient-centered models that integrate symptom management, advance care planning, and psychosocial support alongside disease-specific treatments for patients with ESLD.
Full article

Figure 1
Open AccessArticle
Patterns and Outcomes of Alcoholic Liver Disease (ALD) in Oman: A Retrospective Study in a Culturally Conservative Context
by
Said A. Al-Busafi, Thuwiba A. Al Baluki and Ahmed Alwassief
Livers 2025, 5(3), 38; https://doi.org/10.3390/livers5030038 - 18 Aug 2025
Abstract
►▼
Show Figures
Background: Alcoholic liver disease (ALD) contributes substantially to global liver-related morbidity and mortality. In conservative societies such as Oman, data on ALD are scarce due to stigma and legal constraints. This study aims to characterize the clinical spectrum, complications, and outcomes of
[...] Read more.
Background: Alcoholic liver disease (ALD) contributes substantially to global liver-related morbidity and mortality. In conservative societies such as Oman, data on ALD are scarce due to stigma and legal constraints. This study aims to characterize the clinical spectrum, complications, and outcomes of ALD in Oman, providing the first detailed analysis from a tertiary care setting in the country. Methods: We retrospectively analyzed 131 Omani patients with documented unhealthy alcohol use from 2012 to 2018 at Sultan Qaboos University Hospital. ALD diagnosis was based on clinician judgment per EASL guidelines and DSM-5 criteria, where applicable. Data included demographics, clinical/laboratory findings, and radiologic/endoscopic features. Associations with complications and mortality were assessed using chi-square tests and logistic regression. Results: Of 131 patients, 84 (64.1%) were diagnosed with ALD: fatty liver (34.5%), alcoholic hepatitis (20.2%), cirrhosis (40.5%), and hepatocellular carcinoma (4.8%). Cirrhosis was significantly more prevalent in patients aged 50 years or older (OR = 2.53, 95% CI: 1.02–6.28; p = 0.048). Ascites and portal hypertension were strongly associated with mortality (OR = 5.20, CI: 1.85–14.6 and OR = 6.13, CI: 2.04–18.4, respectively; p < 0.01). Overall mortality in ALD was 28.6%, increasing to 44.1% in cirrhotics. Conclusion: ALD is a significant yet underrecognized problem in Oman, with high rates of late-stage presentation and mortality. Early detection and culturally tailored strategies are needed to improve care outcomes.
Full article

Figure 1
Open AccessReview
Cutaneous Manifestations of Liver Cirrhosis: Clinical Significance and Diagnostic Implications
by
Rita Kamoua, Rebecca Reese, Risha Annamraju, Tian Chen, Colleen Doyle, Adriana Parella, Amelia Liu, Yazan Abboud, Craig Rohan and Jeffrey B. Travers
Livers 2025, 5(3), 37; https://doi.org/10.3390/livers5030037 - 15 Aug 2025
Abstract
Liver cirrhosis, a progressive and often irreversible condition, exerts widespread systemic effects, with the skin frequently serving as a visible window into the extent of hepatic dysfunction. Cutaneous manifestations, such as spider angiomas, palmar erythema, jaundice, and pruritus, not only reflect underlying pathophysiologic
[...] Read more.
Liver cirrhosis, a progressive and often irreversible condition, exerts widespread systemic effects, with the skin frequently serving as a visible window into the extent of hepatic dysfunction. Cutaneous manifestations, such as spider angiomas, palmar erythema, jaundice, and pruritus, not only reflect underlying pathophysiologic changes but also serve as important, non-invasive diagnostic and prognostic markers of disease severity. Early detection of such cutaneous findings may allow for early treatment, optimize patient management, and improve outcomes. This review addresses the various cutaneous manifestations of liver cirrhosis, their pathogenesis, and their prognostic and diagnostic importance, emphasizing the need for heightened clinical awareness of the improvement in patient care.
Full article
(This article belongs to the Special Issue Liver Fibrosis: Mechanisms, Targets, Assessment and Treatment)
►▼
Show Figures

Figure 1
Open AccessArticle
Serum Level of Glypican-3 in Patients with Hepatocellular Carcinoma and Advanced Chronic Liver Disease: A Pilot Study
by
Irina Ivanova, Sonya Banova-Chakyrova, Pavlina Boykova-Vylcheva and Yana Bocheva
Livers 2025, 5(3), 36; https://doi.org/10.3390/livers5030036 - 8 Aug 2025
Abstract
►▼
Show Figures
Background: Early diagnosis of hepatocellular carcinoma (HCC) and monitoring of therapeutic results remain clinical challenges. Methods: In a prospective study, we evaluated the diagnostic capabilities of the serum level of glypican-3 in 70 patients with chronic advanced compensated liver disease: 40 cases with
[...] Read more.
Background: Early diagnosis of hepatocellular carcinoma (HCC) and monitoring of therapeutic results remain clinical challenges. Methods: In a prospective study, we evaluated the diagnostic capabilities of the serum level of glypican-3 in 70 patients with chronic advanced compensated liver disease: 40 cases with confirmed HCC and 30 cases with chronic viral hepatitis with bridging fibrosis or cirrhosis as a control group. The glypican-3 concentration was analyzed in the context of the disease characteristics. Results: The mean level of glypican-3 in HCC patients was 50.84 ± 75.98 ng/mL, significantly higher compared to the control group of 5.69 ± 10.43 ng/mL. A progressive increase in alpha-fetoprotein in accordance with the stage of neoplastic disease was observed, but this tendency was not assessed for glypican-3. Two cut-off levels can be suggested for glypican-3: 2.5 ng/mL to exclude HCC with an optimal sensitivity of 85%, and 33.7 ng/mL for confirmation of HCC, with a specificity of 96.7%. The diagnostic accuracy of serum glypican-3 was 80.0% for HCC, 82.1% for alpha-fetoprotein, and 87.4% for both tumor markers. Conclusions: This pilot study suggests a complementary role of glypican-3 with alpha-fetoprotein and better diagnostic performance when combining tumor biomarkers.
Full article

Figure 1
Open AccessReview
Synthalin, Buformin, Phenformin, and Metformin: A Century of Intestinal “Glucose Excretion” as Oral Antidiabetic Strategy in Overweight/Obese Patients
by
Giuliano Pasquale Ramadori
Livers 2025, 5(3), 35; https://doi.org/10.3390/livers5030035 - 31 Jul 2025
Abstract
►▼
Show Figures
After the first release of synthalin B (dodecamethylenbiguanide) in 1928 and its later retraction in the 1940s in Germany, the retraction of phenformin (N-Phenethylbiguanide) and of Buformin in the USA (but not outside) because of the lethal complication of acidosis seemed to have
[...] Read more.
After the first release of synthalin B (dodecamethylenbiguanide) in 1928 and its later retraction in the 1940s in Germany, the retraction of phenformin (N-Phenethylbiguanide) and of Buformin in the USA (but not outside) because of the lethal complication of acidosis seemed to have put an end to the era of the biguanides as oral antidiabetics. The strongly hygroscopic metformin (1-1-dimethylbiguanide), first synthesized 1922 and resuscitated as an oral antidiabetic (type 2 of the elderly) compound first released in 1959 in France and in other European countries, was used in the first large multicenter prospective long-term trial in England in the UKPDS (1977–1997). It was then released in the USA after a short-term prospective trial in healthy overweight “young” type 2 diabetics (mean age 53 years) in 1995 for oral treatment of type 2 diabetes. It was, however, prescribed to mostly multimorbid older patients (above 60–65 years of age). Metformin is now the most used oral drug for type 2 diabetes worldwide. While intravenous administration of biguanides does not have any glucose-lowering effect, their oral administration leads to enormous increase in their intestinal concentration (up to 300-fold compared to that measured in the blood), to reduced absorption of glucose from the diet, to increased excretion of glucose through the stool, and to decrease in insulin serum level through increased hepatic uptake and decreased production. Intravenously injected F18-labeled glucose in metformin-treated type 2 diabetics accumulates in the small and even more in the large intestine. The densitometry picture observed in metformin-treated overweight diabetics is like that observed in patients after bowel-cleansing or chronically taking different types of laxatives, where the accumulated radioactivity can even reach values observed in colon cancer. The glucose-lowering mechanism of action of metformin is therefore not only due to inhibition of glucose uptake in the small intestine but also to “attraction” of glucose from the hepatocyte into the intestine, possibly through the insulin-mediated uptake in the hepatocyte and its secretion into the bile. Furthermore, these compounds have also a diuretic effect (loss of sodium and water in the urine) Acute gastrointestinal side effects accompanied by fluid loss often lead to the drugs’ dose reduction and strongly limit adherence to therapy. Main long-term consequences are “chronic” dehydration, deficiency of vitamin B12 and of iron, and, as observed for all the biguanides, to “chronic” increase in fasting and postprandial lactate plasma level as a laboratory marker of a clinical condition characterized by hypotension, oliguria, adynamia, and evident lactic acidosis. Metformin is not different from the other biguanides: synthalin B, buformin, and phenformin. The mechanism of action of the biguanides as antihyperglycemic substances and their side effects are comparable if not even stronger (abdominal pain, nausea, vomiting, diarrhea, fluid loss) to those of laxatives.
Full article

Figure 1
Open AccessReview
Low Hepatic CEACAM1 Tethers Metabolic Dysfunction Steatohepatitis to Atherosclerosis
by
Sacha El Khoury, Sami N. Al Harake, Tya Youssef, Carl E. Risk, Naim G. Helou, Natalie M. Doumet, Karl Aramouni, Sami Azar, Sonia M. Najjar and Hilda E. Ghadieh
Livers 2025, 5(3), 34; https://doi.org/10.3390/livers5030034 - 30 Jul 2025
Cited by 1
Abstract
Metabolic dysfunction-associated steatohepatitis (MASH) and atherosclerosis are cardiometabolic twin disorders with shared underlying pathophysiological mechanisms such as insulin resistance and chronic inflammation. This review explores the salient role of carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1) in linking hepatic dysfunction to cardiovascular disease.
[...] Read more.
Metabolic dysfunction-associated steatohepatitis (MASH) and atherosclerosis are cardiometabolic twin disorders with shared underlying pathophysiological mechanisms such as insulin resistance and chronic inflammation. This review explores the salient role of carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1) in linking hepatic dysfunction to cardiovascular disease. Findings in mice with genetic modulation of Ceacam1 gene established a critical role for CEACAM1 protein in regulating insulin and lipid metabolism and endothelial integrity and modulating immune response. Loss of CEACAM1 in hepatocytes impairs insulin clearance, causing chronic hyperinsulinemia, a process that ultimately leads to insulin resistance and hepatic and extra-hepatic fat accumulation, which in turn causes inflammatory infiltration. This prompts a paradigm shift that positions impaired hepatic CEACAM1 function as a mechanistic underpinning of the link between insulin resistance, MASH, and atherosclerosis.
Full article
(This article belongs to the Special Issue Liver Fibrosis: Mechanisms, Targets, Assessment and Treatment)
►▼
Show Figures

Figure 1
Open AccessReview
Multifaceted Human Antigen R (HuR): A Key Player in Liver Metabolism and MASLD
by
Natalie Eppler, Elizabeth Jones, Forkan Ahamed and Yuxia Zhang
Livers 2025, 5(3), 33; https://doi.org/10.3390/livers5030033 - 21 Jul 2025
Abstract
►▼
Show Figures
Metabolic dysfunction-associated steatotic liver disease (MASLD) has become the leading cause of chronic liver disease worldwide, affecting approximately 25–30% of the global adult population and highlighting the urgent need for effective therapeutics and prevention strategies. MASLD is characterized by excessive hepatic lipid accumulation
[...] Read more.
Metabolic dysfunction-associated steatotic liver disease (MASLD) has become the leading cause of chronic liver disease worldwide, affecting approximately 25–30% of the global adult population and highlighting the urgent need for effective therapeutics and prevention strategies. MASLD is characterized by excessive hepatic lipid accumulation and can progress, in a subset of patients, to metabolic dysfunction-associated steatohepatitis (MASH), a pro-inflammatory and pro-fibrotic condition associated with increased risk of liver cirrhosis and hepatocellular carcinoma. Although the molecular drivers of MASLD progression remain incompletely understood, several key metabolic pathways—such as triglyceride handling, cholesterol catabolism, bile acid metabolism, mitochondrial function, and autophagy—are consistently dysregulated in MASLD livers. This narrative review summarizes primary literature and highlights insights from recent reviews on the multifaceted role of the mRNA-binding protein Human antigen R (HuR) in the post-transcriptional regulation of critical cellular processes, including nutrient metabolism, cell survival, and stress responses. Emerging evidence underscores HuR’s essential role in maintaining liver homeostasis, particularly under metabolic stress conditions characteristic of MASLD, with hepatocyte-specific HuR depletion associated with exacerbated disease severity. Moreover, comorbid conditions such as obesity, type 2 diabetes mellitus, and cardiovascular disease not only exacerbate MASLD progression but also involve HuR dysregulation in extrahepatic tissues, further contributing to liver dysfunction. A deeper understanding of HuR-regulated post-transcriptional networks across metabolic organs may enable the development of targeted therapies aimed at halting or reversing MASLD progression.
Full article

Figure 1
Open AccessArticle
Robotic Liver Resection for Breast Cancer Metastasis: A Multicenter Case Series and Literature Review
by
Silvio Caringi, Antonella Girardi, Francesca Ratti, Paolo Magistri, Andrea Belli, Giuseppe Memeo, Tommaso Maria Manzia, Francesco Izzo, Nicola De’Angelis, Fabrizio Di Benedetto, Luca Aldrighetti and Riccardo Memeo
Livers 2025, 5(3), 32; https://doi.org/10.3390/livers5030032 - 15 Jul 2025
Abstract
Background: Breast cancer is a widespread disease and, when metastatic, has a bleak prognosis. The surgical approach for BCLM has had a limited role, but robotic surgery could find an important place. Methods: Data were collected from a multicenter retrospective database that includes
[...] Read more.
Background: Breast cancer is a widespread disease and, when metastatic, has a bleak prognosis. The surgical approach for BCLM has had a limited role, but robotic surgery could find an important place. Methods: Data were collected from a multicenter retrospective database that includes 1070 consecutive robotic liver resections performed in nine European hospital centers from 2011 to 2023. Of the entire series, 35 were performed for BCLM in five European hospital centers. Results: The post-operative complication rate was 11.44%, but no severe complications occurred. The mean hospital stay was 4.65 days. One patient (2.85%) was readmitted to the hospital within 90 days after discharge and died due to heart failure, with a 90-day mortality of 2.85%. Conclusions: Robotic liver resection for BCLM is feasible and safe when performed in experienced centers by surgeons who have completed the learning curve.
Full article
Open AccessReview
Exploring the Role of Probiotics, Prebiotics, and Synbiotics in the Treatment of Metabolic Dysfunction-Associated Steatotic Liver Disease—A Scoping Review
by
Anastasia Ntikoudi, Anastasia Papachristou, Alketa Spirou, Eleni Evangelou, Athanasios Tsartsalis, Eugenia Vlachou and George Mastorakos
Livers 2025, 5(3), 31; https://doi.org/10.3390/livers5030031 - 7 Jul 2025
Abstract
►▼
Show Figures
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) has emerged as the most prevalent chronic liver condition. Its prevalence is estimated to further increase. The gut–liver axis, which represents both anatomical and functional connections, contributes significantly to the development of MASLD. Dysbiosis, characterized by
[...] Read more.
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) has emerged as the most prevalent chronic liver condition. Its prevalence is estimated to further increase. The gut–liver axis, which represents both anatomical and functional connections, contributes significantly to the development of MASLD. Dysbiosis, characterized by an imbalance in gut microbiota, can exacerbate the disease by increasing intestinal permeability, which permits harmful bacteria and their components to enter the bloodstream. This review sought to explore the impact of probiotics, prebiotics, and synbiotics on the treatment of MASLD. Method: The methodology for scoping reviews in accordance with Prisma-ScR guidelines was followed. A comprehensive search was conducted in databases such as PubMed, Scopus, and Medline. Out of 1390 studies screened, 25 were selected for the final analysis. Results: The findings of this scoping review highlight the therapeutic potential of probiotics, prebiotics, and synbiotics in the management and treatment of MASLD, as showcased by the existing literature. Conclusions: This scoping review offers important insights into the advantages of probiotics, prebiotics, and synbiotics in the treatment of MASLD. The limitations identified in this study emphasize the necessity for larger, long-term, and geographically diverse studies in order to obtain more solid scientific results.
Full article

Figure 1
Open AccessArticle
Hepatitis C Virus Opportunistic Screening in South-Eastern Tuscany Residents Admitted to the University Hospital in Siena
by
Cristina Stasi, Tommaso Marzotti, Filippo Nassi, Giovanna Giugliano, Sabrina Pacini, Silvia Rentini, Riccardo Accioli, Raffaele Macchiarelli, Luigi Gennari, Pietro Enea Lazzerini and Stefano Brillanti
Livers 2025, 5(3), 30; https://doi.org/10.3390/livers5030030 - 30 Jun 2025
Abstract
Background. To meet the WHO’s viral hepatitis elimination goal by 2030, the Minister of Health (Italy) introduced free HCV screening among people born between 1969 and 1989 and those at greater risk (people in the care of the addiction services and detained).
[...] Read more.
Background. To meet the WHO’s viral hepatitis elimination goal by 2030, the Minister of Health (Italy) introduced free HCV screening among people born between 1969 and 1989 and those at greater risk (people in the care of the addiction services and detained). Aims. To estimate the following: (i) the prevalence of HCV in hospitalized patients born before 1969 not included in the free HCV screening, (ii) the prevalence of transaminase values outside the range, and (iii) the HBV prevalence in a subgroup of patients. Methods. Anti-HCV antibodies and transaminase values were prospectively evaluated in patients born before 1969 and admitted to the Santa Maria alle Scotte Hospital in Siena. The first screening (October 2021–July 2022) was conducted in the Internal Medicine Division (cohort 0), and the second one (May 2024–October 2024) in Internal Medicine, Gastroenterology, and Geriatric Units (cohorts 1–3), including clinical features and HBV markers in a subgroup of patients. Results. Overall, 774 subjects underwent HCV screening. In the first screening period, 1.4% (8/567) of patients were anti-HCV+, of whom 0.7% were HCV RNA+ (4/567). In the second, 3.9% of patients (8/207) were anti-HCV+ and 0.9% were viremic (2/207). Overall, HCV prevalence was 0.8%. Of 96 patients in the gastroenterology cohort, 8 patients were at risk for occult HBV infection (8.3%). Conclusions. Our study demonstrates a chronic HCV infection prevalence of 0.8% in hospitalised patients born before 1969 and a prevalence of 8.3% of people at risk for occult HBV infection in a subgroup of patients residing in South-Eastern Tuscany, confirming that an opportunistic screening can identify the unrecognized people affected by viral hepatitis.
Full article
(This article belongs to the Special Issue The Surveillance, Prevention, and Treatment of Viral Hepatitis: Looking Forward to Global Elimination)
►▼
Show Figures

Figure 1
Open AccessReview
Liver and Vascular Involvement in Philadelphia-Negative Chronic Myeloproliferative Neoplasms—A Narrative Review
by
Romeo G. Mihăilă, Samuel B. Todor and Marius D. Mihăilă
Livers 2025, 5(3), 29; https://doi.org/10.3390/livers5030029 - 30 Jun 2025
Abstract
►▼
Show Figures
Hepatosplenomegaly can occur in extrahepatic diseases such as Philadelphia-negative chronic myeloproliferative neoplasms (MPNs), which may involve the liver and vasculature. In myelofibrosis, extramedullary hematopoiesis can be present in the liver, even within hepatic sinusoids. Liver biopsies in MPN patients have shown platelet aggregates
[...] Read more.
Hepatosplenomegaly can occur in extrahepatic diseases such as Philadelphia-negative chronic myeloproliferative neoplasms (MPNs), which may involve the liver and vasculature. In myelofibrosis, extramedullary hematopoiesis can be present in the liver, even within hepatic sinusoids. Liver biopsies in MPN patients have shown platelet aggregates obstructing these sinusoids. Both liver and spleen stiffness are significantly higher in myelofibrosis, correlating with the severity of bone marrow fibrosis. Spleen stiffness is also elevated in myelofibrosis and polycythemia Vera compared to essential thrombocythemia. MPNs are a leading cause of splanchnic vein thrombosis in the absence of cirrhosis or local malignancy, especially in the presence of the JAK2V617F mutation. This mutation promotes thrombosis through endothelial dysfunction and inflammation. It is found in endothelial cells, where it enhances leukocyte adhesion and upregulates thrombogenic and inflammatory genes. Hepatic sinusoidal microthromboses in MPNs may contribute to portal hypertension and liver dysfunction. MPN therapies can also affect liver function. While hepatocytolysis has been reported, agents such as Hydroxycarbamide and Ruxolitinib exhibit antifibrotic hepatic effects in experimental models. Overall, MPNs are linked to chronic inflammation, increased thrombotic risk—particularly splanchnic thrombosis—and atherogenesis.
Full article
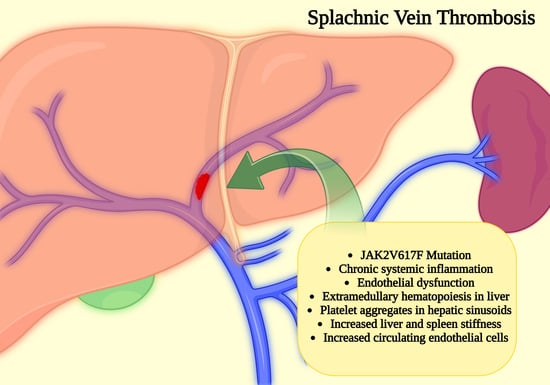
Graphical abstract
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biomolecules, Cancers, Cells, JMP, Livers
Signaling Pathways in Liver Disease 2nd Edition
Topic Editors: Ralf Weiskirchen, Amedeo AmedeiDeadline: 20 March 2026
Topic in
Biomedicines, Current Oncology, Diagnostics, JCM, Livers, Transplantology, Gastrointestinal Disorders
Advances in Gastrointestinal and Liver Disease: From Physiological Mechanisms to Clinical Practice, 2nd Edition
Topic Editors: Davide Giuseppe Ribaldone, Gian Paolo CavigliaDeadline: 20 December 2026

Conferences
Special Issues
Special Issue in
Livers
The Surveillance, Prevention, and Treatment of Viral Hepatitis: Looking Forward to Global Elimination
Guest Editor: Melanie DeutschDeadline: 31 October 2025
Special Issue in
Livers
Mechanistic and Prognostic Biomarkers in Liver Diseases
Guest Editors: Hartmut W. Jaeschke, Mitchell McGillDeadline: 30 November 2025
Special Issue in
Livers
Liver Cancer Heterogeneity in the Era of Single-Cell and Spatial Multiomics
Guest Editors: Veronika Lukacs-Kornek, Ralf WeiskirchenDeadline: 30 December 2025
Special Issue in
Livers
Recent Advances in the Detection and Pathophysiology of Steatotic, Alcoholic and Drug-Induced Liver Diseases
Guest Editors: Leonard Nelson, Michel Kranendonk, Anabel Martinez Lyons, Francisco EstevesDeadline: 31 December 2025