1. Introduction
Following the COVID-19 emergency, face-to-face teaching activities relating to the 2019/2020 school year had to be suspended throughout Italy from March 2020, activating distance learning to protect the school staff and students’ health and guaranteeing the continuation of study.
The following school year continued to alternate between closure and reopening. Various procedures have been taken to ensure the safe resumption of classes in person, such as physical distancing, the obligation to wear a mask, and body temperature measurement.
All these practices are used to prevent infection. In particular, body temperature detection is a parameter that can be characteristic of active infections.
To reduce the infections of the SARS-CoV-2 virus, several types of body temperature sensors are used to monitor people’s access to enclosed spaces. More specifically, thermal imaging cameras and infrared thermometers are extensively used for this aim. However, these approaches cause the concentration of people at checkpoints, increasing the risk of exposure. In addition, the risk of COVID-19 in some buildings, where the people are located for several hours, e.g., schools, universities, or industries, could be reduced by continuously monitoring body temperature.
In many cases, a high-precision and wearable sensors network is the only possible solution to implement punctual (capillary) and continuous real-time monitoring of one or more quantities of interest (physical or biochemical) to prevent a cluster of infections and to safeguard health.
Wearable sensors technology is growing as researchers and developers learn of its potential benefits and possibilities [
1].
Many applications, e.g., electronics or smartphone applications, encourage physical activity by measuring the user’s daily step count and other parameters. Wearable sensors can come in the form of a wearable sensor network, also known as a wearable body sensor network, or even a wearable health monitoring system (WHMS) [
2].
In a wearable sensor network, multiple sensors can communicate to one another or with a server to form a network, with great potential, particularly in medical and safety applications. In fact, wearable sensor networks have been successfully used to monitor body parameters, such as fluid, ph, temperature, blood pressure, etc., leading to the opportunity to monitor our health during activity, with immediate feedback on a smartphone or a PC [
3].
However, this approach is typically used only in physical activities, and it is realized exploiting a personal device (e.g., smartwatches).
Numerous scientists have been bringing forward different research lines on body temperature monitoring sensors for 10 years, proving that wearable body sensor networks are a potential tool for the real-time monitoring of vital parameters. Their flexibility, constant, and low-cost operation make them suitable for applications ranging from medical diagnosis, patient monitoring, and disease treatment. Many branches of medical science benefit from a non-invasive and low-cost tool that enables the accurate measurement of body temperature. Body sensor networks have the potential to improve medical research [
4].
Important examples of wearable sensor networks are also the applications of this technology for temperature monitoring to investigate psychological and emotional changes in biomedical applications [
5] or for temperature measurements in different environments for several application fields, as in [
6,
7,
8].
In this work, we present the exploitation of a wearable sensor network for the continuous monitoring of school staff and students’ body temperature to reduce the risk of SARS-CoV-2 infection in the school and thus allow for on-site learning activities. More specifically, we have designed a sensing strategy based on a body temperature sensor network and its specific application to address the COVID-19 emergency in a school scenario. After that, we installed approximately 4500 devices in three schools, and its test is in progress. The three schools are located in the province of Naples (Italy), and it could be extended to other schools.
2. A Sensor Network for Body Temperature Detection
We have proposed and tested a wearable body temperature sensor to realize an interesting sensor network used to implement the continuous and real-time temperature monitoring of people in school buildings. The used temperature sensors measure the parameter of interest and transmit it via Bluetooth 5.0 to smartphones and/or custom gateways (with a maximum of about 150 per gateway and about 50 per smartphone). Then, the collected data are transmitted on a server via the internet.
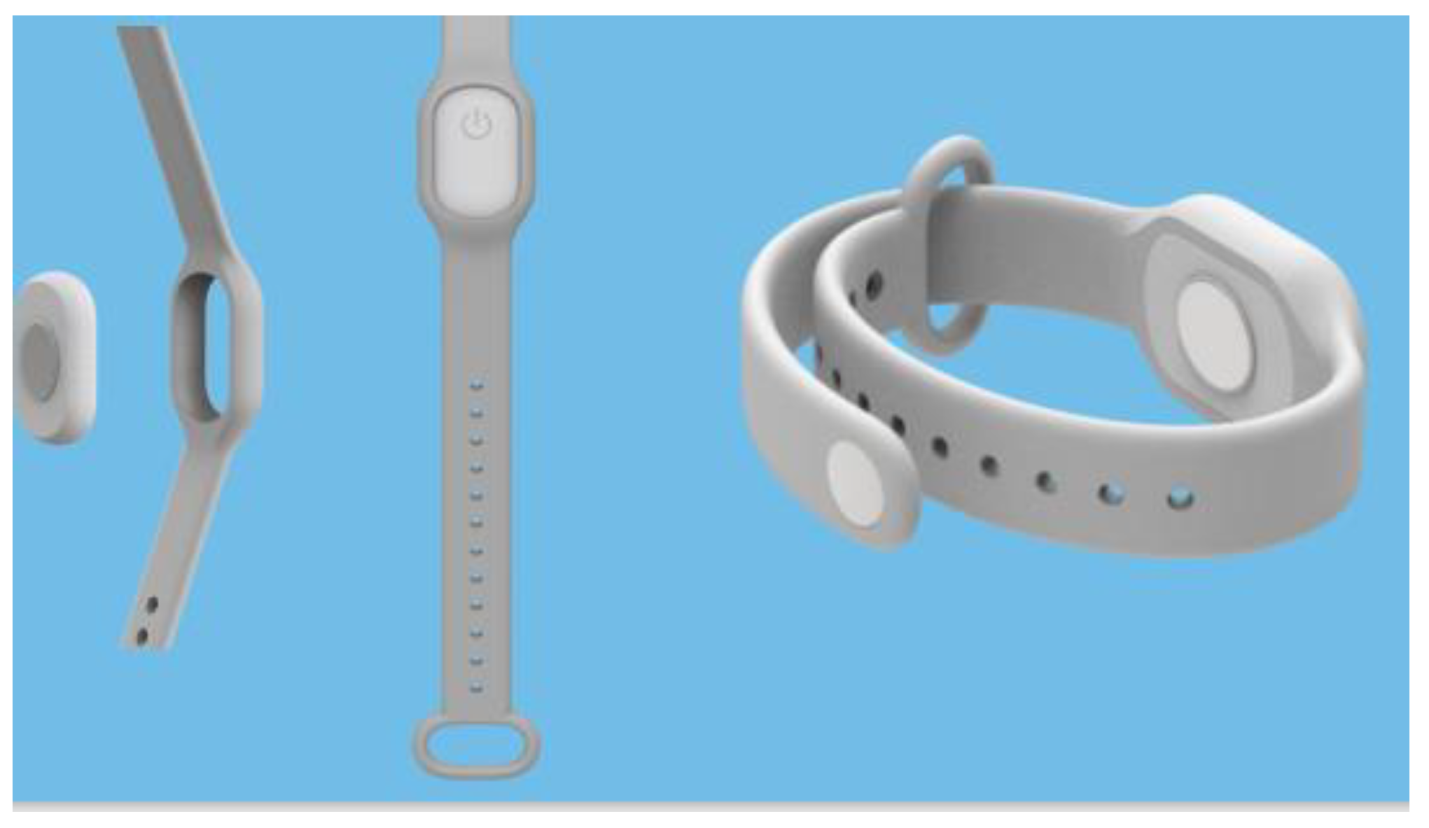
As shown in
Figure 1, the wearable sensor system is a small-size chip with an accuracy of ±0.1 °C, with a detectable range between 32 °C and 43 °C that can be inset into a specific rubber bracelet for continuous and real-time temperature monitoring and data transmission. In detail, the used temperature sensor (model “Jw1656”) falls into the “Bluetooth beacons” category. The latter includes BLE (Bluetooth low energy) class devices that are able to send, at regular intervals, a signal (for instance, hexadecimal values) that can be detected by other devices.
The sensor system presents a communication system and other components that are integrated onboard. In its entirety, the system is composed of a frontend (Dashboard), realized through a Microsoft development environment, and a frontend (server) based on a Linux operating system (v. 8.x) with microservices logic in PHP language 7.x. The frontend permits us to handle and monitor the system. In particular, it is possible to set reference and warning temperature values, as well as alerts (text messages) to recipients; in addition, it is also possible to visualize some statistics related to temperature data acquisitions. In contrast, the backend allows us to store, handle, and process the collected data.
This sensor system chip is waterproof, and it does not provide a display to reduce battery consumption. Moreover, the smartphone app (available for IoS and Android) not only transmits the data but also displays the temperature of all the sensors connected to it.
Figure 2 show an outline of the sensor network in terms of communication architecture and capabilities, together with images of the software interface. The flow of information exchanges can be summarized as follows: the BLE sensor acquires the physical quantity (temperature) and sends the data to a smartphone. The latter, through an internet connection (TCP/IP protocol), transmits the data to the server. In detail, the data exchange between the sensor and smartphone takes place through BLE protocol (Bluetooth “2010” version 4.0). This protocol implements the master/slave principle: the master (i.e., the smartphone in our case) can handle multiple connections at the same time with different slaves (i.e., the temperature sensors), whereas each slave can only be connected to one master at a time. We have also reported more detail about the data structure in
Appendix A.
The smartphone (master) keeps waiting on the channel where the sensors (slaves) send their advertising. Once the data package is received, the smartphone sends it to the server through rest calls in https with Basic Auth. About the data collection, we have chosen MySQL 8.0 (with relational architecture) as a database management system (DBMS).
To obtain a body temperature sensor network that is able to conduct constant and safe monitoring, the developed software is used to analyze the database present on the server, to control the measured temperature, and to produce warnings automatically.
The sensor network is provided with a web interface to view the data stored on the server. In particular, each school can see only the data relative to its students and staff, even if the database is the same for all to allow statistical analysis, etc. It is important to underline that the data collection is regulated by the European General Data Protection Regulation (EU) 2016/679.
More specifically, we are testing this sensor network in three schools: IPSEOA “C. Russo” in Cicciano (Naples), IPSSAR “Di Gennaro” in Vico Equense (Naples), and IS “A. Torrente” in Casoria (Naples).
In each school, in addition to the installation of the app on smartphones and tablets, we installed a monitoring gateway covering the entire school. Moreover, we set up a background service system running in the cloud.
All students and staff members were assigned bracelets. Each wearer is a monitored object and, exploiting the smartphone app, can monitor other people connected in a range of 100 m.
3. Conclusions
We have presented an innovative strategy for continuous and real-time body temperature monitoring using a sensor network based on simple wearable sensors inserted into bracelets. This sensing approach is presently tested in three different schools. It exploits the real-time notification of the monitoring system and allows immediate isolation of the person with abnormal temperature after an alert notification.
Moreover, it could be the first paradigm for monitoring body parameters in a community exploiting a sensor network; in fact, the same sensor network system can be used to measure different parameters of interest for diagnostics and health protection. In this sense, the proposed paradigm is helpful, considering effective and far-reaching “pandemic plans”. Furthermore, this technology could also monitor students’ health looking for congenital pathologies and/or possible infections in progress, simply by using suitable sensors to measure the markers of interest.
Author Contributions
Conceptualization, C.D., A.F. and N.C.; methodology, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; validation, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; formal analysis, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; investigation, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; resources, G.D.R., C.M.N. and S.T.; data curation, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; writing—original draft preparation, C.D., A.F., N.C., G.D.R., C.M.N. and S.T.; writing—review and editing, C.D. and N.C.; supervision, C.D. and N.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data is available on reasonable request from the corresponding author.
Acknowledgments
This work was supported by Ministero dell’Istruzione (Rome, Italy).
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
For the sake of completeness, in this section, we report more information regarding the data structure that the BLE sensor sends to the smartphone. The data format can be expressed as schematically represented in
Figure A1, where four different parts can be distinguished. Please note that, in all parts, all numbers are expressed in hexadecimals.
Figure A1.
Schematization of the BLE sensor data structure.
Figure A1.
Schematization of the BLE sensor data structure.
In particular:
“Part A” is reserved for “Eddystone Protocol”, a specification that defines a BLE message format for proximity beacon messages;
“Part B” deals both with the current temperature value and the time interval with which this physical quantity is acquired;
“Part C” is relative to the history of previous temperature records;
“Part D” is relative to the voltage;
“Part E” is reserved as “AC” and could be used to identify data from multiple data with Bluetooth Eddystone protocol;
“Part F” is the MAC address of the Bluetooth chip in the device.
References
- Pantelopoulos, A.; Bourbakis, N.G. A Survey on Wearable Sensor-Based Systems for Health Monitoring and Prognosis. IEEE Trans. Syst. Man Cybern. Part C (Appl. Rev.) 2010, 40, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Olson, J.S.; Redkar, S. A survey of wearable sensor networks in health and entertainment. MOJ Appl. Bionics Biomech. 2018, 2, 280–287. [Google Scholar] [CrossRef] [Green Version]
- Caldara, M.; Colleoni, C.; Guido, E.; Rosace, G.; Re, V.; Vitali, A. A wearable sensor platform to monitor sweat pH and skin temperature. In Proceedings of the IEEE International Conference on Body Sensor Networks, Cambridge, MA, USA, 6–9 May 2013. [Google Scholar]
- Boano, C.A.; Lasagni, M.; Romer, K.; Lange, T. Accurate Temperature Measurements for Medical Research using Body Sensor Networks. In Proceedings of the 14th IEEE International Symposium on Object/Component/Service-Oriented Real-Time Distributed Computing Workshops, Newport Beach, CA, USA, 28–31 March 2011. [Google Scholar]
- Li, Q.; Zhang, L.N.; Tao, X.M.; Ding, X. Review of flexible temperature sensing networks for wearable physiological monitoring. Adv. Healthc. Mater. 2017, 6, 1601371. [Google Scholar] [CrossRef] [PubMed]
- Mikhaylov, K.; Tervonen, J.; Heikkilä, J.; Känsäkoski, J. Wireless Sensor Networks in industrial environment: Real-life evaluation results. In Proceedings of the 2nd Baltic Congress on Future Internet Communications, Vilnius, Lithuania, 25–27 April 2012; pp. 1–7. [Google Scholar]
- Pérez, C.A.; Jiménez, M.; Soto, F.; Torres, R.; López, J.A.; Iborra, A. A system for monitoring marine environments based on Wireless Sensor Networks. In Proceedings of the OCEANS 2011 IEEE, Santander, Spain, 6–9 June 2011; pp. 1–6. [Google Scholar]
- Low, K.S.; Win, W.N.N.; Er, M.J. Wireless Sensor Networks for Industrial Environments. In Proceedings of the International Conference on Computational Intelligence for Modelling, Control and Automation and International Conference on Intelligent Agents, Web Technologies and Internet Commerce (CIMCA-IAWTIC’06), Vienna, Austria, 28–30 November 2005; pp. 271–276. [Google Scholar]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).