1. Introduction
During the COVID-19 pandemic, the degree of psychological distress has been reported to have reached historically high levels in the US and elsewhere [
1,
2] although the extent to which the pandemic is the cause of the current level of distress is unclear [
2,
3]. Regardless of whether or not the COVID-19 pandemic is the primary cause of the current level of psychological distress, the distress is real, and it has clearly come at a bad time. Although psychological distress appears to motivate people to get vaccinated, it also interferes with mitigation behaviors, particularly social distancing [
4]. It has been hypothesized that this interference occurs because social deprivation is a major cause of the current distress, and behaviors like social distancing and mask wearing may actually increase people’s feelings of social deprivation [
5]. Thus, the more distressed (and socially deprived) a person is, the less likely they are to engage in behaviors that would increase their social deprivation and exacerbate their distress.
This is especially unfortunate because the occurrence of breakthrough infections with COVID-19 in vaccinated and even boosted individuals suggests that it may be a bad time to abandon mitigation efforts such as social distancing, regardless of how aversive those behaviors are. Still, if mitigation behaviors increase distress, people’s decision not to engage in behaviors that increase their distress may have some benefits. It has long been known that psychological distress can impair immune function (e.g., [
6,
7]). Recently, distress was reported to predict the likelihood of hospitalization with SARS-CoV-2 infection [
8], and even more recently, distress levels have been reported to predict post-COVID conditions often known as “long-COVID” [
9,
10].
Previously, we called attention to the public health conundrum posed by the fact that while distress increases the likelihood of vaccination against SARS-CoV-2, it simultaneously decreases the likelihood of mitigation behaviors [
4]. The effects of distress, and social deprivation, in particular, on the function of the immune system only deepen this conundrum, particularly as it affects the public health messaging strategy. Traditional “fear messages” are intended to increase distress while motivating specific health behaviors (e.g., vaccination) that can alleviate that distress. In the present situation, however, increasing distress can clearly have unintended negative health consequences in addition to the intended positive ones. The goal of the present study was to explore the possibility of an alternative, prosocial messaging strategy that could promote effective health behaviors without increasing psychological distress.
Studies suggest that both mitigation and vaccination may be motivated by appeals highlighting their benefits to others [
11,
12,
13]. It is unclear, however, whether this approach works better than appeals to personal benefits [
14], whether it works better for some decisions than others (e.g., decisions regarding vaccination compared with mitigation), and whether it works better for some people than others. Older adults, for example, are well known to be more altruistic than younger adults [
15]. Are they therefore also more likely to have engaged in or to plan actions that decrease the possibility of infection because this also decreases the possibility of infecting others?
The questions addressed by the present study concern pandemic-related distress, specific personality traits consistent with prosocial attitudes and behaviors, and health behaviors recommended by the Centers for Disease Control and Prevention (CDC), such as social distancing and the likelihood of getting vaccinated in the future (e.g., with a “booster”). Previous research on mitigation and vaccination suggests that when it comes to devising a messaging strategy to encourage healthy behaviors during the COVID-19 pandemic, one size will
not fit all [
1,
4,
5]—different demographic groups may be responsive to different messages, and different target behaviors may also be responsive to different messages. Compared to young adults, for example, older adults’ likelihood of social distancing is much less sensitive to their level of psychological distress. Regardless of age, social distancing decreases with the level of distress, whereas more distressed individuals are more likely to report having been vaccinated [
4].
Although our research during the pandemic underscores the important role of distress in health decision-making [
3,
4,
5], such decisions are complex, because distress can have differential implications for how messaging campaigns might need to be designed in order to manage different behaviors. Moreover, distress and pandemic-related stressors may not be the only important motivating factors. Indeed, given our social nature and the importance of social outcomes, it would be surprising if concern for others was not also important in the decision-making process. If true, then future messaging campaigns would have another avenue for motivating appropriate health behaviors and for engaging in broader social outcomes that are important to well-being. Therefore, the present study explored potentially relevant individual and age differences in personality and other psychological factors that might provide a basis for positive, prosocial appeals.
More specifically, the present study assessed a diverse sample of online participants on three facets of the trait of agreeableness (altruism, sympathy, and trust) from the NEO [
16], facets that appear to be directly relevant to healthy behaviors recommended by the CDC. Our working assumption was that individuals who scored highly on a particular personality scale would be more likely to respond positively to appeals consistent with that trait than individuals who scored low on the trait. We hypothesized that those who scored high on altruism and sympathy, for example, would be more responsive to appeals emphasizing a particular behavior’s potential benefits to others than those who scored low on these scales.
We tested our hypothesis by examining the association between individuals’ altruism, sympathy, and trust scores with their vaccination intentions, because the decreased likelihood of getting infected following vaccination necessarily results in a decreased likelihood that one would be infectious—a clear benefit to others. An issue was whether individuals with higher altruism and sympathy scores would report that they were more likely to get vaccinated (or boosted) against the shot. Following the same logic, would they also be more likely to engage in mitigation behaviors because, like vaccination, mitigation behaviors also decrease the likelihood of becoming infectious, thereby benefiting others? Additionally, do individuals with higher trust scores report that they are more likely to get a booster shot, consistent with their having greater trust in claims by doctors and others regarding the efficacy of COVID vaccines?
To address these questions, the present study gathered evidence concerning the relations among personality scores and pandemic-related attitudes and behaviors, evidence that we believe is consistent with the relevance of prosocial personality traits and the potential power of prosocial messaging. Thus, this study broadens the scope of our past work [
3,
4,
5] by investigating personality variables specific to trust and concern for others, while also replicating our previous work on distress, to provide a fuller picture of what might motivate people to engage in recommended behaviors during the pandemic and in the post-COVID period.
4. Discussion
The present study had two major goals: first, to assess the replicability of the association of psychological distress with mitigation and vaccination that led to formulation of the differential distress hypothesis [
4], and second, to examine the association of specific personality traits with mitigation and vaccination decisions. With respect to the first goal, it should be noted that our initial findings regarding mitigation were based on data collected in April 2020, at the very beginning of the COVID-19 pandemic [
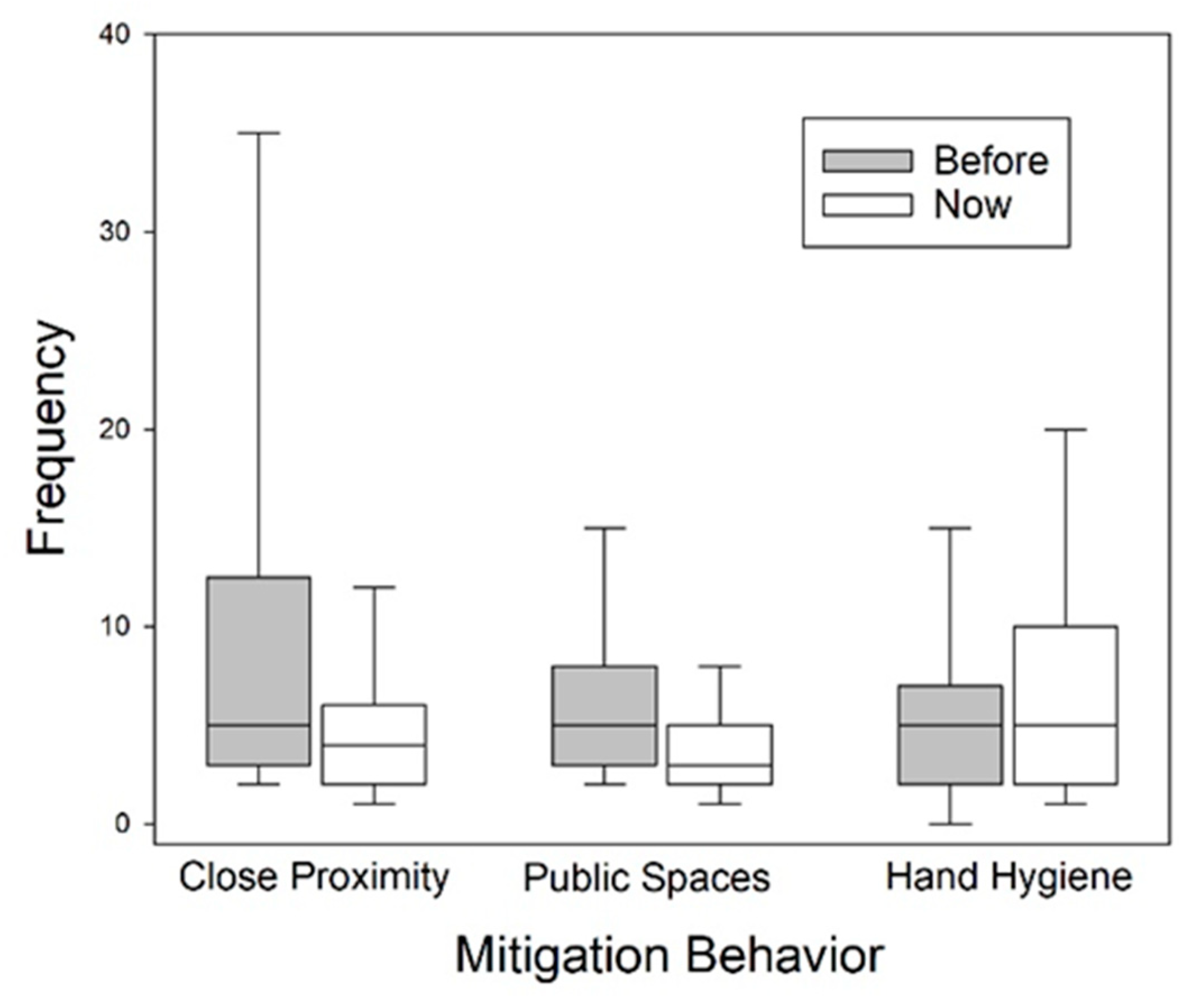
5]. In the present sample, surveyed nearly two years later, the majority of the participants were engaged in social distancing. In fact, the percentage (67.3%) of those in the sample who reported they had decreased the frequency of their close proximity interactions with nonhousehold members since before the pandemic was very similar to the corresponding percentage (61.0%) of the sample studied more than two years before. Moreover, not only was the overall level of psychological distress in the present study similar to that measured in the two previous studies, but so were the levels of the two components of distress measure. For example, the mean anxiety and depression scores on the HADS for participants in the present sample were 8.97 and 6.63; the corresponding means for the initial sample were 8.03 and 6.33. The stability of these measures is a positive sign suggesting that online surveys such as that used in the present study potentially provide reliable information concerning psychological phenomena in a continuously changing pandemic environment.
4.1. Mitigation
The differential distress hypothesis specifically predicts that social distancing will decrease with the level of psychological distress. The negative association between the level of distress and social distancing, initially observed in 2020 [
5] and first replicated in a follow-up study conducted a year later [
4], was replicated again in the present study. More specifically, not only were decreases in the frequency of close proximity interactions with nonhousehold members significantly associated with the level of psychological distress, as shown in both of the previous studies in this series (i.e., [
4,
5]), but as predicted by the differential distress hypothesis, so too were decreases in the frequency of visits to enclosed public spaces, another social distancing behavior.
As Myerson et al. [
4] pointed out, the observed negative association of psychological distress with mitigation behaviors poses potential problems for the use of traditional fear appeals to promote mitigation behaviors. Such messages typically highlight current stressors (e.g., social deprivation and risks of infection in the present situation) and indicate that specific health behaviors could change the situation. According to the differential distress hypothesis, there are two problems with this approach. First, the messages call attention to current stressors, and while this may have some positive effects (e.g., increasing the likelihood of vaccination), it may simultaneously have serious negative effects (e.g., decreasing mitigation behaviors like social distancing). This might not be a problem if, for example, vaccines are always completely effective, but they are not (e.g., breakthrough infections), and the deliberately increased distress may interfere with the very mitigation behaviors that could decrease the likelihood of subsequent infections. Second, as Myerson et al. found, older adults are not only less sensitive to pandemic stressors, but even when their distress levels were high, their vaccination decisions are much less affected than those of younger adults with equivalent levels of distress [
4].
The use of prosocial health messages could represent an alternative approach that, in contrast, would build specifically on the strengths of older adults. This is because it could appeal to people’s altruism and sympathy for others, both of which increase significantly with age and are obviously relevant to people’s mitigation and vaccination decisions. (trust increases significantly with age as well, but to a lesser degree.)
When compassion and trust were both included in logistic regression models of social distancing behaviors along with age and distress, compassion was a significant predictor, but age, distress, and trust were not. Notably, when political preferences, as reflected in participants’ votes in the 2020 presidential election, were added to a model that also included age, distress, compassion, and trust (e.g., as independent variables, such preferences were not significant. This finding may have important implications because, as discussed in the following section, it is one of several significant differences between the present results for mitigation and vaccination, suggesting that different factors are involved in mitigation and vaccination decisions. The results for compassion and mitigation may be especially important because they are directly relevant to the problem of determining how to motivate mitigation behaviors such as social distancing without distressing the recipients of public health messages that are intended to motivate such behaviors, as other findings indicate that increased distress in such cases would be counterproductive.
4.2. Vaccination Intentions
Linear regression models designed to test the differential distress hypothesis and assess whether compassion scores predicted vaccination intentions, as was the case with mitigation behaviors in the present study, accounted for less than one percent of the variance and failed to reach significance in both cases. A model that added trust to the independent variables was significant, however, and a model that added voter preference in the 2020 election to the potential predictors of vaccination intentions was not only significant, it more than tripled the variance accounted for in vaccination intentions (R2 = 0.146). Further analysis identified beliefs about the safety and efficacy of current vaccines as the single best predictor of intentions. This measure (Vacc) alone accounted for 34.2% of the variance in vaccination intentions. When Vacc, trust, and voter preference in 2020 were all used as independent variables in a regression model predicting vaccination intentions, all three independent variables were significant.
These findings are consistent with the politicization of vaccination. For example, Biden and Trump voters, perhaps not surprisingly, differed significantly not only in their beliefs in vaccine safety and efficacy but also in their vaccination intentions. In contrast, they did not differ in their levels of psychological distress or trust, although it should be noted that the trust facet of agreeableness measures trust in other people and not in institutions, either in general or specifically, so, for example, it does not apply to trust in science or medicine or the public health system itself.
Taken together these findings suggest that although it is possible that the assumptions of the differential distress hypothesis are correct with respect to psychological distress and vaccination, the role of distress as a predictor may be overwhelmed by the effects of variation in political attitudes, beliefs, and preferences. The same does not seem to be true for individual differences in trust, which appear to vary independently of people’s politics. Notably, trust does appear to play a role in vaccination decisions and in people’s evaluation of present vaccines themselves and even makes similar contributions to the vaccination intentions of Trump and Biden supporters, despite the fact that, on average, their intentions differ markedly.
While information regarding individual differences in vaccination intentions that is more directly applicable to public health messaging will obviously require further research, it seems clear that the differential distress hypothesis is correct about one thing: vaccination and mitigation decisions are affected by different factors. While the hypothesis focused on the differential effects of psychological distress, the present results suggest that there are other variables that can play more prominent roles. These include several aspects of personality traits as well as political preferences and attitudes. With respect to aspects of personality, the present results reveal the importance of individual differences in trust in other people in determining the vaccination intentions of the present sample, regardless of their political inclinations, whereas mitigation behaviors appear to be independent of trust in other people but are significantly affected by differences in compassion (i.e., one’s altruism and sympathy for others). Further, political preferences currently appear to play a major role in one’s vaccination intentions, whereas they do not contribute significantly to mitigation behaviors (e.g., social distancing).
4.3. Implications
What are the implications of the present findings for public health messaging? First, and most obviously, they argue against a one-size-fits-all approach, and more specifically, are in favor of approaching the issues of mitigation and vaccination differently. The present results are consistent with previous studies (e.g., [
4,
5]) in showing that distress may interfere with social distancing, implying that fear messages must be handled with care, but that is an example of what not to do, or what needs, at least, to be approached carefully. The present exploration of the role of individual differences in personality attributes was, of course, motivated by a search for an alternative approach.
With respect to mitigation, the important role that appears to be played by compassion does not just mean that prosocial appeals may be a good fit for altruistic and sympathetic or empathetic people and that messaging should consider market segmentation approaches to communication. In addition, it should be noted that, while altruism is a propensity for a certain kind of behavior, those with a lower propensity may also be motivated by prosocial appeals. Altruistic appeals for donations, for example, are successful with all kinds of people although, consistent with the age differences observed here, they may be more successful with older adults, who appear to be more compassionate than younger adults (for a meta-analytic review, see [
15]). Interestingly, stress may actually increase altruism in younger adults, although not in older adults, perhaps because older adults are less affected by stress [
3]. Nevertheless, older adults are more altruistic under both stressed and unstressed conditions [
20], suggesting that prosocial appeals may be especially effective with them.
We note in passing that, although we focused on age largely because of older adults’ special vulnerability to COVID-19, and neither income nor education appeared to play significant roles, other demographic groups may also be especially at risk, and further studies targeting such groups is clearly needed. While older adults, fortunately, tend to be less sensitive to pandemic and other stressors, females, for example, appear to be especially sensitive [
2,
3], which is another factor that perhaps probably should be taken into account in public health messaging.
With respect to vaccination intentions, the present results suggest that while political inclinations can play a major role, the importance of individual differences in trust may present significant opportunities. Indeed, reliance on messengers already trusted in the community is now recognized as very important [
21]. Indeed, while the present results showed that, not unexpectedly, beliefs about the safety and efficacy of vaccines play a critical role, the results also suggest that individual differences in trust are important in the formation of those beliefs. Indeed, the corresponding variables trust and Vacc are strongly correlated (
r = 0.585), suggesting that trust also plays a critical role in determining those beliefs. Importantly, it appears to have played a similar role in modulating participants’ intentions independently of their political views.
One of the biggest challenges for public health messaging in the immediate future may be that it has become increasingly clear how much lower the risk of serious consequences from SARS-CoV-2 infection is for younger and middle-aged adults compared to that for older adults. Indeed, the CDC website notes that the rate of hospitalization for those 65–74 is 4.9 times that of young adults (18–29 years), increasing to 8.9 times the young adult rate for those aged 75–84 years. The age differences in the rate of deaths from COVID-19 are even starker: 60 and 140 times the young adult rate for those aged 65–74 and 75–84 years, respectively [
22], which may suggest to younger adults that only the elderly and those with compromised immune systems really need to maintain their mitigation behaviors. Perhaps exacerbating the problem, public health policies and messaging both have begun emphasizing the importance of everyone evaluating the risks to themselves personally. Unfortunately, this may lead those at high risk, whose safety continues to rely heavily on the precautions taken by others, to believe, perhaps correctly, that the system is beginning to abandon them.
Although new medications (e.g., Paxlovid) and treatment approaches may help, of course, the asymmetry of the problem remains. More specifically, this asymmetry creates what may be termed an altruistic paradox in that, paradoxically, those for whom prosocial, altruistic appeals would seem to be ethically most appropriate (i.e., those at relatively lower risk, such as younger adults) are those whom the present findings suggest may be least responsive to such appeals. This is because compassion appears to be lowest in younger adults and highest in older adults, who should be most motivated by personal concerns. This is the challenge. Although younger adults also appear to be lower in trust than older adults, the age difference is relatively small, which suggests that it will be especially important to use people already trusted by younger adults to communicate the need for them to “play it safe,” acknowledging that it is others who are the most likely to benefit. In other words, what may be required is not just communicating, but also leading. The challenge for public health messaging will be to motivate younger adults to take the consequences of their mitigation decisions for others into account.