A Review of Environmental Factors for an Ontology-Based Risk Analysis for Pandemic Spread
Abstract
:- The Susceptible-Exposed-Infected-Recovered (SEIR) models are widely used to predict possible contagion scenarios. It uses individuals’ contagion statuses, such as not yet infected, incubation period, confirmed cases, and recovered or dead cases to build the pandemic spread model.
- Pandemic spreading, however, depends on how the environmental factors influencing human behaviors of pandemic prevention. It is not a linear problem but is a multi-dimensional and non-linear problem.
- This research, therefore, identified the major environmental factors from literatures, including fear of the spread of the pandemic, attitudes toward hygiene practices, community culture, government policies on pandemic prevention, economic activity restrictions, pandemic education, multimedia, and technologies uses for information dissemination and disclosure, resulting in an increase in the spread of the pandemic.
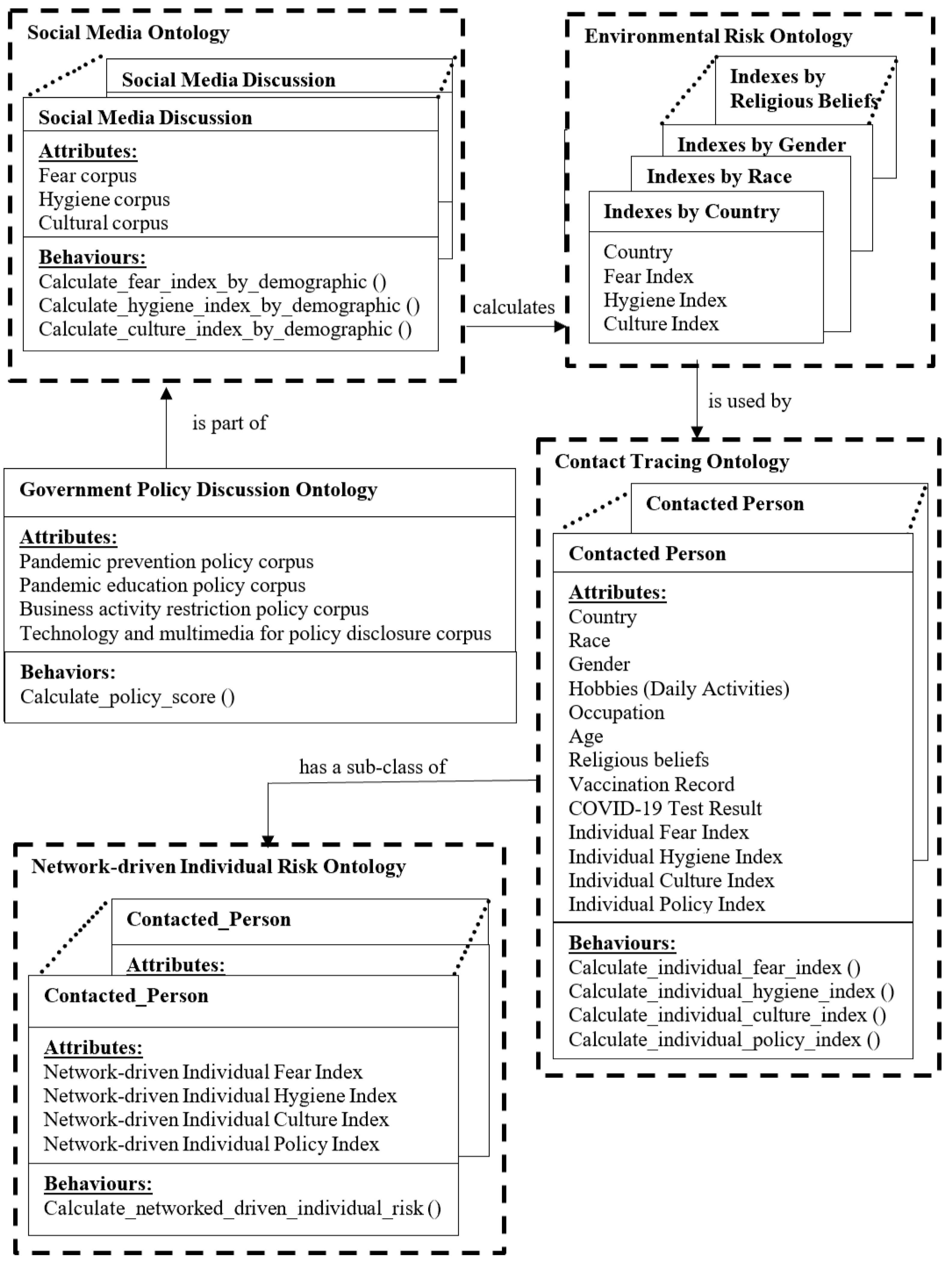
- The design of ontology-based big data architecture uses ontologies, sentiment analyses, a clustered 3D CNN model, and a clustered GCN model to model the environmental factors into different dimensions and uses the 3D-CNN/GCN architecture to model the contagion scenarios for spread prediction.
- The conceptual design of the big data information architecture allows researchers to continue our work to conduct the sentiment analyses of the government policies and use the 3D-CNN/GCN architecture to model the complex contagion scenarios for predicting individual or community’s pandemic spreading risk that no researchers have done before.
1. Introduction
2. Literature Review
3. Research Methods
4. Results
5. Discussion
5.1. Fear of the Pandemic Spreading
5.2. Hygiene Practices and Pandemic Transmission
5.3. Cultural Behavior of Pandemic Prevention
5.4. Attitude of Government Policies on Pandemic Prevention
5.5. Economic and Business Restrictions
5.6. Pandemic Prevention Education Programs
5.7. Technology Infrastructure and Multimedia for Information Disclosure
6. Recommendations
- First, contact-tracing data, social media data, pandemic prevention methods, government policies for pandemic prevention, educational programs, business activity restrictions, multimedia, and technology infrastructure were collected. The contact-tracing data were modeled using an ontology. The ontology defines the attributes and behaviors of entries [111,112].
- Second, the discussion topics on social media were classified into pandemic fear, hygiene measures, cultural practices, prevention policy, education programs, business activity restriction, multimedia disclosure, and technology infrastructure for sentiment analysis. Commonly used topic classification methods include Naïve Bayes, support vector machine model, and linear discriminant analysis.
- The keywords of the posts for each topic were extracted to measure the pandemic indices of fear, hygiene, culture, and policy in the next step [79,113]. Natural language processing, word frequency count, term frequency-inverse document frequency [114], and n-gram [115] are commonly used text analysis methods for keyword extraction.
- Categorical and dimensional methods are the two major sentiment-analysis methods [116,117]. The categorical method classifies sentiments into different fear descriptors, such as sadness, nervousness, and worry [116,117]. The dimensional method classifies sentiments into positive and negative affectivity [117,118,119]. The extracted keywords and phrases were mapped to the vocabularies of categorical and dimensional databases. The classified sentiments were counted and used to calculate fear, hygiene, culture, and policy indices. Some artificial intelligence methods such as the support vector machine model, word2vec, TextCNN, and 2D CNN methods can be used together with sentiment counts to predict sentiments [120,121,122,123,124].
- After the sentiments were analyzed, a clustered ontology model was constructed to capture the four indices’ values per demographic group to predict the individuals’ pandemic spreading risk based on their demographic information. The contact-tracing information of contact activity, time, location, duration, and contact person can be used to predict the network-driven individual pandemic spread risk based on the connected nodes in the network. The community outbreak risk in the contact network was calculated. The 3D CNN network analysis model and graph convolutional network [125] can be used to train and predict individual risks and network-driven individual risks using the COVID-19 test history and the COVID-19 test result, respectively. Policymakers can use this information to plan pandemic prevention programs.
7. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Contact Tracing. 19 October 2021. Available online: https://www.cdc.gov/coronapandemic/2019-ncov/daily-life-coping/contact-tracing.html (accessed on 22 January 2023).
- Munzert, S.; Selb, P.; Gohdes, A.; Stoetzer, L.F.; Lowe, W. Tracking and promoting the usage of a COVID-19 contact tracing app. Nat. Hum. Behav. 2021, 5, 247–255. [Google Scholar] [CrossRef]
- World Health Organization. Contact Tracing in the Context of COVID-19. Surveillance, Case Investigation and Epidemiological Protocols. 2021. Available online: https://www.who.int/publications/i/item/contact-tracing-in-the-context-of-covid-19 (accessed on 22 January 2023).
- Maheshwari, P.; Albert, R. Network model and analysis of the spread of COVID-19 with social distancing. Appl. Netw. Sci. 2020, 5, 100. Available online: https://appliednetsci.springeropen.com/articles/10.1007/s41109-020-00344-5 (accessed on 22 January 2023). [CrossRef]
- Melegaro, A.; Jit, M.; Gay, N.; Zagheni, E.; Edmunds, W.J. What types of contacts are important for the spread of infections? Using contact survey data to explore European mixing patterns. Pandemics 2011, 3, 143–151. [Google Scholar] [CrossRef]
- Scherr, T.F.; DeSousa, J.M.; Moore, C.P.; Hardcastle, A.; Wright, D.W. App Use and Usability of a Barcode-Based Digital Platform to Augment COVID-19 Contact Tracing: Postpilot Survey and Paradata Analysis. JMIR Public Health Surveill. 2021, 7, e25859. [Google Scholar] [CrossRef]
- Shahroz, M.; Ahmad, F.; Younis, M.S.; Ahmad, N.; Boulos, M.N.K.; Vinuesa, R.; Qadire, J. COVID-19 digital contact tracing applications and techniques: A review post initial deployments. Transp. Eng. 2021, 5, e100072. [Google Scholar] [CrossRef]
- Kong, J.D.; Tekwa, E.W.; Gignoux-Wolfsohn, S.A. Social, economic, and environmental factors influencing the basic reproduction number of COVID-19 across countries. PLoS ONE 2021, 16, e0252373. [Google Scholar] [CrossRef]
- Laires, P.A.; Dias, S.; Gama, A.; Moniz, M.; Pedro, A.R.; Soares, P.; Aguiar, P.; Nunes, C. The Association Between Chronic Disease and Serious COVID-19 Outcomes and Its Influence on Risk Perception: Survey Study and Database Analysis. JMIR Public Health Surveill. 2021, 7, e22794. [Google Scholar] [CrossRef]
- Bruns, D.P.; Kraguljac, N.V.; Bruns, T.R. COVID-19: Facts, Cultural Considerations, and Risk of Stigmatization. J. Transcult. Nurs. 2020, 31, 326–332. [Google Scholar] [CrossRef]
- Zhang, N.; Shi, T.; Zhong, H.; Guo, Y. COVID-19 Prevention and Control Public Health Strategies in Shanghai, China. J. Public Health Manag. Pract. 2020, 26, 334–344. [Google Scholar] [CrossRef]
- Zhang, X.; Luo, W.; Zhu, J. Top-Down and Bottom-Up Lockdown: Evidence from COVID-19 Prevention and Control in China. J. Chin. Political Sci. 2021, 26, 189–211. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.T.; Kanji, R.; Wang, A.H.; Mamuji, A.; Rozdilsky, J.; Chu, T. Cultural contexts during a pandemic: A qualitative description of cultural factors that shape protective behaviours in the Chinese-Canadian community. BMC Public Health 2021, 21, 1897. [Google Scholar] [CrossRef]
- Ting, R.S.K.; Yong, Y.Y.A.; Tan, M.M.; Yap, C.K. Cultural Responses to COVID-19 Pandemic: Religions, Illness Perception, and Perceived Stress. Front. Psychol. 2021, 12, e634863. [Google Scholar] [CrossRef] [PubMed]
- Rivas, D.R.C.; Jaldin, M.L.L.; Canaviri, B.N.; Escalante, L.F.P.; Fernández, A.M.C.A.; Ticona, J.P.A. Social media exposure, risk perception, preventive behaviors and attitudes during the COVID-19 pandemic in La Paz, Bolivia: A cross sectional study. PLoS ONE 2021, 16, e0245859. [Google Scholar] [CrossRef]
- Hassounah, M.; Raheel, H.; Alhefzi, M. Digital Response During the COVID-19 Pandemic in Saudi Arabia. J. Med. Internet Res. 2020, 22, e19338. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Folarin, A.A.; Ranjan, Y.; Rashid, Z.; Conde, P.; Stewart, C.; Cummins, N.; Matcham, F.; Costa, G.D.; Simblett, S.; et al. Using Smartphones and Wearable Devices to Monitor Behavioral Changes During COVID-19. J. Med. Internet Res. 2020, 22, e19992. [Google Scholar] [CrossRef]
- Budd, J.; Miller, B.S.; Manning, E.M.; Lampos, V.; Zhuang, M.; Edelstein, E.; Rees, G.; Emery, V.C.; Stevens, M.M.; Keegan, N.; et al. Digital technologies in the public-health response to COVID-19. Nat. Med. 2020, 26, 1183–1192. [Google Scholar] [CrossRef]
- Altundag, Y.; Altundag, S. Examining the Relationship between the Fear of COVID-19, Resilience and Religion. Int. J. Psychol. Educ. Stud. 2021, 8, 180–192. [Google Scholar] [CrossRef]
- Brailovskaia, J.; Stirnberg, J.; Rozgonjuk, D.; Margraf, J.; Elhai, J.D. From low sense of control to problematic smartphone use severity during COVID-19 outbreak: The mediating role of fear of missing out and the moderating role of repetitive negative thinking. PLoS ONE 2021, 16, e0261023. [Google Scholar] [CrossRef] [PubMed]
- Brennan, M.E.; Marinovich, M.L.; Verdonk, B.; Vukasovic, M.; Coggins, A. Symptoms of anxiety, depression and fear in healthcare workers and non-healthcare workers undergoing outpatient COVID-19 testing in an urban Australian setting. Aust. J. Prim. Health 2021, 27, 442–449. [Google Scholar] [CrossRef]
- Brubaker, J.; Kilic, T.; Wollburg, P. Representativeness of individual-level data in COVID-19 phone surveys: Findings from Sub-Saharan Africa. PLoS ONE 2021, 16, e0258877. [Google Scholar] [CrossRef]
- Duong, H.T.; Massey, Z.B.; Churchill, V.; Popova, L. Are smokers scared by COVID-19 risk? How fear and comparative optimism influence smokers’ intentions to take measures to quit smoking. PLoS ONE 2021, 16, e0260478. [Google Scholar] [CrossRef]
- Hardy, L.J.; Mana, A.; Mundell, L.; Neuman, M.; Benheim, S.; Otenyo, E. Who is to blame for COVID-19? Examining politicized fear and health behavior through a mixed methods study in the United States. PLoS ONE 2021, 16, e0256136. [Google Scholar] [CrossRef]
- Huang, F.; Ding, H.; Liu, Z.; Wu, P.; Zhu, M.; Li, A.; Zhu, T. How fear and collectivism influence public’s preventive intention towards COVID-19 infection: A study based on big data from the social media. BMC Public Health 2020, 20, 1707. [Google Scholar] [CrossRef]
- Okan, N. Investigating the Moderator Effect of Fear of COVID-19 in the Relation between Communication Anxiety and Self-Efficacy. Educ. Process Int. J. 2021, 10, 62–77. [Google Scholar] [CrossRef]
- Stockman, J.K.; Wood, B.A.; Anderson, K.M. Racial and Ethnic Differences in COVID-19 Outcomes, Stressors, Fear, and Prevention Behaviors Among US Women: Web-Based Cross-sectional Study. J. Med. Internet Res. 2021, 23, e26296. [Google Scholar] [CrossRef]
- Sugawara, D.; Gu, Y.; Masuyama, A.; Ng, S.L.; Phoo, E.Y.M.; Raja, R.S.R.; Kubo, T.; Chishima, Y.; Tee, E.Y.J. RE-COVER project: A survey on resilience, mental health, and fear of COVID-19 in four countries. BMC Res. Notes 2021, 14, 409. [Google Scholar] [CrossRef]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef]
- Zarrouq, B.; Abbas, N.; Hilaly, J.E.; Asri, A.E.; Abbouyi, S.; Omari, M.; Malki, H.; Bouazza, S.; Moutawakkil, S.G.; Halim, K.; et al. An investigation of the association between religious coping, fatigue, anxiety and depressive symptoms during the COVID-19 pandemic in Morocco: A web-based cross-sectional survey. BMC Psychiatry 2021, 21, 264. [Google Scholar] [CrossRef]
- Barrett, C.; Cheung, K.L. Knowledge, socio-cognitive perceptions and the practice of hand hygiene and social distancing during the COVID-19 pandemic: A cross-sectional study of UK university students. BMC Public Health 2021, 21, 426. [Google Scholar] [CrossRef] [PubMed]
- Dwivedi, H.; Paul, N.; Banerjee, K.L.; Singh, S.; Jain, R.; Kumar, S. Denture hygiene awareness, attitude and practice among complete denture wearers during COVID-19 lockdown Pandemic: A questionnaire-based survey. J. Pharm. Bioallied Sci. 2021, 13, 1119–1123. [Google Scholar] [CrossRef]
- Manghisi, V.M.; Fiorentino, M.; Boccaccio, A.; Gattullo, M.; Cascella, G.L.; Toschi, N.; Pietroiusti, A.; Uva, A.E. A Body Tracking-Based Low-Cost Solution for Monitoring Workers’ Hygiene Best Practices during Pandemics. Sensors 2000, 20, 6149. [Google Scholar] [CrossRef]
- Natnael, T.; Adane, M.; Alemnew, Y.; Andualem, A.; Hailu, F. COVID-19 knowledge, attitude and frequent hand hygiene practices among taxi drivers and associated factors in urban areas of Ethiopia. PLoS ONE 2021, 16, e0253452. [Google Scholar] [CrossRef]
- Veys, K.; Dockx, K.; Van Remoortel, H.; Vandekerckhove, P.; De Buck, E. The effect of hand hygiene promotion programs during epidemics and pandemics of respiratory droplet-transmissible infections on health outcomes: A rapid systematic review. BMC Public Health 2021, 21, 1745. [Google Scholar] [CrossRef]
- Von Wyl, V. Challenges for Nontechnical Implementation of Digital Proximity Tracing During the COVID-19 Pandemic: Media Analysis of the SwissCovid App. JMIR mHealth uHealth 2021, 9, e25345. [Google Scholar] [CrossRef]
- Bearth, A.; Berthold, A.; Siegrist, M. People’s perceptions of, willingness-to-take preventive remedies and their willingness-to-vaccinate during times of heightened health threats. PLoS ONE 2022, 17, e0263351. [Google Scholar] [CrossRef]
- Bekele, D.; Tolossa, T.; Tsegaye, R.; Teshome, W. The knowledge and practice towards COVID-19 pandemic prevention among residents of Ethiopia. An online cross-sectional study. PLoS ONE 2021, 16, e0234585. [Google Scholar] [CrossRef]
- Bor, R.; Szántó, K.J.; Fábián, A.; Farkas, K.; Szűcs, M.; Rutka, M.; Tóth, T.; Bálint, A.; Milassin, Á.; Dubravcsik, Z.; et al. Effect of COVID-19 pandemic on workflows and infection prevention strategies of endoscopy units in Hungary: A cross-sectional survey. BMC Gastroenterol. 2021, 21, 98. [Google Scholar] [CrossRef]
- Kozyreva, A.; Lorenz-Spreen, P.; Lewandowsky, S.; Garrett, P.M.; Herzog, S.M.; Pachur, T.; Hertwig, R. Psychological factors shaping public responses to COVID-19 digital contact tracing technologies in Germany. Sci. Rep. 2021, 11, e18716. [Google Scholar] [CrossRef]
- Ladiwala, Z.F.; Dhillon, R.A.; Zahid, I.; Irfan, O.; Khan, M.S.; Awan, S.; Khan, J.A. Knowledge, attitude and perception of Pakistanis towards COVID-19; a large cross-sectional survey. BMC Public Health 2021, 21, 21. [Google Scholar] [CrossRef] [PubMed]
- Lewandowsky, S.; Dennis, S.; Perfors, A.; Kashima, Y.; White, J.P.; Garrett, P.; Little, D.R.; Yesilada, M. Public acceptance of privacy-encroaching policies to address the COVID-19 pandemic in the United Kingdom. PLoS ONE 2021, 16, e0245740. [Google Scholar] [CrossRef] [PubMed]
- Maytin, L.; Maytin, J.; Agarwal, P.; Krenitsky, A.; Krenitsky, J.; Epstein, R.S. Attitudes and Perceptions Toward COVID-19 Digital Surveillance: Survey of Young Adults in the United States. JMIR Form. Res. 2021, 5, e23000. [Google Scholar] [CrossRef]
- McCarthy, H.; Potts, H.W.W.; Fisher, A. Physical Activity Behavior Before, During, and After COVID-19 Restrictions: Longitudinal Smartphone-Tracking Study of Adults in the United Kingdom. J. Med. Internet Res. 2021, 23, e23701. [Google Scholar] [CrossRef]
- Narayanan, R.P.; Nordlund, J.; Pace, R.K.; Ratnadiwakara, D. Demographic, jurisdictional, and spatial effects on social distancing in the United States during the COVID-19 pandemic. PLoS ONE 2020, 15, e0239572. [Google Scholar] [CrossRef]
- Chung, H.W.; Apio, C.; Goo, T.; Heo, G.; Han, K.; Kim, T.; Kim, H.; Ko, Y.; Lee, D.; Lim, J.; et al. Effects of government policies on the spread of COVID-19 worldwide. Sci. Rep. 2021, 11, 20495. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.É.; Howard, M.E.; Robbins, R.; Barger, L.K.; Facer-Childs, E.R.; Rajaratnam, S.M.W.; Czeisler, C.A. Early public adherence with and support for stay-at-home COVID-19 mitigation strategies despite adverse life impact: A transnational cross-sectional survey study in the United States and Australia. BMC Public Health 2021, 21, 503. [Google Scholar] [CrossRef]
- Cohen, K.; Leshem, A. Suppressing the impact of the COVID-19 pandemic using controlled testing and isolation. Sci. Rep. 2021, 11, 6279. [Google Scholar] [CrossRef]
- Dong, C.; Tian, Y.; Xu, W.; He, J.; Chen, D.; Zhu, J.; Lu, P. Introduction on collective quarantine of close contacts of patients with COVID-19 for medical observation in China: From the perspective of frontline staff. Biosci. Trends 2020, 14, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Dörr, J.O.; Kinne, J.; Lenz, D.; Licht, G.; Winker, P. An integrated data framework for policy guidance during the coronavirus pandemic: Towards real-time decision support for economic policymakers. PLoS ONE 2022, 17, e0263898. [Google Scholar] [CrossRef]
- Ebrahim, S.; Ashworth, H.; Noah, C.; Kadambi, A.; Toumi, A.; Chhatwal, J. Reduction of COVID-19 Incidence and Nonpharmacologic Interventions: Analysis Using a US County-Level Policy Data Set. J. Med. Internet Res. 2020, 22, e24614. [Google Scholar] [CrossRef] [PubMed]
- Fosco, C.; Zurita, F. Assessing the short-run effects of lockdown policies on economic activity, with an application to the Santiago Metropolitan Region, Chile. PLoS ONE 2021, 16, e0252938. [Google Scholar] [CrossRef]
- Gonçalves, B.; Mendes, R.; Folgado, H.; Figueiredo, P.; Travassos, B.; Barros, H.; Beckert, P.; Brito, J. Can Tracking Data Help in Assessing Interpersonal Contact Exposure in Team Sports during the COVID-19 Pandemic? Sensors 2020, 20, 6163. [Google Scholar] [CrossRef]
- Heimes, D.; Müller, L.K.; Schellin, A.; Naujokat, H.; Graetz, C.; Schwendicke, F.; Goedecke, M.; Beck-Broichsitter, B.; Kämmerer, P.W. Consequences of the COVID-19 Pandemic and Governmental Containment Policies on the Detection and Therapy of Oral Malignant Lesions-A Retrospective, Multicenter Cohort Study from Germany. Cancers 2021, 13, 2892. [Google Scholar] [CrossRef]
- Hendrix, M.J.; Walde, C.; Findley, K.; Trotman, R. Absence of Apparent Transmission of SARS-CoV-2 from Two Stylists After Exposure at a Hair Salon with a Universal Face Covering Policy. Morb. Mortal. Wkly. Rep. 2020, 69, 930–932. [Google Scholar] [CrossRef]
- Jarvis, C.I.; Van Zandvoort, K.; Gimma, A.; Prem, K.; Klepac, P.; Rubin, G.J.; Edmunds, W.J. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020, 18, 124. [Google Scholar] [CrossRef]
- Jiao, J.; Shi, L.; Zhang, Y.; Chen, H.; Wang, X.; Yang, M.; Yang, J.; Liu, M.; Sun, G. Core policies disparity response to COVID-19 among BRICS countries. Int. J. Equity Health 2022, 21, 9. [Google Scholar] [CrossRef]
- Knaul, F.; Arreola-Ornelas, H.; Porteny, T.; Touchton, M.; Sánchez-Talanquer, M.; Méndez, Ó.; Chertorivski, S.; Ortega, S.; Chudnovsky, M.; Kuri, P. Not far enough: Public health policies to combat COVID-19 in Mexico’s states. PLoS ONE 2021, 16, e0251722. [Google Scholar] [CrossRef]
- Lo, S.N.; Skarbek, A.; Capon, A. Recovery from the pandemic: Evidence-based public policy to safeguard health. Med. J. Aust. 2020, 213, 284. [Google Scholar] [CrossRef]
- Lu, G.; Razum, O.; Jahn, A.; Zhang, Y.; Sutton, B.; Sridhar, D.; Ariyoshi, K.; von Seidlein, L.; Müller, O. COVID-19 in Germany and China: Mitigation versus elimination strategy. Glob. Health Action 2021, 14, e1875601. [Google Scholar] [CrossRef]
- Luo, M.; Liu, Q.; Wang, J.; Gong, Z. From SARS to the Omicron variant of COVID-19: China’s policy adjustments and changes to prevent and control infectious diseases. Biosci. Trends 2022, 15, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Mack, C.D.; Wasserman, E.B.; Perrine, C.G.; MacNeil, A.; Anderson, D.J.; Myers, E.; Smith, S.; McDonald, L.C.; Osterholm, M.; Solomon, G.S.; et al. Implementation and Evolution of Mitigation Measures, Testing, and Contact Tracing in the National Football League. Morb. Mortal. Wkly. Rep. 2020, 70, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Pillonetto, G.; Bisiacco, M.; Palù, G.; Cobelli, C. Tracking the time course of reproduction number and lockdown’s effect on human behaviour during SARS-CoV-2 epidemic: Nonparametric estimation. Sci. Rep. 2021, 11, 9772. [Google Scholar] [CrossRef]
- Qian, Y.; Xie, W.; Zhao, J.; Xue, M.; Liu, S.; Wang, L.; Li, W.; Dai, L.; Cai, Y. Investigating the effectiveness of re-opening policies before vaccination during a pandemic: SD modelling research based on COVID-19 in Wuhan. BMC Public Health 2021, 21, 1638. [Google Scholar] [CrossRef]
- Raoofi, A.; Takian, A.; Akbari, S.A.; Olyaeemanesh, A.; Haghighi, H.; Aarabi, M. COVID-19 Pandemic and Comparative Health Policy Learning in Iran. Arch. Iran. Med. 2020, 23, 220–234. [Google Scholar] [CrossRef]
- Riley, C.; Xie, B.; Khurshid, A. Challenges encountered in comparing international policy responses to COVID-19 and their effects. Health Res. Policy Syst. 2021, 19, 134. [Google Scholar] [CrossRef]
- Talabis, D.A.S.; Babierra, A.L.; Buhat, C.A.H.; Lutero, D.S.; Quindala, K.M., 3rd; Rabajante, J.F. Local government responses for COVID-19 management in the Philippines. BMC Public Health 2021, 21, 1711. [Google Scholar] [CrossRef]
- Vo, D.H.; Doan, B. Effects from containment and closure policies to market quality: Do they really matter in Vietnam during COVID-19? PLoS ONE 2021, 16, e0248703. [Google Scholar] [CrossRef]
- Banerji, A.K. The Need for Uniform Residency Training Programs and the Challenges During COVID-19 Pandemic for India. Neurol. India 2021, 69, 751–752. [Google Scholar] [CrossRef]
- Timmers, T.; Janssen, L.; Stohr, J.; Murk, J.L.; Berrevoets, M. Using eHealth to Support COVID-19 Education, Self-Assessment, and Symptom Monitoring in the Netherlands: Observational Study. JMIR mhealth uhealth 2020, 8, e19822. [Google Scholar] [CrossRef]
- Gimbrone, C.; Rutherford, C.; Kandula, S.; Martínez-Alés, G.; Shaman, J.; Olfson, M.; Gould, M.S.; Pei, S.; Galanti, M.; Keyes, K.M. Associations between COVID-19 mobility restrictions and economic, mental health, and suicide-related concerns in the US using cellular phone GPS and Google search volume data. PLoS ONE 2021, 16, e0260931. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, B.A.; Peitzmeier, S.M.; Restar, A.; Adamson, T.; Howell, S.; Baral, S.; Beckham, S.W. Gender-affirming care, mental health, and economic stability in the time of COVID-19: A multi-national, cross-sectional study of transgender and nonbinary people. PLoS ONE 2021, 16, e0254215. [Google Scholar] [CrossRef] [PubMed]
- Al-Sa’d, M.; Kiranyaz, S.; Ahmad, I.; Sundell, C.; Vakkuri, M.; Gabbouj, M. A Social Distance Estimation and Crowd Monitoring System for Surveillance Cameras. Sensors 2022, 22, 418. [Google Scholar] [CrossRef]
- Albouy-Llaty, M.; Martin, C.; Benamouzig, D.; Bothorel, E.; Munier, G.; Simonin, C.; Guéant, J.L.; Rusch, E. Positioning Digital Tracing Applications in the Management of the COVID-19 Pandemic in France. J. Med. Internet Res. 2021, 23, e27301. [Google Scholar] [CrossRef] [PubMed]
- Alo, U.R.; Nkwo, F.O.; Nweke, H.F.; Achi, I.I.; Okemiri, H.A. Non-Pharmaceutical Interventions against COVID-19 Pandemic: Review of Contact Tracing and Social Distancing Technologies, Protocols, Apps, Security and Open Research Directions. Sensors 2021, 22, 280. [Google Scholar] [CrossRef] [PubMed]
- Garrett, P.M.; White, J.P.; Lewandowsky, S.; Kashima, Y.; Perfors, A.; Little, D.R.; Geard, N.; Mitchell, L.; Tomko, M.; Dennis, S. The acceptability and uptake of smartphone tracking for COVID-19 in Australia. PLoS ONE 2021, 16, e0244827. [Google Scholar] [CrossRef] [PubMed]
- Gazizov, R.R. Dynamics of Russian Television News Broadcasting in the Context of the Reflection of the COVID-19 Pandemic. J. Educ. Psychol. 2020, 8, e758. [Google Scholar] [CrossRef]
- Hu, G.; Li, P.; Yuan, C.; Tao, C.; Wen, H.; Liu, Q.; Qiu, W. Information Disclosure During the COVID-19 Epidemic in China: City-Level Observational Study. J. Med. Internet Res. 2020, 22, e19572. [Google Scholar] [CrossRef]
- Jang, H.; Rempel, E.; Roth, D.; Carenini, G.; Janjua, N.Z. Tracking COVID-19 Discourse on Twitter in North America: Infodemiology Study Using Topic Modeling and Aspect-Based Sentiment Analysis. J. Med. Internet Res. 2021, 23, e25431. [Google Scholar] [CrossRef] [PubMed]
- Kamel Boulos, M.N.; Geraghty, E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020, 19, 8. [Google Scholar] [CrossRef]
- Kondylakis, H.; Katehakis, D.G.; Kouroubali, A.; Logothetidisal, F.; Triantafyllidis, A.; Kalamaras, I.; Votis, K.; Tzovaras, D. COVID-19 Mobile Apps: A Systematic Review of the Literature. J. Med. Internet Res. 2020, 22, e23170. [Google Scholar] [CrossRef]
- Leins, K.; Culnane, C.; Rubinstein, B.I. Tracking, tracing, trust: Contemplating mitigating the impact of COVID-19 with technological interventions. Med. J. Aust. 2020, 213, 6–8. [Google Scholar] [CrossRef]
- Manfredi-Sánchez, J.L.; Amado-Suárez, A.; Waisbord, S. Presidential Twitter in the Face of COVID-19: Between Populism and Pop Politics. Comun. Media Educ. Res. J. 2021, 29, 79–90. [Google Scholar] [CrossRef]
- Moon, H.; Lee, G.H. Evaluation of Korean-Language COVID-19-Related Medical Information on YouTube: Cross-Sectional Infodemiology Study. J. Med. Internet Res. 2020, 22, e20775. [Google Scholar] [CrossRef] [PubMed]
- Ngai, C.S.B.; Singh, R.G.; Lu, W.; Koon, A.C. Grappling with the COVID-19 Health Crisis: Content Analysis of Communication Strategies and Their Effects on Public Engagement on Social Media. J. Med. Internet Res. 2020, 22, e21360. [Google Scholar] [CrossRef] [PubMed]
- Phillips, J.; Babcock, R.A.; Orbinski, J. The digital response to COVID-19: Exploring the use of digital technology for information collection, dissemination and social control in a global pandemic. J. Bus. Contin. Emerg. Plan. 2021, 14, 333–353. Available online: https://aircconline.com/hiij/V11N1/11122hiij01.pdf (accessed on 22 January 2023).
- Saw, Y.E.; Tan, E.Y.Q.; Liu, J.S.; Liu, J.C.J. Predicting Public Uptake of Digital Contact Tracing During the COVID-19 Pandemic: Results From a Nationwide Survey in Singapore. J. Med. Internet Res. 2021, 23, e24730. [Google Scholar] [CrossRef] [PubMed]
- Soldano, G.J.; Fraire, J.A.; Finochietto, J.M.; Quiroga, R. COVID-19 mitigation by digital contact tracing and contact prevention (app-based social exposure warnings). Sci. Rep. 2021, 11, 14421. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Fernández, E.; Astorza, A.D.; Pérez de Llano, L.A.; Fernández-Villar, A.; Carnicer-Pont, D.; Alcázar-Navarrete, B.; García, A.; Morales, A.; Lobo, M.; et al. Hospital Pandemics Tracker (HEpiTracker): Description and Pilot Study of a Mobile App to Track COVID-19 in Hospital Workers. JMIR Public Health Surveill. 2020, 6, e21653. [Google Scholar] [CrossRef] [PubMed]
- Vavrinsky, E.; Zavodnik, T.; Debnar, T.; Cernaj, L.; Kozarik, J.; Micjan, M.; Nevrela, J.; Donoval, M.; Kopani, M.; Kosnacova, H. Research and Development of a COVID-19 Tracking System in Order to Implement Analytical Tools to Reduce the Infection Risk. Sensors 2022, 22, 526. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ding, S.; Li, X. A New System for Surveillance and Digital Contact Tracing for COVID-19: Spatiotemporal Reporting Over Network and GPS. J. Med. Internet Res. 2020, 22, e19457. [Google Scholar] [CrossRef]
- Wnuk, A.; Oleksy, T.; Maison, D. The acceptance of COVID-19 tracking technologies: The role of perceived threat, lack of control, and ideological beliefs. PLoS ONE 2020, 15, e0238973. [Google Scholar] [CrossRef]
- Zeng, K.; Bernardo, S.N.; Havins, W.E. The Use of Digital Tools to Mitigate the COVID-19 Pandemic: Comparative Retrospective Study of Six Countries. JMIR Public Health Surveill. 2020, 6, e24598. [Google Scholar] [CrossRef] [PubMed]
- Zeng, R.; Li, M. Social Media Use for Health Communication by the CDC in Mainland China: National Survey Study 2009–2020. J. Med. Internet Res. 2020, 22, e19470. [Google Scholar] [CrossRef] [PubMed]
- Cerda, A.A.; García, L.Y. Factors explaining the fear of being infected with COVID-19. Health Expect 2022, 25, 506–512. [Google Scholar] [CrossRef]
- Lau, A. Hospital-Based Nurses’ Perceptions of the Adoption of Web 2.0 Tools for Knowledge Sharing, Learning, Social Interaction and the Production of Collective Intelligence. J. Med. Internet Res. 2011, 13, e92. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.L. COVID-19 information on social media and preventive behaviors: Managing the pandemic through personal responsibility. Soc. Sci. Med. 2021, 277, 113928. [Google Scholar] [CrossRef] [PubMed]
- Nagarajan, K.; Muniyandi, M.; Palani, B.; Sellappan, S. Social network analysis methods for exploring SARS-CoV-2 contact tracing data. BMC Med. Res. Methodol. 2020, 20, 233. [Google Scholar] [CrossRef] [PubMed]
- Jayaweera, M.; Perera, M.; Gunawardana, B.; Manatungea, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819. [Google Scholar] [CrossRef] [PubMed]
- Lio, C.F.; Cheong, H.H.; Lei, C.I.; Lo, I.L.; Yai, L.; Lam, C.; Leong, L.H. Effectiveness of personal protective health behaviour against COVID-19. BMC Public Health 2021, 21, 827. [Google Scholar] [CrossRef] [PubMed]
- Lau, A. Strategies to Encourage the Adoption of G2C E-government Services in Hong Kong. Int. J. Electron. Gov. 2004, 1, 273–292. [Google Scholar] [CrossRef]
- Lau, A.S.M.; Kwok, V.W.S. How Government Strategies Influence E-commerce Adoption by SME. Int. J. Electron. Gov. 2007, 4, 20–42. [Google Scholar] [CrossRef]
- Bi, X.; Zhang, Q.; Fan, K.; Tang, S.Y.; Guan, H.W.; Gao, X.Q.; Cui, Y.; Ma, Y.; Wu, Q.H.; Hao, Y.H.; et al. Risk Culture and COVID-19 Protective Behaviors: A Cross-Sectional Survey of Residents in China. Front. Public Health 2021, 9, e686705. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Biswas, M.I. Impact of national culture on the severity of the COVID-19 pandemic. Curr. Psychol. 2022, 42, 15813–15826. [Google Scholar] [CrossRef] [PubMed]
- Dawi, N.M.; Namazi, H.; Maresova, P. Predictors of COVID-19 Preventive Behavior Adoption Intention in Malaysia. Front. Psychol. 2021, 12, 616749. [Google Scholar] [CrossRef] [PubMed]
- Wollast, R.; Schmitz, M. The Theory of Planned Behavior during the COVID-19 pandemic: A comparison of health behaviors between Belgian and French residents. PLoS ONE 2021, 6, e0258320. [Google Scholar] [CrossRef] [PubMed]
- Yamaka, W.; Lomwanawong, S.; Magel, D.; Maneejuk, P. Analysis of the Lockdown Effects on the Economy, Environment, and COVID-19 Spread: Lesson Learnt from a Global Pandemic in 2020. Int. J. Environ. Res. Public Health 2023, 19, 12868. [Google Scholar] [CrossRef] [PubMed]
- Kundu, S.; Hasan Al Banna, K.; Sayeed, A.; Begum, M.R.; Brazendale, K.; Hasan, M.T.; Habiba, S.J.; Abid, M.T.; Khan, M.A.; Chowdhury, S.; et al. Knowledge, attitudes, and preventive practices toward the COVID-19 pandemic: An online survey among bangladeshi residents. J. Public Health 2021, 31, 1121–1135. [Google Scholar] [CrossRef] [PubMed]
- Buckner, H.T. A Theory of Rumor Transmission. Public Opin. Q. 1965, 29, 54–70. [Google Scholar] [CrossRef]
- Agarwal, P.; Aziz, P.A.; Zhuang, J. Interplay of rumor propagation and clarification on social media during crisis events—A game-theoretic approach. Eur. J. Oper. Res. 2022, 298, 714–733. [Google Scholar] [CrossRef]
- Lau, A. Implementation of an onto-wiki toolkit using web services to improve the efficiency and effectiveness of medical ontology co-authoring and analysis. Inform. Health Soc. Care 2009, 34, 73–80. [Google Scholar] [CrossRef]
- Lau, A.; Tsui, E.; Lee, W.B. An Ontology-based Similarity Measurement for Problem-based Case Reasoning. Expert Syst. Appl. 2009, 36, 6574–6579. [Google Scholar] [CrossRef]
- Xue, J.; Chen, J.; Hu, R.; Chen, C.; Zheng, C.; Su, Y.; Zhu, T. Twitter Discussions and Emotions About the COVID-19 Pandemic: Machine Learning Approach. J. Med. Internet Res. 2020, 22, e20550. [Google Scholar] [CrossRef] [PubMed]
- Hernández-García, I.; Giménez-Júlvez, T. Assessment of Health Information About COVID-19 Prevention on the Internet: Infodemiological Study. JMIR Public Health Surveill. 2020, 6, e18717. [Google Scholar] [CrossRef] [PubMed]
- Nasser, N.; Karim, L.; Ouadrhiri, A.E.; Ali, A.; Khanb, N. N-Gram based language processing using Twitter dataset to identify COVID-19 patients. Sustain. Cities Soc. 2021, 72, e103048. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.T.; Fujimura, T.; Katahira, K.; Okada, M.; Ueno, K.; Cheng, K.; Okanoya, K. The implicit processing of categorical and dimensional strategies: An fMRI study of facial emotion perception. Front. Hum. Neurosci. 2013, 7, 551. [Google Scholar] [CrossRef] [PubMed]
- Shu, L.; Xie, J.; Yang, M.; Li, Z.; Li, Z.; Liao, D.; Xu, X.; Yang, X. A Review of Emotion Recognition Using Physiological Signals. Sensors 2018, 18, 2074. [Google Scholar] [CrossRef] [PubMed]
- Ojo, A.; Guntuku, S.C.; Zheng, M.; Beidas, R.S.; Ranney, M.L. How Health Care Workers Wield Influence Through Twitter Hashtags: Retrospective Cross-sectional Study of the Gun Violence and COVID-19 Public Health Crises. JMIR Public Health Surveill. 2021, 7, e24562. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Lin, W.; Lin, S.; Wang, J.; Yu, L.C. A multi-dimensional relation model for dimensional sentiment analysis. Inf. Sci. 2021, 579, 832–844. [Google Scholar] [CrossRef]
- Ahmad, M.; Aftab, S.; Muhammad, S.S.; Ahmad, S. Machine Learning Techniques for Sentiment Analysis: A Review. Int. J. Multidiscip. Sci. Eng. 2017, 8, 27–32. [Google Scholar]
- Hung, M.; Lauren, E.; Hon, E.s.; Birmingham, W.C.; Xu, J.; Su, S.; Hon, S.D.; Park, J.; Dang, P.; Lipsky, M.S. Social Network Analysis of COVID-19 Sentiments: Application of Artificial Intelligence. J. Med. Internet Res. 2020, 22, e22590. [Google Scholar] [CrossRef]
- Liew, T.M.; Lee, C.S. Examining the Utility of Social Media in COVID-19 Vaccination: Unsupervised Learning of 672, 133 Twitter Posts. JMIR Public Health Surveill. 2021, 7, e29789. [Google Scholar] [CrossRef]
- Mehta, P.; Pandya, S. A Review On Sentiment Analysis Methodologies, Practices And Applications. Int. J. Sci. Technol. Res. 2020, 9, 601–609. [Google Scholar] [CrossRef]
- Petrescu, L.; Petrescu, C.; Oprea, A.; Mitrut, O.; Moise, G.; Moldoveanu, A.; Moldoveanu, F. Machine Learning Methods for Fear Classification Based on Physiological Features. Sensors 2021, 21, 4519. [Google Scholar] [CrossRef] [PubMed]
- Mao, Z.; Yao, H.; Zou, Q.; Zhang, Q.; Dong, Y. Digital Contact Tracing Based on a Graph Database Algorithm for Emergency Management During the COVID-19 Pandemic: Case Study. J. Med. Internet Res. 2021, 9, e26836. [Google Scholar] [CrossRef]

| Keywords Search with COVID-19 | Relevant/Returned Studies | Environmental Factors | References |
|---|---|---|---|
| Fear, anxiety, worry | 14/127 | Fear of the spread of pandemic | [9,15,19,20,21,22,23,24,25,26,27,28,29,30] |
| Hygiene practice | 5/7 | Intentional behaviors of hygiene practices | [31,32,33,34,35] |
| Pandemic prevention | 12/96 | Cultural behaviors of pandemic prevention | [14,36,37,38,39,40,41,42,43,44,45] |
| Government policy, pandemic policy | 25/220 | Government policies on pandemic prevention | [11,12,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] |
| Pandemic education program | 2/31 | Attitudes of pandemic education program | [69,70] |
| Pandemic economic, business restriction | 2/16 | Attitudes of economic and business restrictions | [71,72] |
| Contact-tracking technology, Multimedia, channel, information dissemination | 24/91 | Attitudes of technology infrastructure and multimedia for information dissemination and disclosure | [2,18,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94] |
| Environmental Factors | Measurement Metrics or Experiments for Future Work |
|---|---|
| Fear of the pandemic spreading | Fear index is a measurement metric to measure the risk perception on pandemic spread of individuals. The public sentiments on the fear of the pandemic spread (e.g., stress, anxiety, etc.) from social media are calculated. |
| Intentional behaviors of hygiene practices | Hygiene index is a measurement metric to measure the attitudes of hygiene practices of individuals (e.g., handwash, wearing mask, social distancing, contact tracking, decontamination, etc.) for pandemic prevention. The public sentiment scores on hygiene practices are calculated from social media. |
| Cultural behaviors of pandemic prevention | Culture index is a measurement metric to measure the cultural attitudes on pandemic prevention (e.g., handwash, wearing masks, social distancing, contact tracking, decontamination, etc.). The public sentiment score of pandemic prevention of different races or religions from social media are calculated. |
| Attitudes of government policies on pandemic prevention | Policy index is a measurement metric to measure the attitudes of government policies on pandemic prevention (including pandemic prevention, education programs, economic and business activity restrictions, technology and multimedia infrastructure). The public sentiment score of government policies on pandemic prevention are calculated from social media. |
| Attitudes of pandemic education program | It is a sub-score of policy index. This measures the attitudes of the governmental pandemic education programs (e.g., procedures of wearing masks, washing hands, and COVID-19 testing). The public sentiment score on governmental pandemic education programs from social media are calculated. |
| Attitudes of economic and business restrictions | It is a sub-score of policy index. This measures the attitudes of the economic and business restriction policies (e.g., lockdown cities, travel ban and quarantine, and COVID-19 vaccination requirement of visitors). The public sentiment score on economic and business restriction policies from social media are calculated. |
| Attitudes of technology infrastructure and multimedia for information dissemination and disclosure | It is a sub-score of policy index. This measures the attitudes of the technology infrastructure for information dissemination (e.g., social monitoring app, COVID-19 reporting system, and temperature measurement equipment in public places) and the multimedia for information disclosure (e.g., news, social media, and government web pages). The public sentiment score on technology infrastructure and multimedia for pandemic information dissemination from social media are calculated. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheung, L.; Lau, A.S.M.; Lam, K.F.; Ng, P.Y. A Review of Environmental Factors for an Ontology-Based Risk Analysis for Pandemic Spread. COVID 2024, 4, 466-480. https://doi.org/10.3390/covid4040031
Cheung L, Lau ASM, Lam KF, Ng PY. A Review of Environmental Factors for an Ontology-Based Risk Analysis for Pandemic Spread. COVID. 2024; 4(4):466-480. https://doi.org/10.3390/covid4040031
Chicago/Turabian StyleCheung, Liege, Adela S. M. Lau, Kwok Fai Lam, and Pauline Yeung Ng. 2024. "A Review of Environmental Factors for an Ontology-Based Risk Analysis for Pandemic Spread" COVID 4, no. 4: 466-480. https://doi.org/10.3390/covid4040031






