Pain, Function and Trunk/Hip Flexibility Changes Immediately after Clinical Pilates Exercises in Young Adults with Mild Chronic Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
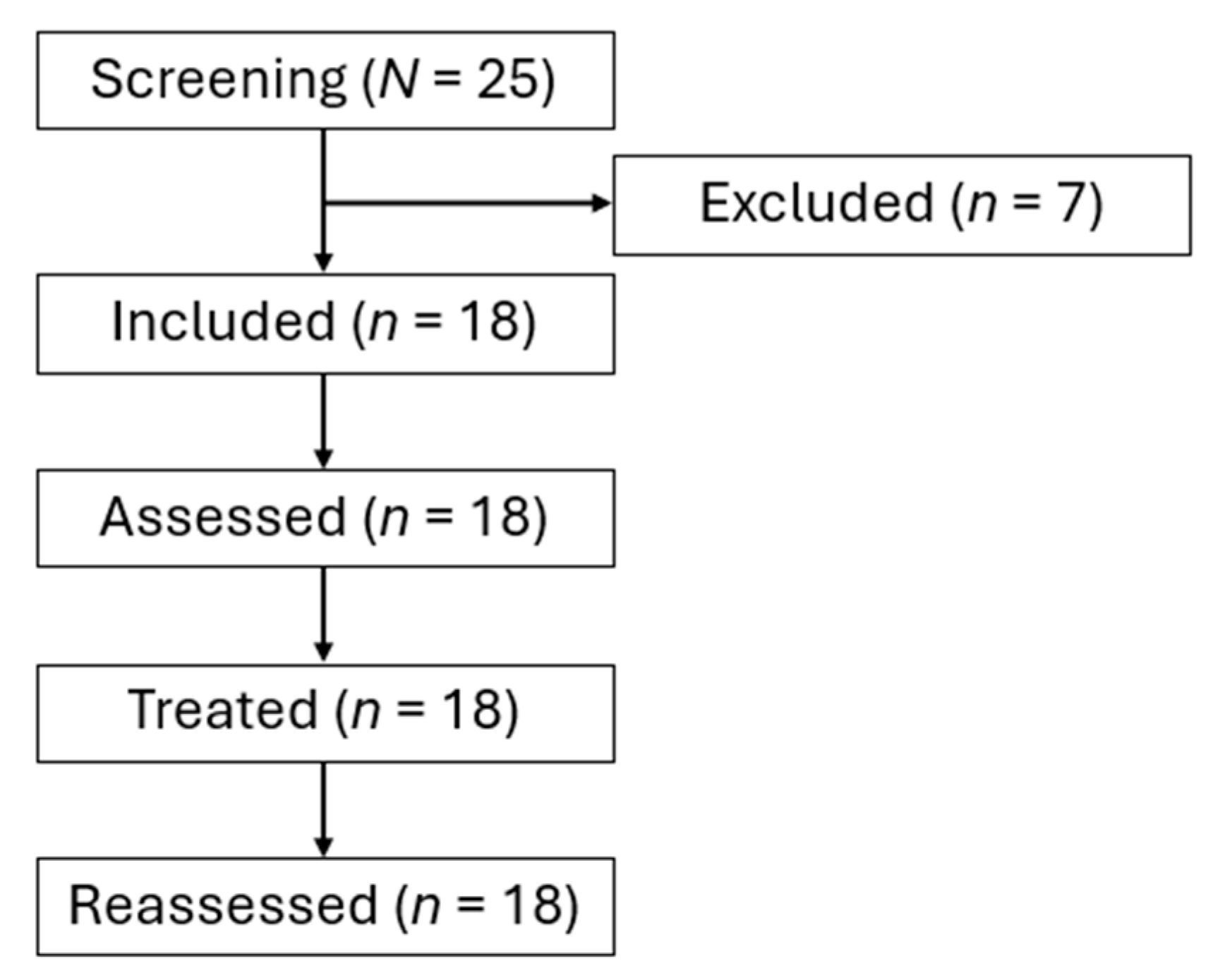
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
2.3.1. Self-Reported Outcomes
2.3.2. Physical Strength Outcomes
2.3.3. Flexibility Outcomes
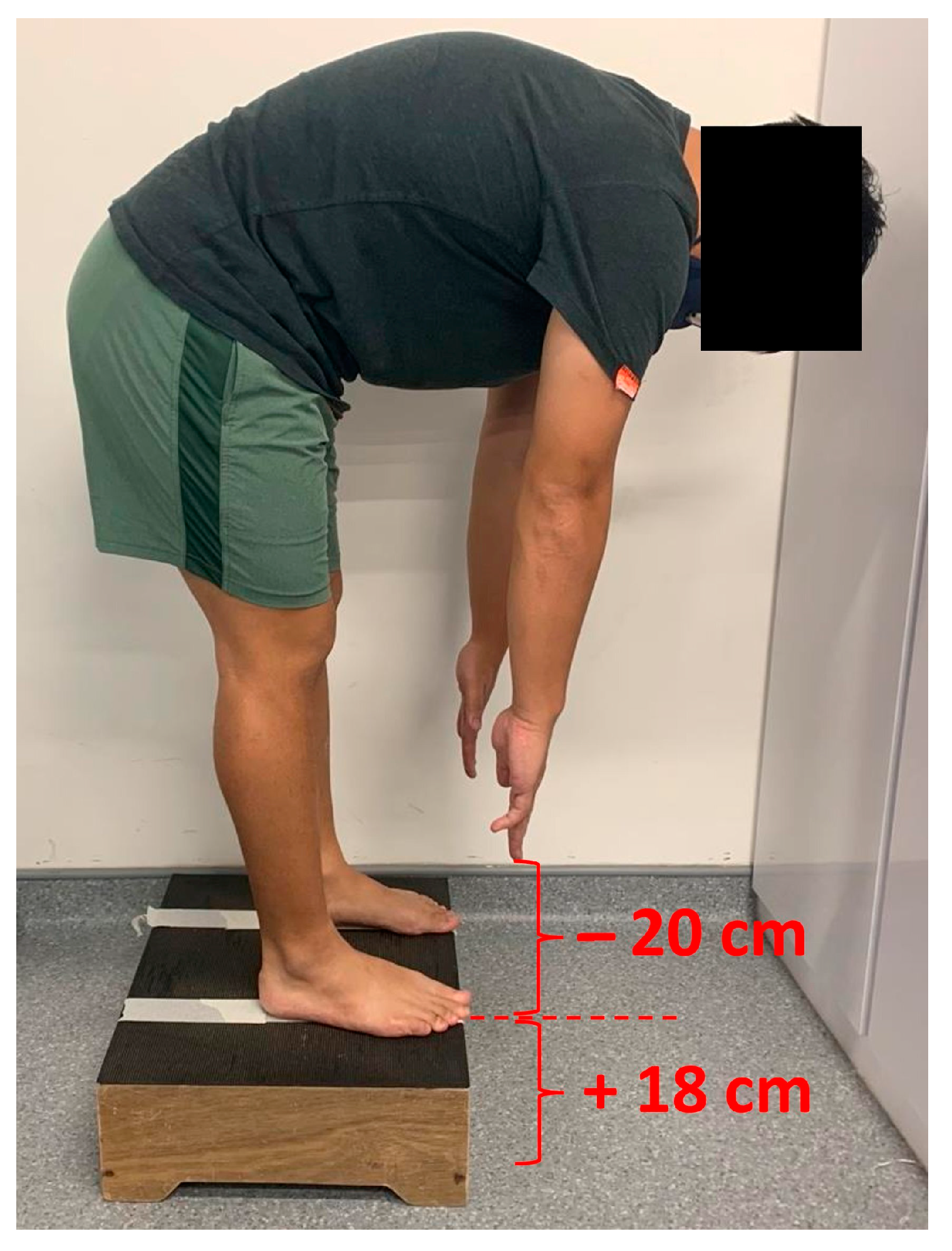
2.4. Intervention
2.5. Sample Size
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fatoye, F.; Gebrye, T.; Odeyemi, I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol. Int. 2019, 39, 619–626. [Google Scholar] [CrossRef]
- Yeo, S.N.; Tay, K.H. Pain prevalence in singapore. Ann. Acad. Med. Singap. 2009, 38, 937–942. [Google Scholar] [CrossRef]
- Leboeuf-Yde, C.; Kyvik, K.O. At what age does low back pain become a common problem?: A study of 29,424 individuals aged 12-41 years. Spine 1998, 23, 228–234. [Google Scholar] [CrossRef]
- Maher, C.; Underwood, M.; Buchbinder, R. Non-specific low back pain. Lancet 2017, 389, 736–747. [Google Scholar] [CrossRef]
- Cassidy, J.D.; Cote, P.; Carroll, L.J.; Kristman, V. Incidence and course of low back pain episodes in the general population. Spine 2005, 30, 2817–2823. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, J.; Carter, A.; Casey, D.C.; Charlson, F.J.; Coates, M.M.; Coggeshall, M. Global, regional, and national disability-adjusted life-years (dalys) for 315 diseases and injuries and healthy life expectancy (hale), 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet 2016, 388, 1603–1658. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the global burden of disease study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef] [PubMed]
- Chou, R.; Deyo, R.; Friedly, J.; Skelly, A.; Hashimoto, R.; Weimer, M.; Fu, R.; Dana, T.; Kraegel, P.; Griffin, J.; et al. Nonpharmacologic therapies for low back pain: A systematic review for an american college of physicians clinical practice guideline. Ann. Intern. Med. 2017, 166, 493–505. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Stewart, S.A.; Bagg, M.K.; Stanojevic, S.; Yamato, T.P.; Saragiotto, B.T. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J. Physiother. 2021, 67, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Rodriguez, R.; Alvarez-Bueno, C.; Cavero-Redondo, I.; Torres-Costoso, A.; Pozuelo-Carrascosa, D.P.; Reina-Gutierrez, S.; Pascual-Morena, C.; Martinez-Vizcaino, V. Best exercise options for reducing pain and disability in adults with chronic low back pain: Pilates, strength, core-based, and mind-body. A network meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 505–521. [Google Scholar] [CrossRef]
- Patti, A.; Thornton, J.S.; Giustino, V.; Drid, P.; Paoli, A.; Schulz, J.M.; Palma, A.; Bianco, A. Effectiveness of pilates exercise on low back pain: A systematic review with meta-analysis. Disabil. Rehabil. 2023, 1–14. [Google Scholar] [CrossRef]
- Kwok, B.C.; Lim, J.X.L.; Kong, P.W. The theoretical framework of the clinical pilates exercise method in managing non-specific chronic low back pain: A narrative review. Biology 2021, 10, 1096. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, E.; Phillips, C.; Sole, G.; Carman, A.; Abbott, J.H. Dma clinical pilates directional-bias assessment: Reliability and predictive validity. J. Orthop. Sports Phys. Ther. 2012, 42, 676–687. [Google Scholar] [CrossRef]
- Lim, E.A.Y.Y.; Yeo, R.Y.T.; Kwok, B.C. Influence of hip flexion angle on strength and gluteal muscle activities in the clinical pilates clamshell exercise. J. Bodyw. Mov. Ther. 2023, 36, 417–424. [Google Scholar] [CrossRef]
- Wajswelner, H.; Metcalf, B.; Bennell, K. Clinical pilates versus general exercise for chronic low back pain: Randomized trial. Med. Sci. Sports Exerc. 2012, 44, 1197–1205. [Google Scholar] [CrossRef]
- Cai, C.; Yang, Y.; Kong, P.W. Comparison of lower limb and back exercises for runners with chronic low back pain. Med. Sci. Sports Exerc. 2017, 49, 2374–2384. [Google Scholar] [CrossRef]
- Vatovec, R.; Voglar, M. Changes of trunk muscle stiffness in individuals with low back pain: A systematic review with meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 155. [Google Scholar] [CrossRef] [PubMed]
- Hashemirad, F.; Talebian, S.; Hatef, B.; Kahlaee, A.H. The relationship between flexibility and emg activity pattern of the erector spinae muscles during trunk flexion-extension. J. Electromyogr. Kinesiol. 2009, 19, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Valenza, M.C.; Rodriguez-Torres, J.; Cabrera-Martos, I.; Diaz-Pelegrina, A.; Aguilar-Ferrandiz, M.E.; Castellote-Caballero, Y. Results of a pilates exercise program in patients with chronic non-specific low back pain: A randomized controlled trial. Clin. Rehabil. 2017, 31, 753–760. [Google Scholar] [CrossRef]
- Mostagi, F.Q.; Dias, J.M.; Pereira, L.M.; Obara, K.; Mazuquin, B.F.; Silva, M.F.; Silva, M.A.; de Campos, R.R.; Barreto, M.S.; Nogueira, J.F.; et al. Pilates versus general exercise effectiveness on pain and functionality in non-specific chronic low back pain subjects. J. Bodyw. Mov. Ther. 2015, 19, 636–645. [Google Scholar] [CrossRef]
- Dworkin, R.H.; Turk, D.C.; Farrar, J.T.; Haythornthwaite, J.A.; Jensen, M.P.; Katz, N.P.; Kerns, R.D.; Stucki, G.; Allen, R.R.; Bellamy, N. Core outcome measures for chronic pain clinical trials: Immpact recommendations. Pain. 2005, 113, 9–19. [Google Scholar] [CrossRef]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short-form mcgill pain questionnaire (sf-mpq), chronic pain grade scale (cpgs), short form-36 bodily pain scale (sf-36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis Care Res. (Hoboken) 2011, 63 (Suppl. S11), S240–S252. [Google Scholar]
- Stratford, P.; Gill, C.; Westaway, M.; Binkley, J. Assessing disability and change on individual patients: A report of a patient specific measure. Physiother. Can. 1995, 47, 258–263. [Google Scholar] [CrossRef]
- Katoh, M.; Yamasaki, H. Test-retest reliability of isometric leg muscle strength measurements made using a hand-held dynamometer restrained by a belt: Comparisons during and between sessions. J. Phys. Ther. Sci. 2009, 21, 239–243. [Google Scholar] [CrossRef]
- Jackson, A.W.; Morrow, J.R., Jr.; Brill, P.A.; Kohl, H.W., 3rd; Gordon, N.F.; Blair, S.N. Relations of sit-up and sit-and-reach tests to low back pain in adults. J. Orthop. Sports Phys. Ther. 1998, 27, 22–26. [Google Scholar] [CrossRef]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain 2004, 8, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Bogduk, N. Calibrating effect-size for studies of pain treatment. Interv. Pain Med. 2022, 1, 100123. [Google Scholar] [CrossRef]
- Picha, K.J.; Howell, D.M. A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self-efficacy. Musculoskelet. Care 2018, 16, 233–237. [Google Scholar] [CrossRef]
- Maughan, E.F.; Lewis, J.S. Outcome measures in chronic low back pain. Eur. Spine J. 2010, 19, 1484–1494. [Google Scholar] [CrossRef]
- Hagg, O.; Fritzell, P.; Nordwall, A.; Swedish Lumbar Spine Study, G. The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur. Spine J. 2003, 12, 12–20. [Google Scholar] [CrossRef]
- Miyamoto, G.C.; Costa, L.O.; Cabral, C.M. Efficacy of the pilates method for pain and disability in patients with chronic nonspecific low back pain: A systematic review with meta-analysis. Braz. J. Phys. Ther. 2013, 17, 517–532. [Google Scholar] [CrossRef] [PubMed]
- Altenburger, P.; Ambike, S.S.; Haddad, J.M. Integrating motor variability evaluation into movement system assessment. Phys. Ther. 2023, 103, pzad075. [Google Scholar] [CrossRef] [PubMed]
- Bacurau, R.F.; Monteiro, G.A.; Ugrinowitsch, C.; Tricoli, V.; Cabral, L.F.; Aoki, M.S. Acute effect of a ballistic and a static stretching exercise bout on flexibility and maximal strength. J. Strength. Cond. Res. 2009, 23, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Carroll, T.J.; Taylor, J.L.; Gandevia, S.C. Recovery of central and peripheral neuromuscular fatigue after exercise. J. Appl. Physiol. 2017, 122, 1068–1076. [Google Scholar] [CrossRef] [PubMed]
- Morton, S.K.; Whitehead, J.R.; Brinkert, R.H.; Caine, D.J. Resistance training vs. Static stretching: Effects on flexibility and strength. J. Strength. Cond. Res. 2011, 25, 3391–3398. [Google Scholar] [CrossRef] [PubMed]
- Harkapaa, K.; Jarvikoski, A.; Mellin, G.; Hurri, H.; Luoma, J. Health locus of control beliefs and psychological distress as predictors for treatment outcome in low-back pain patients: Results of a 3-month follow-up of a controlled intervention study. Pain 1991, 46, 35–41. [Google Scholar] [CrossRef]
- French, O.; Mattacola, E. How has the covid-19 pandemic affected patients’ experience of pain management therapy? Br. J. Pain 2023, 17, 46–57. [Google Scholar] [CrossRef]

| Demographics | Distribution |
|---|---|
| Age, years, mean (SD) | 23.1 (1.8) |
| Gender, female, n (%) | 12 (66.67) |
| Body weight, kg, mean (SD) | 65.06 (11.65) |
| Height, m, mean (SD) | 1.67 (0.06) |
| Body mass index, kg/m2, mean (SD) | 23.41 (3.79) |
| Fear-Avoidance Beliefs Questionnaire—Physical activity, /24, mean (SD) | 11.28 (5.42) |
| International Physical Activity Questionnaire—short, n (%) | |
| Low | 9 (50) |
| Moderate | 7 (38.9) |
| High | 2 (11.1) |
| Oswestry Disability Index, %, mean (SD) | 12.79 (5.87) |
| Outcome Measures | Time-Points, Mean (SD) | Mean Difference (SD) | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Pre | Post | ||||
| Self-reported | |||||
| Pain visual analog scale, /10 | 2.22 (1.87) | 0.67 (1.03) | 1.56 (1.46) | 0.83 to 2.28 | <0.001 |
| Patient-specific functional scale, /10 | 6.36 (1.40) | 7.88 (0.98) | −1.52 (0.83) | −1.93 to −1.10 | <0.001 |
| Strength—problem side | |||||
| Hip extensors, N | 198.08 (79.73) | 192.92 (70.68) | 5.16 (34.46) | −11.98 to 22.29 | 0.534 |
| Hip abductors, N | 225.64 (77.64) | 227.81 (84.20) | −2.17 (33.63) | −18.90 to 14.55 | 0.787 |
| Knee extensors, N | 220.93 (71.98) | 236.88 (75.35) | −15.94 (38.80) | −35.24 to 3.35 | 0.099 |
| Strength—non-problem side | |||||
| Hip extensors, N | 204.83 (63.45) | 195.08 (63.21) | 9.74 (42.74) | −11.51 to 31.00 | 0.347 |
| Hip abductors, N | 237.93 (95.62) | 226.73 (72.18) | 11.19 (37.52) | −7.46 to 29.85 | 0.223 |
| Knee extensors, N | 224.76 (44.33) | 234.27 (79.32) | −9.52 (44.36) | −31.58 to 12.54 | 0.375 |
| Flexibility | |||||
| Sit-and-reach test, cm | 24.06 (7.99) | 27.50 (6.51) | −3.44 (3.33) | −5.10 to −1.79 | <0.001 |
| Finger-to-floor test, cm | −10.42 (12.80) | −4.13 (9.57) | −6.29 (6.49) | −9.51 to −3.06 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, L.Y.; Teh, R.H.R.; Kwok, B.C. Pain, Function and Trunk/Hip Flexibility Changes Immediately after Clinical Pilates Exercises in Young Adults with Mild Chronic Low Back Pain. BioMed 2024, 4, 203-212. https://doi.org/10.3390/biomed4030016
Tan LY, Teh RHR, Kwok BC. Pain, Function and Trunk/Hip Flexibility Changes Immediately after Clinical Pilates Exercises in Young Adults with Mild Chronic Low Back Pain. BioMed. 2024; 4(3):203-212. https://doi.org/10.3390/biomed4030016
Chicago/Turabian StyleTan, Li Yi, Ryan Han Rong Teh, and Boon Chong Kwok. 2024. "Pain, Function and Trunk/Hip Flexibility Changes Immediately after Clinical Pilates Exercises in Young Adults with Mild Chronic Low Back Pain" BioMed 4, no. 3: 203-212. https://doi.org/10.3390/biomed4030016
APA StyleTan, L. Y., Teh, R. H. R., & Kwok, B. C. (2024). Pain, Function and Trunk/Hip Flexibility Changes Immediately after Clinical Pilates Exercises in Young Adults with Mild Chronic Low Back Pain. BioMed, 4(3), 203-212. https://doi.org/10.3390/biomed4030016







