Organic Dust Exposure Enhances SARS-CoV-2 Entry in a PKCα- and ADAM-17-Dependent Manner
Abstract
1. Introduction
2. Materials and Methods
2.1. SARS-CoV-2 Pseudovirus
2.2. Mice Experiments
2.3. Mouse Lung ACE2 Quantitation
2.4. RNA Extraction and Quantitative Polymerase Chain Reaction (qPCR)
2.5. BEAS-2B Cells
2.6. PKCα Activity Assay
2.7. BEAS-2B Cell Treatments and Infection
2.8. ACE2 Expression by Flow Cytometry
2.9. Quantification of BEAS-2B Pseudovirus Infection by Immunofluorescence
2.10. Interleukin-8 (IL-8) ELISA
2.11. Statistical Analysis
3. Results
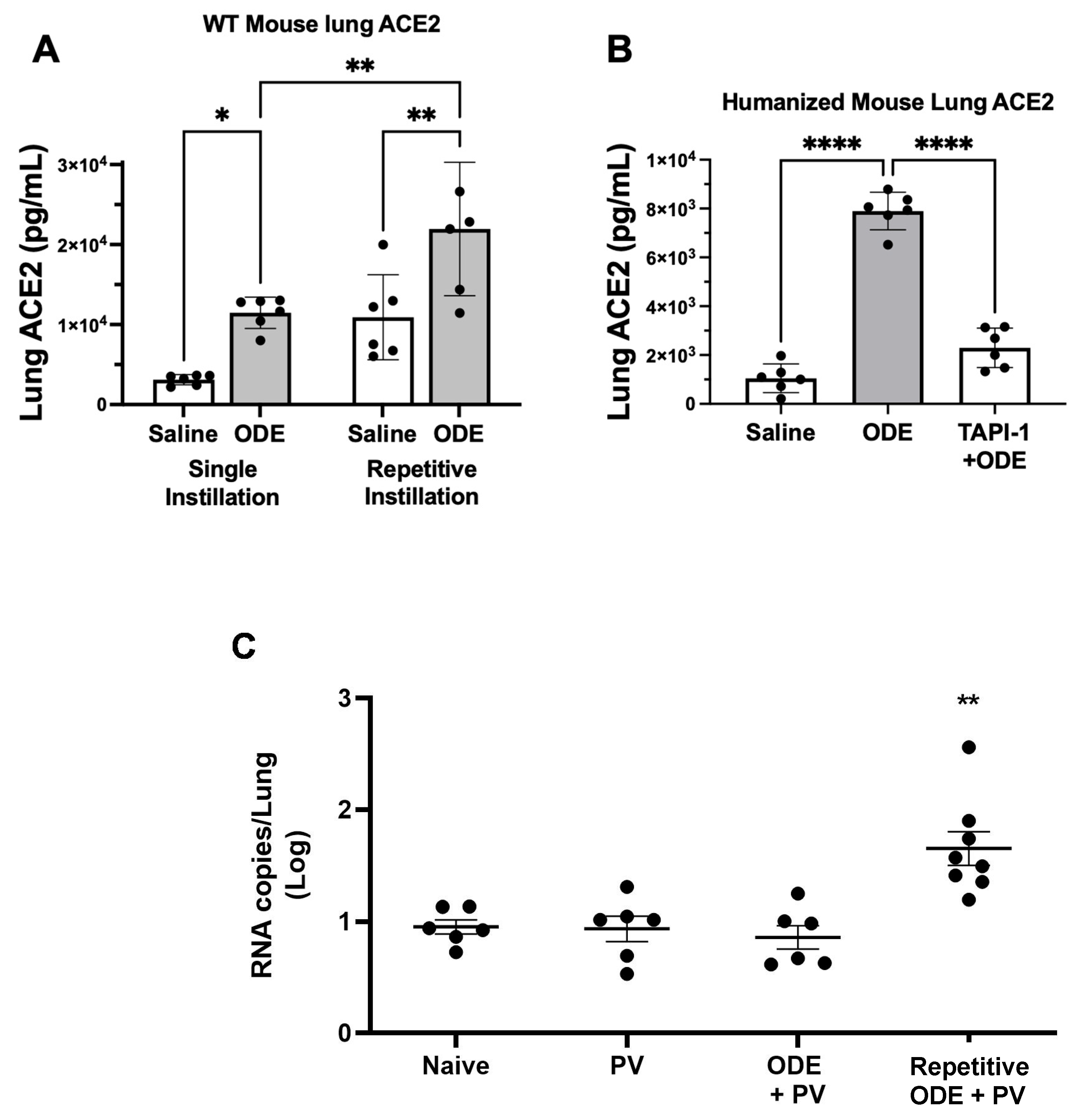
3.1. ODE Single and Repetitive Exposure Increases Murine Lung Soluble ACE2 Levels Dependent upon ADAM-17 with an Associated Effect on SARS-CoV-2 Pseudovirus Infectivity
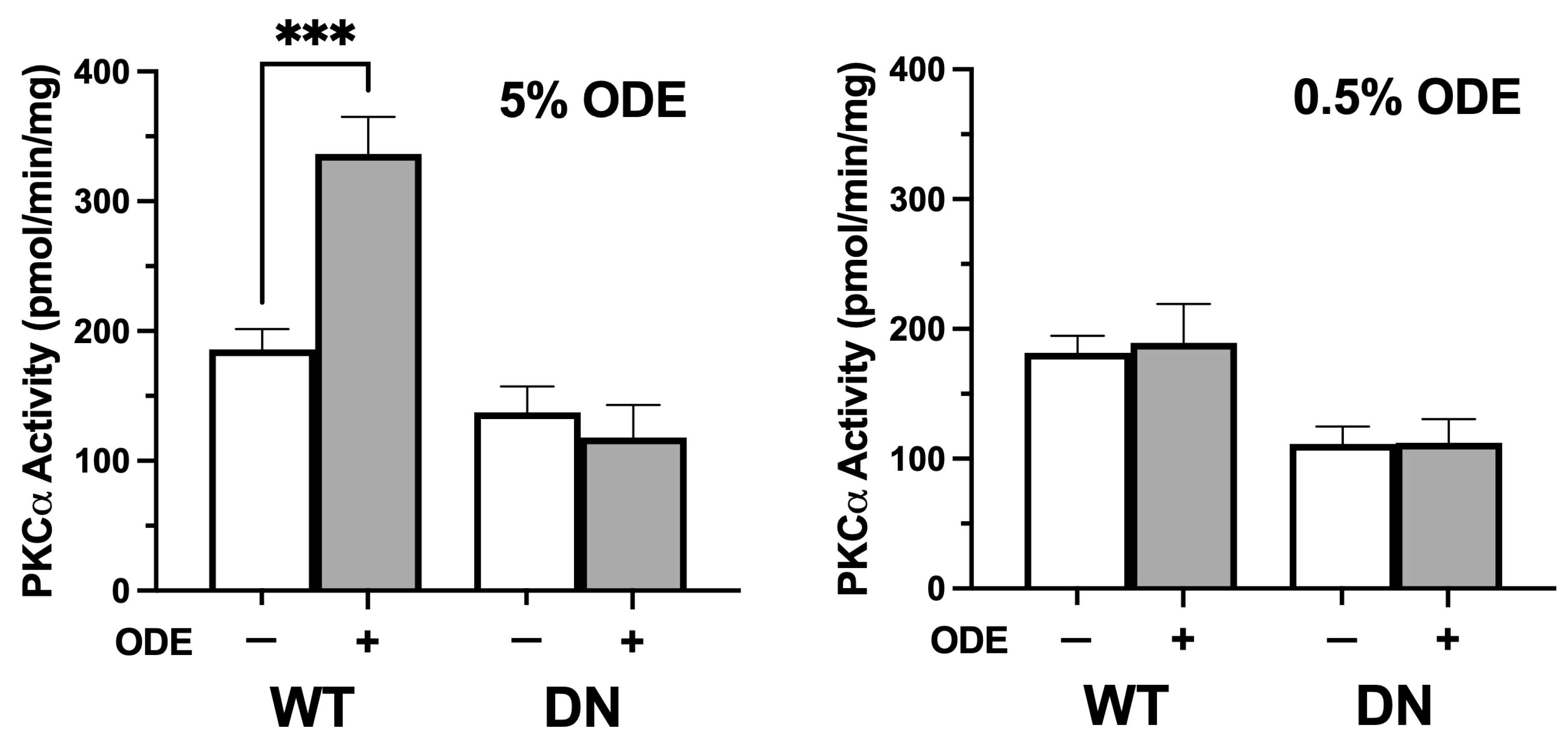
3.2. ODE Treatment Increases Human Bronchial Epithelial Cell PKCα Activity
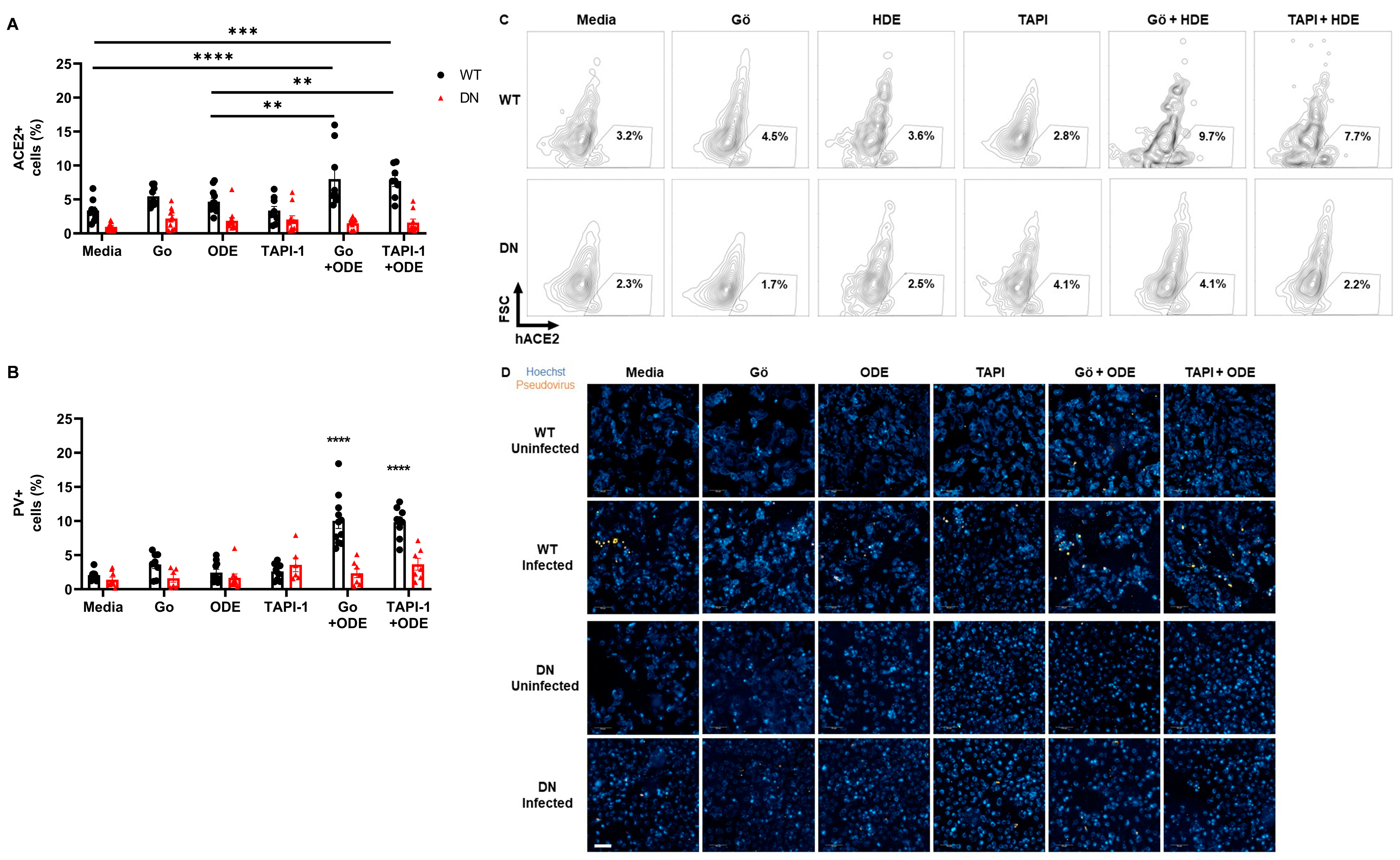
3.3. Inhibition of PKCα and ADAM-17 along with ODE Treatment Synergistically Increases Membrane ACE2 Levels, Enhancing SARS-CoV-2 Pseudovirus Entry in BEAS-2B Cells In Vitro
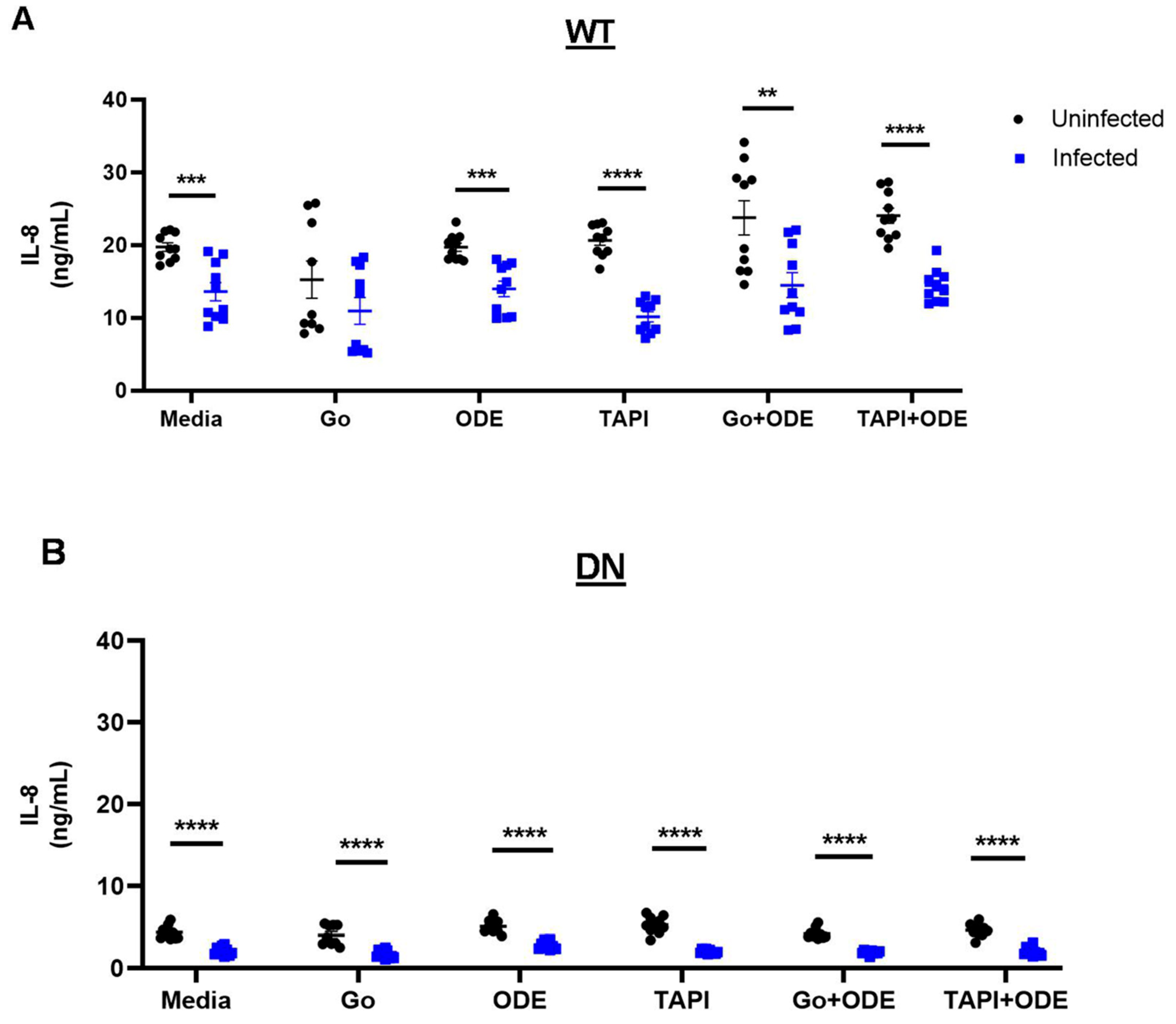
3.4. SARS-CoV-2 Pseudovirus Infection Reduces IL-8 Secretion in a PKCα-Independent Manner in Low-Dose ODE-Treated BEAS-2B Cells
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ganesh, B.; Rajakumar, T.; Malathi, M.; Manikandan, N.; Nagaraj, J.; Santhakumar, A.; Elangovan, A.; Malik, Y.S. Epidemiology and pathobiology of SARS-CoV-2 (COVID-19) in comparison with SARS, MERS: An updated overview of current knowledge and future perspectives. Clin. Epidemiol. Glob. Health 2021, 10, 100694. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Sigsgaard, T.; Basinas, I.; Doekes, G.; de Blay, F.; Folletti, I.; Heederik, D.; Lipinska-Ojrzanowska, A.; Nowak, D.; Olivieri, M.; Quirce, S.; et al. Respiratory diseases and allergy in farmers working with livestock: A EAACI position paper. Clin. Transl. Allergy 2020, 10, 29. [Google Scholar] [CrossRef] [PubMed]
- Bongers, P.; Houthuijs, D.; Remijn, B.; Brouwer, R.; Biersteker, K. Lung function and respiratory symptoms in pig farmers. Br. J. Ind. Med. 1987, 44, 819–823. [Google Scholar] [CrossRef] [PubMed]
- Haglind, P.; Rylander, R. Occupational exposure and lung function measurements among workers in swine confinement buildings. J. Occup. Med. 1987, 29, 904–907. [Google Scholar] [PubMed]
- Holness, D.L.; O’Blenis, E.L.; Sass-Kortsak, A.; Pilger, C.; Nethercott, J.R. Respiratory effects and dust exposures in hog confinement farming. Am. J. Ind. Med. 1987, 11, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Haleem, N.; Osabutey, A.; Cen, Z.; Albert, K.L.; Autenrieth, D. Particulate Matter in Swine Barns: A Comprehensive Review. Atmosphere 2022, 13, 490. [Google Scholar] [CrossRef]
- Warren, K.J.; Dickinson, J.D.; Nelson, A.J.; Wyatt, T.A.; Romberger, D.J.; Poole, J.A. Ovalbumin-sensitized mice have altered airway inflammation to agriculture organic dust. Respir. Res. 2019, 20, 51. [Google Scholar] [CrossRef]
- Wyatt, T.A.; Slager, R.E.; Heires, A.J.; Devasure, J.M.; Vonessen, S.G.; Poole, J.A.; Romberger, D.J. Sequential activation of protein kinase C isoforms by organic dust is mediated by tumor necrosis factor. Am. J. Respir. Cell Mol. Biol. 2010, 42, 706–715. [Google Scholar] [CrossRef]
- Burvall, K.; Palmberg, L.; Larsson, K. Expression of TNFalpha and its receptors R1 and R2 in human alveolar epithelial cells exposed to organic dust and the effects of 8-bromo-cAMP and protein kinase A modulation. Inflamm. Res. 2005, 54, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Bauer, C.; Kielian, T.; Wyatt, T.A.; Romberger, D.J.; West, W.W.; Gleason, A.M.; Poole, J.A. Myeloid differentiation factor 88-dependent signaling is critical for acute organic dust-induced airway inflammation in mice. Am. J. Respir. Cell Mol. Biol. 2013, 48, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Zipeto, D.; Palmeira, J.D.F.; Arganaraz, G.A.; Arganaraz, E.R. ACE2/ADAM17/TMPRSS2 Interplay May Be the Main Risk Factor for COVID-19. Front. Immunol. 2020, 11, 576745. [Google Scholar] [CrossRef] [PubMed]
- Gooz, M. ADAM-17: The enzyme that does it all. Crit. Rev. Biochem. Mol. Biol. 2010, 45, 146–169. [Google Scholar] [CrossRef] [PubMed]
- Hamming, I.; Timens, W.; Bulthuis, M.L.; Lely, A.T.; Navis, G.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, J.H.; Li, W.; Choe, H.; Farzan, M. Angiotensin-converting enzyme 2: A functional receptor for SARS coronavirus. Cell. Mol. Life Sci. 2004, 61, 2738–2743. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, H.; Pohlmann, S. Cellular entry of the SARS coronavirus. Trends Microbiol. 2004, 12, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Boissy, R.J.; Romberger, D.J.; Roughead, W.A.; Weissenburger-Moser, L.; Poole, J.A.; LeVan, T.D. Shotgun pyrosequencing metagenomic analyses of dusts from swine confinement and grain facilities. PLoS ONE 2014, 9, e95578. [Google Scholar] [CrossRef]
- Allen-Gipson, D.S.; Floreani, A.A.; Heires, A.J.; Sanderson, S.D.; MacDonald, R.G.; Wyatt, T.A. Cigarette smoke extract increases C5a receptor expression in human bronchial epithelial cells. J. Pharmacol. Exp. Ther. 2005, 314, 476–482. [Google Scholar] [CrossRef]
- Hahn, D.; Pischitzis, A.; Roesmann, S.; Hansen, M.K.; Leuenberger, B.; Luginbuehl, U.; Sterchi, E.E. Phorbol 12-myristate 13-acetate-induced ectodomain shedding and phosphorylation of the human meprinbeta metalloprotease. J. Biol. Chem. 2003, 278, 42829–42839. [Google Scholar] [CrossRef]
- Lewnard, J.A.; Mora, A.M.; Nkwocha, O.; Kogut, K.; Rauch, S.A.; Morga, N.; Hernandez, S.; Wong, M.P.; Huen, K.; Andrejko, K.; et al. Prevalence and Clinical Profile of Severe Acute Respiratory Syndrome Coronavirus 2 Infection among Farmworkers, California, USA, June–November 2020. Emerg. Infect. Dis. 2021, 27, 1330–1342. [Google Scholar] [CrossRef] [PubMed]
- Mora, A.M.; Lewnard, J.A.; Kogut, K.; Rauch, S.A.; Hernandez, S.; Wong, M.P.; Huen, K.; Chang, C.; Jewell, N.P.; Holland, N.; et al. Risk Factors Associated with SARS-CoV-2 Infection Among Farmworkers in Monterey County, California. JAMA Netw. Open 2021, 4, e2124116. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, C.; Lesteberg, K.E.; Lamb, M.M.; Calvimontes, D.M.; Guo, K.; Barrett, B.S.; Mickens, K.L.; Duca, L.M.; Monzon, J.; Chard, A.N.; et al. High SARS-CoV-2 Seroprevalence and Rapid Neutralizing Antibody Decline among Agricultural Workers in Rural Guatemala, June 2020–March 2021. Vaccines 2022, 10, 1160. [Google Scholar] [CrossRef] [PubMed]
- Wunschel, J.; Poole, J.A. Occupational agriculture organic dust exposure and its relationship to asthma and airway inflammation in adults. J. Asthma 2016, 53, 471–477. [Google Scholar] [CrossRef]
- Poole, J.A.; Wyatt, T.A.; Oldenburg, P.J.; Elliott, M.K.; West, W.W.; Sisson, J.H.; Von Essen, S.G.; Romberger, D.J. Intranasal organic dust exposure-induced airway adaptation response marked by persistent lung inflammation and pathology in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2009, 296, L1085–L1095. [Google Scholar] [CrossRef] [PubMed]
- Yeung, M.L.; Teng, J.L.L.; Jia, L.; Zhang, C.; Huang, C.; Cai, J.P.; Zhou, R.; Chan, K.H.; Zhao, H.; Zhu, L.; et al. Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin-angiotensin system. Cell 2021, 184, 2212–2228.e12. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Yan, Y.; Shu, Y.; Gao, R.; Sun, Y.; Li, X.; Ju, X.; Liang, Z.; Liu, Q.; Zhao, Y.; et al. Angiotensin-converting enzyme 2 protects from lethal avian influenza A H5N1 infections. Nat. Commun. 2014, 5, 3594. [Google Scholar] [CrossRef] [PubMed]
- Gu, H.; Xie, Z.; Li, T.; Zhang, S.; Lai, C.; Zhu, P.; Wang, K.; Han, L.; Duan, Y.; Zhao, Z.; et al. Angiotensin-converting enzyme 2 inhibits lung injury induced by respiratory syncytial virus. Sci. Rep. 2016, 6, 19840. [Google Scholar] [CrossRef] [PubMed]
- Gheblawi, M.; Wang, K.; Viveiros, A.; Nguyen, Q.; Zhong, J.C.; Turner, A.J.; Raizada, M.K.; Grant, M.B.; Oudit, G.Y. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ. Res. 2020, 126, 1456–1474. [Google Scholar] [CrossRef]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef]
- Gemmati, D.; Bramanti, B.; Serino, M.L.; Secchiero, P.; Zauli, G.; Tisato, V. COVID-19 and Individual Genetic Susceptibility/Receptivity: Role of ACE1/ACE2 Genes, Immunity, Inflammation and Coagulation. Might the Double X-chromosome in Females Be Protective against SARS-CoV-2 Compared to the Single X-Chromosome in Males? Int. J. Mol. Sci. 2020, 21, 3474. [Google Scholar] [CrossRef] [PubMed]
- Kuba, K.; Imai, Y.; Ohto-Nakanishi, T.; Penninger, J.M. Trilogy of ACE2: A peptidase in the renin-angiotensin system, a SARS receptor, and a partner for amino acid transporters. Pharmacol. Ther. 2010, 128, 119–128. [Google Scholar] [CrossRef]
- Kuba, K.; Imai, Y.; Rao, S.; Gao, H.; Guo, F.; Guan, B.; Huan, Y.; Yang, P.; Zhang, Y.; Deng, W.; et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005, 11, 875–879. [Google Scholar] [CrossRef] [PubMed]
- Zhong, J.; Basu, R.; Guo, D.; Chow, F.L.; Byrns, S.; Schuster, M.; Loibner, H.; Wang, X.H.; Penninger, J.M.; Kassiri, Z.; et al. Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation 2010, 122, 717–728. [Google Scholar] [CrossRef]
- Patel, V.B.; Zhong, J.C.; Grant, M.B.; Oudit, G.Y. Role of the ACE2/Angiotensin 1-7 Axis of the Renin-Angiotensin System in Heart Failure. Circ. Res. 2016, 118, 1313–1326. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Gheblawi, M.; Oudit, G.Y. Angiotensin Converting Enzyme 2: A Double-Edged Sword. Circulation 2020, 142, 426–428. [Google Scholar] [CrossRef]
- Larsson, B.M.; Palmberg, L.; Malmberg, P.O.; Larsson, K. Effect of exposure to swine dust on levels of IL-8 in airway lavage fluid. Thorax 1997, 52, 638–642. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muralidharan, A.; Bauer, C.D.; Nissen, C.G.; Reid, S.P.; Poole, J.A.; Wyatt, T.A. Organic Dust Exposure Enhances SARS-CoV-2 Entry in a PKCα- and ADAM-17-Dependent Manner. Int. J. Transl. Med. 2024, 4, 486-497. https://doi.org/10.3390/ijtm4030032
Muralidharan A, Bauer CD, Nissen CG, Reid SP, Poole JA, Wyatt TA. Organic Dust Exposure Enhances SARS-CoV-2 Entry in a PKCα- and ADAM-17-Dependent Manner. International Journal of Translational Medicine. 2024; 4(3):486-497. https://doi.org/10.3390/ijtm4030032
Chicago/Turabian StyleMuralidharan, Abenaya, Christopher D. Bauer, Claire G. Nissen, St Patrick Reid, Jill A. Poole, and Todd A. Wyatt. 2024. "Organic Dust Exposure Enhances SARS-CoV-2 Entry in a PKCα- and ADAM-17-Dependent Manner" International Journal of Translational Medicine 4, no. 3: 486-497. https://doi.org/10.3390/ijtm4030032
APA StyleMuralidharan, A., Bauer, C. D., Nissen, C. G., Reid, S. P., Poole, J. A., & Wyatt, T. A. (2024). Organic Dust Exposure Enhances SARS-CoV-2 Entry in a PKCα- and ADAM-17-Dependent Manner. International Journal of Translational Medicine, 4(3), 486-497. https://doi.org/10.3390/ijtm4030032






