Substance Delivery across the Blood-Brain Barrier or the Blood-Retinal Barrier Using Organic Cation Transporter Novel Type 2 (OCTN2)
Abstract
:1. Introduction
2. Discussion
2.1. Transporters
2.2. Carrier-Mediated Transport Using OCTN2
2.3. OCTN2-Mediated Endocytosis/Transcytosis
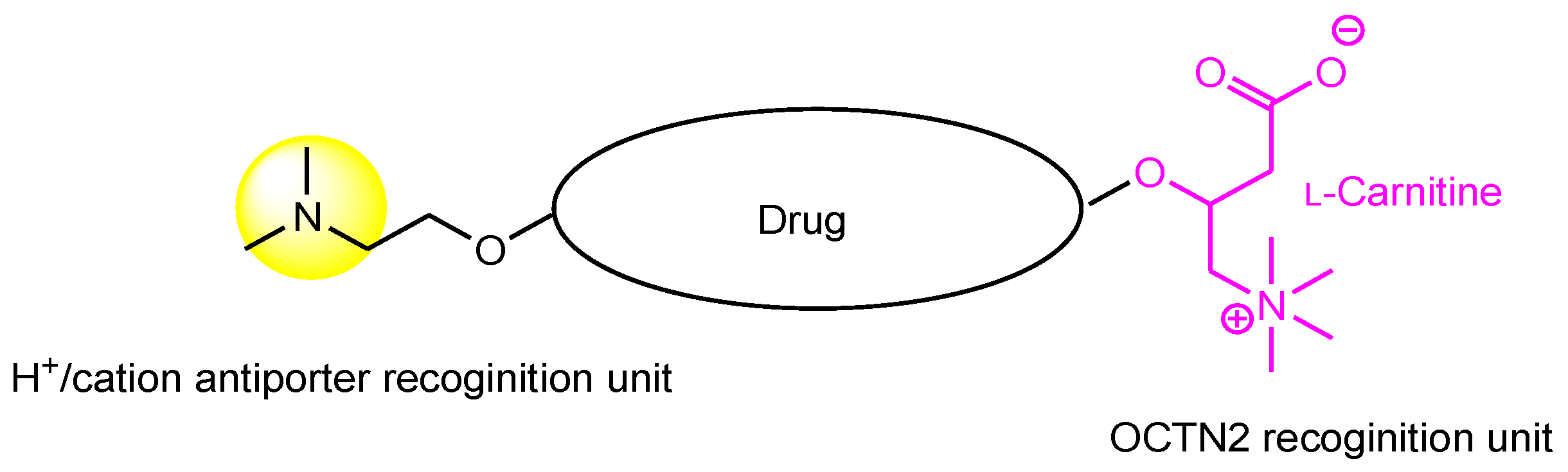
2.4. A Promising Method for Delivering Substances into the Brain across the BBB
2.5. Possibilities of Carrier-Mediated Transport into the Eyes Using OCTN2
3. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stimulus package. Nat. Med. 2018, 24, 247. [CrossRef] [PubMed]
- Pardridge, W.M. Blood-Brain Barrier and Delivery of Protein and Gene Therapeutics to Brain. Front. Aging Neurosci. 2020, 11, 373. [Google Scholar] [CrossRef] [PubMed]
- van Dyck, C.H.; Swanson, C.J.; Aisen, P.; Bateman, R.J.; Chen, C.; Gee, M.; Kanekiyo, M.; Li, D.; Reyderman, L.; Cohen, S.; et al. Lecanemab in Early Alzheimer’s Disease. N. Engl. J. Med. 2023, 388, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Rashad, A.; Rasool, A.; Shaheryar, M.; Sarfraz, A.; Sarfraz, Z.; Robles-Velasco, K.; Cherrez-Ojeda, I. Donanemab for Alzheimer’s Disease: A Systematic Review of Clinical Trials. Healthcare 2023, 11, 32. [Google Scholar] [CrossRef] [PubMed]
- Sousa, J.A.; Bernardes, C.; Bernardo-Castro, S.; Lino, M.; Albino, I.; Ferreira, L.; Brás, J.; Guerreiro, R.; Tábuas-Pereira, M.; Baldeiras, I.; et al. Reconsidering the role of blood-brain barrier in Alzheimer’s disease: From delivery to target. Front. Aging Neurosci. 2023, 15, 1102809. [Google Scholar] [CrossRef] [PubMed]
- Kadry, H.; Noorani, B.; Cucullo, L. A blood-brain barrier overview on structure, function, impairment, and biomarkers of integrity. Fluids Barriers CNS 2020, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, C.D.; D’Aquili, E.G. Biogenetic Structuralism; Columbia University Press: New York, NY, USA, 1974. [Google Scholar]
- Leavy, S.A. Biogenetic Structuralism. Yale J. Biol. Med. 1976, 49, 420–421. [Google Scholar]
- Tashima, T. Smart Strategies for Therapeutic Agent Delivery into Brain across the Blood-Brain Barrier Using Receptor-Mediated Transcytosis. Chem. Pharm. Bull. 2020, 68, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Betterton, R.D.; Davis, T.P.; Ronaldson, P.T. Organic Cation Transporter (OCT/OCTN) Expression at Brain Barrier Sites: Focus on CNS Drug Delivery. Handb. Exp. Pharmacol. 2021, 266, 301–328. [Google Scholar] [CrossRef]
- Kurosawa, T.; Tega, Y.; Uchida, Y.; Higuchi, K.; Tabata, H.; Sumiyoshi, T.; Kubo, Y.; Terasaki, T.; Deguchi, Y. Proteomics-Based Transporter Identification by the PICK Method: Involvement of TM7SF3 and LHFPL6 in Proton-Coupled Organic Cation Antiport at the Blood–Brain Barrier. Pharmaceutics 2022, 14, 1683. [Google Scholar] [CrossRef]
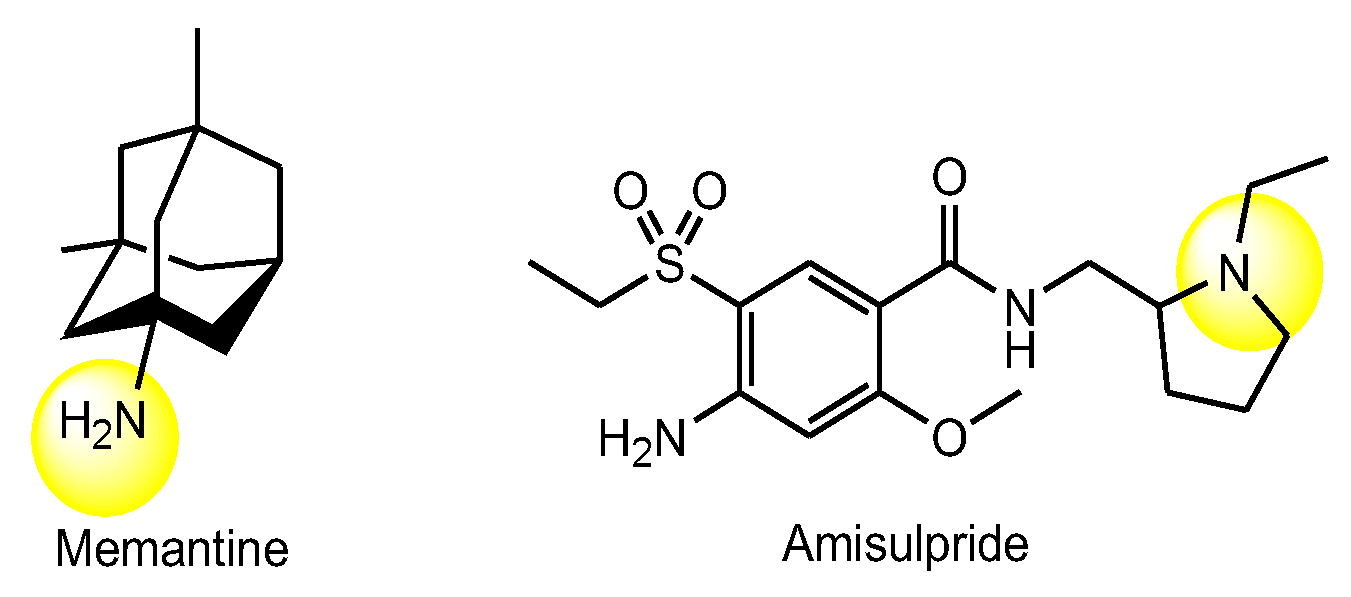
- Tega, Y.; Tabata, H.; Kurosawa, T.; Kitamura, A.; Itagaki, F.; Oshitari, T.; Deguchi, Y. Structural Requirements for Uptake of Diphenhydramine Analogs into hCMEC/D3 Cells Via the Proton-Coupled Organic Cation Antiporter. J. Pharm. Sci. 2021, 110, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Sekhar, G.N.; Fleckney, A.L.; Boyanova, S.T.; Rupawala, H.; Lo, R.; Wang, H.; Farag, D.B.; Rahman, K.M.; Broadstock, M.; Reeves, S.; et al. Region-specific blood–brain barrier transporter changes leads to increased sensitivity to amisulpride in Alzheimer’s disease. Fluids Barriers CNS 2019, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- Tashima, T. Intriguing possibilities and beneficial aspects of transporter-conscious drug design. Bioorg. Med. Chem. 2015, 23, 4119–4131. [Google Scholar] [CrossRef] [PubMed]
- Tashima, T. Carrier-Mediated Delivery of Low-Molecular-Weight N-Containing Drugs across the Blood–Brain Barrier or the Blood–Retinal Barrier Using the Proton-Coupled Organic Cation Antiporter. Future Pharmacol. 2023, 3, 742–762. [Google Scholar] [CrossRef]
- Xu, S.; Flanagan, J.L.; Simmons, P.A.; Vehige, J.; Willcox, M.D.; Garrett, Q. Transport of L-carnitine in human corneal and conjunctival epithelial cells. Mol. Vis. 2010, 16, 1823–1831. [Google Scholar]
- Tachikawa, M.; Takeda, Y.; Tomi, M.; Hosoya, K. Involvement of OCTN2 in the Transport of Acetyl-L-Carnitine across the Inner Blood–Retinal Barrie. Investig. Ophthalmol. Vis. Sci. 2010, 51, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Zamek-Gliszczynski, M.J.; Taub, M.E.; Chothe, P.P.; Chu, X.; Giacomini, K.M.; Kim, R.B.; Ray, A.S.; Stocker, S.L.; Unadkat, J.D.; Wittwer, M.B.; et al. Transporters in Drug Development: 2018 ITC Recommendations for Transporters of Emerging Clinical Importance. Clin. Pharmacol. Ther. 2018, 104, 890–899. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Sun, K.; Meng, Z.; Chen, L. The SLC transporter in nutrient and metabolic sensing, regulation, and drug development. J. Mol. Cell Biol. 2019, 11, 1–13. [Google Scholar] [CrossRef]
- Dean, M.; Rzhetsky, A.; Allikmets, R. The Human ATP-Binding Cassette (ABC) Transporter Superfamily. Genome Res. 2001, 11, 1156–1166. [Google Scholar] [CrossRef]
- Jaramillo, A.C.; Saig, F.A.; Cloos, J.; Jansen, G.; Peters, G.J. How to overcome ATP-binding cassette drug efflux transporter-mediated drug resistance? Cancer Drug Resist. 2018, 1, 6. [Google Scholar] [CrossRef]
- Mehta, D.C.; Short, J.L.; Nicolazzo, J.A. Memantine transport across the mouse blood-brain barrier is mediated by a cationic influx H+ antiporter. Mol. Pharm. 2013, 10, 4491–4498. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.G. The Structure and Mechanism of Drug Transporters. Methods Mol. Biol. 2021, 2342, 193–234. [Google Scholar] [CrossRef] [PubMed]
- Christianson, H.C.; Belting, M. Heparan sulfate proteoglycan as a cell-surface endocytosis receptor. Matrix Biol. 2014, 35, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Tamai, I. Pharmacological and pathophysiological roles of carnitine/organic cation transporters (OCTNs: SLC22A4, SLC22A5 and Slc22a21). Biopharm. Drug Dispos. 2013, 34, 29–44. [Google Scholar] [CrossRef] [PubMed]
- Inano, A.; Sai, Y.; Kato, Y.; Tamai, I.; Ishiguro, M.; Tsuji, A. Functional regions of organic cation/carnitine transporter OCTN2 (SLC22A5): Roles in carnitine recognition. Drug Metab. Pharmacokin. 2004, 19, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Pereira, J.N.; Tadjerpisheh, S.; Abu Abed, M.; Saadatmand, A.R.; Weksler, B.; Romero, I.A.; Couraud, P.O.; Brockmöller, J.; Tzvetkov, M.V. The Poorly Membrane Permeable Antipsychotic Drugs Amisulpride and Sulpiride Are Substrates of the Organic Cation Transporters from the SLC22 Family. AAPS J. 2014, 16, 1247–1258. [Google Scholar] [CrossRef] [PubMed]
- Shimomura, K.; Okura, T.; Kato, S.; Couraud, P.-O.; Schermann, J.-M.; Terasaki, T.; Deguchi, Y. Functional expression of a proton-coupled organic cation (H+/OC) antiporter in human brain capillary endothelial cell line hCMEC/D3, a human blood–brain barrier model. Fluids Barriers CNS 2013, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Indiveri, C.; Pochini, L.; Oppedisano, F.; Tonazzi, A. The Carnitine Transporter Network: Interactions with Drugs. Curr. Chem. Biol. 2010, 4, 108–123. [Google Scholar]
- Ekins, S.; Diao, L.; Polli, J.E. A Substrate Pharmacophore for the Human Organic Cation/Carnitine Transporter Identi-fies Compounds Associated with Rhabdomyolysis. Mol. Pharm. 2012, 9, 905–913. [Google Scholar] [CrossRef]
- Kato, Y.; Sugiura, M.; Sugiura, T.; Wakayama, T.; Kubo, Y.; Kobayashi, D.; Sai, Y.; Tamai, I.; Iseki, S.; Tsuji, A. Organic cation/carnitine transporter OCTN2 (Slc22a5) is responsible for carnitine transport across apical membranes of small intestinal epithelial cells in mouse. Mol. Pharmacol. 2006, 70, 829–837. [Google Scholar] [CrossRef]
- Grube, M.; Meyer zu Schwabedissen, H.E.; Präger, D.; Haney, J.; Möritz, K.U.; Meissner, K.; Rosskopf, D.; Eckel, L.; Böhm, M.; Jedlitschky, G.; et al. Uptake of cardiovascular drugs into the human heart: Expression, regulation, and function of the carnitine transporter OCTN2 (SLC22A5). Circulation 2006, 113, 1114–1122. [Google Scholar] [CrossRef]
- Juraszek, B.; Nałęcz, K.A. SLC22A5 (OCTN2) Carnitine Transporter-Indispensable for Cell Metabolism, a Jekyll and Hyde of Human Cancer. Molecules 2020, 25, 14. [Google Scholar] [CrossRef] [PubMed]
- Visentin, M.; Gai, Z.; Torozi, A.; Hiller, C.; Kullak-Ublick, G.A. Colistin is Substrate of the Carnitine/Organic Cation Transporter 2 (OCTN2, SLC22A5). Drug Metab. Dispos. 2017, 45, 1240–1244. [Google Scholar] [CrossRef]
- Salomon, J.J.; Gausterer, J.C.; Selo, M.A.; Hosoya, K.-i.; Huwer, H.; Schneider-Daum, N.; Lehr, C.-M.; Ehrhardt, C. OCTN2-Mediated Acetyl-l-Carnitine Transport in Human Pulmonary Epithelial Cells In Vitro. Pharmaceutics 2019, 11, 396. [Google Scholar] [CrossRef]
- Wang, G.; Zhao, L.; Jiang, Q.; Sun, Y.; Zhao, D.; Sun, M.; He, Z.; Sun, J.; Wang, Y. Intestinal OCTN2- and MCT1-targeted drug delivery to improve oral bioavailability. Asian J. Pharm. Sci. 2020, 15, 158–172. [Google Scholar] [CrossRef] [PubMed]
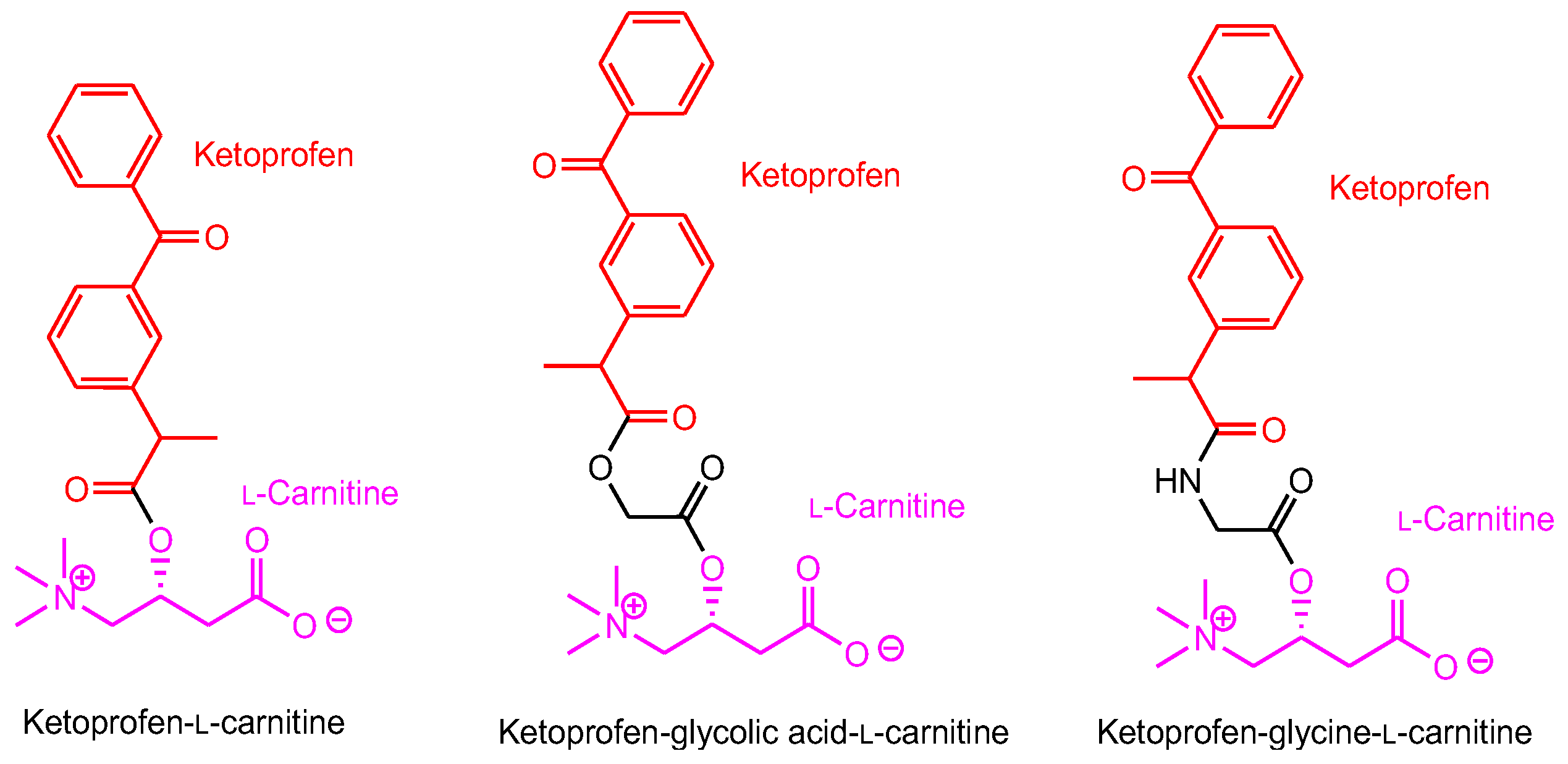
- Diao, L.; Polli, J.E. Synthesis and in vitro characterization of drug conjugates of l-carnitine as potential prodrugs that target human Octn2. J. Pharm. Sci. 2011, 100, 3802–3816. [Google Scholar] [CrossRef]
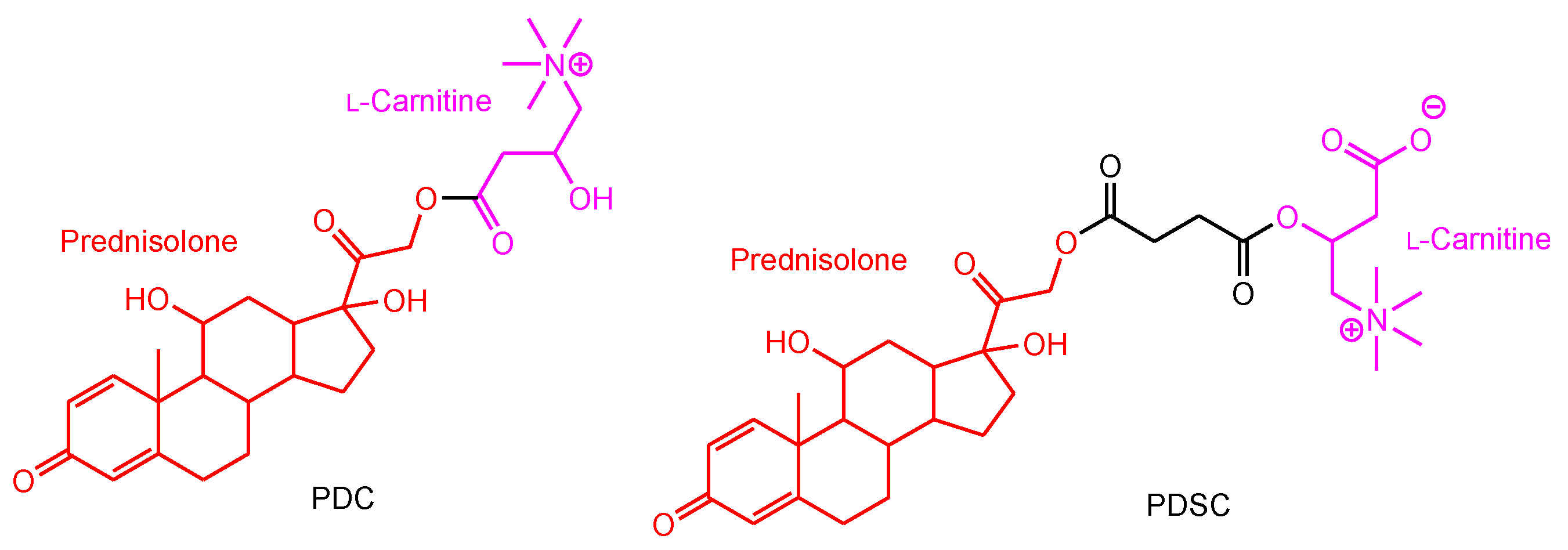
- Mo, J.X.; Shi, S.J.; Zhang, Q.; Gong, T.; Sun, X.; Zhang, Z.R. Synthesis, transport and mechanism of a type I prodrug: L-carnitine ester of prednisolone. Mol. Pharm. 2011, 8, 1629–1640. [Google Scholar] [CrossRef]
- Gyimesi, G.; Hediger, M.A. Transporter-Mediated Drug Delivery. Molecules 2023, 28, 1151. [Google Scholar] [CrossRef]
- Kou, L.; Sun, R.; Xiao, S.; Cui, X.; Sun, J.; Ganapathy, V.; Yao, Q.; Chen, R. OCTN2-targeted nanoparticles for oral delivery of paclitaxel: Differential impact of the polyethylene glycol linker size on drug delivery in vitro, in situ, and in vivo. Drug Deliv. 2020, 27, 170–179. [Google Scholar] [CrossRef]
- Kou, L.; Yao, Q.; Sun, M.; Wu, C.; Wang, J.; Luo, Q.; Wang, G.; Du, Y.; Fu, Q.; Wang, J.; et al. Cotransporting Ion is a Trigger for Cellular Endocytosis of Transporter-Targeting Nanoparticles: A Case Study of High-Efficiency SLC22A5 (OCTN2)-Mediated Carnitine-Conjugated Nanoparticles for Oral Delivery of Therapeutic Drugs. Adv. Healthc. Mater. 2017, 6, 1700165. [Google Scholar] [CrossRef]
- Kou, L.; Yao, Q.; Sivaprakasam, S.; Luo, Q.; Sun, Y.; Fu, Q.; He, Z.; Sun, J.; Ganapathy, V. Dual targeting of l-carnitine-conjugated nanoparticles to OCTN2 and ATB0,+ to deliver chemotherapeutic agents for colon cancer therapy. Drug Deliv. 2017, 24, 1338–1349. [Google Scholar] [CrossRef] [PubMed]
- Andreana, I.; Malatesta, M.; Lacavalla, M.A.; Boschi, F.; Milla, P.; Bincoletto, V.; Pellicciari, C.; Arpicco, S.; Stella, B. L-Carnitine Functionalization to Increase Skeletal Muscle Tropism of PLGA Nanoparticles. Int. J. Mol. Sci. 2023, 24, 294. [Google Scholar] [CrossRef]
- Kou, L.; Hou, Y.; Yao, Q.; Guo, W.; Wang, G.; Wang, M.; Fu, Q.; He, Z.; Ganapathy, V.; Sun, J. L-Carnitine-conjugated nanoparticles to promote permeation across blood-brain barrier and to target glioma cells for drug delivery via the novel organic cation/carnitine transporter OCTN2. Artif. Cells Nanomed. Biotechnol. 2018, 46, 1605–1616. [Google Scholar] [CrossRef]
- Walle, U.K.; Walle, T. Taxol transport by human intestinal epithelial Caco-2 cells. Drug Metab. Dispos. 1998, 26, 343–346. [Google Scholar]
- Jang, S.H.; Wientjes, M.G.; Au, J.L. Kinetics of P-glycoprotein-mediated efflux of paclitaxel. J. Pharmacol. Exp. Ther. 2001, 298, 1236–1242. [Google Scholar] [PubMed]
- Fink, M.A.; Paland, H.; Herzog, S.; Grube, M.; Vogelgesang, S.; Weitmann, K.; Bialke, A.; Hoffmann, W.; Rauch, B.H.; Schroeder, H.W.S.; et al. L-Carnitine–Mediated Tumor Cell Protection and Poor Patient Survival Associated with OCTN2 Overexpression in Glioblastoma Multiforme. Clin. Cancer Res. 2019, 25, 2874–2886. [Google Scholar] [CrossRef]
- Fukumura, M.; Nonoguchi, N.; Kawabata, S.; Hiramatsu, R.; Futamura, G.; Takeuchi, K.; Kanemitsu, T.; Takata, T.; Tanaka, H.; Suzuki, M.; et al. 5-Aminolevulinic acid increases boronophenylalanine uptake into glioma stem cells and may sensitize malignant glioma to boron neutron capture therapy. Sci. Rep. 2023, 13, 10173. [Google Scholar] [CrossRef]
- Liu, A.P.; Aguet, F.; Danuser, G.; Schmid, S.L. Local clustering of transferrin receptors promotes clathrin-coated pit initiation. J. Cell Biol. 2010, 191, 1381–1393. [Google Scholar] [CrossRef]
- Cureton, D.K.; Harbison, C.E.; Cocucci, E.; Parrish, C.R.; Kirchhausen, T. Limited transferrin receptor clustering allows rapid diffusion of canine parvovirus into clathrin endocytic structures. J. Virol. 2012, 86, 5330–5340. [Google Scholar] [CrossRef]
- Kibbey, R.G.; Rizo, J.; Gierasch, L.M.; Anderson, R.G. The LDL Receptor Clustering Motif Interacts with the Clathrin Terminal Domain in a Reverse Turn Conformation. J. Cell Biol. 1998, 142, 59–67. [Google Scholar] [CrossRef]
- Sousa de Almeida, M.; Susnik, E.; Drasler, B.; Taladriz-Blanco, P.; Petri-Fink, A.; Rothen-Rutishauser, B. Understanding nanoparticle endocytosis to improve targeting strategies in nanomedicine. Chem. Soc. Rev. 2021, 50, 5397–5434. [Google Scholar] [CrossRef] [PubMed]
- Oh, N.; Park, J.H. Endocytosis and exocytosis of nanoparticles in mammalian cells. Int. J. Nanomed. 2014, 9 (Suppl. S1), 51–63. [Google Scholar] [CrossRef]
- Pochini, L.; Galluccio, M.; Scalise, M.; Console, L.; Indiveri, C. OCTN: A Small Transporter Subfamily with Great Relevance to Human Pathophysiology, Drug Discovery, and Diagnostics. SLAS Discov. 2019, 24, 89–110. [Google Scholar] [CrossRef] [PubMed]
- Adeva-Andany, M.M.; Calvo-Castro, I.; Fernández-Fernández, C.; Donapetry-García, C.; Pedre-Piñeiro, A.M. Significance of L-Carnitine for Human Health. IUBMB Life 2017, 69, 578–594. [Google Scholar] [CrossRef] [PubMed]
- Tamai, I.; China, K.; Sai, Y.; Kobayashi, D.; Nezu, J.; Kawahara, E.; Tsuji, A. Na(+)-coupled transport of L-carnitine via high-affinity carnitine transporter OCTN2 and its subcellular localization in kidney. Biochim. Biophys. Acta 2001, 1512, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Iwata, D.; Kato, Y.; Wakayama, T.; Sai, Y.; Kubo, Y.; Iseki, S.; Tsuji, A. Involvement of carnitine/organic cation transporter OCTN2 (SLC22A5) in distribution of its substrate carnitine to the heart. Drug Metab. Pharmacokinet. 2008, 23, 207–215. [Google Scholar] [CrossRef]
- Kimura, Y.; Morita, S.; Matsuo, M.; Ueda, K. Mechanism of multidrug recognition by MDR1/ABCB1. Cancer Sci. 2007, 98, 1303–1310. [Google Scholar]
- Famta, P.; Shah, S.; Chatterjee, E.; Singh, H.; Dey, B.; Guru, S.K.; Singh, S.B.; Srivastava, S. Exploring new Horizons in overcoming P-glycoprotein-mediated multi-drug-resistant breast cancer via nanoscale drug delivery platforms. Curr. Res. Pharmacol. Drug Discov. 2021, 2, 100054. [Google Scholar] [CrossRef]
- Koleske, M.L.; McInnes, G.; Brown, J.E.H.; Thomas, N.; Hutchinson, K.; Chin, M.Y.; Koehl, A.; Arkin, M.R.; Schlessinger, A.; Gallagher, R.C.; et al. Functional genomics of OCTN2 variants informs protein-specific variant effect predictor for Carnitine Transporter Deficiency. Proc. Natl. Acad. Sci. USA 2022, 119, e2210247119. [Google Scholar] [CrossRef]
- Yokogawa, K.; Higashi, Y.; Tamai, T.; Nornura, M.; Hashirnoto, N.; Nikaido, H.; Hayakawa, J.; Miyarnoto, K.; Tsuji, A. Decreased tissue distribution of L-carnitine in juvenile visceral steatosis mice. J. Pharmacol. Exp. Ther. 1999, 289, 224–230. [Google Scholar]
- Chen, Y.; Liu, L. Modern methods for delivery of drugs across the blood–brain barrier. Adv. Drug Deliv. Rev. 2012, 64, 640–665. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, F.; Campbell, M. The blood–retina barrier in health and disease. FEBS J. 2023, 290, 878–891. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Coránguez, M.; Ramos, C.; Antonetti, D.A. The inner blood-retinal barrier: Cellu-lar basis and development. Vis. Res. 2017, 139, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Tashima, T. Ocular Drug Delivery into the Eyes Using Drug-Releasing Soft Contact Lens. Future Pharmacol. 2024, 4, 336–351. [Google Scholar] [CrossRef]
- Pray, L. Eukaryotic genome complexity. Nat. Educ. 2008, 1, 96. Available online: https://www.nature.com/scitable/topicpage/eukaryotic-genome-complexity-437/ (accessed on 1 March 2024).
- Lu, C.; Xing, Y.; Cai, H.; Shi, Y.; Liu, J.; Huang, Y. Identification and analysis of long non-coding RNAs in response to H5N1 influenza viruses in duck (Anas platyrhynchos). BMC Genom. 2019, 20, 36. [Google Scholar] [CrossRef]



| # | Compounds | Disease | OCTN2 Substrate | Cargo | Linker between Cargo and Carrier | Uptake Mechanism | Status | References |
|---|---|---|---|---|---|---|---|---|
| 1 | Conjugates of L-carnitine and gemcitabine | Cancer | L-Carnitine | Gemcitabine | Cleavable alkyl chain | Carrier-mediated transport | Basic research | [36], [Figure 4] |
| 2 | Conjugates of L-carnitine and ketoprofen | Inflammation | L-Carnitine | Ketoprofen | Cleavable alkyl chain | Carrier-mediated transport | Basic research | [37], [Figure 5] |
| 3 | Conjugates of L-carnitine and prednisolone | Asthma | L-Carnitine | Prednisolone | Cleavable alkyl chain | Carrier-mediated transport | Basic research | [38], [Figure 6] |
| 4 | Paclitaxel-encapsulated poly(lactic-co-glycolic acid) nanoparticles (PLGA NPs) conjugated to L-carnitine | Cancer | L-Carnitine | Paclitaxel | Non-covalent bond | Receptor-mediated endocytosis | Basic research | [40] |
| 5 | Paclitaxel-encapsulated LC-PLGA NPs conjugated to L-carnitine | Cancer | L-Carnitine | Paclitaxel | Non-covalent bond | Receptor-mediated endocytosis | Basic research | [41] |
| 6 | 5-FU-encapsulatied PLGA NPs conjugated to L-carnitine | Colon cancer | L-Carnitine and ATB0,+ | 5-FU | Non-covalent bond | [42] | ||
| 7 | Stearoyl-L-carnitine conjugated poly(lactic-co-glycolic acid) nanoparticles (SC-LC-PLGA NPs) | Muscular dystrophies | L-Carnitine | - | Non-covalent bond | Receptor-mediated endocytosis | Basic research | [43] |
| 8 | Paclitaxel-encapsulated PLGA NPs conjugated to L-carnitine | Glioma | L-Carnitine | Paclitaxel | Non-covalent bond | Receptor-mediated endocytosis | Basic research | [44] |
| 9 | Conjugates of L-carnitine and CNS drug | CNS disease | L-Carnitine | CNS drug | Cleavable alkyl chain | Carrier-mediated transport | Under analysis in Tashima lab | [Figure 7] |
| 10 | Conjugates of L-carnitine and CNS drug | CNS disease | N-containing group | CNS drug | Cleavable alkyl chain/non-Cleavable alkyl chain | Carrier-mediated transport | Under analysis in Tashima lab | - |
| 11 | CNS drug-encapsulated nanoparticle conjugated to L-carnitine | CNS disease | L-Carnitine | CNS drug | Non-covalent bond | Receptor-mediated endocytosis | Under analysis in Tashima lab | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tashima, T. Substance Delivery across the Blood-Brain Barrier or the Blood-Retinal Barrier Using Organic Cation Transporter Novel Type 2 (OCTN2). Future Pharmacol. 2024, 4, 479-493. https://doi.org/10.3390/futurepharmacol4030027
Tashima T. Substance Delivery across the Blood-Brain Barrier or the Blood-Retinal Barrier Using Organic Cation Transporter Novel Type 2 (OCTN2). Future Pharmacology. 2024; 4(3):479-493. https://doi.org/10.3390/futurepharmacol4030027
Chicago/Turabian StyleTashima, Toshihiko. 2024. "Substance Delivery across the Blood-Brain Barrier or the Blood-Retinal Barrier Using Organic Cation Transporter Novel Type 2 (OCTN2)" Future Pharmacology 4, no. 3: 479-493. https://doi.org/10.3390/futurepharmacol4030027





