1. Introduction
Research on the use and adverse outcomes of opioids is an emerging theme in developed countries [
1,
2,
3,
4,
5,
6,
7]. Surgical and trauma patients have been a focal point in international studies on opioid use, mostly from the United States (US) [
1,
8,
9]. These patients are routinely prescribed opioids for pain after hospitalisation so are at high risk of becoming opioid-dependent. Opioid dependence and the harm directly and indirectly associated with this are a major public health problem in many countries [
10,
11]. However, in New Zealand (NZ), little is known about the extent of this problem. Therefore, we are interested in studying the utilisation and associated adverse outcomes of opioids after surgery and trauma in this country. One way of doing this would be through the retrospective analysis of large datasets collected for administrative or other purposes, but such datasets are not available in all regions of the world.
In NZ, public hospital admissions are fully funded by the government for all NZ citizens, permanent residents, and certain work visa holders. 100 percent of public and 90 percent of private hospitalisations are reported to the Ministry of Health (MoH), which maintains almost a fully representative national data set [
12]. Each patient is assigned a unique National Health Index (NHI) number when admitted to a private or public hospital, visits a primary health physician, or is dispensed with a subsidised medication from any community pharmacy. The MoH encrypts all NHIs to ensure patients’ privacy when using these data for statistical purposes to report on the health of the NZ population [
13]. The encrypted NHI allows for data linkage across different datasets for research. The availability of these data allows a relatively novel pharmacoepidemiologic approach to be taken to study many influences on healthcare outcomes, including the impact of opioid prescribing [
14].
The purpose of our current study was to use routinely collected health data from the NZ MoH to identify and describe a cohort of patients admitted to any NZ hospital for trauma or to undergo a surgical procedure between 1 January 2007 to 31 December 2019. We aimed to describe key characteristics of these cohorts including sociodemographic and clinical factors, baseline comorbidities and the use of opioids before surgery or trauma. We aim to then use the surgical and trauma cohorts separately in future research to investigate the prevalence and outcomes of persistent opioid use after surgery and trauma in NZ. The demonstration that it is feasible to identify and collect considerable information on large cohorts of patients admitted to NZ hospitals for surgery or trauma, and access to our methods and datasets (upon request- see data sharing statement), may also be of interest to other investigators and other stakeholders for research into various aspects of surgery and trauma in NZ [
14].
2. Results
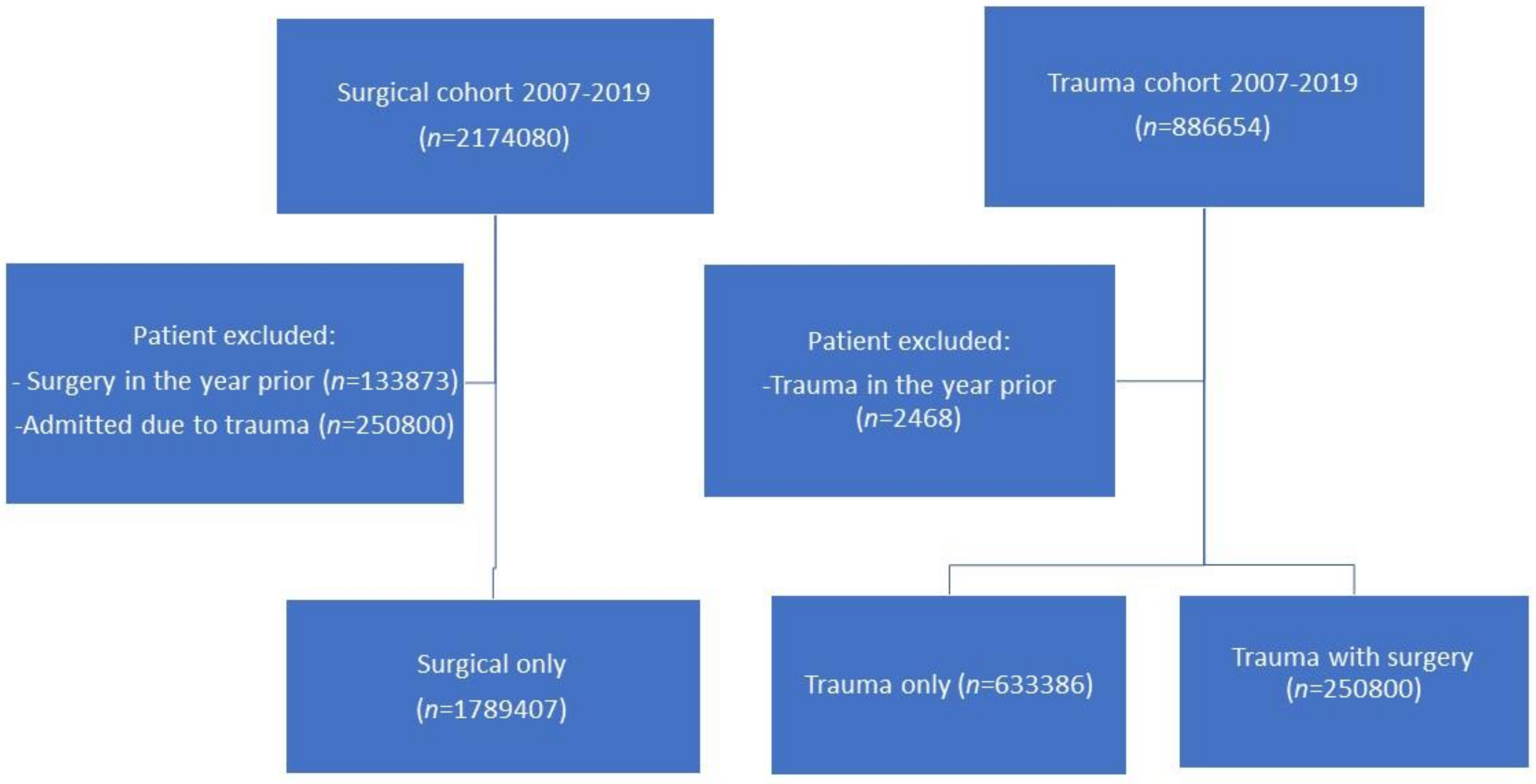
Between 2007–2019, we identified 1.78 million surgical only patients, 633,386 trauma only, and 250,800 trauma with surgery. We excluded 133,873 patients from the surgical cohort and 2468 patients from the trauma cohort (see
Figure 1).
Patient characteristics of all three cohorts are shown in
Table 1, and patient comorbidity in
Table 2.
For the surgical only cohort variables of ASA and surgical urgency (p < 0.001), only half of the patients had an ASA score documented: 415,926 patients (23.2%) had an ASA score of one, 365,440 (20.4%) of two, 98,031 (5.5%) three and 16,181 (0.9%) four. The urgency of the surgery for the surgical only cohort was elective for 191,066 patients (10.7%) and acute for 1,598,341 patients (89.3%).
Amongst the patient characteristics, there were variables with significant differences across the three cohorts. For age, more than half of the patients were <30 years old in the trauma with surgery group (52.8%). Patients of Māori ethnicity had higher prevalence in the trauma only (17.0%) and trauma with surgery group (19.7%) compared to surgical only patients (13.5%). Auckland was the domicile region with the highest prevalence of admission, with rates of 18.8% for trauma only patients, 17.7% for surgical only patients and 17.4% for trauma with surgery patients. More than half (51.1%) of the trauma with surgery patients had a length of stay of longer than one day. Trauma only patients had the highest prevalence of death within one year of event (17.8%) and pre-trauma history of opioid dispensing (18.3%). Amongst the comorbidities, trauma only patients also seemed to be overrepresented in most categories including: hypertension (18.1%), congestive heart failure (8.9%), COPD (3.6%), diabetes mellitus, mental health disorders (17.0%), chronic pain (2.3%), osteoarthritis (1.1), chronic kidney disease (2.3%), previous history of cancer with either malignant diagnostic codes (2.9%) or benign diagnostic codes (1.0%). However, most of the patients across the three cohorts did not have comorbidities as calculated using either the Charlson and M3 Index.
3. Method
3.1. Study Design
This retrospective descriptive study aimed to identify and characterise all patients admitted to any NZ hospital for trauma or surgery. Data were extracted and linked across multiple routinely collected health datasets administered by the MoH. Data access was approved by the Auckland Health Research Ethics Committee (AH1159). The cohort is linked with the Australian New Zealand Clinical Trials Registry (ANZCTR): ACTRN12620000924954.
3.2. Data Sources
Data for surgical and trauma patients were accessed from national healthcare datasets: the National Minimum Dataset for Hospital Events (NMDS), the Pharmaceutical Collection (PHARMS), the Mortality Collection (MORT), the National Health Index (NHI) database and the Primary Health Organisation Enrolment Collection (PHO).
The NMDS contains information on public and privately funded New Zealand hospital admissions [
15]. Data in the NMDS includes all patient hospitalisation episodes and discharge diagnoses recorded and coded using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) [
16]. The NMDS uses the Australian Classification of Health Interventions (ACHI) to code surgical procedures.
The PHARMS database contains claim and payment information for all subsidised medications dispensed in community pharmacies [
17]. This includes the date of dispensing, the generic name of the chemical dispensed, its formulation, the quantity prescribed, and the duration of supply where this is recorded. A ‘Chemical ID’ and a ‘Formulation ID’ are available to indicate both the medication and formulation dispensed. Data from PHARMS are available from 2006.
The MORT database contains the date of death and cause of death based on the coroner’s report; there is a one year delay in reporting the date of death and two years for the cause of death due to the timeframe of the coronial process [
18]. The PHO and NHI databases provide sociodemographic and health utilisation data on patients, including their domicile region [
13,
19].
We chose the dates 1 January 2007 to 31 December 2019 for this study due to limitations in data availability. At the time of study inception, mortality data were only available up to 2020, and PHARMS data were only reliable from 2006 [
20]. See
Supplementary section for full data variable definitions of variables extracted.
3.3. Surgical and Trauma Cohorts
Patients in the trauma cohort were identified from primary ICD-10-AM diagnostic codes indicating trauma of the Head (S00-S09), Neck (S10-S19), Thorax (S20-S29), Abdomen (S30-S39), Shoulder (S40-S49), Elbow (S50-S59), Wrist (S60-S69), Thigh (S70-S79), Knee (S80-S89), Ankle (S90-S99), Multiple (T00-T07) and unspecified (T08-T14).
For the surgical cohort, patients were identified from ACHI procedures codes recorded by each NZ hospital. Procedures are grouped within three levels of hierarchy, the first being the organ system, the second being the type of procedure given a ‘block’ code, and lastly, the specific method of the procedure given a procedure code. For example, Laparotomy is given a ‘block’ code of [985], and ‘exploratory laparotomy’ a specific procedure code of 30373-800 [985], as opposed to ‘postoperative reopening of laparotomy site’ code 3039-300 [985].
The cohort entry date was the first date of hospital discharge, where this occurred between 1 January 2007 and 31 December 2019. In the surgical cohort we excluded patients who had a surgical event in the year prior to cohort entry to avoid patients whose procedure may have been consequent to previous history of surgery, either in a planned process of staged procedures or in response to complications of a prior procedure. For the trauma cohort we also excluded those with trauma events in the year prior to cohort entry to avoid patients whose trauma event may have been related to previous history of trauma, such as complications related to trauma. The full list of diagnostic and procedure codes used to identify patients is available from our previously published study protocol [
20]. We placed no restrictions regarding age on patients in either cohort. Two cohorts were initially identified, one for surgery and one for trauma. We then identified and separated patients in both cohorts with the same initial hospital admission and discharge dates. This resulted in three independent cohorts for further analysis: surgical only, trauma only and trauma with surgery. At the request of a reviewer, we then undertook statistical tests to facilitate comparisons between these three cohorts of patients.
3.4. Sociodemographic Variables
For each patient, we collated data on age at the time of cohort entry date, sex, socioeconomic status, domicile region in NZ, and the region of the healthcare facility to which they were admitted during their index event. Socioeconomic status was based on the patient’s area of residence and represented a social deprivation score taken from the NZ Deprivation Index (NZDep). NZDep is an area-based socioeconomic deprivation measure with ten deciles. We collapsed this into quintiles between one to five, one being the least deprived and five the most deprived [
19,
21]. The patient domicile region was defined as the general practice location where the patient was registered. The region of the facility was defined as the region of NZ where the patient received care and the location of the facility where the index event occurred. See
Supplementary Table S1 for sociodemographic variable definitions.
3.5. Event Variables
We calculated the length of stay for each hospital admission as the number of days between admission and discharge dates. For the surgical cohort, we determined the urgency of the surgery using the ‘admission type’ variable recorded in the NMDS data. Admissions classified as ‘arranged’ (admission type ‘AA’) or ‘acute’ (‘AC’) were considered acute admissions. Those classified as ‘waiting list’ (‘WN’) were elective. All admissions to private hospitals were considered to be elective admissions. These were coded as ‘Private admission’ (AP). Lastly, we also determined if death occurred in the year following discharge from the index hospital event. See
Supplementary Table S2 for event variable definitions. These event variables were recorded at the time of a patient’s hospital admission as part of routinely collected health data.
Baseline comorbidities were identified from hospital discharge diagnoses and specific pharmaceutical dispensing records. History of opioid dispensing in this study refers to opioid use before trauma or surgery. To determine this we examined each individual’s community pharmacy dispensing history for any opioids dispensed in the 365 days preceding each patient’s trauma or surgical event discharge date. Specific comorbidities included hypertension, congestive heart failure, chronic obstructive pulmonary disease (COPD), asthma, sleep apnoea, diabetes mellitus (types 1 and 2), mental health disorders, chronic pain, rheumatoid arthritis, psoriatic arthritis, gout, osteoarthritis, obesity, smoking, and chronic kidney and liver disease. See our
Supplementary Table S3 for all specific diagnostic and medication codes used.
3.6. Comorbidity Indices
We extracted data for two comorbidity indices, Charlson’s and M3, and quantified the American Society of Anaesthetic’s (ASA) physical status scores for surgical patients. These indices allowed us to evaluate the overall comorbidity burden and pre-anesthesia medical comorbidity. The M3 index was designed specifically for NZ and has outperformed Charlson’s index in the NZ setting [
22]. The ASA scores were only calculated for surgical only patients. Scores are derived from each patient’s anaesthetic procedure codes and may reflect a more clinically oriented assessment of patient health. A pre-baseline period of five years was used for all patients when assessing Charlson and M3 index scores. See
Supplementary Table S3 for full index definition and diagnostic codes.
3.7. Variable Reporting and Data Analysis
Categorical variables were reported as percentages. Continuous data were converted to categorical variables based on clinical relevance and data distribution by discussion and consensus with a multidisciplinary team. Chi-square tests were used to assess differences in baseline characteristics between the different cohorts. We designated a two-tailed
p value < 0.05 as statistically significant. No correction was made for multiple testing. Results are presented in
Table 1 The analyses were done using SPSS v28 IBM corporation, Armonk, NY, USA.
4. Discussion
From 2007 to 2019, we identified nearly 1.8 million NZ patients who had surgery only, over half a million admitted to hospital with trauma, and over a quarter of a million admitted for both trauma and surgery. These represent substantial cohorts for our group’s planned opioid-related research. The fact that such a large number of patients undergoing hospitalisation for surgery or trauma can be identified, and that substantial information can be collected about them, may also be of value to others conducting studies of surgical outcomes in NZ. Even as they stand, our results provide a valuable (and, we believe, novel) picture of the characteristics of patients admitted to hospitals for trauma or surgery in NZ.
Our proposed research into the prevalence and outcomes of persistent opioid use in these cohorts of patients will provide hitherto unavailable information on the extent of this public health problem in NZ that will inform health policy. It will also allow comparisons to be made between NZ and other countries, noting that there are considerable sociopolitical and healthcare differences between NZ and many other high-income countries. Given that the datasets used in this study are maintained on an ongoing basis, our approach opens the opportunity to monitor changes in the prevalence and outcomes of opioid use after surgery or trauma and thus evaluate any interventions arising from changes in healthcare policy (for example). Furthermore, our data could inform the design of potential future prospective studies of investigator-initiated interventions to improve outcomes after trauma or surgery, including but not only informing estimates of the required sample size for such studies.
We found significant differences between the three cohorts across all variables (p < 0.001 in each case). Clinically significant differences between cohorts were seen in age distribution, ethnicity, domicile region, length of stay, previous opioid use, baseline comorbidities and subsequent death within one year. Patients aged under 30 years old and those between the ages of 30 and 65 were overrepresented in the cohorts of trauma with surgery (52.8%), and surgery only (49.3%). This likely reflects that younger patients are more likely to have surgery, especially in those with trauma, as this age group may be considered by the healthcare team to be better suited for surgery.
The NZ national census in 2018 reported the population of European ethnicity to be 70.2%, Māori 16.5%, Pacific 8.1%, Asian 15.1%, and MELAA 1.5% [
23]. On this basis, Māori (19.7%) and Pacific patients (8.7%) are overrepresented in being hospitalised for trauma with surgery but underrepresented in terms of surgery only admissions (13.5% and 6.0%). In all three cohorts Auckland was the patient domicile region with the most patients. Auckland healthcare facilities provided hospital care for most patients in the surgery only and trauma only cohorts. However, more patients were treated in the Counties region in the trauma with surgery cohort. Possible reasons for Auckland’s overrepresentation in both patient regions of domicile and health facility are higher accessibility to primary health care, a regional trauma centre and the provision of many national surgical services. The region of facility may be used to account for regional variations in hospital culture and prescribing practices. Length of stay in hospital and surgical urgency are important clinical variables. They have been used in other opioid-related studies as covariates of opioid prescribing on discharge and persistent opioid use [
24,
25]. For our subsequent studies on persistent opioid use and its related harm, other important confounding variables include evidence of previous opioid use disorder or overdose and prior use of opioids [
20]. Across the three cohorts, the trauma only cohort had the greatest proportion of patients with both pre-trauma opioid use and pre-trauma diagnosis of opioid use disorder. Data on patients’ history of opioid use before surgery or trauma will allow us to establish an opioid-naïve sample to use in future studies to assess de novo complications related to opioid use.
Of the 18 comorbidities examined, eight occurred in less than 1% of patients across all three cohorts. We also calculated two comorbidity indices, the Charlson and M3, the latter being a more NZ focused index. Based on our analyses for the three cohorts, it would appear that the M3 is a more sensitive measure for analysing patient comorbidity with fewer patients scoring zero compared to the Charlson index: for surgical only patients (84.5% vs. 93.1%), trauma only (70.8% vs. 82.8%) and trauma with surgery (90.3% vs. 95.1%). The M3 index may perform better since it was specifically designed to measure comorbidity burden, and the data to calculate this was available to the study [
22], and because it contains 55 patient conditions compared with 20 conditions used in the Charlson index. Lastly, in terms of mortality, patients admitted with trauma only had the highest prevalence of death within one year following the index. This difference is likely due to the nature of the trauma admissions being severe, as it likely included mostly major trauma requiring hospitalisation. Patients admitted with trauma may have more risk factors for developing persistent opioid use than those admitted for surgery only, or trauma with surgery. For example, the trauma only cohort had a higher rate of pre-trauma opioid use, pre-trauma diagnosis of an opioid use disorder, comorbidity burden, mental health disorder and chronic pain, and all these factors have been shown to have a significant association with persistent opioid use [
26,
27].
Strength and Limitations
The strength of our research is based on the use of NZ-wide national data, and it includes almost all of NZ’s hospitalisations for surgical and trauma patients. It also includes a wide range of surgical procedures considered interventional and thus highly relevant for post-surgical research. We purposely did not set any age restrictions on our patient cohorts as this would allow us to investigate opioid utilisation and associated harm across age groups. Whilst the NZ national data collections contain rich and valuable clinical information, and the validity of the data has been tested in previous observational studies, there are still certain limitations when used for research [
14]. Patients not requiring tertiary care would not have been included in our studies. Patients with less than three hours of hospital admissions would also have been excluded, as these admissions are not recorded in the NMDS. It is a considerable challenge to identify patients who have undergone surgery from NMDS data. In the most current ACHI 11th edition, there are a total of 6231 procedure codes [
16]. Unfortunately, this classification includes both interventional and non-interventional procedures, and no priority is assigned to a primary procedure in the NMDS records. Only surgical patients who had undergone interventional surgery were included in our study. We adopted a similar method of identifying interventional surgeries with accompanying anaesthetic codes as used in a previous study examining surgical outcomes in NZ patients by Campbell et al. [
12]. This included a high priority list of surgical procedures considered to be interventional with a surgical severity score assigned from one to five, with one being least severe and five the most severe [
28]. This provides a degree of priority for each surgical hospital episode and eliminates patients with no procedures of interest. Hospitalisation data may also have underestimated the level of comorbidity in our cohorts as we could not include diagnostic codes recorded in primary care. For some specific comorbidities, we included both hospital diagnoses and community pharmacy dispensing of specific pharmaceuticals to identify patients. In this case, the particular diagnoses and pharmaceuticals included were based on previously published studies but are only proxies and may over or underrepresent comorbidity rates depending on the sensitivity and specificity of the coding [
29,
30,
31]. For opioid use, we only considered opioid use before trauma or surgery; opioid use after either trauma or surgery was beyond the scope of this study and will be the subject of future studies.
Our national ethnicity data was based on patient prioritised ethnicity, a NZ specific coding system in which patients identifying with multiple ethnicities are assigned a priority ethnic group. Māori ethnicity is prioritised first, followed by Pacific, Asian, other ethnic groups, and European ethnicity. Thus, a certain proportion of patients identifying with several ethnic groups will have been coded Māori [
15]. Notably, European and Asian ethnicities also consist of a diverse and heterogeneous population in terms of origin, health risks and diverse cultures. In our subsequent studies, this is important given that there may be an overestimation of outcomes due to the priority assignment of ethnicities.
The PHARMS data also poses certain limitations due to changes in data collection over time. This dataset only records dispensing of subsidised medication; medications that are self-funded by patients, purchased over the counter, or if the medication cost is less than the patient co-payment of five dollars (from 2013 onwards) or three dollars (2004–2008) are not recorded. Thus, medication dispensing in small quantities and for shorter duration courses may be under-reported. Data before 2006 are not recorded comprehensively. Hence, our cohort identification only encompassed the years 2007–2019. Another challenge of working with the national databases is checking demographic details such as date of birth and sex. This is especially important when linking data from different national datasets, as the data recorded for a small proportion of patients may differ across the five data collections. We referred to the PHO and NHI collections for our baseline demographic data. Lastly, privately funded hospital admissions data are limited as these are deemed commercially sensitive information by the MoH. An example of this was notable in recording the hospital facility variable, which was missing for over 300,000 patients. It was unavailable for all privately funded hospitalisations, mostly in the surgical cohort. However, during our analysis of this data variable, certain private hospital facilities were recorded due to the procedure being publicly funded. The facility variable demonstrates the complex intermingling of the public and private health sectors in NZ. Public hospitals outsource procedures to private hospitals when there is insufficient capacity in the public system to do that procedure at that time. For publicly funded admissions, it is mandatory to report this variable to the MoH [
32]. Although privately funded admissions are mostly omitted, our research group feel the variable is good enough to include in future studies to reflect regional variations in practice. Differences between the three cohorts should be interpreted cautiously noting that allocation to cohorts was not randomised and that a large number of statistical tests were undertaken, making type I errors quite likely.
5. Conclusions
We have identified and described cohorts of patients who have either undergone surgery or were admitted to a hospital for trauma in NZ between 2007 and 2019. We plan to use these cohorts in a series of studies to describe the prevalence of persistent opioid use in surgical and trauma patients and to assess the clinical outcomes of morbidity and mortality related to persistent opioid use. Significant differences in baseline characteristics in relation to opioid use and persistent opioid use were observed across the three cohorts, suggesting that future studies related to opioid use should treat surgical and trauma patients separately. These patient cohorts are also available for other researchers wishing to explore other influences on the outcomes of surgery and trauma in NZ.
Author Contributions
J.G., A.H.Y.C., A.F.M., K.B. and P.J. conceived and designed this study idea. A.T. was the data analyst and was responsible for data linkage and extraction. J.G. and A.H.Y.C. obtained ethics approval for the study. J.G. completed the first draft of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by non-commercial entities, the Auckland Academic Health Alliance (AAHA) no. 8753 and the NZ HRC no. 21/056. Neither funding body has input into design, data collection, analysis, interpretation of data and writing of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Auckland Health Research Ethics Committee (AHREC) AH1159 (date of approval 15 April 2020).
Informed Consent Statement
Not Applicable.
Data Availability Statement
The datasets generated during the current study are not publicly avariable due to legal and ethical restrictions in New Zealand. The data may be made available on reasonable request at the discretion of the primary author of this paper (jay.gong@auckland.ac.nz).
Acknowledgments
This paper will contribute to JG’s PhD from the University of Auckland.
Conflicts of Interest
J.G. receives grants from Auckland Academic Health Alliance (AAHA) and the NZ Health Research Council (HRC). K.B. reports grants from A+ charitable trust, New Zealand Pharmacy Education and Research Foundation, outside this submitted work, and U21 Health Sciences Research Development Fund. A.H.Y.C. reports consultancy fees from Spoonful of Sugar Ltd., a UCL-Business spin-out company, and grants from Health Research Council (HRC), New Zealand Pharmacy Education and Research Foundation, Chorus Ltd., Oakley Mental Health Foundation, WHO, Universitas 21, A+ charitable trust (Auckland District Health Board), and Maurice and Phyllis Paykel Trust, outside this submitted work. A.H.Y.C. is also the holder of the Robert Irwin Postdoctoral Fellowship and the Auckland Medical Research Foundation Senior Research Fellowship. P.J. reports grants from A+ Charitable Trust and HRC outside this submitted work. All authors declare there are no competing interests related to the submitted work.
References
- Brummett, C.M.; Waljee, J.F.; Goesling, J.; Moser, S.; Lin, P.; Englesbe, M.J.; Bohnert, A.S.B.; Kheterpal, S.; Nallamothu, B.K. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017, 152, e170504. [Google Scholar] [CrossRef] [PubMed]
- Harbaugh, C.M.; Lee, J.S.; Hu, H.M.; McCabe, S.E.; Voepel-Lewis, T.; Englesbe, M.J.; Brummett, C.M.; Waljee, J.F. Persistent Opioid Use Among Pediatric Patients After Surgery. Pediatrics 2018, 141, e20172439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larach, D.B.; Sahara, M.J.; As-Sanie, S.; Moser, S.E.; Urquhart, A.G.; Lin, J.; Hassett, A.L.; Wakeford, J.A.; Clauw, D.J.; Waljee, J.F.; et al. Patient Factors Associated with Opioid Consumption in the Month Following Major Surgery. Ann. Surg. 2019, 273, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Peahl, A.F.; Morgan, D.M.; Dalton, V.K.; Zivin, K.; Lai, Y.-L.; Hu, H.M.; Langen, E.; Low, L.K.; Brummett, C.M.; Waljee, J.F.; et al. New persistent opioid use after acute opioid prescribing in pregnancy: A nationwide analysis. Am. J. Obstet. Gynecol. 2020, 223, 566.e561–566.e513. [Google Scholar] [CrossRef] [PubMed]
- Alghnam, S.; Castillo, R. Traumatic injuries and persistent opioid use in the USA: Findings from a nationally representative survey. Inj. Prev. 2017, 23, 87–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bell, T.M.; Raymond, J.; Vetor, A.; Mongalo, A.; Adams, Z.; Rouse, T.; Carroll, A. Long-term prescription opioid utilization, substance use disorders, and opioid overdoses after adolescent trauma. J. Trauma Acute Care Surg. 2019, 87, 836–840. [Google Scholar] [CrossRef] [Green Version]
- Elkbuli, A.; Narvel, R.I.; Boneva, D.; McKenney, M. The Impact of Chronic Opioid Use on Trauma Outcomes. Am. Surg. 2020, 86, E35–E37. [Google Scholar] [CrossRef]
- Clement, K.C.; Canner, J.K.; Whitman, G.J.R.; Lawton, J.S.; Grant, M.C.; Sussman, M.S. New Persistent Opioid Use After Aortic and Mitral Valve Surgery in Commercially Insured Patients. Ann. Thorac. Surg. 2020, 110, 829–835. [Google Scholar] [CrossRef]
- Daoust, R.; Paquet, J.; Moore, L.; Gosselin, S.; Gélinas, C.; Rouleau, D.M.; Bérubé, M.; Morris, J. Incidence and Risk Factors of Long-term Opioid Use in Elderly Trauma Patients. Ann. Surg. 2018, 268, 985–991. [Google Scholar] [CrossRef]
- von Oelreich, E.; Eriksson, M.; Brattstrom, O.; Sjolund, K.F.; Discacciati, A.; Larsson, E.; Oldner, A. Risk factors and outcomes of chronic opioid use following trauma. Br. J. Surg. 2020, 107, 413–421. [Google Scholar] [CrossRef]
- Brummett, C.M.; England, C.; Evans-Shields, J.; Kong, A.M.; Lew, C.R.; Henriques, C.; Zimmerman, N.M.; Pawasauskas, J.; Oderda, G. Health Care Burden Associated with Outpatient Opioid Use Following Inpatient or Outpatient Surgery. J. Manag. Care Spec. Pharm. 2019, 25, 973–983. [Google Scholar] [CrossRef]
- Campbell, D.; Boyle, L.; Soakell-Ho, M.; Hider, P.; Wilson, L.; Koea, J.; Merry, A.F.; Frampton, C.; Short, T.G. National risk prediction model for perioperative mortality in non-cardiac surgery. Br. J. Surg. 2019, 106, 1549–1557. [Google Scholar] [CrossRef]
- New Zealand (NZ) Ministry of Health. The National Health Index (NHI) Number. Available online: https://www.health.govt.nz/our-work/health-identity/national-health-index (accessed on 1 May 2020).
- Nishtala, P.; Ndukwe, H.; Chyou, T.Y.; Salahudeen, M.; Narayan, S. An overview of pharmacoepidemiology in New Zealand: Medical databases, registries and research achievements. N. Z. Med. J. 2017, 130, 52–61. [Google Scholar]
- New Zealand (NZ) Ministry of Health. The National Minimum Dataset (NMDS). Available online: http://www.health.govt.nz/nz-healthstatistics/national-collections-and-surveys/collections/national-minimum-dataset-hospital-events (accessed on 1 May 2020).
- The Australian Consortium for Classification Development (ACCD). The Australian Classification of Health Interventions (ACHI). Available online: https://www.health.govt.nz/nz-health-statistics/classification-and-terminology/using-icd-10-am-achi-acs (accessed on 20 May 2020).
- New Zealand (NZ) Ministry of Health. Pharmaceutical Collection Dataset. Available online: https://minhealthnz.shinyapps.io/datapharm/ (accessed on 1 May 2020).
- New Zealand (NZ) Ministry of Health. The Mortality Collection. Available online: https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/collections/mortality-collection (accessed on 1 May 2020).
- New Zealand (NZ) Ministry of Health. The Primary Health Organisation Enrolment Collection (PHO). Available online: https://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/collections/primary-health-organisation-enrolment-collection (accessed on 1 May 2020).
- Gong, J.; Merry, A.F.; Beyene, K.A.; Campbell, D.; Frampton, C.; Jones, P.; McCall, J.; Moore, M.; Chan, A.H.Y. Persistent opioid use and opioid-related harm after hospital admissions for surgery and trauma in New Zealand: A population-based cohort study. BMJ Open 2021, 11, e044493. [Google Scholar] [CrossRef]
- Atkinson, J.; Salmond, C.; Crampton, P. NZDep2013 Index of Deprivation; University of Otago: Dunedin, New Zealand, 2014. [Google Scholar]
- Stanley, J.; Sarfati, D. The new measuring multimorbidity index predicted mortality better than Charlson and Elixhauser indices among the general population. J. Clin. Epidemiol. 2017, 92, 99–110. [Google Scholar] [CrossRef]
- NZ, S. New Zealand Census 2018. Available online: https://www.stats.govt.nz/topics/population (accessed on 10 July 2020).
- Kim, S.C.; Choudhry, N.; Franklin, J.M.; Bykov, K.; Eikermann, M.; Lii, J.; Fischer, M.A.; Bateman, B.T. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthr. Cartil. 2017, 25, 1399–1406. [Google Scholar] [CrossRef] [Green Version]
- Brescia, A.A.; Harrington, C.A.; Mazurek, A.A.; Ward, S.T.; Lee, J.S.J.; Hu, H.M.; Brummett, C.M.; Waljee, J.F.; Lagisetty, P.A.; Lagisetty, K.H. Factors Associated With New Persistent Opioid Usage After Lung Resection. Ann. Thorac. Surg. 2019, 107, 363–368. [Google Scholar] [CrossRef]
- Riva, J.J.; Noor, S.T.; Wang, L.; Ashoorion, V.; Foroutan, F.; Sadeghirad, B.; Couban, R.; Busse, J.W. Predictors of Prolonged Opioid Use After Initial Prescription for Acute Musculoskeletal Injuries in Adults. Ann. Intern. Med. 2020, 173, 721–729. [Google Scholar] [CrossRef]
- Pagé, M.G.; Kudrina, I.; Zomahoun, H.T.V.; Croteau, J.; Ziegler, D.; Ngangue, P.; Martin, E.; Fortier, M.; Boisvert, E.E.; Beaulieu, P.; et al. A Systematic Review of the Relative Frequency and Risk Factors for Prolonged Opioid Prescription Following Surgery and Trauma Among Adults. Ann. Surg. 2020, 271, 845–854. [Google Scholar] [CrossRef]
- Pasternak, L.R. Preanesthesia Evaluation of the Surgical Patient. ASA Refresh. Courses Anesthesiol. 1996, 24, 205–219. [Google Scholar] [CrossRef]
- Schug, S.A.; Lavandʼhomme, P.; Barke, A.; Korwisi, B.; Rief, W.; Treede, R.D. The IASP classification of chronic pain for ICD-11: Chronic postsurgical or posttraumatic pain. Pain 2019, 160, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Bowden, N.; Gibb, S.; Thabrew, H.; Kokaua, J.; Audas, R.; Merry, S.; Taylor, B.; Hetrick, S.E. Case identification of mental health and related problems in children and young people using the New Zealand Integrated Data Infrastructure. BMC Med. Inform. Decis. Mak. 2020, 20, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- VIEW. VIEW Variables and Definitions. Available online: https://wiki.auckland.ac.nz/display/VIEW/VIEW+Variables+and+Definitions (accessed on 1 January 2021).
- New Zealand (NZ) Ministry of Health. New Zealand Health System. Available online: https://www.health.govt.nz/new-zealand-health-system (accessed on 1 May 2020).
- Schrepf, A.; Phan, V.; Clemens, J.Q.; Maixner, W.; Hanauer, D.; Williams, D.A. ICD-10 Codes for the Study of Chronic Overlapping Pain Conditions in Administrative Databases. J. Pain 2020, 21, 59–70. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).