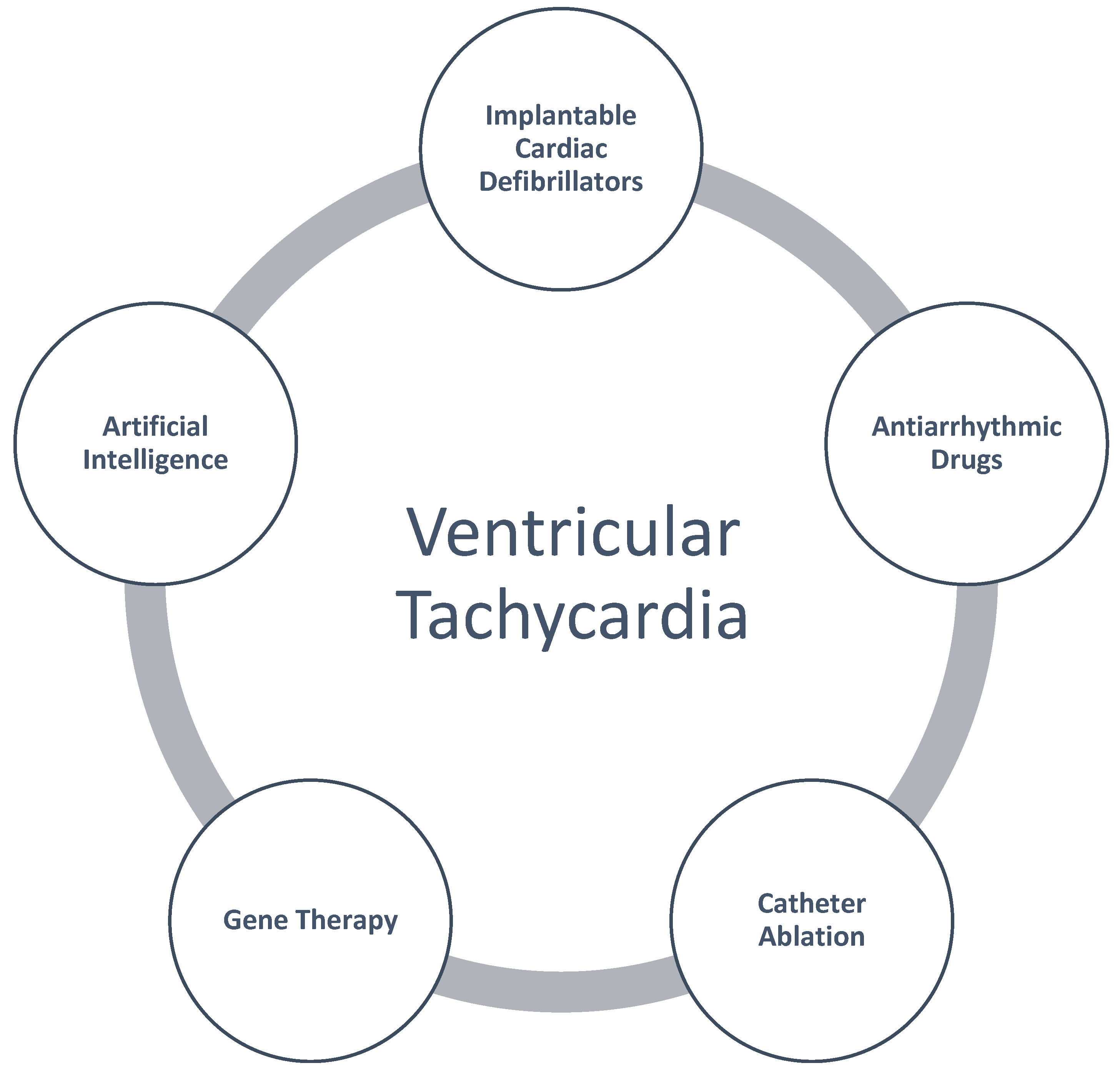
Multi-Faceted Approach to Ventricular Tachycardia: A Review of Management Strategies
Abstract
:1. Introduction
2. Methods
3. History and Epidemiology of Ventricular Tachycardia
4. Landmark Trials
4.1. Antiarrhythmic Drugs vs. ICD in the Management of VT
4.2. Catheter Ablation
4.3. Neuromodulation
5. Anti-Arrhythmic Drugs
5.1. Class I Medications
- -
- Procainamide
- -
- Quinidine
- -
- Disopyramide
5.2. Class II Agents
- -
- Beta blockers
- -
- Digoxin
5.3. Class III Medications
- -
- Amiodarone
- -
- Sotalol
- -
- Dronedarone
- -
- Dofetilide
5.4. Class IV Medications
6. Special Populations
6.1. Brugada Syndrome
6.2. Early Repolarization Syndrome
6.3. Catecholaminergic Polymorphic Ventricular Tachycardia
6.4. Idiopathic Ventricular Fibrillation
6.5. Congenital Long QT Syndrome
6.6. Anderson–Tawil Syndrome Type 1
6.7. Congenital Short QT Syndrome
6.8. Arrhythmogenic Cardiomyopathy
6.9. Hypertrophic Cardiomyopathy
6.10. Cardiac Sarcoidosis
7. Gene Therapy in VT
8. Artificial Intelligence in VT
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lewis, T. Single and successive extra-systoles. Lancet 1909, 173, 382–385. [Google Scholar] [CrossRef]
- Lewis, T. Experimental Production of Paroxysmal Tachycardia and the Effects of Ligation of the Coronary Arteries. Heart 1909, 1, 10. [Google Scholar]
- Jervell, A.; Lange-Nielsen, F. Congenital deaf-mutism, functional heart disease with prolongation of the Q-T interval, and sudden death. Am. Heart J. 1957, 54, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Romano, C.; Gemme, G.; Pongiglione, R. Rare cardiac arrythmias of the pediatric age. II. Syncopal attacks due to paroxysmal ventricular fibrillation. (presentation of 1st case in italian pediatric literature). Clin. Pediatr. 1963, 45, 656–683. [Google Scholar]
- Ward, O.C. A new familial cardiac syndrome in children. J. Ir. Med. Assoc. 1964, 54, 103–106. [Google Scholar] [PubMed]
- Dessertenne, F. Ventricular tachycardia with 2 variable opposing foci. Arch. Mal. Coeur Vaiss. 1966, 59, 263–272. [Google Scholar]
- Olshansky, B.; Chung, M.K.; Pogwizd, S.M.; Goldschlager, N. Arrhythmia Essentials, 2nd ed.; Elsevier: Philadelphia, PA, USA, 2017. [Google Scholar]
- Jong-Ming Pang, B.; Green, M.S. Epidemiology of ventricular tachyarrhythmia. Herzschrittmacherther. Elektrophysiol. 2017, 28, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Deo, R.; Albert, C.M. Epidemiology and Genetics of Sudden Cardiac Death. Circulation 2012, 125, 620–637. [Google Scholar] [CrossRef]
- Olarte, N.; Vincent, L.; Loyd, Q.; Ebner, B.; Grant, J.; Maning, J.; Hernandez, R.J.; Rivera-Rodriguez, B.; Giraldo, M.; Lambrakos, L. Gender disparities in ventricular tachycardia: Evaluating clinical outcomes and interventions. Eur. Heart J. 2022, 43 (Suppl. S2), ehac544.675. [Google Scholar] [CrossRef]
- Patel, H.P.; Thakkar, S.; Mehta, N.; Faisaluddin, M.; Munshi, R.F.; Kumar, A.; Khan, S.U.; Parikh, R.; DeSimone, C.V.; Sharma, G.; et al. Racial disparities in ventricular tachycardia in young adults: Analysis of national trends. J. Interv. Card. Electrophysiol. 2023, 66, 193–202. [Google Scholar] [CrossRef]
- Aronow, W.S.; Ahn, C.; Mercando, A.D.; Epstein, S.; Kronzon, I. Prevalence and Association of Ventricular Tachycardia and Complex Ventricular Arrhythmias with New Coronary Events in Older Men and Women with and without Cardiovascular Disease. J. Gerontol. Ser. A 2002, 57, M178–M180. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, D.M. Long-term survival after ventricular fibrillation complicating acute myocardial infarction. Lancet 1969, 294, 1085–1087. [Google Scholar] [CrossRef] [PubMed]
- Ohlow, M.-A.; Geller, J.C.; Richter, S.; Farah, A.; Müller, S.; Fuhrmann, J.T.; Lauer, B. Incidence and predictors of ventricular arrhythmias after ST-segment elevation myocardial infarction. Am. J. Emerg. Med. 2012, 30, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Bunch, T.J.; Mahapatra, S.; Murdock, D.; Molden, J.; Weiss, J.P.; May, H.T.; Bair, T.L.; Mader, K.M.; Crandall, B.G.; Day, J.D.; et al. Ranolazine Reduces Ventricular Tachycardia Burden and ICD Shocks in Patients with Drug-Refractory ICD Shocks. Pacing Clin. Electrophysiol. 2011, 34, 1600–1606. [Google Scholar] [CrossRef] [PubMed]
- Meyer, L.; Stubbs, B.; Fahrenbruch, C.; Maeda, C.; Harmon, K.; Eisenberg, M.; Drezner, J. Incidence, Causes, and Survival Trends from Cardiovascular-Related Sudden Cardiac Arrest in Children and Young Adults 0 to 35 Years of Age. Circulation 2012, 126, 1363–1372. [Google Scholar] [CrossRef]
- Brooks, R.; Burgess, J.H. Idiopathic Ventricular Tachycardia a Review. Medicine 1988, 67, 271–294. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2018, 72, e91–e220. [Google Scholar] [CrossRef] [PubMed]
- Hallstrom, A.P.; Greene, H.L.; Wyse, D.G.; Zipes, D.; Epstein, A.E.; Domanski, M.J.; Schron, E.B. Antiarrhythmics Versus Implantable Defibrillators (AVID)—Rationale, design, and methods. Am. J. Cardiol. 1995, 75, 470–475. [Google Scholar]
- Connolly, S.J.; Gent, M.; Roberts, R.S.; Dorian, P.; Roy, D.; Sheldon, R.S.; Mitchell, L.B.; Green, M.S.; Klein, G.J.; O’Brien, B. Canadian implantable defibrillator study (CIDS): A randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 2000, 101, 1297–1302. [Google Scholar] [CrossRef]
- Kuck, K.-H.; Cappato, R.; Siebels, J.; Rüppel, R. Randomized Comparison of Antiarrhythmic Drug Therapy with Implantable Defibrillators in Patients Resuscitated from Cardiac Arrest. Circulation 2000, 102, 748–754. [Google Scholar] [CrossRef]
- Zeppenfeld, K.; Tfelt-Hansen, J.; De Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; De Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef] [PubMed]
- Sapp, J.L.; Wells, G.A.; Parkash, R.; Stevenson, W.G.; Blier, L.; Sarrazin, J.F.; Thibault, B.; Rivard, L.; Gula, L.; Leong-Sit, P.; et al. Ventricular Tachycardia Ablation versus Escalation of Antiarrhythmic Drugs. N. Engl. J. Med. 2016, 375, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Hasselblad, V.; Jackson, K.P.; Pokorney, S.D.; Daubert, J.P.; Al-Khatib, S.M. Catheter ablation for ventricular tachycardia (VT) in patients with ischemic heart disease: A systematic review and a meta-analysis of randomized controlled trials. J. Interv. Card. Electrophysiol. 2016, 45, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Fudim, M.; Qadri, Y.J.; Waldron, N.H.; Boortz-Marx, R.L.; Ganesh, A.; Patel, C.B.; Podgoreanu, M.V.; Sun, A.Y.; Milano, C.A.; Tong, B.C.; et al. Stellate Ganglion Blockade for the Treatment of Refractory Ventricular Arrhythmias. JACC Clin. Electrophysiol. 2020, 6, 562–571. [Google Scholar] [CrossRef] [PubMed]
- van Welsenes, G.H.; van Rees, J.B.; Borleffs, C.J.W.; Cannegieter, S.C.; Bax, J.J.; van Erven, L.; Schalij, M.J. Long-term follow-up of primary and secondary prevention implantable cardioverter defibrillator patients. EP Europace 2011, 13, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Patel, C.; Yan, G.X.; Kocovic, D.; Kowey, P.R. Should catheter ablation be the preferred therapy for reducing ICD shocks?: Ventricular tachycardia ablation versus drugs for preventing ICD shocks: Role of adjuvant antiarrhythmic drug therapy. Circ. Arrhythmia Electrophysiol. 2009, 2, 705–711, discussion 712. [Google Scholar] [CrossRef] [PubMed]
- Movsowitz, C.; Marchlinski, F.E. Interactions between implantable cardioverter-defibrillators and class III agents. Am. J. Cardiol. 1998, 82 (Suppl. S1), 41I–48I. [Google Scholar] [CrossRef] [PubMed]
- Lei, M.; Wu, L.; Terrar, D.A.; Huang, C.L. Modernized Classification of Cardiac Antiarrhythmic Drugs. Circulation 2018, 138, 1879–1896. [Google Scholar] [CrossRef]
- The Sicilian gambit. A new approach to the classification of antiarrhythmic drugs based on their actions on arrhythmogenic mechanisms. Task Force of the Working Group on Arrhythmias of the European Society of Cardiology. Circulation 1991, 84, 1831–1851. [Google Scholar] [CrossRef]
- Ruskin, J.N. The cardiac arrhythmia suppression trial (CAST). N. Engl. J. Med. 1989, 321, 386–388. [Google Scholar] [CrossRef]
- Ortiz, M.; Martín, A.; Arribas, F.; Coll-Vinent, B.; Del Arco, C.; Peinado, R.; Almendral, J. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: The PROCAMIO study. Eur. Heart J. 2017, 38, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Toniolo, M.; Muser, D.; Grilli, G.; Burelli, M.; Rebellato, L.; Daleffe, E.; Facchin, D.; Imazio, M. Oral procainamide as pharmacological treatment of recurrent and refractory ventricular tachyarrhythmias: A single-center experience. Heart Rhythm O2 2021, 2, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Anguera, I.; García-Alberola, A.; Dallaglio, P.; Toquero, J.; Pérez, L.; Martínez, J.G.; Peinado, R.; Rubín, J.M.; Brugada, J.; Cequier, A. Shock Reduction with Long-Term Quinidine in Patients with Brugada Syndrome and Malignant Ventricular Arrhythmia Episodes. J. Am. Coll. Cardiol. 2016, 67, 1653–1654. [Google Scholar] [CrossRef]
- Li, D.L.; Cox, Z.L.; Richardson, T.D.; Kanagasundram, A.N.; Saavedra, P.J.; Shen, S.T.; Montgomery, J.A.; Murray, K.T.; Roden, D.M.; Stevenson, W.G. Quinidine in the Management of Recurrent Ventricular Arrhythmias: A Reappraisal. JACC Clin. Electrophysiol. 2021, 7, 1254–1263. [Google Scholar] [CrossRef] [PubMed]
- U.K. Rythmodan Multicentre Study Group. Oral disopyramide after admission to hospital with suspected acute myocardial infarction. Postgrad. Med. J. 1984, 60, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Moss, A.J.; Windle, J.R.; Hall, W.J.; Zareba, W.; Robinson, J.L.; McNitt, S.; Severski, P.; Rosero, S.; Daubert, J.P.; Qi, M.; et al. Safety and Efficacy of Flecainide in Subjects with Long QT-3 Syndrome (ΔKPQ Mutation): A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Ann. Noninvasive Electrocardiol. 2005, 10, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Haïssaguerre, M.; Sacher, F.; Nogami, A.; Komiya, N.; Bernard, A.; Probst, V.; Yli-Mayry, S.; Defaye, P.; Aizawa, Y.; Frank, R.; et al. Characteristics of recurrent ventricular fibrillation associated with inferolateral early repolarization role of drug therapy. J. Am. Coll. Cardiol. 2009, 53, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Kaliebe, J.W.; Murdock, D.K. Suppression of non-sustained ventricular tachycardia with ranolazine: A case report. Wmj 2009, 108, 373–375. [Google Scholar] [PubMed]
- CIBIS-II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): A randomised trial. Lancet 1999, 353, 9–13. [Google Scholar] [CrossRef]
- Gheorghiade, M.; Adams, K.F.; Colucci, W.S. Digoxin in the Management of Cardiovascular Disorders. Circulation 2004, 109, 2959–2964. [Google Scholar] [CrossRef]
- Lee, A.Y.; Kutyifa, V.; Ruwald, M.H.; McNitt, S.; Polonsky, B.; Zareba, W.; Moss, A.J.; Ruwald, A.C. Digoxin therapy and associated clinical outcomes in the MADIT-CRT trial. Heart Rhythm 2015, 12, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Julian, D.G.; Camm, A.J.; Frangin, G.; Janse, M.J.; Munoz, A.; Schwartz, P.J.; Simon, P.; European Myocardial Infarct Amiodarone Trial Investigators. Randomised trial of effect of amiodarone on mortality in patients with left-ventricular dysfunction after recent myocardial infarction: EMIAT. Lancet 1997, 349, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Cairns, J.A.; Connolly, S.J.; Roberts, R.; Gent, M.; Canadian Amiodarone Myocardial Infarction Arrhythmia Trial Investigators. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisations: CAMIAT. Lancet 1997, 349, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Køber, L.; Torp-Pedersen, C.; McMurray, J.J.V.; Gøtzsche, O.; Lévy, S.; Crijns, H.; Amlie, J.; Carlsen, J. Increased Mortality after Dronedarone Therapy for Severe Heart Failure. N. Engl. J. Med. 2008, 358, 2678–2687. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Camm, A.J.; Halperin, J.L.; Joyner, C.; Alings, M.; Amerena, J.; Atar, D.; Avezum, Á.; Blomström, P.; Borggrefe, M.; et al. Dronedarone in High-Risk Permanent Atrial Fibrillation. N. Engl. J. Med. 2011, 365, 2268–2276. [Google Scholar] [CrossRef]
- Baquero, G.A.; Banchs, J.E.; Depalma, S.; Young, S.K.; Penny-Peterson, E.D.; Samii, S.M.; Wolbrette, D.L.; Naccarelli, G.V.; Gonzalez, M.D. Dofetilide Reduces the Frequency of Ventricular Arrhythmias and Implantable Cardioverter Defibrillator Therapies. J. Cardiovasc. Electrophysiol. 2012, 23, 296–301. [Google Scholar] [CrossRef]
- Boriani, G.; Lubinski, A.; Capucci, A.; Niederle, R.; Kornacewicz-Jack, Z.; Wnuk-Wojnar, A.M.; Borggrefe, M.; Brachmann, J.; Biffi, M.; Butrous, G.S. A multicentre, double-blind randomized crossover comparative study on the efficacy and safety of dofetilide vs sotalol in patients with inducible sustained ventricular tachycardia and ischaemic heart disease. Eur. Heart J. 2001, 22, 2180–2191. [Google Scholar] [CrossRef] [PubMed]
- Ohe, T.; Shimomura, K.; Aihara, N.; Kamakura, S.; Matsuhisa, M.; Sato, I.; Nakagawa, H.; Shimizu, A. Idiopathic sustained left ventricular tachycardia: Clinical and electrophysiologic characteristics. Circulation 1988, 77, 560–568. [Google Scholar] [CrossRef]
- Nogami, A.; Naito, S.; Tada, H.; Taniguchi, K.; Okamoto, Y.; Nishimura, S.; Yamauchi, Y.; Aonuma, K.; Goya, M.; Iesaka, Y.; et al. Demonstration of diastolic and presystolic purkinje potentials as critical potentials in a macroreentry circuit of verapamil-sensitive idiopathic left ventricular tachycardia. J. Am. Coll. Cardiol. 2000, 36, 811–823. [Google Scholar] [CrossRef]
- Rosso, R.; Kalman, J.M.; Rogowski, O.; Diamant, S.; Birger, A.; Biner, S.; Belhassen, B.; Viskin, S. Calcium channel blockers and beta-blockers versus beta-blockers alone for preventing exercise-induced arrhythmias in catecholaminergic polymorphic ventricular tachycardia. Heart Rhythm 2007, 4, 1149–1154. [Google Scholar] [CrossRef]
- Brugada, P.; Brugada, J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome: A multicenter report. J. Am. Coll. Cardiol. 1992, 20, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Krahn, A.D.; Healey, J.S.; Chauhan, V.; Birnie, D.H.; Simpson, C.S.; Champagne, J.; Gardner, M.; Sanatani, S.; Exner, D.V.; Klein, G.J.; et al. Systematic assessment of patients with unexplained cardiac arrest: Cardiac Arrest Survivors with Preserved Ejection Fraction Registry (CASPER). Circulation 2009, 120, 278–285. [Google Scholar] [CrossRef]
- Nakano, Y.; Shimizu, W. Brugada Syndrome as a Major Cause of Sudden Cardiac Death in Asians. JACC Asia 2022, 2, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Antzelevitch, C.; Brugada, P.; Borggrefe, M.; Brugada, J.; Brugada, R.; Corrado, D.; Gussak, I.; LeMarec, H.; Nademanee, K.; Riera, A.R.P.; et al. Brugada Syndrome: Report of the Second Consensus Conference. Heart Rhythm 2005, 2, 429–440. [Google Scholar] [CrossRef]
- Krahn, A.D.; Behr, E.R.; Hamilton, R.; Probst, V.; Laksman, Z.; Han, H.C. Brugada Syndrome. JACC Clin. Electrophysiol. 2022, 8, 386–405. [Google Scholar] [CrossRef] [PubMed]
- Belhassen, B.; Rahkovich, M.; Michowitz, Y.; Glick, A.; Viskin, S. Management of Brugada Syndrome: Thirty-Three-Year Experience Using Electrophysiologically Guided Therapy with Class 1A Antiarrhythmic Drugs. Circ. Arrhythmia Electrophysiol. 2015, 8, 1393–1402. [Google Scholar] [CrossRef] [PubMed]
- Szel, T.; Koncz, I.; Antzelevitch, C. Cellular mechanisms underlying the effects of milrinone and cilostazol to suppress arrhythmogenesis associated with Brugada syndrome. Heart Rhythm 2013, 10, 1720–1727. [Google Scholar] [CrossRef]
- Nademanee, K.; Chung, F.P.; Sacher, F.; Nogami, A.; Nakagawa, H.; Jiang, C.; Hocini, M.; Behr, E.; Veerakul, G.; Jan Smit, J.; et al. Long-Term Outcomes of Brugada Substrate Ablation: A Report from BRAVO (Brugada Ablation of VF Substrate Ongoing Multicenter Registry). Circulation 2023, 147, 1568–1578. [Google Scholar] [CrossRef]
- Antzelevitch, C.; Yan, G.X.; Ackerman, M.J.; Borggrefe, M.; Corrado, D.; Guo, J.; Gussak, I.; Hasdemir, C.; Horie, M.; Huikuri, H.; et al. J-Wave syndromes expert consensus conference report: Emerging concepts and gaps in knowledge. Heart Rhythm 2016, 13, e295–e324. [Google Scholar] [CrossRef]
- Agac, M.T.; Erkan, H.; Korkmaz, L. Conversion of Brugada type I to type III and successful control of recurrent ventricular arrhythmia with cilostazol. Arch. Cardiovasc. Dis. 2014, 107, 476–478. [Google Scholar] [CrossRef]
- Patocskai, B.; Barajas-Martinez, H.; Hu, D.; Gurabi, Z.; Koncz, I.; Antzelevitch, C. Cellular and ionic mechanisms underlying the effects of cilostazol, milrinone, and isoproterenol to suppress arrhythmogenesis in an experimental model of early repolarization syndrome. Heart Rhythm 2016, 13, 1326–1334. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, T.; Ashikaga, K.; Honda, T.; Arita, M. Prevention of ventricular fibrillation by cilostazol, an oral phosphodiesterase inhibitor, in a patient with Brugada syndrome. J. Cardiovasc. Electrophysiol. 2002, 13, 698–701. [Google Scholar] [CrossRef] [PubMed]
- Leenhardt, A.; Denjoy, I.; Guicheney, P. Catecholaminergic polymorphic ventricular tachycardia. Circ. Arrhythmia Electrophysiol. 2012, 5, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Abbas, M.; Miles, C.; Behr, E. Catecholaminergic Polymorphic Ventricular Tachycardia. Arrhythmia Electrophysiol. Rev. 2022, 11, e20. [Google Scholar] [CrossRef]
- van der Werf, C.; Nederend, I.; Hofman, N.; van Geloven, N.; Ebink, C.; Frohn-Mulder, I.M.; Alings, A.M.; Bosker, H.A.; Bracke, F.A.; van den Heuvel, F.; et al. Familial evaluation in catecholaminergic polymorphic ventricular tachycardia: Disease penetrance and expression in cardiac ryanodine receptor mutation-carrying relatives. Circ. Arrhythmia Electrophysiol. 2012, 5, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Asatryan, B.; Schaller, A.; Seiler, J.; Servatius, H.; Noti, F.; Baldinger, S.H.; Tanner, H.; Roten, L.; Dillier, R.; Lam, A.; et al. Usefulness of Genetic Testing in Sudden Cardiac Arrest Survivors with or without Previous Clinical Evidence of Heart Disease. Am. J. Cardiol. 2019, 123, 2031–2038. [Google Scholar] [CrossRef] [PubMed]
- Conte, G.; Caputo, M.L.; Regoli, F.; Marcon, S.; Klersy, C.; Adjibodou, B.; Del Bufalo, A.; Moccetti, T.; Auricchio, A. True idiopathic ventricular fibrillation in out-of-hospital cardiac arrest survivors in the Swiss Canton Ticino: Prevalence, clinical features, and long-term follow-up. EP Europace 2017, 19, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Stampe, N.K.; Jespersen, C.B.; Glinge, C.; Bundgaard, H.; Tfelt-Hansen, J.; Winkel, B.G. Clinical characteristics and risk factors of arrhythmia during follow-up of patients with idiopathic ventricular fibrillation. J. Cardiovasc. Electrophysiol. 2020, 31, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Belhassen, B.; Glick, A.; Viskin, S. Excellent long-term reproducibility of the electrophysiologic efficacy of quinidine in patients with idiopathic ventricular fibrillation and Brugada syndrome. Pacing Clin. Electrophysiol. 2009, 32, 294–301. [Google Scholar] [CrossRef]
- Leenhardt, A.; Glaser, E.; Burguera, M.; Nurnberg, M.; Maison-Blanche, P.; Coumel, P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994, 89, 206–215. [Google Scholar] [CrossRef]
- Malhi, N.; Cheung, C.C.; Deif, B.; Roberts, J.D.; Gula, L.J.; Green, M.S.; Pang, B.; Sultan, O.; Konieczny, K.M.; Angaran, P.; et al. Challenge and Impact of Quinidine Access in Sudden Death Syndromes: A National Experience. JACC Clin. Electrophysiol. 2019, 5, 376–382. [Google Scholar] [CrossRef] [PubMed]
- Belhassen, B.; Viskin, S.; Fish, R.; Glick, A.; Setbon, I.; Eldar, M. Effects of electrophysiologic-guided therapy with Class IA antiarrhythmic drugs on the long-term outcome of patients with idiopathic ventricular fibrillation with or without the Brugada syndrome. J. Cardiovasc. Electrophysiol. 1999, 10, 1301–1312. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, P.J.; Stramba-Badiale, M.; Crotti, L.; Pedrazzini, M.; Besana, A.; Bosi, G.; Gabbarini, F.; Goulene, K.; Insolia, R.; Mannarino, S.; et al. Prevalence of the Congenital Long-QT Syndrome. Circulation 2009, 120, 1761–1767. [Google Scholar] [CrossRef] [PubMed]
- Krahn, A.D.; Laksman, Z.; Sy, R.W.; Postema, P.G.; Ackerman, M.J.; Wilde, A.A.M.; Han, H.C. Congenital Long QT Syndrome. JACC Clin. Electrophysiol. 2022, 8, 687–706. [Google Scholar] [CrossRef] [PubMed]
- Wilde, A.A.M.; Amin, A.S.; Postema, P.G. Diagnosis, management and therapeutic strategies for congenital long QT syndrome. Heart 2022, 108, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Bos, J.M.; Crotti, L.; Rohatgi, R.K.; Castelletti, S.; Dagradi, F.; Schwartz, P.J.; Ackerman, M.J. Mexiletine Shortens the QT Interval in Patients with Potassium Channel-Mediated Type 2 Long QT Syndrome. Circ. Arrhythmia Electrophysiol. 2019, 12, e007280. [Google Scholar] [CrossRef] [PubMed]
- Etheridge, S.P.; Compton, S.J.; Tristani-Firouzi, M.; Mason, J.W. A new oral therapy for long QT syndrome: Long-term oral potassium improves repolarization in patients with HERG mutations. J. Am. Coll. Cardiol. 2003, 42, 1777–1782. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.; Ramachandra, C.J.A.; Singh, P.; Chitre, A.; Lua, C.H.; Mura, M.; Crotti, L.; Wong, P.; Schwartz, P.J.; Gnecchi, M.; et al. Identification of a targeted and testable antiarrhythmic therapy for long-QT syndrome type 2 using a patient-specific cellular model. Eur. Heart J. 2018, 39, 1446–1455. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, B.J.; John Kim, C.S.; Hamrick, S.K.; Ye, D.; Tester, D.J.; Ackerman, M.J. Promise and Potential Peril with Lumacaftor for the Trafficking Defective Type 2 Long-QT Syndrome-Causative Variants, p.G604S, p.N633S, and p.R685P, Using Patient-Specific Re-Engineered Cardiomyocytes. Circ. Genom. Precis. Med. 2020, 13, 466–475. [Google Scholar] [CrossRef]
- Schwartz, P.J.; Gnecchi, M.; Dagradi, F.; Castelletti, S.; Parati, G.; Spazzolini, C.; Sala, L.; Crotti, L. From patient-specific induced pluripotent stem cells to clinical translation in long QT syndrome Type 2. Eur. Heart J. 2019, 40, 1832–1836. [Google Scholar] [CrossRef] [PubMed]
- Delannoy, E.; Sacher, F.; Maury, P.; Mabo, P.; Mansourati, J.; Magnin, I.; Camous, J.P.; Tournant, G.; Rendu, E.; Kyndt, F.; et al. Cardiac characteristics and long-term outcome in Andersen-Tawil syndrome patients related to KCNJ2 mutation. EP Europace 2013, 15, 1805–1811. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, K.; Aiba, T.; Kimura, H.; Hayashi, H.; Ohno, S.; Yasuoka, C.; Tanioka, Y.; Tsuchiya, T.; Yoshida, Y.; Hayashi, H.; et al. Efficacy and safety of flecainide for ventricular arrhythmias in patients with Andersen-Tawil syndrome with KCNJ2 mutations. Heart Rhythm 2015, 12, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Dewi, I.P.; Dharmadjati, B.B. Short QT syndrome: The current evidences of diagnosis and management. J. Arrhythmia 2020, 36, 962–966. [Google Scholar] [CrossRef] [PubMed]
- El-Battrawy, I.; Besler, J.; Li, X.; Lan, H.; Zhao, Z.; Liebe, V.; Schimpf, R.; Lang, S.; Wolpert, C.; Zhou, X.; et al. Impact of Antiarrhythmic Drugs on the Outcome of Short QT Syndrome. Front. Pharmacol. 2019, 10, 771. [Google Scholar] [CrossRef] [PubMed]
- Mazzanti, A.; Maragna, R.; Vacanti, G.; Kostopoulou, A.; Marino, M.; Monteforte, N.; Bloise, R.; Underwood, K.; Tibollo, V.; Pagan, E.; et al. Hydroquinidine Prevents Life-Threatening Arrhythmic Events in Patients with Short QT Syndrome. J. Am. Coll. Cardiol. 2017, 70, 3010–3015. [Google Scholar] [CrossRef] [PubMed]
- Schimpf, R.; Veltmann, C.; Giustetto, C.; Gaita, F.; Borggrefe, M.; Wolpert, C. In vivo effects of mutant HERG K+ channel inhibition by disopyramide in patients with a short QT-1 syndrome: A pilot study. J. Cardiovasc. Electrophysiol. 2007, 18, 1157–1160. [Google Scholar] [CrossRef] [PubMed]
- Bun, S.S.; Maury, P.; Giustetto, C.; Deharo, J.C. Electrical storm in short-QT syndrome successfully treated with Isoproterenol. J. Cardiovasc. Electrophysiol. 2012, 23, 1028–1030. [Google Scholar] [CrossRef] [PubMed]
- Gaita, F.; Giustetto, C.; Bianchi, F.; Schimpf, R.; Haissaguerre, M.; Calo, L.; Brugada, R.; Antzelevitch, C.; Borggrefe, M.; Wolpert, C. Short QT syndrome: Pharmacological treatment. J. Am. Coll. Cardiol. 2004, 43, 1494–1499. [Google Scholar] [CrossRef]
- Te Riele, A.S.; James, C.A.; Philips, B.; Rastegar, N.; Bhonsale, A.; Groeneweg, J.A.; Murray, B.; Tichnell, C.; Judge, D.P.; Van Der Heijden, J.F.; et al. Mutation-positive arrhythmogenic right ventricular dysplasia/cardiomyopathy: The triangle of dysplasia displaced. J. Cardiovasc. Electrophysiol. 2013, 24, 1311–1320. [Google Scholar] [CrossRef]
- Cappelletto, C.; Gregorio, C.; Barbati, G.; Romani, S.; De Luca, A.; Merlo, M.; Mestroni, L.; Stolfo, D.; Sinagra, G. Antiarrhythmic therapy and risk of cumulative ventricular arrhythmias in arrhythmogenic right ventricle cardiomyopathy. Int. J. Cardiol. 2021, 334, 58–64. [Google Scholar] [CrossRef]
- Wichter, T.; Borggrefe, M.; Haverkamp, W.; Chen, X.; Breithardt, G. Efficacy of antiarrhythmic drugs in patients with arrhythmogenic right ventricular disease. Results in patients with inducible and noninducible ventricular tachycardia. Circulation 1992, 86, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Marcus, G.M.; Glidden, D.V.; Polonsky, B.; Zareba, W.; Smith, L.M.; Cannom, D.S.; Estes, N.A., 3rd; Marcus, F.; Scheinman, M.M.; Multidisciplinary Study of Right Ventricular Dysplasia Investigators. Efficacy of antiarrhythmic drugs in arrhythmogenic right ventricular cardiomyopathy: A report from the North American ARVC Registry. J. Am. Coll. Cardiol. 2009, 54, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Orgeron, G.; Tichnell, C.; Murray, B.; Crosson, J.; Monfredi, O.; Cadrin-Tourigny, J.; Tandri, H.; Calkins, H.; James, C.A. Impact of Exercise Restriction on Arrhythmic Risk among Patients with Arrhythmogenic Right Ventricular Cardiomyopathy. J. Am. Heart Assoc. 2018, 7, e008843. [Google Scholar] [CrossRef] [PubMed]
- Rolland, T.; Badenco, N.; Maupain, C.; Duthoit, G.; Waintraub, X.; Laredo, M.; Himbert, C.; Frank, R.; Hidden-Lucet, F.; Gandjbakhch, E. Safety and efficacy of flecainide associated with beta-blockers in arrhythmogenic right ventricular cardiomyopathy. EP Europace 2022, 24, 278–284. [Google Scholar] [CrossRef]
- Zareba, W.; Tichnell, C.; Rosero, S.Z.; Cerrone, M.; Zipse, M.M.; Marchlinski, F.E.; Sun, A.Y.; Indik, J.H.; James, C.A.; Mestroni, L.; et al. Ce-452779-3 randomized placebo-controlled trial of flecainide in patients with arrhythmogenic right ventricular cardiomyopathy. Heart Rhythm 2023, 20, S24. [Google Scholar] [CrossRef]
- Al-Aidarous, S.; Protonotarios, A.; Elliott, P.M.; Lambiase, P.D. Management of arrhythmogenic right ventricular cardiomyopathy. Heart 2023, 110, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Krahn, A.D.; Wilde, A.A.M.; Calkins, H.; La Gerche, A.; Cadrin-Tourigny, J.; Roberts, J.D.; Han, H.C. Arrhythmogenic Right Ventricular Cardiomyopathy. JACC Clin. Electrophysiol. 2022, 8, 533–553. [Google Scholar] [CrossRef] [PubMed]
- Chelko, S.P.; Asimaki, A.; Andersen, P.; Bedja, D.; Amat-Alarcon, N.; DeMazumder, D.; Jasti, R.; MacRae, C.A.; Leber, R.; Kleber, A.G.; et al. Central role for GSK3β in the pathogenesis of arrhythmogenic cardiomyopathy. JCI Insight 2016, 1, e85923. [Google Scholar] [CrossRef]
- Maron, B.J.; Rowin, E.J.; Maron, M.S. Global Burden of Hypertrophic Cardiomyopathy. JACC Heart Fail. 2018, 6, 376–378. [Google Scholar] [CrossRef]
- Ommen, S.R.; Semsarian, C. Hypertrophic cardiomyopathy: A practical approach to guideline directed management. Lancet 2021, 398, 2102–2108. [Google Scholar] [CrossRef]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2020, 76, e159–e240. [Google Scholar] [CrossRef]
- McKenna, W.J.; Oakley, C.M.; Krikler, D.M.; Goodwin, J.F. Improved survival with amiodarone in patients with hypertrophic cardiomyopathy and ventricular tachycardia. Br. Heart J. 1985, 53, 412–416. [Google Scholar] [CrossRef] [PubMed]
- Santangeli, P.; Muser, D.; Maeda, S.; Filtz, A.; Zado, E.S.; Frankel, D.S.; Dixit, S.; Epstein, A.E.; Callans, D.J.; Marchlinski, F.E. Comparative effectiveness of antiarrhythmic drugs and catheter ablation for the prevention of recurrent ventricular tachycardia in patients with implantable cardioverter-defibrillators: A systematic review and meta-analysis of randomized controlled trials. Heart Rhythm 2016, 13, 1552–1559. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm 2018, 15, e190–e252. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Van Herendael, H.; Alshengeiti, L.; Dorian, P.; Mangat, I.; Korley, V.; Ahmad, K.; Golovchiner, G.; Aves, T.; Pinter, A. Mexiletine as an adjunctive therapy to amiodarone reduces the frequency of ventricular tachyarrhythmia events in patients with an implantable defibrillator. J. Cardiovasc. Pharmacol. 2013, 62, 199–204. [Google Scholar] [CrossRef]
- Packard, E.; de Feria, A.; Peshin, S.; Reza, N.; Owens, A.T. Contemporary Therapies and Future Directions in the Management of Hypertrophic Cardiomyopathy. Cardiol. Ther. 2022, 11, 491–507. [Google Scholar] [CrossRef]
- Muser, D.; Santangeli, P.; Liang, J.J.; Castro, S.A.; Magnani, S.; Hayashi, T.; Garcia, F.C.; Frankel, D.S.; Dixit, S.; Zado, E.S.; et al. Characterization of the Electroanatomic Substrate in Cardiac Sarcoidosis: Correlation with Imaging Findings of Scar and Inflammation. JACC Clin. Electrophysiol. 2018, 4, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Mehta, D.; Mori, N.; Goldbarg, S.H.; Lubitz, S.; Wisnivesky, J.P.; Teirstein, A. Primary prevention of sudden cardiac death in silent cardiac sarcoidosis: Role of programmed ventricular stimulation. Circ. Arrhythmia Electrophysiol. 2011, 4, 43–48. [Google Scholar] [CrossRef]
- Birnie, D.H.; Sauer, W.H.; Bogun, F.; Cooper, J.M.; Culver, D.A.; Duvernoy, C.S.; Judson, M.A.; Kron, J.; Mehta, D.; Cosedis Nielsen, J.; et al. HRS expert consensus statement on the diagnosis and management of arrhythmias associated with cardiac sarcoidosis. Heart Rhythm 2014, 11, 1304–1323. [Google Scholar] [CrossRef] [PubMed]
- Cherrett, C.; Lee, W.; Bart, N.; Subbiah, R. Management of the arrhythmic manifestations of cardiac sarcoidosis. Front. Cardiovasc. Med. 2023, 10, 1104947. [Google Scholar] [CrossRef]
- Bongianino, R.; Denegri, M.; Mazzanti, A.; Lodola, F.; Vollero, A.; Boncompagni, S.; Fasciano, S.; Rizzo, G.; Mangione, D.; Barbaro, S.; et al. Allele-Specific Silencing of Mutant mRNA Rescues Ultrastructural and Arrhythmic Phenotype in Mice Carriers of the R4496C Mutation in the Ryanodine Receptor Gene (RYR2). Circ. Res. 2017, 121, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Bezzerides, V.J.; Caballero, A.; Wang, S.; Ai, Y.; Hylind, R.J.; Lu, F.; Heims-Waldron, D.A.; Chambers, K.D.; Zhang, D.; Abrams, D.J.; et al. Gene Therapy for Catecholaminergic Polymorphic Ventricular Tachycardia by Inhibition of Ca(2+)/Calmodulin-Dependent Kinase II. Circulation 2019, 140, 405–419. [Google Scholar] [CrossRef] [PubMed]
- Denegri, M.; Bongianino, R.; Lodola, F.; Boncompagni, S.; De Giusti, V.C.; Avelino-Cruz, J.E.; Liu, N.; Persampieri, S.; Curcio, A.; Esposito, F.; et al. Single delivery of an adeno-associated viral construct to transfer the CASQ2 gene to knock-in mice affected by catecholaminergic polymorphic ventricular tachycardia is able to cure the disease from birth to advanced age. Circulation 2014, 129, 2673–2681. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Olson, E.N. CRISPR Modeling and Correction of Cardiovascular Disease. Circ. Res. 2022, 130, 1827–1850. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.; Philippen, L.; Lahiri, S.K.; Lee, C.; Park, S.H.; Word, T.A.; Li, N.; Jarrett, K.E.; Gupta, R.; Reynolds, J.O.; et al. In Vivo Ryr2 Editing Corrects Catecholaminergic Polymorphic Ventricular Tachycardia. Circ. Res. 2018, 123, 953–963. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Ma, S.; Sun, C. RNA interference-based therapeutics for inherited long QT syndrome. Exp. Ther. Med. 2015, 10, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Yu, G.; Chakrabarti, S.; Tischenko, M.; Chen, A.L.; Wang, Z.; Cho, H.; French, B.A.; Naga Prasad, S.V.; Chen, Q.; Wang, Q.K. Gene therapy targeting protein trafficking regulator MOG1 in mouse models of Brugada syndrome, arrhythmias, and mild cardiomyopathy. Sci. Transl. Med. 2022, 14, eabf3136. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, F.; Zhang, J.; Wang, J.; Bradford, W.H.; Nair, A.; Fargnoli, A.; Selvan, N.; Gutierrez, S.; Law, K.; Fenn, T.; et al. LX2020, an Adeno Associated Viral-Based Plakophilin 2 Gene Therapy Stabilizes Cardiac Disease Phenotype in a Severe Mouse Model of Arrhythmogenic Right Ventricular Cardiomyopathy. Circulation 2022, 146 (Suppl. S1), A13599. [Google Scholar] [CrossRef]
- Feeny, A.K.; Chung, M.K.; Madabhushi, A.; Attia, Z.I.; Cikes, M.; Firouznia, M.; Friedman, P.A.; Kalscheur, M.M.; Kapa, S.; Narayan, S.M.; et al. Artificial Intelligence and Machine Learning in Arrhythmias and Cardiac Electrophysiology. Circ. Arrhythmia Electrophysiol. 2020, 13, e007952. [Google Scholar] [CrossRef]
- Bos, J.M.; Attia, Z.I.; Albert, D.E.; Noseworthy, P.A.; Friedman, P.A.; Ackerman, M.J. Use of Artificial Intelligence and Deep Neural Networks in Evaluation of Patients with Electrocardiographically Concealed Long QT Syndrome from the Surface 12-Lead Electrocardiogram. JAMA Cardiol. 2021, 6, 532–538. [Google Scholar] [CrossRef]
- Hong, S.; Lee, S.; Lee, J.; Cha, W.C.; Kim, K. Prediction of Cardiac Arrest in the Emergency Department Based on Machine Learning and Sequential Characteristics: Model Development and Retrospective Clinical Validation Study. JMIR Med. Inform. 2020, 8, e15932. [Google Scholar] [CrossRef] [PubMed]
- Au-Yeung, W.-T.M.; Reinhall, P.G.; Poole, J.E.; Anderson, J.; Johnson, G.; Fletcher, R.D.; Moore, H.J.; Mark, D.B.; Lee, K.L.; Bardy, G.H. SCD-HeFT: Use of R-R interval statistics for long-term risk stratification for arrhythmic sudden cardiac death. Heart Rhythm 2015, 12, 2058–2066. [Google Scholar] [CrossRef] [PubMed]
- Shade, J.K.; Prakosa, A.; Popescu, D.M.; Yu, R.; Okada, D.R.; Chrispin, J.; Trayanova, N.A. Predicting risk of sudden cardiac death in patients with cardiac sarcoidosis using multimodality imaging and personalized heart modeling in a multivariable classifier. Sci. Adv. 2021, 7, eabi8020. [Google Scholar] [CrossRef] [PubMed]
- Trayanova, N.A.; Lyon, A.; Shade, J.; Heijman, J. Computational modeling of cardiac electrophysiology and arrhythmogenesis: Toward clinical translation. Physiol. Rev. 2024, 104, 1265–1333. [Google Scholar] [CrossRef] [PubMed]
- Kabra, R.; Israni, S.; Vijay, B.; Baru, C.; Mendu, R.; Fellman, M.; Sridhar, A.; Mason, P.; Cheung, J.W.; DiBiase, L.; et al. Emerging role of artificial intelligence in cardiac electrophysiology. Cardiovasc. Digit. Health J. 2022, 3, 263–275. [Google Scholar] [CrossRef]
- Prakosa, A.; Arevalo, H.J.; Deng, D.; Boyle, P.M.; Nikolov, P.P.; Ashikaga, H.; Blauer, J.J.E.; Ghafoori, E.; Park, C.J.; Blake, R.C.; et al. Personalized virtual-heart technology for guiding the ablation of infarct-related ventricular tachycardia. Nat. Biomed. Eng. 2018, 2, 732–740. [Google Scholar] [CrossRef]
| Special Population | Antiarrhythmic Therapy |
|---|---|
| Primary Arrhythmia Syndromes | |
| Brugada Syndrome | Maintenance treatment:
|
| Early Repolarization | Maintenance treatment:
|
| Catecholaminergic PolymorphicVentricular Tachycardia | First-line treatment:
|
| Idiopathic Ventricular Fibrillation | Maintenance treatment:
|
| Long QT Syndrome | First-line treatment:
|
| Anderson–Tawil Syndrome | First-line treatment:
|
| Short QT Syndrome | First-line treatment:
|
| Cardiomyopathies | |
| Arrhythmogenic Cardiomyopathy | First-line treatment:
|
| Hypertrophic Cardiomyopathy | First-line treatment:
|
| Cardiac Sarcoidosis |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hartge, F.; Skeete, J.; Pinedo, A.; Zeleke, B.; Khan, A.; Mekritthikrai, R.; Dye, C.A. Multi-Faceted Approach to Ventricular Tachycardia: A Review of Management Strategies. Pharmacoepidemiology 2024, 3, 265-284. https://doi.org/10.3390/pharma3030018
Hartge F, Skeete J, Pinedo A, Zeleke B, Khan A, Mekritthikrai R, Dye CA. Multi-Faceted Approach to Ventricular Tachycardia: A Review of Management Strategies. Pharmacoepidemiology. 2024; 3(3):265-284. https://doi.org/10.3390/pharma3030018
Chicago/Turabian StyleHartge, Francis, Jamario Skeete, Alejandro Pinedo, Bethlehem Zeleke, Asad Khan, Raktham Mekritthikrai, and Cicely Anne Dye. 2024. "Multi-Faceted Approach to Ventricular Tachycardia: A Review of Management Strategies" Pharmacoepidemiology 3, no. 3: 265-284. https://doi.org/10.3390/pharma3030018
APA StyleHartge, F., Skeete, J., Pinedo, A., Zeleke, B., Khan, A., Mekritthikrai, R., & Dye, C. A. (2024). Multi-Faceted Approach to Ventricular Tachycardia: A Review of Management Strategies. Pharmacoepidemiology, 3(3), 265-284. https://doi.org/10.3390/pharma3030018






