Inactivation of Avian Influenza Virus Aerosol Using Membrane-Less Electrolyzed Water Spraying
Abstract
:1. Introduction
2. Materials and Methods
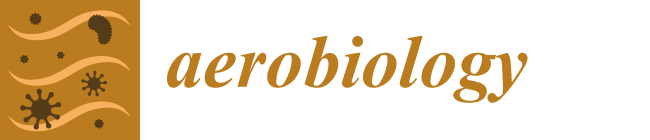
2.1. Generation of Membrane−Less Electrolyzed Water
2.2. H6N1 Viral Preparation and Viability Assay
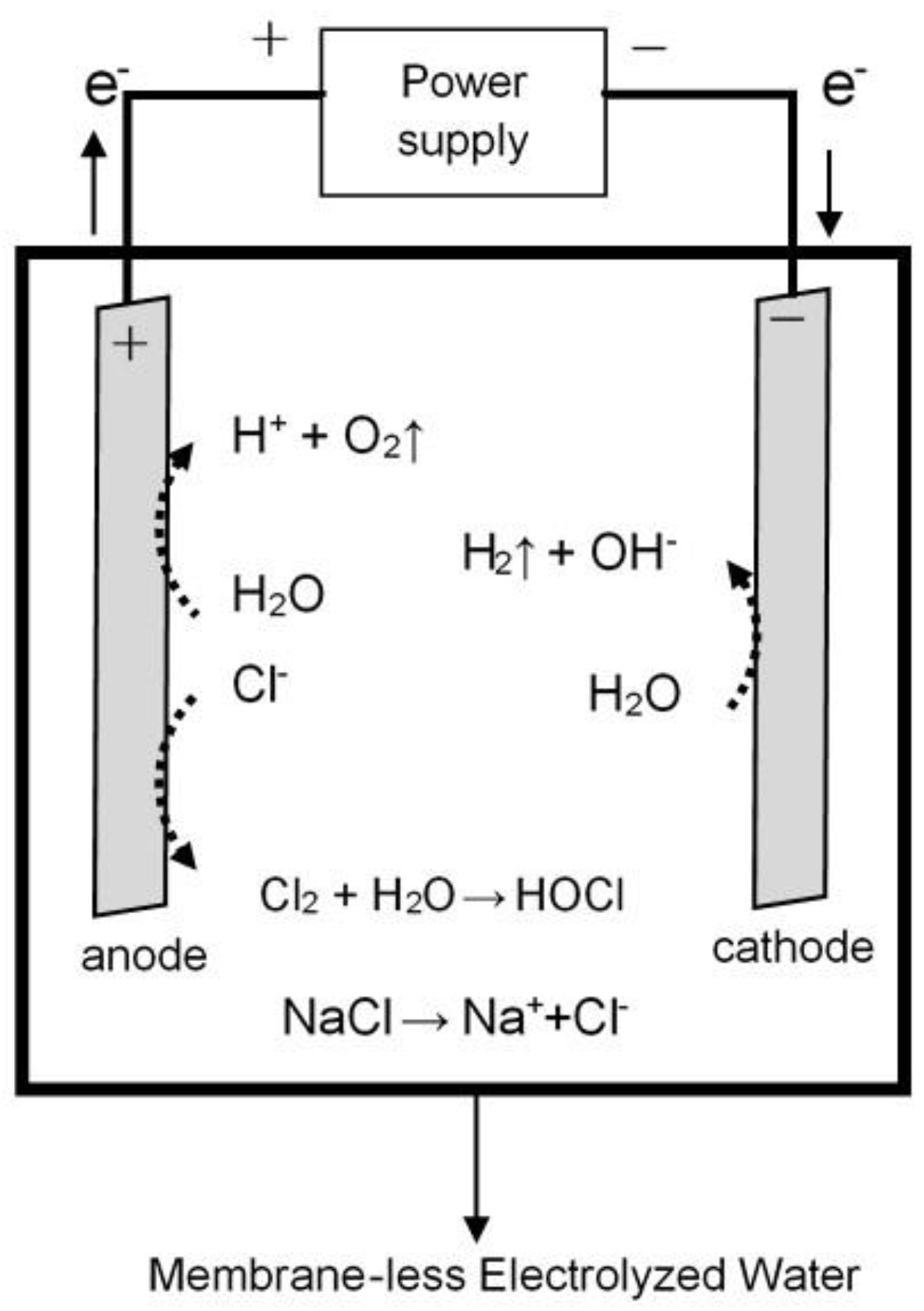
2.3. Environmentally Controlled Experimental Setup
3. Results
3.1. Natural Deposition of H6N1 Viral Aerosol inside the Enclosed Chamber
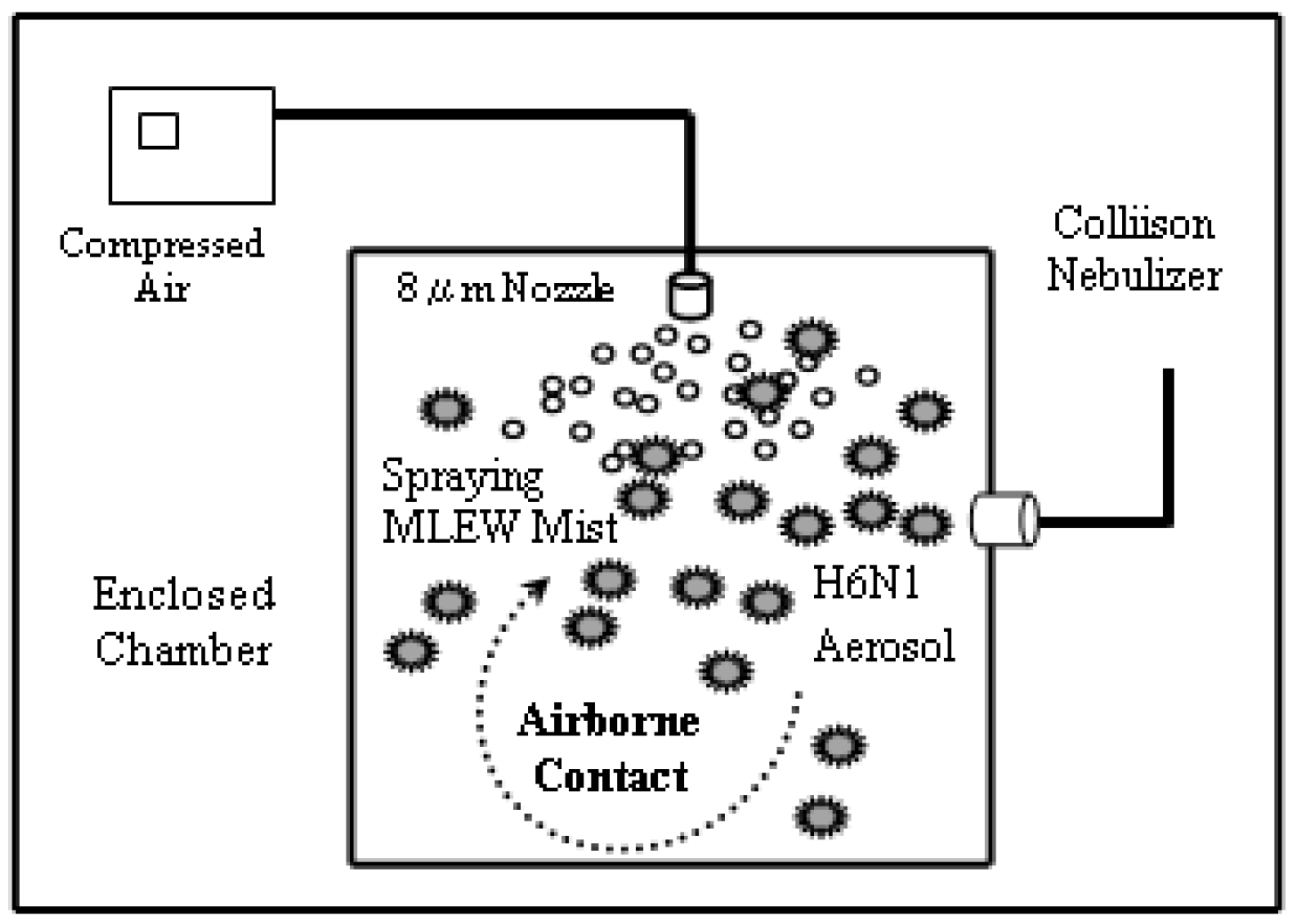
3.2. The Inactivation Ability of Pure Water Spraying against H6N1 Viral Aerosol
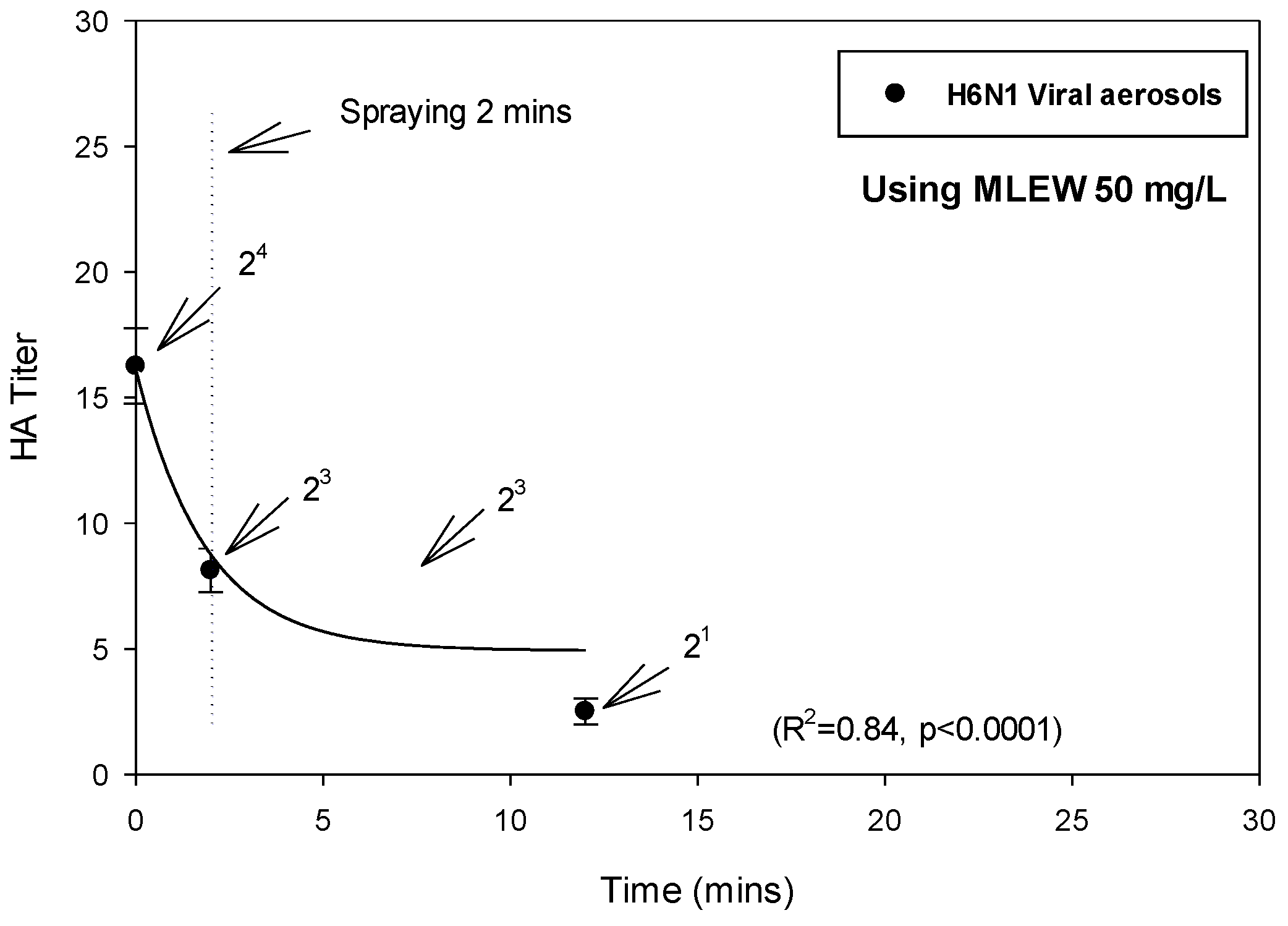
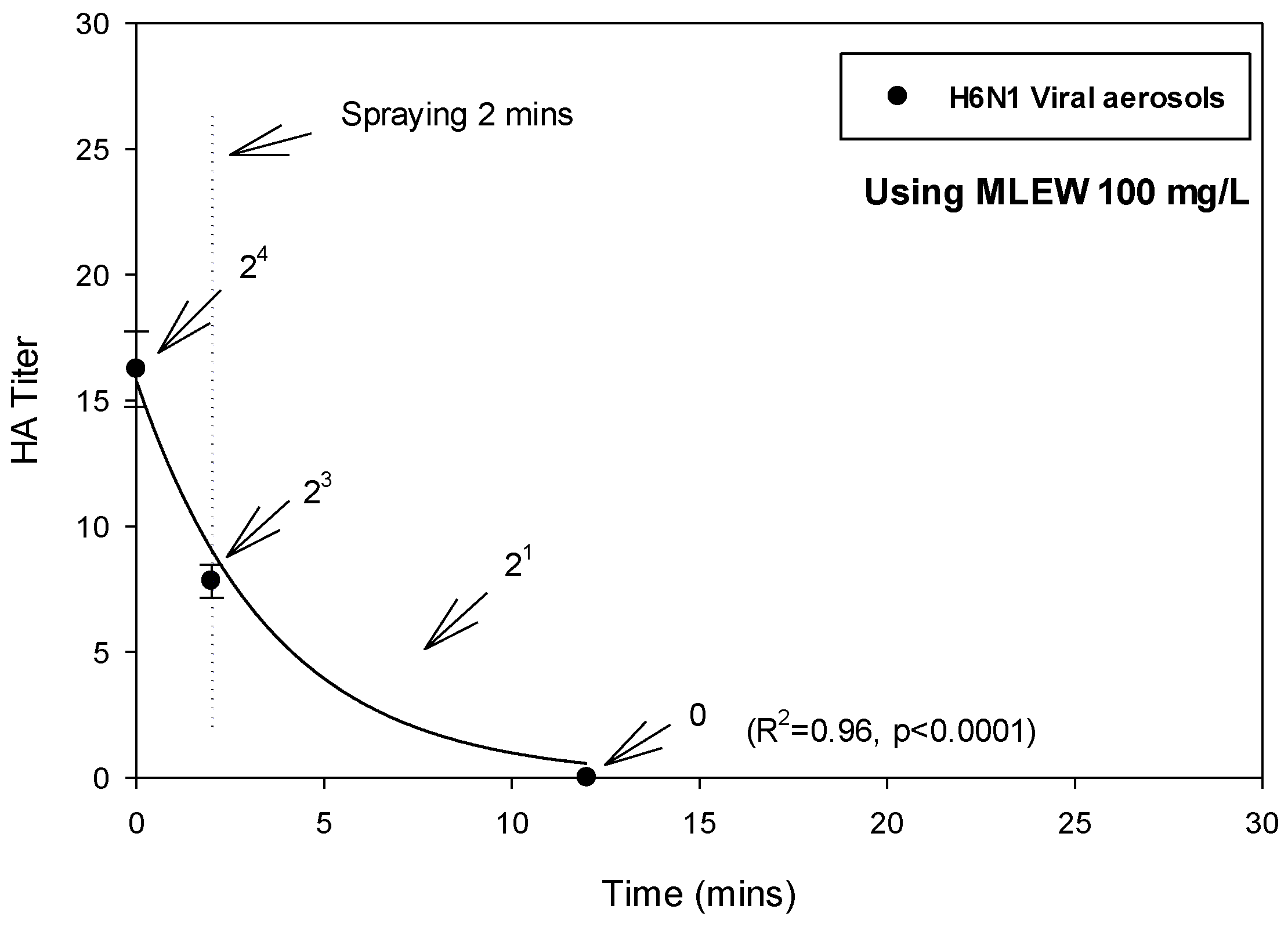
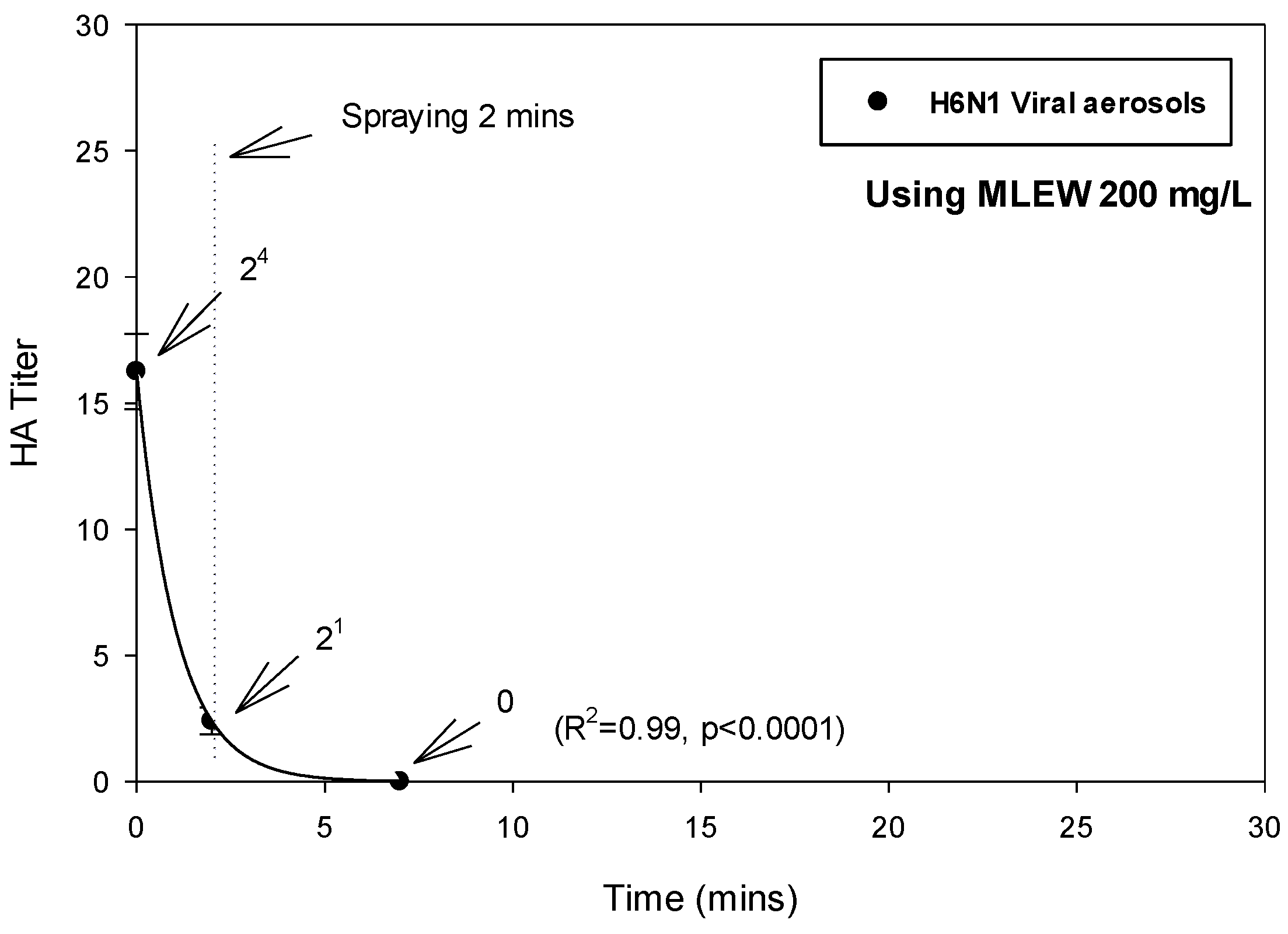
3.3. The Inactivation Effect of MLEW Spraying against H6N1 Viral Aerosol
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, Y.T.; Linster, M.; Mendenhall, I.H.; Su, Y.C.F.; Smith, G.J.D. Avian influenza viruses in humans: Lessons from past outbreaks. Br. Med. Bull. 2019, 132, 81–95. [Google Scholar] [CrossRef]
- Wei, S.H.; Yang, J.R.; Wu, H.S.; Chang, M.C.; Lin, J.S.; Lin, C.Y.; Liu, Y.L.; Lo, Y.C.; Yang, C.H.; Chuang, J.H.; et al. Human infection with avian influenza A H6N1 virus: An epidemiological analysis. Lancet Respir. Med. 2013, 1, 771–778. [Google Scholar] [CrossRef]
- Pantin-Jackwood, M.J.; Swayne, D.E. Pathogenesis and pathobiology of avian influenza virus infection in birds. Rev. Sci. Tech. 2009, 28, 113–136. [Google Scholar] [CrossRef]
- El Zowalaty, M.E.; Bustin, S.A.; Husseiny, M.I.; Ashour, H.M. Avian influenza: Virology, diagnosis and surveillance. Future Microbiol. 2013, 8, 1209–1227. [Google Scholar] [CrossRef]
- Landman, W.J.M.; Germeraad, E.A.; Kense, M.J. An avian influenza virus H6N1 outbreak in commercial layers: Case report and reproduction of the disease. Avian Pathol. J. W.V.P.A 2019, 48, 98–110. [Google Scholar] [CrossRef]
- Wang, G.; Deng, G.; Shi, J.; Luo, W.; Zhang, G.; Zhang, Q.; Liu, L.; Jiang, Y.; Li, C.; Sriwilaijaroen, N.; et al. H6 influenza viruses pose a potential threat to human health. J. Virol. 2014, 88, 3953–3964. [Google Scholar] [CrossRef]
- Cheung, C.L.; Vijaykrishna, D.; Smith, G.J.; Fan, X.H.; Zhang, J.X.; Bahl, J.; Duan, L.; Huang, K.; Tai, H.; Wang, J.; et al. Establishment of influenza A virus (H6N1) in minor poultry species in southern China. J. Virol. 2007, 81, 10402–10412. [Google Scholar] [CrossRef]
- Herfst, S.; Schrauwen, E.J.; Linster, M.; Chutinimitkul, S.; de Wit, E.; Munster, V.J.; Sorrell, E.M.; Bestebroer, T.M.; Burke, D.F.; Smith, D.J.; et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 2012, 336, 1534–1541. [Google Scholar] [CrossRef]
- Jegede, A.; Fu, Q.; Lin, M.; Kumar, A.; Guan, J. Aerosol exposure enhanced infection of low pathogenic avian influenza viruses in chickens. Transbound. Emerg. Dis. 2019, 66, 435–444. [Google Scholar] [CrossRef]
- Herfst, S.; Imai, M.; Kawaoka, Y.; Fouchier, R.A. Avian influenza virus transmission to mammals. Curr. Top. Microbiol. Immunol. 2014, 385, 137–155. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, M.; Lee, S.; Lee, J.; Ko, G. Survival of microorganisms on antimicrobial filters and the removal efficiency of bioaerosols in an environmental chamber. J. Microbiol. Biotechnol. 2012, 22, 1288–1295. [Google Scholar] [CrossRef]
- Wenke, C.; Pospiech, J.; Reutter, T.; Altmann, B.; Truyen, U.; Speck, S. Impact of different supply air and recirculating air filtration systems on stable climate, animal health, and performance of fattening pigs in a commercial pig farm. PLoS ONE 2018, 13, e0194641. [Google Scholar] [CrossRef] [PubMed]
- Guillard, C.; Bui, T.H.; Felix, C.; Moules, V.; Lina, B.; Lejeune, P. Microbiological disinfection of water and air by photocatalysis. Comptes Rendus Chim. 2008, 11, 107–113. [Google Scholar] [CrossRef]
- McDevitt, J.J.; Rudnick, S.N.; Radonovich, L.J. Aerosol susceptibility of influenza virus to UV-C light. Appl. Environ. Microbiol. 2012, 78, 1666–1669. [Google Scholar] [CrossRef]
- Megahed, N.A.; Ghoneim, E.M. Indoor Air Quality: Rethinking rules of building design strategies in post-pandemic architecture. Environ. Res. 2021, 193, 110471. [Google Scholar] [CrossRef]
- Song, L.; Zhou, J.; Wang, C.; Meng, G.; Li, Y.; Jarin, M.; Wu, Z.; Xie, X. Airborne pathogenic microorganisms and air cleaning technology development: A review. J. Hazard. Mater. 2022, 424, 127429. [Google Scholar] [CrossRef]
- Usachev, E.V.; Pyankov, O.V.; Usacheva, O.V.; Agranovski, I.E. Antiviral activity of tea tree and eucalyptus oil aerosol and vapour. J. Aerosol. Sci. 2013, 59, 22–30. [Google Scholar]
- Huang, Y.; Hung, Y.; Hsu, S.; Huang, Y.; Hwang, D. Application of electrolyzed water in the food industry. Food Control 2008, 19, 329–345. [Google Scholar]
- Kormányos, B.; Nagypál, I.; Peintler, G.; Horváth, A. Effect of Chloride Ion on the Kinetics and Mechanism of the Reaction between Chlorite Ion and Hypochlorous Acid. Inorg. Chem. 2008, 47, 7914–7920. [Google Scholar]
- Len, S.; Hung, Y.; Chung, D.; Anderson, J.; Erickson, M.; Morita, K. Effects of storage conditions and pH on chlorine loss in electrolyzed oxidizing (EO) water. J. Agric. Food Chem. 2002, 50, 209–212. [Google Scholar] [CrossRef]
- Ayebah, B.; Hung, Y. Electrolyzed water and its corrosiveness on various surface materials commonly found in food processing facilities. J. Food Process. Eng. 2005, 28, 247–264. [Google Scholar] [CrossRef]
- Sun, J.; Jiang, X.; Chen, Y.; Lin, M.; Tang, J.; Lin, Q.; Fang, L.; Li, M.; Hung, Y.C.; Lin, H. Recent trends and applications of electrolyzed oxidizing water in fresh foodstuff preservation and safety control. Food Chem. 2022, 369, 130873. [Google Scholar] [CrossRef]
- Jemni, M.; Otón, M.; Ramirez, J.G.; Artés-Hernández, F.; Chaira, N.; Ferchichi, A.; Artés, F. Conventional and emergent sanitizers decreased Ectomyelois ceratoniae infestation and maintained quality of date palm after shelf-life. Postharvest Biol. Technol. 2014, 87, 33–41. [Google Scholar] [CrossRef]
- Vásquez-López, A.; Villarreal-Barajas, T.; Rodríguez-Ortiz, G. Effectiveness of Neutral Electrolyzed Water on Incidence of Fungal Rot on Tomato Fruits (Solanum lycopersicum L.). J. Food Prot. 2016, 79, 1802–1806. [Google Scholar] [CrossRef]
- Tamaki, S.; Bui, V.N.; Ngo, L.H.; Ogawa, H.; Imai, K. Virucidal effect of acidic electrolyzed water and neutral electrolyzed water on avian influenza viruses. Arch. Virol. 2014, 159, 405–412. [Google Scholar] [CrossRef]
- Lee, J.H.; Rhee, P.L.; Kim, J.H.; Kim, J.J.; Paik, S.W.; Rhee, J.C.; Song, J.H.; Yeom, J.S.; Lee, N.Y. Efficacy of electrolyzed acid water in reprocessing patient-used flexible upper endoscopes: Comparison with 2% alkaline glutaraldehyde. J. Gastroenterol. Hepatol. 2004, 19, 897–903. [Google Scholar] [CrossRef]
- Urushidani, M.; Kawayoshi, A.; Kotaki, T.; Saeki, K.; Mori, Y.; Kameoka, M. Inactivation of SARS-CoV-2 and influenza A virus by dry fogging hypochlorous acid solution and hydrogen peroxide solution. PLoS ONE 2022, 17, e0261802. [Google Scholar] [CrossRef]
- Chuang, C.; Yang, S.; Chang, M.; Huang, H.; Luo, C.; Fang, W.; Hung, P.; Chung, P. Applying the Membrane-Less Electrolyzed Water Spraying for Inactivating Bioaerosols. Aerosol Air Qual. Res. 2013, 13, 350–359. [Google Scholar] [CrossRef]
- Chuang, C.; Yang, S.; Chang, M.; Huang, H.; Luo, C.; Hung, P.; Fang, W. Inactivation efficiency to Bacillus subtilis and Escherichia coli bacterial aerosols of spraying neutral electrolyzed water. J. Air Waste Manag. Assoc. 2013, 63, 1447–1456. [Google Scholar] [CrossRef]
- WHO. Manual for the Laboratory Diagnosis and Virological Surveillance of Influenza; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- WHO. Manual on Animal Influenza Diagnosis and Surveillance; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Hogan, C.; Kettleson, E.; Lee, M.H.; Ramaswami, B.; Angenent, L.; Biswas, P. Sampling methodologies and dosage assessment techniques for submicrometre and ultrafine virus aerosol particles. J. Appl. Microbiol. 2005, 99, 1422–1434. [Google Scholar]
- Verreault, D.; Moineau, S.; Duchaine, C. Methods for sampling of airborne viruses. Microbiol. Mol. Biol. Rev. 2008, 72, 413–444. [Google Scholar] [CrossRef]
- Chuang, C.-Y.; Hsu, Y.-F.; Hung, P.-C.; Dai, Y.-T.; Yang, S. Evaluation of the Inactivating Ability of Carbon-Nanotube Coated Plasma Treatment on Bioaerosols for Indoor Air Cleaning. Coatings 2022, 12, 1497. [Google Scholar] [CrossRef]
- Pica, N.; Bouvier, N.M. Environmental factors affecting the transmission of respiratory viruses. Curr. Opin. Virol. 2012, 2, 90–95. [Google Scholar] [CrossRef]
- Gralton, J.; Tovey, E.; McLaws, M.-L.; Rawlinson, W.D. The role of particle size in aerosolised pathogen transmission: A review. J. Infect. 2011, 62, 1–13. [Google Scholar] [CrossRef]
- Oswin, H.P.; Haddrell, A.E.; Otero-Fernandez, M.; Mann, J.F.S.; Cogan, T.A.; Hilditch, T.G.; Tian, J.; Hardy, D.A.; Hill, D.J.; Finn, A.; et al. The dynamics of SARS-CoV-2 infectivity with changes in aerosol microenvironment. Proc. Natl. Acad. Sci. USA 2022, 119, e2200109119. [Google Scholar] [CrossRef]
- Abadias, M.; Usall, J.; Oliveira, M.; Alegre, I.; Vinas, I. Efficacy of neutral electrolyzed water (NEW) for reducing microbial contamination on minimally-processed vegetables. Int. J. Food Microbiol. 2008, 123, 151–158. [Google Scholar] [CrossRef]
- Zhao, Y.; Xin, H.; Zhao, D.; Zheng, W.; Tian, W.; Ma, H.; Liu, K.; Hu, H.; Wang, T.; Soupir, M. Free chlorine loss during spraying of membraneless acidic electrolyzed water and its antimicrobial effect on airborne bacteria from poultry house. Ann. Agric. Environ. Med. 2014, 21, 249–255. [Google Scholar] [CrossRef]
- Thorn, R.M.S.; Lee, S.W.H.; Robinson, G.M.; Greenman, J.; Reynolds, D.M. Electrochemically activated solutions: Evidence for antimicrobial efficacy and applications in healthcare environments. Eur. J. Clin. Microbiol. 2012, 31, 641–653. [Google Scholar] [CrossRef]
- Oomori, T.; Oka, T.; Inuta, T.; Arata, Y. The efficiency of disinfection of acidic electrolyzed water in the presence of organic materials. Anal. Sci. 2000, 16, 365–370. [Google Scholar] [CrossRef]
- Block, M.S.; Rowan, B.G. Hypochlorous Acid: A Review. J. Oral Maxillofac. Surg. 2020, 78, 1461–1466. [Google Scholar] [CrossRef]
- Morita, C.; Nishida, T.; Ito, K. Biological toxicity of acid electrolyzed functional water: Effect of oral administration on mouse digestive tract and changes in body weight. Arch. Oral Biol. 2011, 56, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, Y.; Harata, Y.; Mizuhashi, F.; Nakajima, M.; Miwa, N. Biological safety of neutral-pH hydrogen-enriched electrolyzed water upon mutagenicity, genotoxicity and subchronic oral toxicity. Toxicol. Ind. Health 2010, 26, 203–216. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.; Chuang, C.-Y.; Huang, H.-C.; Fang, W. Inactivation of Avian Influenza Virus Aerosol Using Membrane-Less Electrolyzed Water Spraying. Aerobiology 2023, 1, 70-81. https://doi.org/10.3390/aerobiology1020006
Yang S, Chuang C-Y, Huang H-C, Fang W. Inactivation of Avian Influenza Virus Aerosol Using Membrane-Less Electrolyzed Water Spraying. Aerobiology. 2023; 1(2):70-81. https://doi.org/10.3390/aerobiology1020006
Chicago/Turabian StyleYang, Shinhao, Chi-Yu Chuang, Hsiao-Chien Huang, and Wei Fang. 2023. "Inactivation of Avian Influenza Virus Aerosol Using Membrane-Less Electrolyzed Water Spraying" Aerobiology 1, no. 2: 70-81. https://doi.org/10.3390/aerobiology1020006