Interrater Reliability of 99mTc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children
Abstract
:1. Introduction
2. Materials and Methods
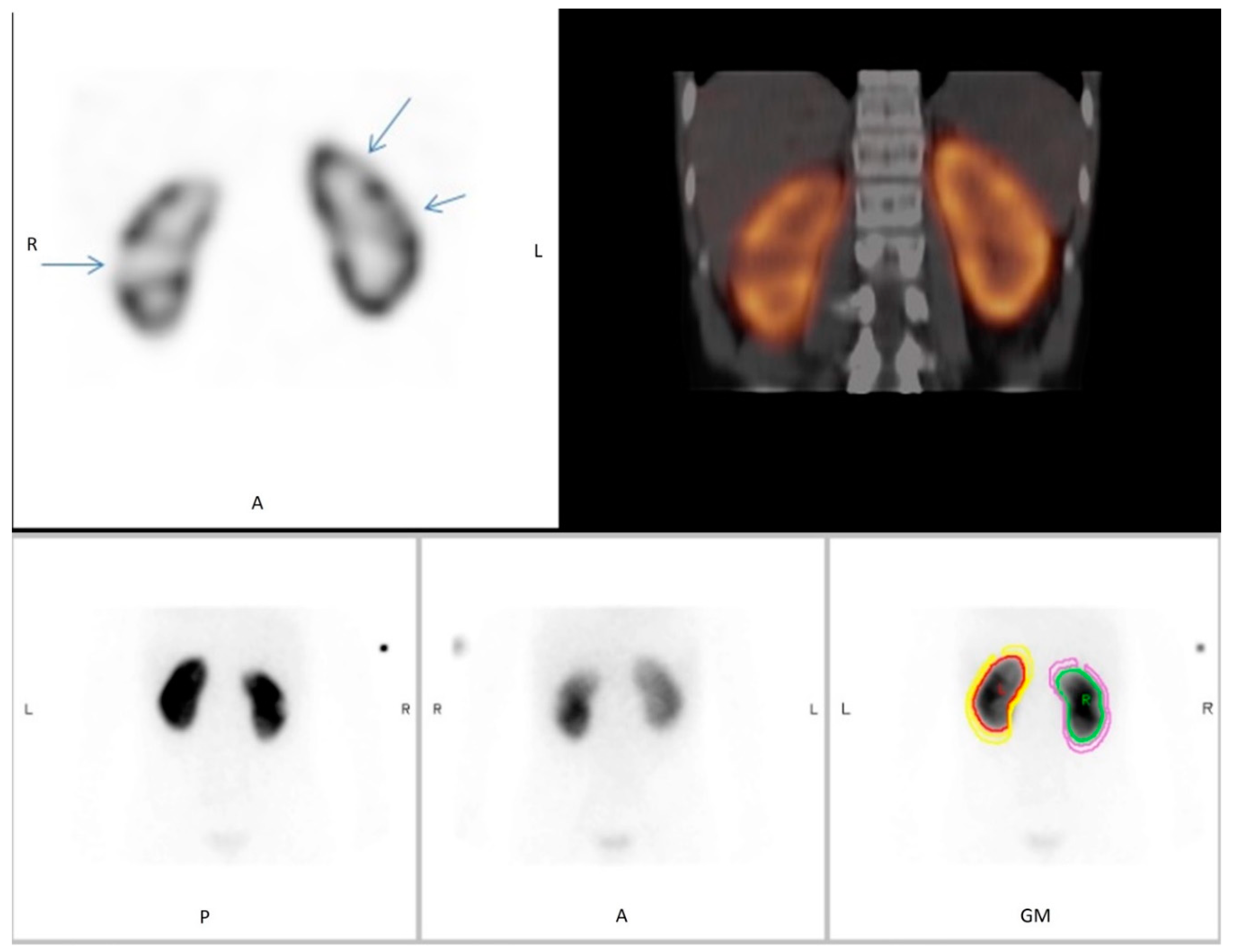
2.1. Scan Protocols and Reconstruction Methods
2.2. DMSA Scintigraphy Readings
2.3. Statistics
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lim, R. Vesicoureteral reflux and urinary tract infection: Evolving practices and current controversies in pediatric imaging. Am. J. Roentgenol. 2009, 192, 1197–1208. [Google Scholar] [CrossRef] [PubMed]
- Mendichovszky, I.; Solar, B.T.; Smeulders, N.; Easty, M.; Biassoni, L. Nuclear medicine in pediatric nephro-urology: An overview. Semin. Nucl. Med. 2017, 47, 204–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piepsz, A.; Colarinha, P.; Gordon, I.; Hahn, K.; Olivier, P.; Roca, I.; Sixt, R.; van Velzen, J. Revised Guidelines on 99mTc-DMSA Scintigraphy in Children. European Association of Nuclear Medicine. Available online: https://eanm.org/publications/guidelines/gl_paed_dmsa_scin.pdf (accessed on 3 October 2009).
- Kim, G.E.; Park, J.H.; Kim, J.S.; Won, K.S.; Kim, H.W. Comparison of Tc-99m DMSA renal planar scan and SPECT for detection of cortical defects in infants with suspected acute pyelonephritis. Indian J. Pediatr. 2019, 86, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Bagni, B.; Orsolon, P.; Fattori, A.; Guerra, U.P. Renal SPECT with Tc-99m DMSA in children with upper urinary tract infections using a triple-headed gamma camera. Clin. Nucl. Med. 1997, 22, 838–843. [Google Scholar] [CrossRef] [PubMed]
- Brenner, M.; Bonta, D.; Eslamy, H.; Ziessman, H.A. Comparison of 99mTc-DMSA dual-head SPECT versus high-resolution parallel-hole planar imaging for the detection of renal cortical defects. Am. J. Roentgenol. 2009, 193, 333–337. [Google Scholar] [CrossRef] [PubMed]
- European Association of Nuclear Medicine Dosage Calculator. Available online: https://www.eanm.org/publications/dosage-calculator (accessed on 1 November 2008).
- Reichkendler, M.H.; Berg, R.M.G.; de Nijs, R.; Nørgaard, H.; Schmidt, I.M.; Borgwardt, L. Planar scan vs. SPECT/low-dose CT for estimating split renal function by 99mTc-DMSA scintigraphy in children. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 729–733. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Everaert, H.; Flamen, P.; Franken, P.R.; Peeters, P.; Bossuyt, A.; Piepsz, A. 99Tcm-DMSA renal scintigraphy for acute pyelonephritis in adults: Planar and/or SPET imaging? Nucl. Med. Commun. 1996, 17, 884–889. [Google Scholar] [CrossRef] [PubMed]
- Beslic, N.; Milardovic, R.; Sadija, A.; Dzananovic, L.; Cavaljuga, S. Interobserver variability in interpretation of planar and SPECT Tc-99m-DMSA renal scintigraphy in children. Acta Inform. Med. 2017, 25, 28–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Reader 1 | Reader 2 | |
|---|---|---|
| Planar Scintigraphy | ||
| Evidence of renal scarring | 20 (43%) | 7 (15%) |
| No evidence of renal scarring | 26 (57%) | 39 (85%) |
| Unconfident about diagnosis | 16 (35%) | 20 (43%) |
| SPECT/ldCT | ||
| Evidence of renal scarring | 13 (28%) | 12 (26%) |
| No evidence of renal scarring | 33 (72%) | 34 (74%) |
| Unconfident about diagnosis | 1 (2%) | 4 (9%) |
| Planar Scintigraphy vs. SPECT/ldCT | ||
| Concordant diagnoses between modalities | 37 (85%) | 35 (76%) |
| Evidence of renal scarring | 12 (32%) | 4 (11%) |
| No evidence of renal scarring | 25 (68%) | 31 (89%) |
| Discordant diagnoses between modalities | 9 (15%) | 11 (24%) |
| Evidence of renal scarring on planar scintigraphy No evidence on SPECT/ldCT | 8 (89%) | 3 (27%) |
| No evidence of renal scarring on planar scintigraphy Evidence on SPECT/ldCT | 1 (11%) | 8 (73%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Einarsdóttir, H.S.; Berg, R.M.G.; Borgwardt, L. Interrater Reliability of 99mTc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children. Diagnostics 2020, 10, 1101. https://doi.org/10.3390/diagnostics10121101
Einarsdóttir HS, Berg RMG, Borgwardt L. Interrater Reliability of 99mTc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children. Diagnostics. 2020; 10(12):1101. https://doi.org/10.3390/diagnostics10121101
Chicago/Turabian StyleEinarsdóttir, Hrefna Sæunn, Ronan Martin Griffin Berg, and Lise Borgwardt. 2020. "Interrater Reliability of 99mTc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children" Diagnostics 10, no. 12: 1101. https://doi.org/10.3390/diagnostics10121101
APA StyleEinarsdóttir, H. S., Berg, R. M. G., & Borgwardt, L. (2020). Interrater Reliability of 99mTc-DMSA Scintigraphy Performed as Planar Scan vs. SPECT/Low Dose CT for Diagnosing Renal Scarring in Children. Diagnostics, 10(12), 1101. https://doi.org/10.3390/diagnostics10121101





