Evaluation of a Locking Autocompression Screw Model in Pauwels Type-3 Femoral Neck Fracture: In Vitro Analysis
Abstract
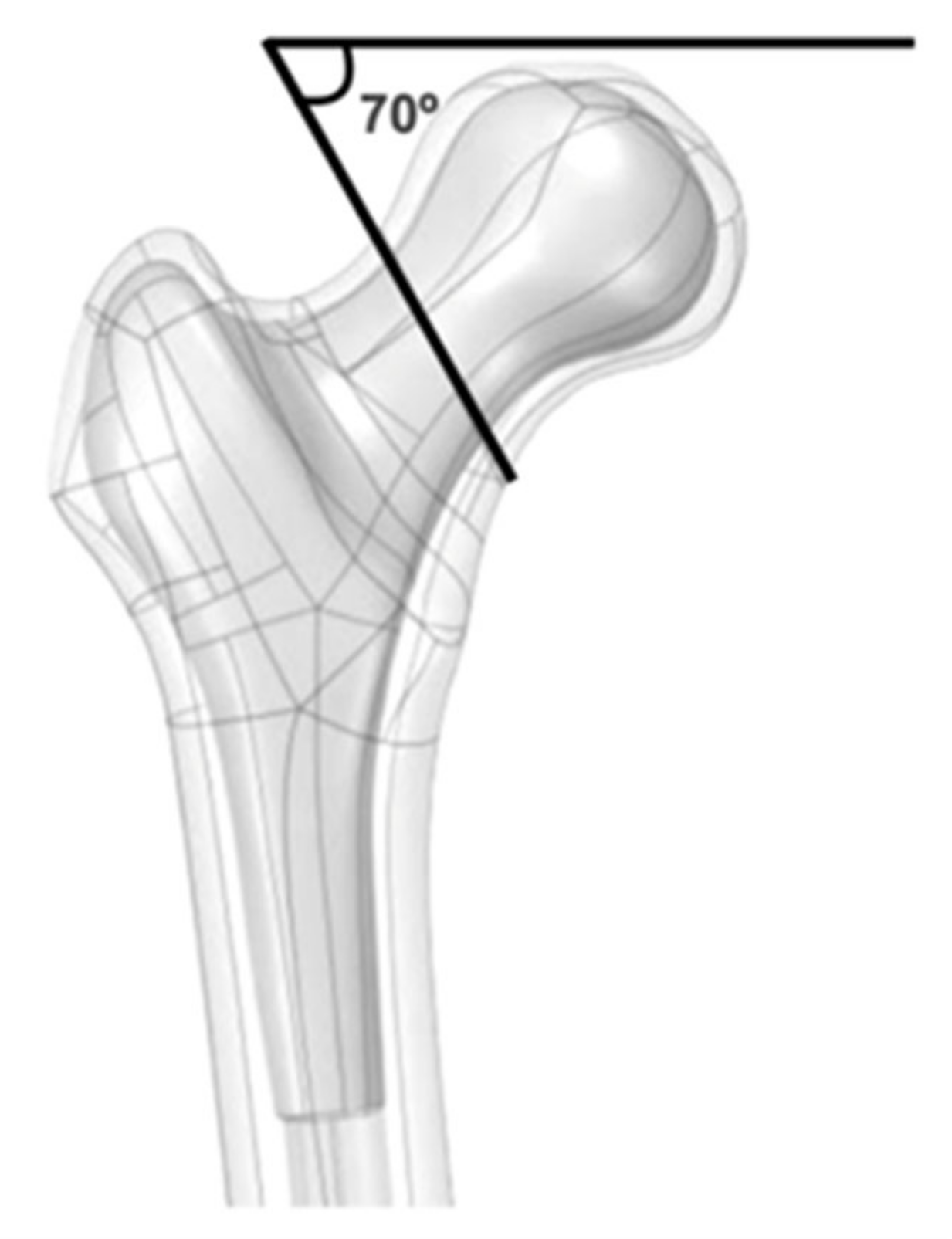
:1. Introduction
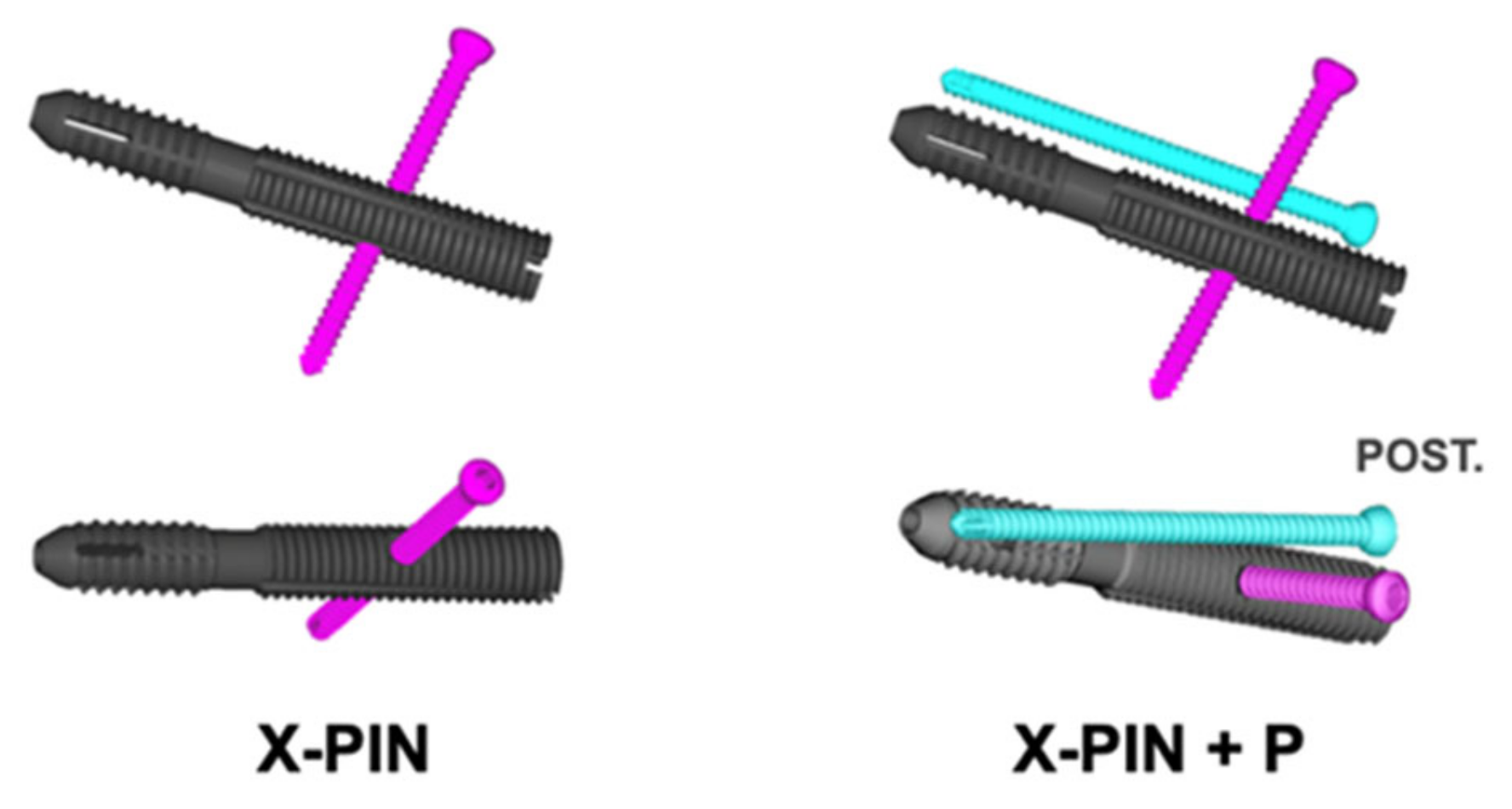
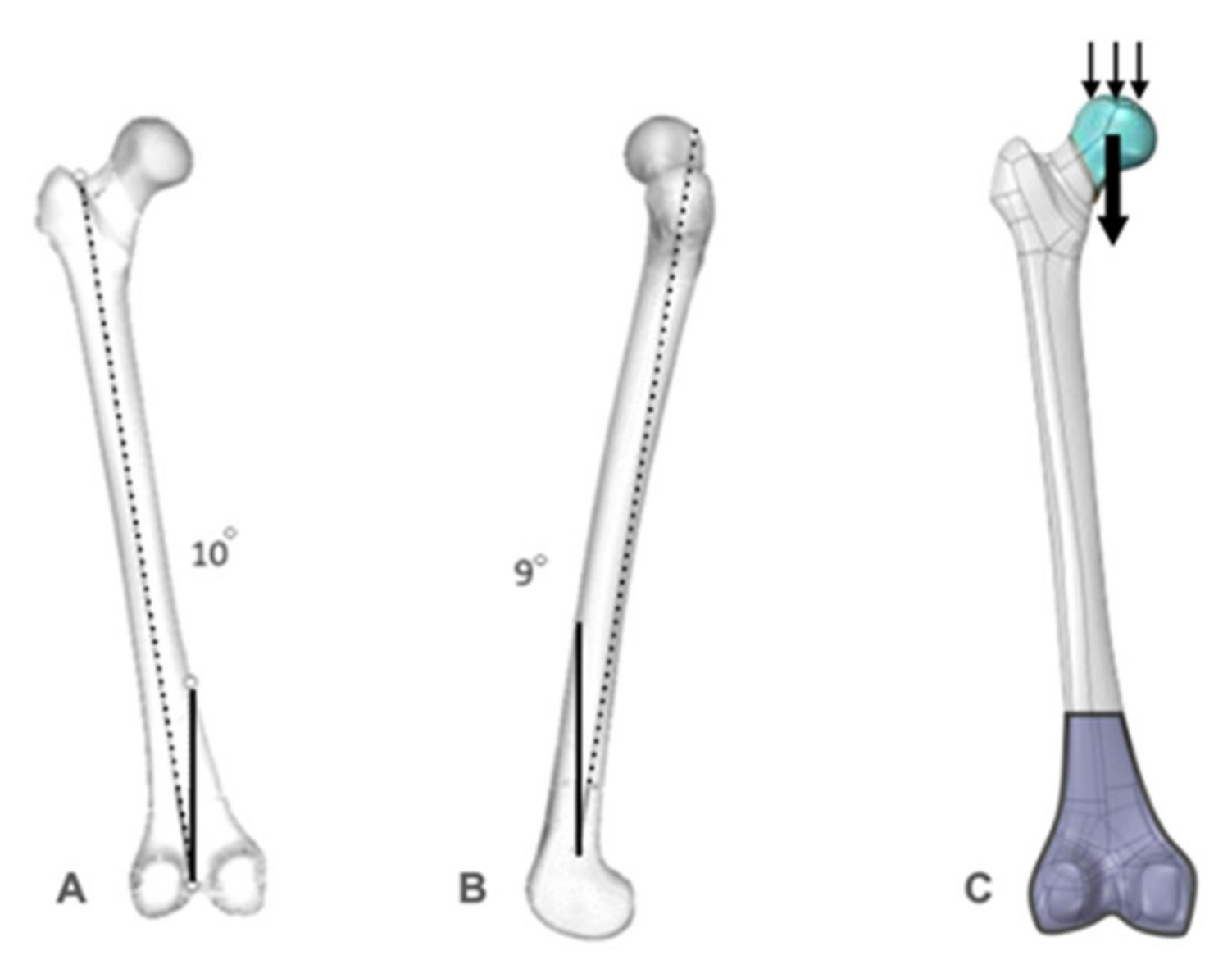
2. Materials and Methods
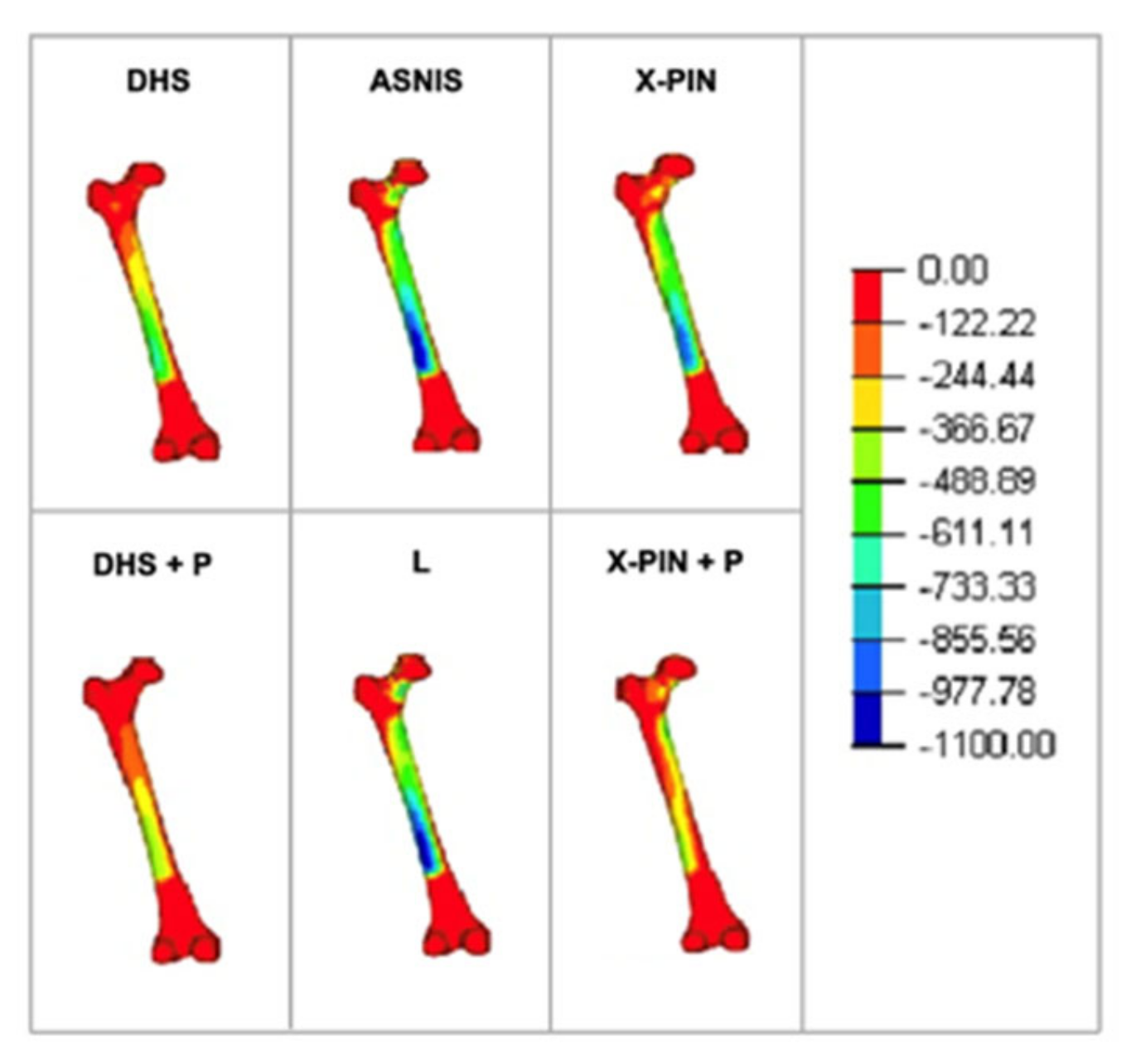
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoskins, W.; Rayner, J.; Sheehy, R.; Claireaux, H.; Bingham, R.; Santos, R.; Bucknill, A.; Griffin, X.L. The effect of patient, fracture and surgery on outcomes of high energy neck of femur fractures in patients aged 15–50. Hip Int. 2019, 29, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Ly, T.V.; Swiontkowski, M.F. Management of femoral neck fractures in young adults. Indian J. Orthop. 2008, 42, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Shen, M.; Wang, C.; Chen, H.; Rui, Y.F.; Zhao, S. An update on the Pauwels classification. J. Orthop. Surg. Res. 2016, 11, 161. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J. Bone Jt. Surg. 2009, 91, 490–491. [Google Scholar]
- Haidukewych, G.J.; Rothwell, W.S.; Jacofsky, D.J.; Torchia, M.E.; Berry, D.J. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. J. Bone Jt. Surg. 2004, 86, 1711–1716. [Google Scholar] [CrossRef] [PubMed]
- Bartonicek, J. Pauwels’ classification of femoral neck fractures: Correct interpretation of the original. J. Orthop. Trauma 2001, 15, 358–360. [Google Scholar] [CrossRef] [PubMed]
- Cha, Y.H.; Yoo, J.I.; Hwang, S.Y.; Kim, K.J.; Kim, H.Y.; Choy, W.S.; Hwang, S.C. Biomechanical evaluation of internal fixation of pauwels type III femoral neck fractures: A systematic review of various fixation methods. Clin. Orthop. Surg. 2019, 11, 1–14. [Google Scholar] [CrossRef]
- Slobogean, G.P.; Sprague, S.A.; Scott, T.; Bhandari, M. Complications following young femoral neck fractures. Injury 2015, 46, 484–491. [Google Scholar] [CrossRef]
- Panteli, M.; Rodham, P.; Giannoudis, P.V. Biomechanical rationale for implant choices in femoral neck fracture fixation in the non-elderly. Injury 2015, 46, 445–452. [Google Scholar] [CrossRef]
- Giordano, V.; Alves, D.D.; Paes, R.P.; Amaral, A.B.; Giordano, M.; Belangero, W.; Freitas, A.; Koch, H.A.; do Amaral, N.P. The role of the medial plate for Pauwels type III femoral neck fracture: A comparative mechanical study using two fixations with cannulated screws. J. Exp. Orthop. 2019, 6, 18. [Google Scholar] [CrossRef]
- Imren, Y.; Gurkan, V.; Bilsel, K.; Desteli, E.E.; Tuna, M.; Gurcan, C.; Tuncay, I.; Sen, C. Biomechanical comparison of dynamic hip screw, proximal femoral nail, cannulated screw, and monoaxial external fixation in the treatment of basicervical femoral neck fractures. Acta Chir. Orthop. Traumatol. Cech. 2015, 82, 140–144. [Google Scholar] [CrossRef]
- Roderer, G.; Moll, S.; Gebhard, F.; Claes, L.; Krischak, G. Side plate fixation vs. intramedullary nailing in an unstable medial femoral neck fracture model: A comparative biomechanical study. Clin. Biomech. 2011, 26, 141–146. [Google Scholar] [CrossRef]
- Rupprecht, M.; Grossterlinden, L.; Ruecker, A.H.; de Oliveira, A.N.; Sellenschloh, K.; Nuchtern, J.; Puschel, K.; Morlock, M.; Rueger, J.M.; Lehmann, W. A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: The Intertan versus cannulated screws or a dynamic hip screw. J. Trauma Acute Care Surg. 2011, 71, 625–634. [Google Scholar] [CrossRef]
- Giordano, V.; Paes, R.P.; Alves, D.D.; Amaral, A.B.; Belangero, W.D.; Giordano, M.; Freitas, A.; Koch, H.A. Stability of L-shaped and inverted triangle fixation assemblies in treating Pauwels type II femoral neck fracture: A comparative mechanical study. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 1359–1367. [Google Scholar] [CrossRef]
- Bonnaire, F.A.; Weber, A.T. Analysis of fracture gap changes, dynamic and static stability of different osteosynthetic procedures in the femoral neck. Injury 2002, 33 (Suppl. 3), 24–32. [Google Scholar] [CrossRef]
- Chan, D.S. Femoral neck fractures in young patients: State of the art. J. Orthop. Trauma 2019, 33, S7–S11. [Google Scholar] [CrossRef]
- Davidovitch, R.I.; Jordan, C.J.; Egol, K.A.; Vrahas, M.S. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J. Trauma Acute Care Surg. 2010, 68, 236–242. [Google Scholar] [CrossRef]
- Swiontkowski, M.F. Intracapsular fractures of the hip. J. Bone Jt. Surg. Am. 1994, 76, 129–138. [Google Scholar] [CrossRef]
- Aminian, A.; Gao, F.; Fedoriw, W.W.; Zhang, L.Q.; Kalainov, D.M.; Merk, B.R. Vertically oriented femoral neck fracture: Mechanical analysis of four fixation techniques. J. Orthop. Trauma 2007, 21, 544–548. [Google Scholar] [CrossRef]
- Liporace, F.; Gaines, R.; Collinge, C.; Haidukewych, G.J. Results of internal fixation of Pauwels type-3 vertical femoral neck fractures. J. Bone Jt. Surg. Am. 2008, 90, 1654–1659. [Google Scholar] [CrossRef]
- Gardner, M.P.; Chong, A.C.; Pollock, A.G.; Wooley, P.H. Mechanical evaluation of large-size fourth-generation composite femur and tibia models. Ann. Biomed. Eng. 2010, 38, 613–620. [Google Scholar] [CrossRef]
- Okolie, O.; Stachurek, I.; Kandasubramanian, B.; Njuguna, J. Material challenges and opportunities in 3D printing for hip implant applications. Recent Prog. Mater. 2022, 4, 004. [Google Scholar] [CrossRef]
- Pfeiffer, F.M. The use of finite element analysis to enhance research and clinical practice in orthopedics. J. Knee Surg. 2016, 29, 149–158. [Google Scholar] [CrossRef]
- Oefner, C.; Herrmann, S.; Kebbach, M.; Lange, H.E.; Kluess, D.; Woiczinski, M. Reporting checklist for verification and validation of finite element analysis in orthopedic and trauma biomechanics. Med. Eng. Phys. 2021, 92, 25–32. [Google Scholar] [CrossRef]
- Ye, Y.; Hao, J.; Mauffrey, C.; Hammerberg, E.M.; Stahel, P.F.; Hak, D.J. Optimizing stability in femoral neck fracture fixation. Orthopedics 2015, 38, 625–630. [Google Scholar] [CrossRef]
- Noda, M.; Saegusa, Y.; Takahashi, M.; Tezuka, D.; Adachi, K.; Naoi, K. Biomechanical study using the finite element method of internal fixation in pauwels type III vertical femoral neck fractures. Arch. Trauma Res. 2015, 4, e23167. [Google Scholar] [CrossRef]
- Samsami, S.; Saberi, S.; Sadighi, S.; Rouhi, G. Comparison of three fixation methods for femoral neck fracture in young adults: Experimental and numerical investigations. J. Med. Biol. Eng. 2015, 35, 566–579. [Google Scholar] [CrossRef]
- Moon, J.K.; Lee, J.I.; Hwang, K.T.; Yang, J.H.; Park, Y.S.; Park, K.C. Biomechanical comparison of the femoral neck system and the dynamic hip screw in basicervical femoral neck fractures. Sci. Rep. 2022, 12, 7915. [Google Scholar] [CrossRef] [PubMed]
- Davidson, A.; Blum, S.; Harats, E.; Kachko, E.; Essa, A.; Efraty, R.; Peyser, A.; Giannoudis, P.V. Neck of femur fractures treated with the femoral neck system: Outcomes of one hundred and two patients and literature review. Int. Orthop. 2022, 46, 2105–2115. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.; Barin, F.R.; Battaglion, L.R.; da Costa, H.I.; Santos, E.D.; Rosado, H.A.; Giordano, M.; Giordano, V.; Shimano, A.C. Proposal for a new fixation method for pauwels type III femoral neck fracture-metaphyseal stem: A finite-element analysis. Indian J. Orthop. 2021, 55, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Freitas, A.; Toledo Junior, J.V.; Ferreira Dos Santos, A.; Aquino, R.J.; Leao, V.N.; Pericles de Alcantara, W. Biomechanical study of different internal fixations in Pauwels type III femoral neck fracture—A finite elements analysis. J. Clin. Orthop. Trauma 2021, 14, 145–150. [Google Scholar] [CrossRef]
- Lim, E.J.; Shon, H.C.; Cho, J.W.; Oh, J.K.; Kim, J.; Kim, C.H. Dynamic hip screw versus cannulated cancellous screw in pauwels Type II or Type III femoral neck fracture: A systematic review and meta-analysis. J. Pers. Med. 2021, 11, 1017. [Google Scholar] [CrossRef]
- Zeng, W.; Liu, Y.; Hou, X. Biomechanical evaluation of internal fixation implants for femoral neck fractures: A comparative finite element analysis. Comput. Methods Programs Biomed. 2020, 196, 105714. [Google Scholar] [CrossRef]
- Augat, P.; Hast, M.W.; Schemitsch, G.; Heyland, M.; Trepczynski, A.; Borgiani, E.; Russow, G.; Märdian, S.; Duda, G.N.; Hollensteiner, M.; et al. Biomechanical models: Key considerations in study design. OTA Int. 2021, 4, e099. [Google Scholar] [CrossRef]
- Knobe, M.; Altgassen, S.; Maier, K.J.; Gradl-Dietsch, G.; Kaczmarek, C.; Nebelung, S.; Klos, K.; Kim, B.S.; Gueorguiev, B.; Horst, K.; et al. Screw-blade fixation systems in Pauwels three femoral neck fractures: A biomechanical evaluation. Int. Orthop. 2018, 42, 409–418. [Google Scholar] [CrossRef]
- Stoffel, K.; Zderic, I.; Gras, F.; Sommer, C.; Eberli, U.; Mueller, D.; Oswald, M.; Gueorguiev, B. Biomechanical evaluation of the Femoral Neck System in unstable Pauwels III femoral neck fractures: A comparison with the Dynamic Hip Screw and cannulated screws. J. Orthop. Trauma 2017, 31, 131–137. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, Y.; Feng, G.; Guo, H.; Chen, Z.; Chen, Y.; Jin, Q. Biomechanical comparison of the femoral neck system versus InterTan nail and three cannulated screws for unstable Pauwels type III femoral neck fracture. BioMed. Eng. OnLine 2022, 21, 34. [Google Scholar] [CrossRef]






| Material | Material Properties | |
|---|---|---|
| Modulus of Elasticity (MPa) | Poisson’s Coefficient (V) | |
| Cortical bone | 16,350 | 0.26 |
| Trabecular bone | 137 | 0.30 |
| Syntheses (steel) | 200,000 | 0.33 |
| Models | ||||||
|---|---|---|---|---|---|---|
| Analysis | X-PIN | X-PIN+P | DHS | DHS+P | ASNIS | L |
| Max total (MPa) | 582 | 1078 | 607 | 711 | 654.3 | 501 |
| Min total (MPa) | −856 | −959 | −765 | −517 | −276 | −597 |
| Max P1 (MPa) | 28 | 25 | 29 | 24 | 23 | 19 |
| Max P2 (MPa) | 31 | 21 | 36 | 27 | 47 | 42 |
| Total displacement. (mm) | 9 | 2.41 | 8.4 | 7.1 | 9.2 | 8.7 |
| Local displacement (mm) | 2.6 | 0.8 | 2.1 | 1.2 | 2 | 1.7 |
| Rotational displacement (mm) | 4.1 | 1.1 | 3.5 | 1.5 | 2.6 | 2.3 |
| Von Mises stress (MPa) | 988 | 1195 | 859 | 1005 | 448 | 393 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giordano, V.; Freitas, A.; Pires, R.E.; Battaglion, L.R.; Lobo, M.d.O.; Belangero, W.D. Evaluation of a Locking Autocompression Screw Model in Pauwels Type-3 Femoral Neck Fracture: In Vitro Analysis. Bioengineering 2022, 9, 464. https://doi.org/10.3390/bioengineering9090464
Giordano V, Freitas A, Pires RE, Battaglion LR, Lobo MdO, Belangero WD. Evaluation of a Locking Autocompression Screw Model in Pauwels Type-3 Femoral Neck Fracture: In Vitro Analysis. Bioengineering. 2022; 9(9):464. https://doi.org/10.3390/bioengineering9090464
Chicago/Turabian StyleGiordano, Vincenzo, Anderson Freitas, Robinson Esteves Pires, Leonardo Rigobello Battaglion, Mariana de Oliveira Lobo, and William Dias Belangero. 2022. "Evaluation of a Locking Autocompression Screw Model in Pauwels Type-3 Femoral Neck Fracture: In Vitro Analysis" Bioengineering 9, no. 9: 464. https://doi.org/10.3390/bioengineering9090464
APA StyleGiordano, V., Freitas, A., Pires, R. E., Battaglion, L. R., Lobo, M. d. O., & Belangero, W. D. (2022). Evaluation of a Locking Autocompression Screw Model in Pauwels Type-3 Femoral Neck Fracture: In Vitro Analysis. Bioengineering, 9(9), 464. https://doi.org/10.3390/bioengineering9090464








