Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Methodological Approach
2.2. Study Population and Sample Size
2.3. Variables and Inclusion Criteria
2.4. Data Quality Indicators
2.5. Statistical Analysis
2.6. Ethical Approval
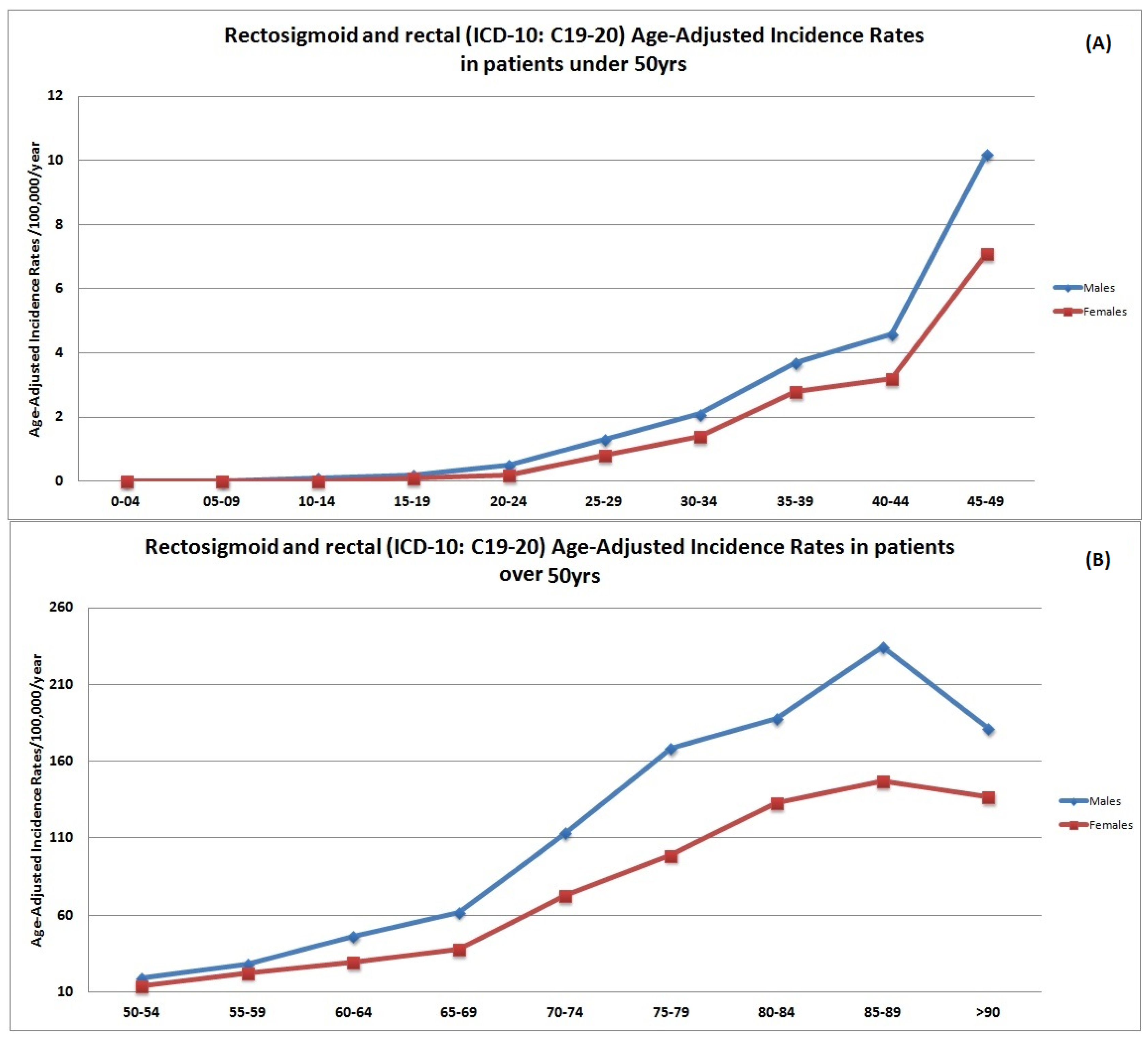
3. Results
4. Discussion
4.1. Main Findings
4.2. Reflections of the Literature
4.3. Impact on Guidelines and Health Care Policy
4.4. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Dwyer, A.J.; Murphy, C.C.; Boland, C.R.; Garcia, R.; Hampel, H.; Limburg, P.; Lowery, J.; Zauber, A.G.; Waring, S.; Worrall, S.; et al. A Summary of the Fight Colorectal Cancer Working Meeting: Exploring Risk Factors and Etiology of Sporadic Early-Age Onset Colorectal Cancer. Gastroenterology 2019, 2, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Jemal, A.; Bray, F.; Center, M.M.; Ferlay, J.; Ward, E.; Forman, D. Global cancer statistics. CA Cancer J. Clin. 2011, 2, 69–90. [Google Scholar] [CrossRef] [PubMed]
- Center, M.M.; Jemal, A.; Ward, E. International trends in colorectal cancer incidence rates. Cancer Epidemiol. Biomarkers Prev. 2009, 6, 1688–1694. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 6, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.E.; Taylor, T.H.; Pan, C.-J.G.; Stamos, M.J.; Zell, J.A. Colorectal Cancer Incidence Among Young Adults in California. J. Adolesc. Young Adult Oncol. 2014, 4, 176–184. [Google Scholar] [CrossRef]
- Kasi, P.M.; Shahjehan, F.; Cochuyt, J.J.; Li, Z.; Colibaseanu, D.T.; Merchea, A. Rising Proportion of Young Individuals with Rectal and Colon Cancer. Clin. Color. Cancer 2019, 18, 87–95. [Google Scholar] [CrossRef]
- Liu, P.H.; Wu, K.; Ng, K.; Zauber, A.G.; Nguyen, L.H.; Song, M.; He, X.; Fuchs, C.S.; Ogino, S.; Willett, W.C.; et al. Association of Obesity with Risk of Early-Onset Colorectal Cancer among Women. JAMA Oncol. 2019, 1, 37–44. [Google Scholar] [CrossRef]
- Murphy, N.; Campbell, P.T.; Gunter, M.J. Unraveling the Etiology of Early-Onset Colorectal Cancer. J. Natl. Cancer Inst. 2021, 5, 505–506. [Google Scholar] [CrossRef]
- O’Sullivan, D.E.; Sutherland, R.L.; Town, S.; Chow, K.; Fan, J.; Forbes, N.; Heitman, S.J.; Hilsden, R.J.; Brenner, D.R. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2022, 6, 1229–1240. [Google Scholar] [CrossRef]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 4, 683–691. [Google Scholar] [CrossRef]
- Wolf, A.; Fontham, E.; Church, T.R.; Flowers, C.R.; Guerra, C.E.; LaMonte, S.J.; Etzioni, R.; McKenna, M.T.; Oeffinger, K.C.; Shih, Y.T.; et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J. Clin. 2018, 4, 250–281. [Google Scholar] [CrossRef]
- Abdelsattar, Z.M.; Wong, S.L.; Regenbogen, S.E.; Jomaa, D.M.; Hardiman, K.M.; Hendren, S. Colorectal cancer outcomes and treatment patterns in patients too young for average-risk screening. Cancer 2016, 6, 929–934. [Google Scholar] [CrossRef]
- Hussan, H.; Patel, A.; Le Roux, M.; Cruz-Monserrate, Z.; Porter, K.; Clinton, S.K.; Carethers, J.M.; Courneya, K.S. Rising Incidence of Colorectal Cancer in Young Adults Corresponds with Increasing Surgical Resections in Obese Patients. Clin. Transl. Gastroenterol. 2020, 4, e00160. [Google Scholar] [CrossRef]
- Chatzea, V.E.; Sifaki-Pistolla, D.; Koinis, F.; Saloustros, E.; Vamvakas, L.; Pitsoulis, G.; Tzanakis, N.; Mavroudis, D.; Georgoulias, V.; Lionis, C. Cancer incidence and mortality trends in Crete, Greece during the last two decades (1992–2013): Results from the cancer registry of Crete. Ann. Oncol. 2017, 28, v516. [Google Scholar] [CrossRef]
- Bray, F.; Parkin, D.M. Evaluation of data quality in the cancer registry: Principles and methods. Part I: Comparability, validity and timeliness. Eur. J. Cancer 2009, 5, 747–755. [Google Scholar] [CrossRef]
- Sifaki-Pistolla, D.; Koinis, F.; Chatzea, V.E.; Lionakis, S.; Epitropaki, K.; Vasilaki, E.; Romanidou, T.; Kouroupi, M.; Frouzi, E.; Georgoulias, V.; et al. Towards developing evidence-based GIS-driven infrastructure for cancer surveillance in Greece. Eur. J. Public Health 2016, 26, ckw171.028. [Google Scholar] [CrossRef]
- Sifaki-Pistolla, D.; Lionis, C.; Georgoulias, V.; Kyriakidis, P.; Koinis, F.; Aggelaki, S.; Tzanakis, N. Lung cancer and tobacco smoking in Crete, Greece: Reflections from a population-based cancer registry from 1992 to 2013. Tob. Induc. Dis. 2017, 1, 6. [Google Scholar] [CrossRef]
- Sifaki-Pistolla, D.; Lionis, C.; Koinis, F.; Georgoulias, V.; Tzanakis, N. Lung cancer and annual mean exposure to outdoor air pollution in Crete, Greece. Eur. J. Cancer Prev. 2017, 26, S208–S214. [Google Scholar] [CrossRef]
- Ahmad, O.B.; Boschi-Pinto, C.; Lopez, A.D.; Murray, C.J.L.; Lozano, R.; Inoue, M. Age Standardization of Rates: A New WHO Standard; GPE Discussion Paper Series; World Health Organization: Geneva, Switzerland, 2001; Available online: https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf (accessed on 12 September 2022).
- Riebler, A.; Held, L. Projecting the future burden of cancer: Bayesian age–period–cohort analysis with integrated nested Laplace approximations. Biom. J. 2017, 59, 531–549. [Google Scholar] [CrossRef]
- Stel, V.S.; Dekker, F.W.; Tripepi, G.; Zoccali, C.; Jager, K.J. Survival analysis I: The Kaplan-Meier method. Nephron-Clin. Pract. 2011, 1, c83–c88. [Google Scholar] [CrossRef] [PubMed]
- Vuik, F.E.; Nieuwenburg, S.A.; Bardou, M.; Lansdorp-Vogelaar, I.; Dinis-Ribeiro, M.; Bento, M.J.; Zadnik, V.; Pellisé, M.; Esteban, L.; Kaminski, M.F.; et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 2019, 10, 1820–1826. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Torre, L.A.; Soerjomataram, I.; Hayes, R.B.; Bray, F.; Weber, T.K.; Jemal, A. Global patterns and trends in colorectal cancer incidence in young adults. Gut 2019, 12, 2179–2185. [Google Scholar] [CrossRef] [PubMed]
- Schreuders, E.H.; Ruco, A.; Rabeneck, L.; Schoen, R.E.; Sung, J.J.; Young, G.P.; Kuipers, E.J. Colorectal cancer screening: A global overview of existing programmes. Gut 2015, 10, 1637–1649. [Google Scholar] [CrossRef]
- Krämer, H.U.; Schöttker, B.; Raum, E.; Brenner, H. Type 2 diabetes mellitus and colorectal cancer: Meta-analysis on sex-specific differences. Eur. J. Cancer 2012, 9, 1269–1282. [Google Scholar] [CrossRef]
- Parajuli, R.; Bjerkaas, E.; Tverdal, A.; Le Marchand, L.; Weiderpass, E.; Gram, I.T. Smoking increases rectal cancer risk to the same extent in women as in men: Results from a Norwegian cohort study. BMC Cancer 2014, 1, 321. [Google Scholar] [CrossRef]
- Lewandowska, A.; Rudzki, G.; Lewandowski, T.; Stryjkowska-Góra, A.; Rudzki, S. Title: Risk Factors for the Diagnosis of Colorectal Cancer. Cancer Control 2022, 29, 10732748211056692. [Google Scholar] [CrossRef]
- Fedirko, V.; Tramacere, I.; Bagnardi, V.; Rota, M.; Scotti, L.; Islami, F.; Negri, E.; Straif, K.; Romieu, I.; La Vecchia, C.; et al. Alcohol drinking and colorectal cancer risk: An overall and dose-Response meta-analysis of published studies. Ann. Oncol. 2011, 9, 1958–1972. [Google Scholar] [CrossRef]
- Duijster, J.; Mughini-Gras, L.; Neefjes, J.; Franz, E. Occupational exposure and risk of colon cancer: A nationwide registry study with emphasis on occupational exposure to zoonotic gastrointestinal pathogens. BMJ Open 2021, 11, e050611. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Theodoridis, X.; Chourdakis, M. International aspects: Abdominal obesity in Greece. In Nutrition in the Prevention and Treatment of Abdominal Obesity; Academic Press: Cambridge, MA, USA, 2019; pp. 301–316. [Google Scholar]
- Tourlouki, E.; Matalas, A.L.; Bountziouka, V.; Tyrovolas, S.; Zeimbekis, A.; Gotsis, E.; Tsiligianni, I.; Protopapa, I.; Protopapas, C.; Metallinos, G.; et al. Are Current Dietary Habits in Mediterranean Islands a Reflection of the Past? Results from the MEDIS Study. Ecol. Food Nutr. 2013, 5, 371–386. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Risvas, G.; Kontogianni, M.D.; Zampelas, A.; Stefanadis, C. Epidemiology of overweight and obesity in a Greek adult population: The ATTICA study. Obes. Res. 2004, 12, 1914–1920. [Google Scholar] [CrossRef]
- Tzotzas, T.; Kapantais, E.; Tziomalos, K.; Ioannidis, I.; Mortoglou, A.; Bakatselos, S.; Kaklamanou, M.; Lanaras, L.; Kaklamanos, I. Epidemiological survey for the prevalence of overweight and abdominal obesity in Greek adolescents. Obesity 2008, 7, 1718–1722. [Google Scholar] [CrossRef]
- Vassilopoulos, P.P.; Kelessis, N.; Plataniotis, G.; Gondikakis, E.; Galanos, A. Colorectal cancer trends by anatomic sides, age and staging. A twenty-year study of 1412 Greek cases. Anticancer Res. 2000, 20, 4773–4776. [Google Scholar]
- Vatandoust, S.; Price, T.J.; Ullah, S.; Roy, A.C.; Beeke, C.; Young, J.P.; Townsend, A.; Padbury, R.; Roder, D.; Karapetis, C.S. Metastatic Colorectal Cancer in Young Adults: A Study from the South Australian Population-Based Registry. Clin. Color. Cancer 2016, 1, 32–36. [Google Scholar] [CrossRef]
- O’Connell, J.B.; Maggard, M.A.; Livingston, E.H.; Yo, C.K. Colorectal cancer in the young. Am. J. Surg. 2004, 3, 343–348. [Google Scholar] [CrossRef]
- Mauri, G.; Sartore-Bianchi, A.; Russo, A.G.; Marsoni, S.; Bardelli, A.; Siena, S. Early-onset colorectal cancer in young individuals. Mol. Oncol 2019, 2, 109–131. [Google Scholar] [CrossRef]
- Chan, K.K.; Dassanayake, B.; Deen, R.; Wickramarachchi, R.E.; Kumarage, S.K.; Samita, S.; Deen, K.I. Young patients with colorectal cancer have poor survival in the first twenty months after operation and predictable survival in the medium and long-term: Analysis of survival and prognostic markers. World J. Surg. Oncol. 2010, 8, 82. [Google Scholar] [CrossRef]
- Palmer, M.L.; Herrera, L.; Petrelli, N.J. Colorectal adenocarcinoma in patients less than 40 years of age. Dis. Colon Rectum. 1991, 4, 343–346. [Google Scholar] [CrossRef]
- Cusack, J.C.; Giacco, G.G.; Cleary, K.; Davidson, B.S.; Izzo, F.; Skibber, J.; Yen, J.; Curley, S.A. Survival factors in 186 patients younger than 40 years old with colorectal adenocarcinoma. J. Am. Coll. Surg. 1996, 2, 105–112. [Google Scholar]
- Paraf, F.; Jothy, S. Colorectal cancer before the age of 40: A case-control study. Dis. Colon Rectum 2000, 9, 1222–1226. [Google Scholar] [CrossRef]
- Chung, Y.F.; Eu, K.W.; Machin, D.; Ho, J.M.; Nyam, D.C.; Leong, A.F.; Ho, Y.H.; Seow-Choen, F. Young age is not a poor prognostic marker in colorectal cancer. Br. J. Surg. 1998, 9, 1255–1259. [Google Scholar] [CrossRef] [PubMed]
- Turkiewicz, D.; Miller, B.; Schache, D.; Cohen, J.; Theile, D. Young patients with colorectal cancer: How do they fare? ANZ J. Surg. 2001, 12, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Enblad, G.; Enblad, P.; Adami, H.O.; Glimelius, B.; Krusemo, U.; Påhlman, L. Relationship between age and survival in cancer of the colon and rectum with special reference to patients less than 40 years of age. Br. J. Surg. 1990, 6, 611–616. [Google Scholar] [CrossRef]
- Willauer, A.N.; Liu, Y.; Pereira, A.; Lam, M.; Morris, J.S.; Raghav, K.; Morris, V.K.; Menter, D.; Broaddus, R.; Meric-Bernstam, F.; et al. Clinical and molecular characterization of early-onset colorectal cancer. Cancer 2019, 12, 2002–2010. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | N (%) | Annual Percentage Change (95% CI) |
|---|---|---|
| Colon cases | 2895 (75.1) | 1.5 (1.3–1.7) a |
| Rectosigmoid junction and rectal cases | 962 (24.9) | 0.9 (0.0–1.6) |
| Gender | ||
| Males | 2141 (55.5) | 0.7 (0.5–0.9) a |
| Females | 1716 (44.5) | 1.8 (1.4–2.2) a |
| Age | ||
| 20–34 | 42 (1.1) | 1.8 (1.2–2.6) a |
| 35–49 | 116 (3.0) | 1.6 (1.3–1.9) a |
| 50–74 | 1137 (29.5) | −1.1 (−1.4–−0.5) a |
| >75 | 2562 (66.4) | −1.4 (−1.3–−1.0) a |
| Stage at diagnosis | ||
| Stage I | 497 (12.9) | 0.2 (0.0–0.4) a |
| Stage II | 927 (24.0) | 2.2 (1.9–2.2) a |
| Stage III | 1269 (32.9) | 1.3 (1.1–1.5) a |
| Stage IV | 817 (21.2) | −2.2 (−2.3–−2.1) a |
| Stage unknown | 347 (9.0) | - |
| Place of residence | ||
| County of Heraklion | 1193 (30.9) | 0.7 (0.6–1.1) a |
| County of Lasithi | 1121 (29.1) | 1.9 (1.7–2.3) a |
| County of Rethymnon | 697 (18.1) | 1.4 (1.2–1.6) a |
| County of Chania | 846 (21.9) | 0.8 (0.5–1.2) |
| Risk Factors | Time Period RR a (95% CI) | p-Value for Interaction b | ||
|---|---|---|---|---|
| 1992–2000 | 2001–2011 | 2012–2021 | ||
| Body Mass Index (kg/m2) * | 1.2 (1.1–1.3) | 1.8 (1.4–2.1) | 2.5 (2.2–2.7) | 0.04 |
| BSA (m2) * | 1.4 (1.1–1.8) | 2.3 (2.1–2.6) | 3.4 (3.3–3.5) | <0.001 |
| Smoking status | ||||
| Never smokers | 1 | 1 | 1 | |
| Ever smokers (ex and current) | 1.7 (1.4–2.1) | 1.8 (1.4–2.2) | 2.1 (2.0–2.2) | 0.58 |
| Packyears | 1.8 (1.5–2.2) | 2.5 (2.3–2.7) | 3.1 (3.0–3.2) | 0.01 |
| Alcohol consumption | 0.02 | |||
| Never consumers | 1 | 1 | 1 | |
| Ever consumers (ex and current) | 1.9 (1.7–2.2) | 2.6 (2.4–2.8) | 3.3 (3.0–3.4) | |
| Number of glasses per week | 2.1 (1.9–2.3) | 2.9 (2.7–3.1) | 4.1 (3.9–4.3) | <0.001 |
| Occupation | 0.04 | |||
| Other occupations | 1 | 1 | 1 | |
| Farmers | 1.5 (1.4–1.6) | 1.8 (1.7–2.0) | (2.1–2.5) | |
| Selected Parameters | Younger Adults | Older Adults | p-Value |
|---|---|---|---|
| 5-year Net survival (%) | |||
| Period 1992–2000 | 67.0 | 58.4 | 0.03 |
| Period 2001–2011 | 64.1 | 60.5 | |
| Period 2012–2021 | 61.2 | 61.9 | |
| Stage at diagnosis (Stage III & IV) | |||
| Period 1992–2000 | 19.8 | 27.4 | 0.03 |
| Period 2001–2011 | 27.3 | 26.1 | |
| Period 2012–2021 | 29.1 | 25.7 | |
| Metastatic cancer (yes) | |||
| Period 1992–2000 | 23.1 | 25.8 | 0.72 |
| Period 2001–2011 | 24.7 | 25.7 | |
| Period 2012–2021 | 25.2 | 25.1 | |
| Treatment (Surgery) | |||
| Period 1992–2000 | 63.1 | 63.2 | 0.81 |
| Period 2001–2011 | 64.7 | 63.1 | |
| Period 2012–2021 | 64.7 | 63.8 | |
| Treatment (Chemotherapy) | |||
| Period 1992–2000 | 32.7 | 42.5 | 0.04 |
| Period 2001–2011 | 38.9 | 38.0 | |
| Period 2012–2021 | 43.2 | 32.5 | |
| Treatment (Radiotherapy) | |||
| Period 1992–2000 | 18.6 | 20.9 | 0.52 |
| Period 2001–2011 | 21.5 | 21.6 | |
| Period 2012–2021 | 22.0 | 22.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sifaki-Pistolla, D.; Poimenaki, V.; Fotopoulou, I.; Saloustros, E.; Mavroudis, D.; Vamvakas, L.; Lionis, C. Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s. Cancers 2022, 14, 4799. https://doi.org/10.3390/cancers14194799
Sifaki-Pistolla D, Poimenaki V, Fotopoulou I, Saloustros E, Mavroudis D, Vamvakas L, Lionis C. Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s. Cancers. 2022; 14(19):4799. https://doi.org/10.3390/cancers14194799
Chicago/Turabian StyleSifaki-Pistolla, Dimitra, Viktoria Poimenaki, Ilektra Fotopoulou, Emmanouil Saloustros, Dimitrios Mavroudis, Lampros Vamvakas, and Christos Lionis. 2022. "Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s" Cancers 14, no. 19: 4799. https://doi.org/10.3390/cancers14194799
APA StyleSifaki-Pistolla, D., Poimenaki, V., Fotopoulou, I., Saloustros, E., Mavroudis, D., Vamvakas, L., & Lionis, C. (2022). Significant Rise of Colorectal Cancer Incidence in Younger Adults and Strong Determinants: 30 Years Longitudinal Differences between under and over 50s. Cancers, 14(19), 4799. https://doi.org/10.3390/cancers14194799









