The Development and Application of Echocardiography in Heart Disease
A project collection of Journal of Clinical Medicine (ISSN 2077-0383). This project collection belongs to the section "Cardiology".
Papers displayed on this page all arise from the same project. Editorial decisions were made independently of project staff and handled by the Editor-in-Chief or qualified Editorial Board members.
Submission Status: Closed | Viewed by 67187Editors
Interests: advanced cardiovascular imaging; CMR; echocardiography; cardiovascular emergencies
Special Issues, Collections and Topics in MDPI journals
2. Mediterranea Cardiocentro, 80122 Naples, Italy
Interests: echocardiography; speckle tracking echocardiography; valvular heart disease; ischemic heart disease; cardiomyopathies
Special Issues, Collections and Topics in MDPI journals
Project Overview
Dear Colleagues,
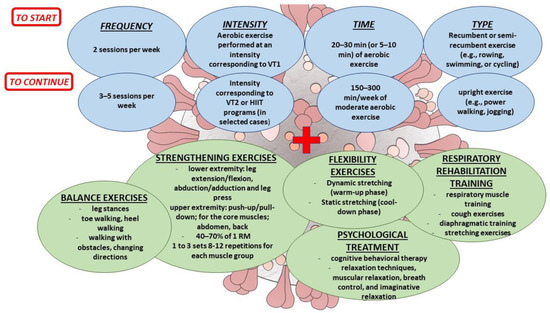
Cardiovascular diseases are the leading causes of mortality and morbidity in developed countries, with ischemic heart disease and non-ischemic cardiomyopathies playing the most relevant role. Many imaging techniques, either non-invasive or invasive, are being developed to allow a prompt detection of myocardial structural and functional abnormalities, as well as to guide therapeutic strategies.
Echocardiography is one of the most powerful diagnostic and monitoring tools available in clinical practice. Its wide availability, non-invasiveness and high diagnostic accuracy make echocardiography a fundamental step in the management of patients with cardiovascular disease.
Moreover, the ultimate role of echocardiography in managing heart disease has been highlighted, not only from a diagnostic perspective, but also for prognostic purposes.
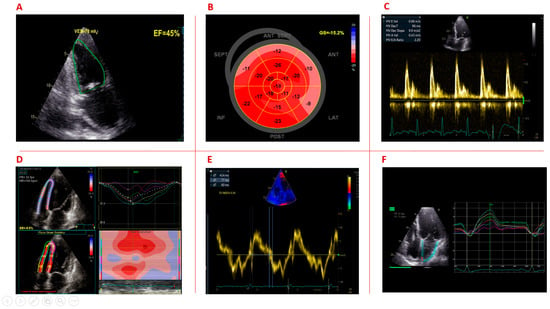
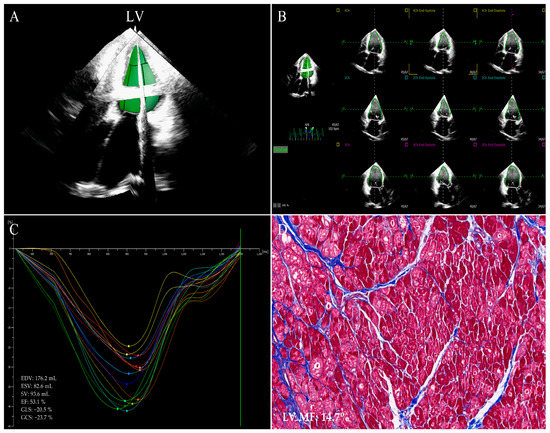
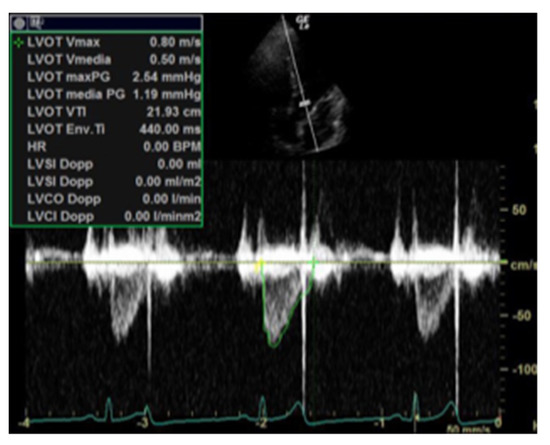
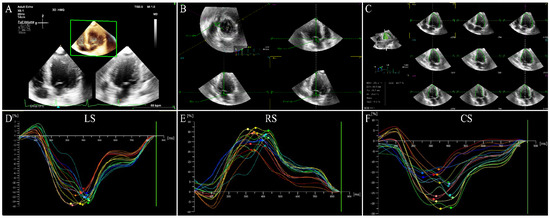
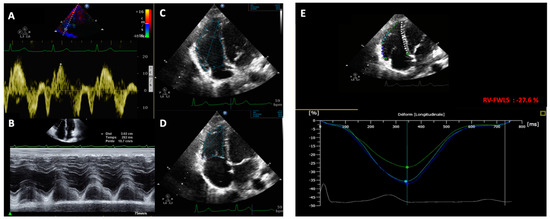
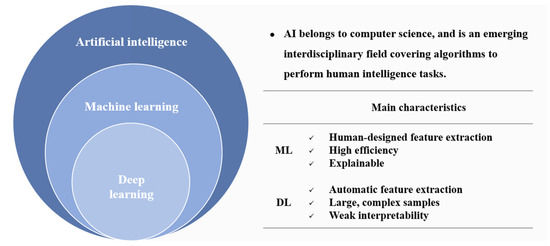
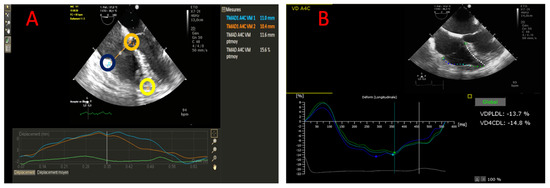
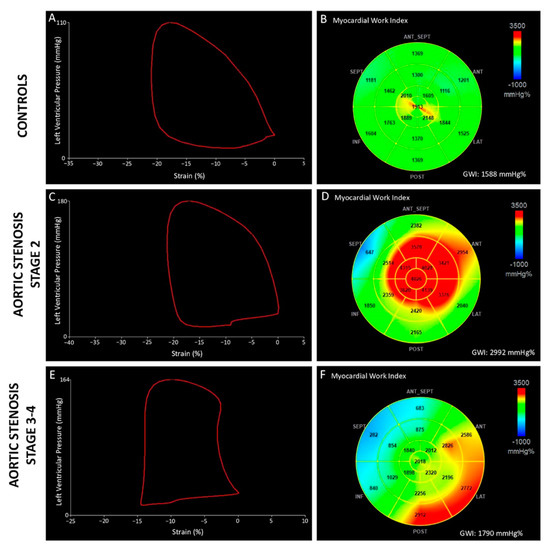
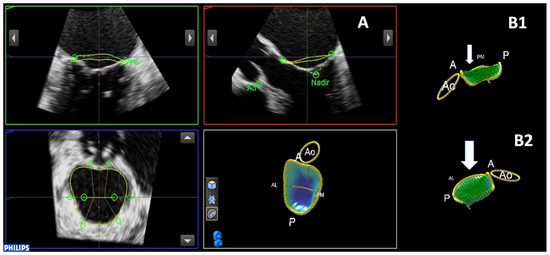
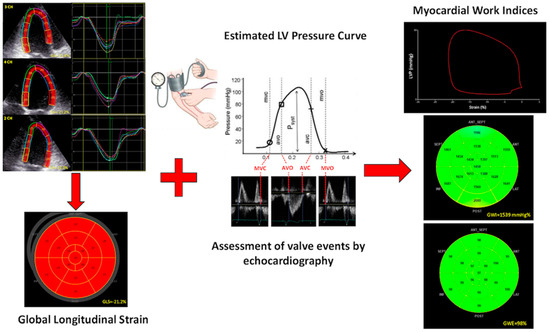
The advent of more advanced techniques, such as three-dimensional echocardiography, speckle-tracking-derived longitudinal strain, and, more recently, non-invasive myocardial work assessment, has provided further insight into the detection of the structural and pathophysiological mechanisms underlying cardiovascular disease and has further extended the application of such technics in many clinical scenarios.
This Special Issue of Journal of Clinical Medicine is now open for submission, welcoming papers that aim to present the current role of echocardiography in the diagnosis and management of cardiovascular diseases, with particular attention on novel techniques that could contribute to relevant achievements in the near future.
Prof. Dr. Antonello D'Andrea
Dr. Federica Ilardi
Guest Editors
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the collection website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2600 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- Speckle tracking echocardiography
- Global longitudinal strain
- Strain rate
- Non-invasive myocardial work
- 3D echocardiography
- Stress echocardiography
- Ischemic cardiomyopathy
- Non-ischemic cardiomyopathy
- Valvular heart disease