Quantitative Imaging Parameters of Contrast-Enhanced Micro-Computed Tomography Correlate with Angiogenesis and Necrosis in a Subcutaneous C6 Glioma Model
Abstract
:Simple Summary
Abstract
1. Introduction
2. Results
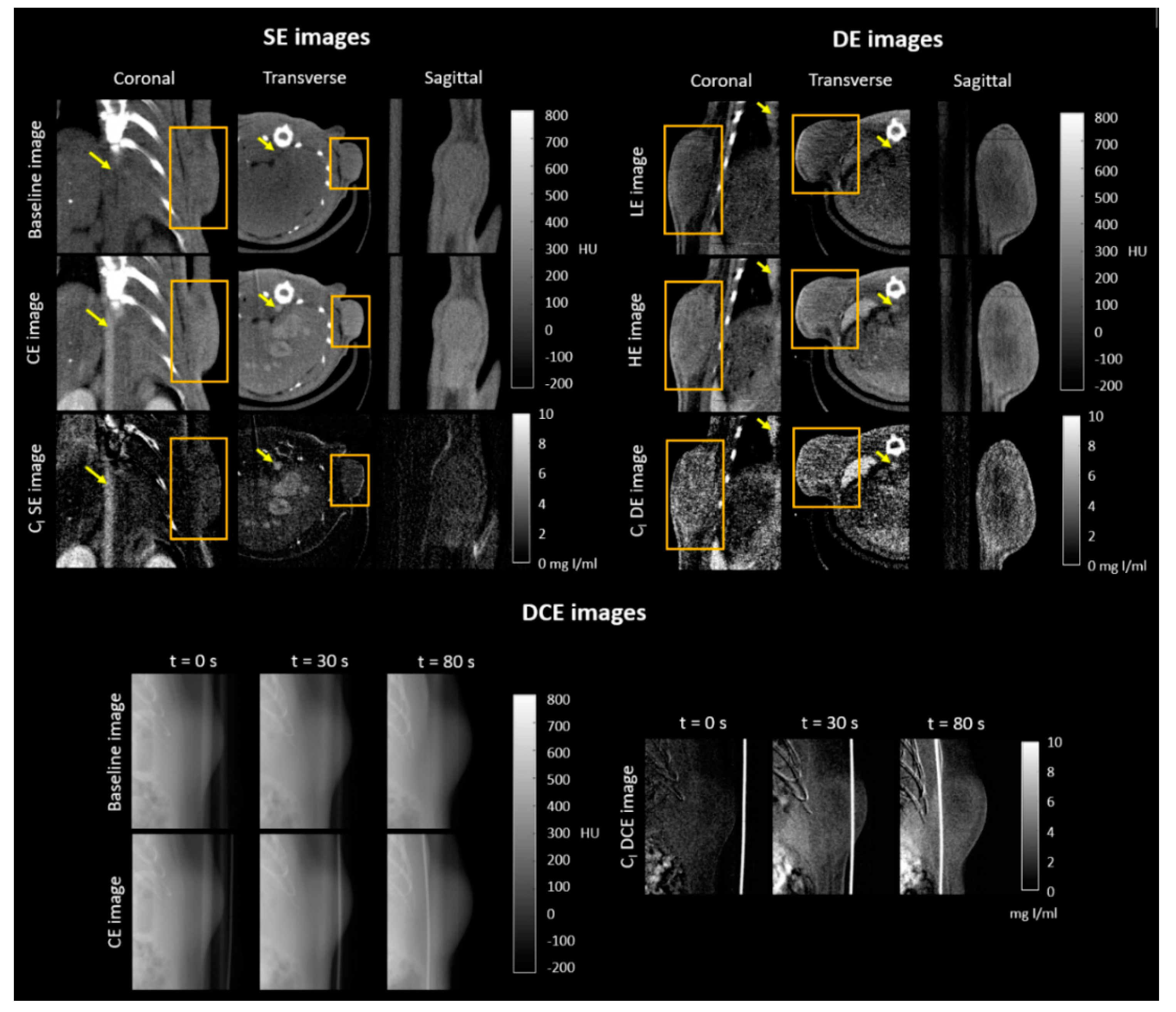
2.1. Qualitative Evaluation of CE X-ray Images of the Subcutaneous C6 Glioma Model
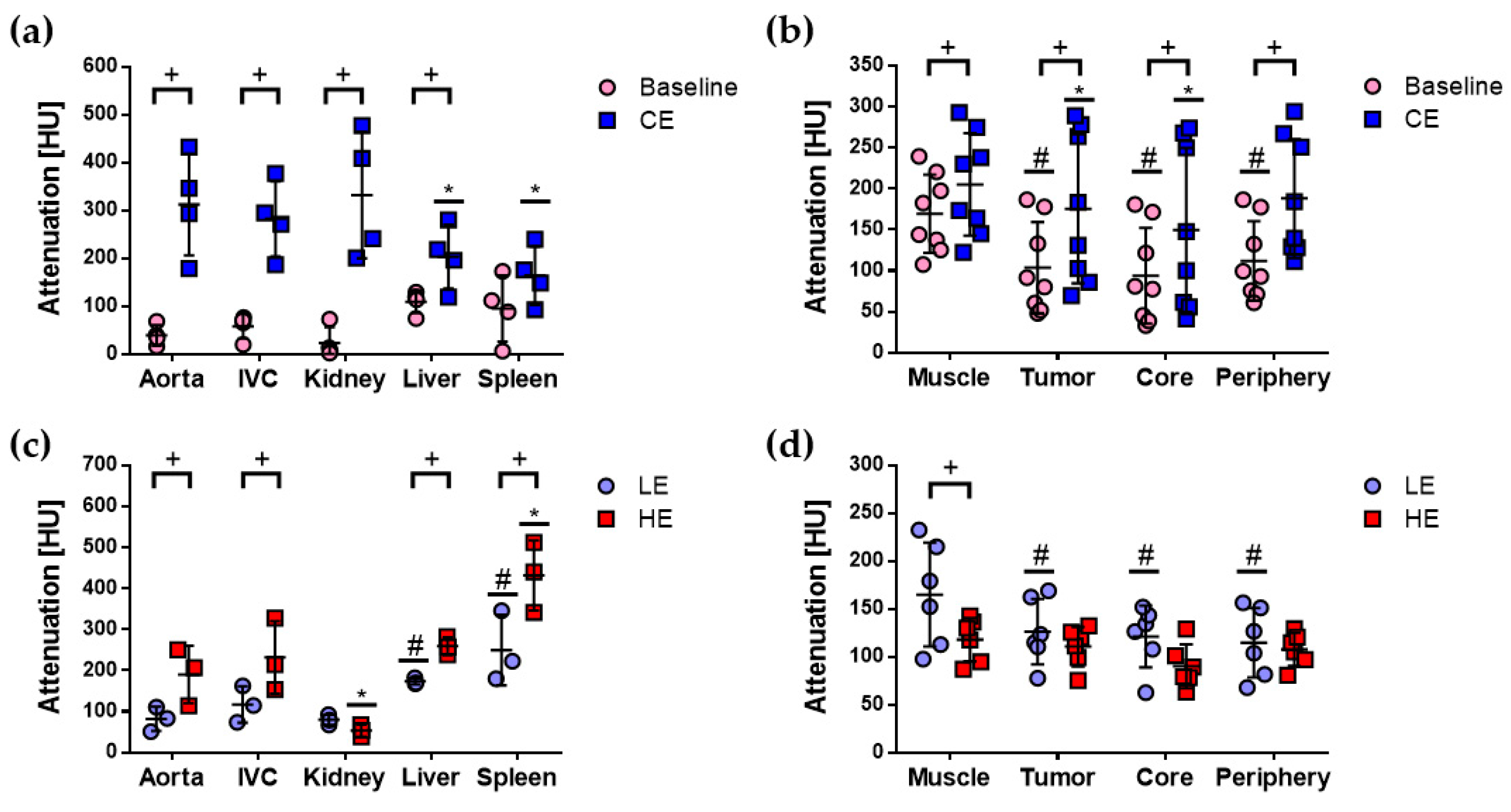
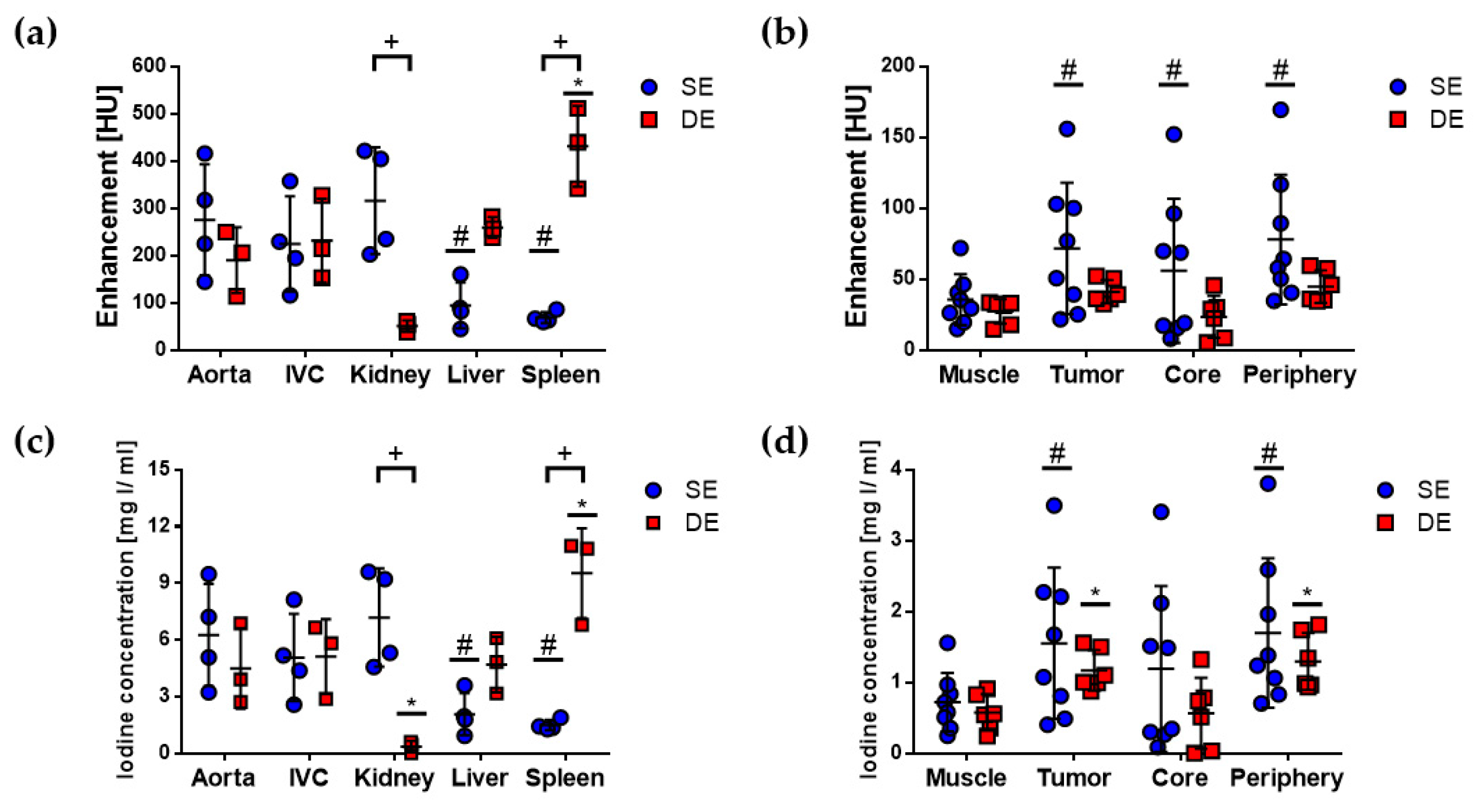
2.2. Quantitative Evaluation of CE X-ray Images of the Subcutaneous C6 Glioma Model
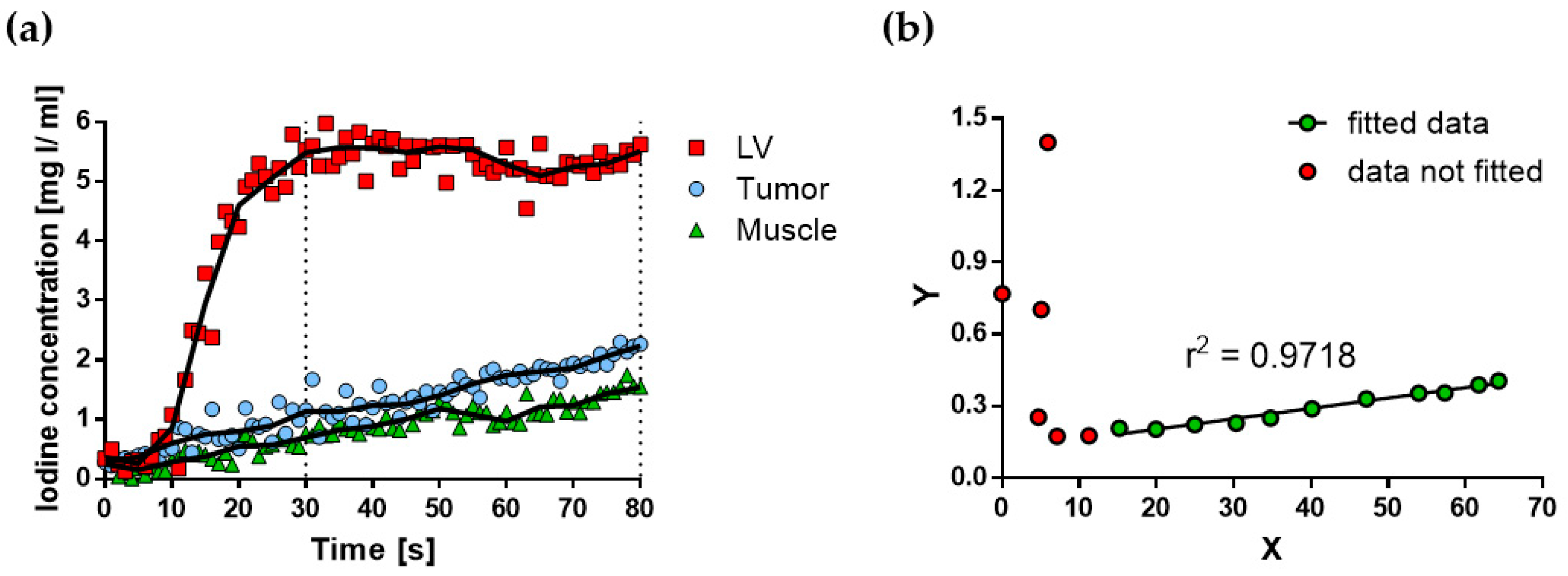
2.3. Quantification of rBV and Ktrans
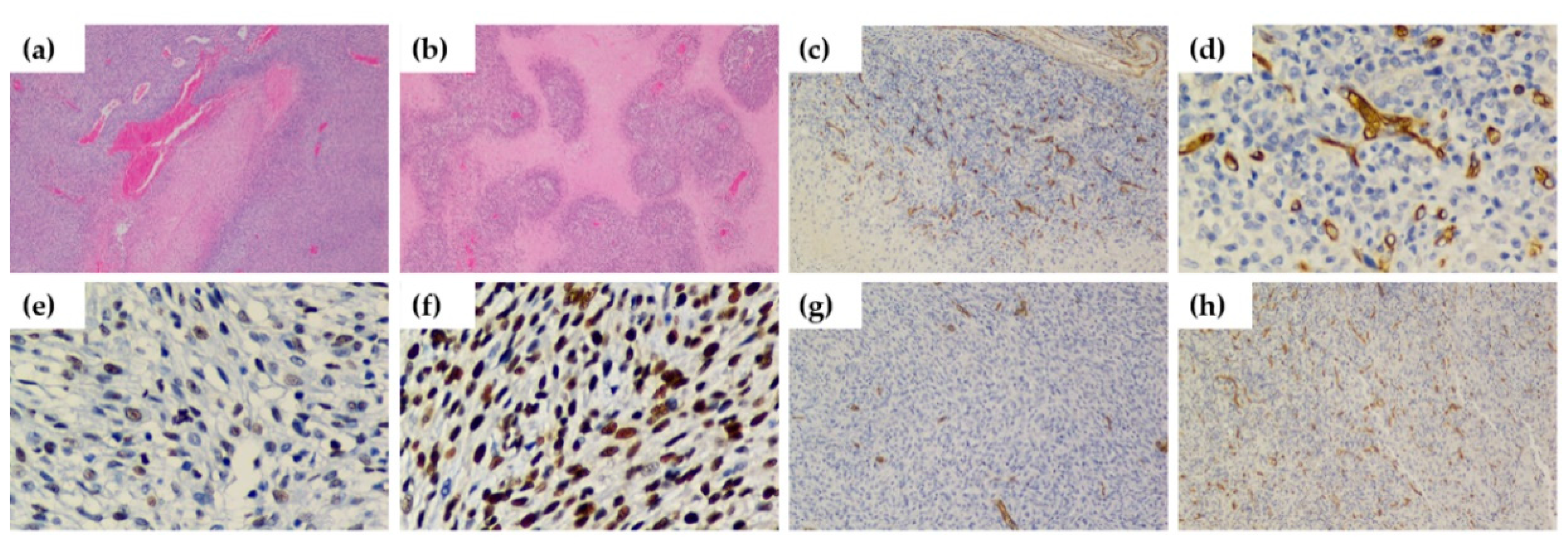
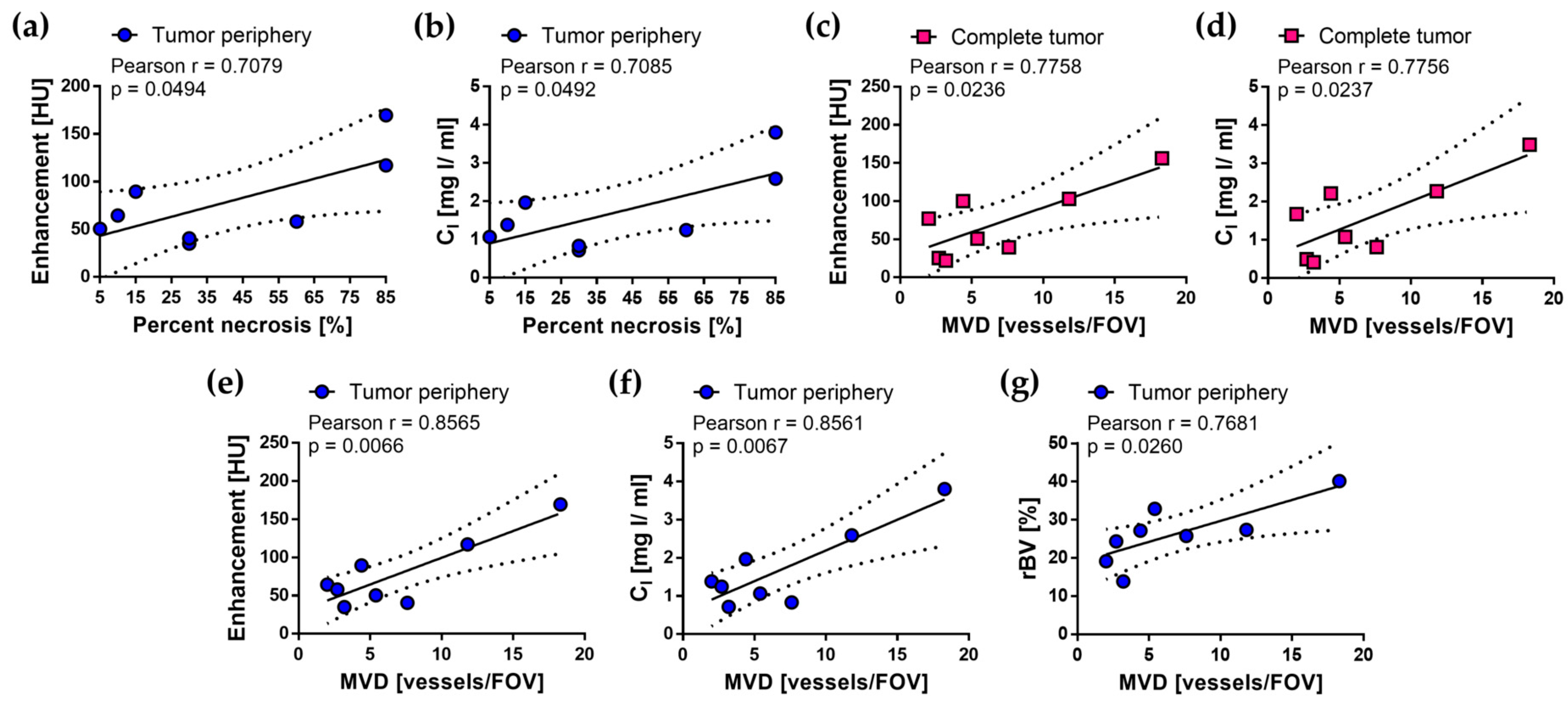
2.4. Histological Validation of Quantitative Imaging Parameters
3. Discussion
4. Materials and Methods
4.1. Subcutaneous C6 Glioma Animal Model
4.2. Albira ARS Micro-CT Scanner
4.3. Imaging Protocols
4.3.1. SE Protocol
4.3.2. DE Protocol
4.3.3. DCE Protocol
4.4. Image Analysis
4.4.1. Image Subtraction
4.4.2. Quantification of Imaging Parameters in SE and DE Micro-CT Images
4.4.3. Quantification of Imaging Parameters in DCE Planar Images
4.5. Histological Analysis
4.6. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hanahan, D.; Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 1996, 86, 353–364. [Google Scholar] [CrossRef] [Green Version]
- Weidner, N. Intratumor microvessel density as a prognostic factor in cancer. Am. J. Pathol. 1995, 147, 9–19. [Google Scholar] [PubMed]
- Bais, C.; Mueller, B.; Brady, M.F.; Mannel, R.S.; Burger, R.A.; Wei, W.; Marien, K.M.; Kockx, M.M.; Husain, A.; Birrer, M.J.; et al. Tumor Microvessel Density as a Potential Predictive Marker for Bevacizumab Benefit: GOG-0218 Biomarker Analyses. J. Natl. Cancer Inst. 2017, 109, djx066. [Google Scholar] [CrossRef] [PubMed]
- García-Figueiras, R.; Padhani, A.R.; Beer, A.J.; Baleato-González, S.; Vilanova, J.C.; Luna, A.; Oleaga, L.; Gómez-Caamaño, A.; Koh, D.M. Imaging of Tumor Angiogenesis for Radiologists—Part 1: Biological and Technical Basis. Curr. Probl. Diagn. Radiol. 2015, 44, 407–424. [Google Scholar] [CrossRef]
- Ulyte, A.; Katsaros, V.K.; Liouta, E.; Stranjalis, G.; Boskos, C.; Papanikolaou, N.; Usinskiene, J.; Bisdas, S. Prognostic value of preoperative dynamic contrast-enhanced MRI perfusion parameters for high-grade glioma patients. Neuroradiology 2016, 58, 1197–1208. [Google Scholar] [CrossRef] [Green Version]
- Yu, C.; Li, T.; Zhang, R.; Yang, X.; Yang, Z.; Xin, L.; Zhao, Z. Dual-energy CT perfusion imaging for differentiating WHO subtypes of thymic epithelial tumors. Sci. Rep. 2020, 10, 5511. [Google Scholar] [CrossRef]
- Ayala-Domínguez, L.; Brandan, M.E. Quantification of tumor angiogenesis with contrast-enhanced x-ray imaging in preclinical studies: A review. Biomed. Phys. Eng. Express 2018, 4, 062001. [Google Scholar] [CrossRef]
- Park, C.M.; Goo, J.M.; Lee, H.J.; Kim, M.A.; Kim, H.C.; Kim, K.G.; Lee, C.H.; Im, J.G. FN13762 murine breast cancer: Region-by-region correlation of first-pass perfusion CT indexes with histologic vascular parameters. Radiology 2009, 251, 721–730. [Google Scholar] [CrossRef]
- Guan, L.M.; Qi, X.X.; Xia, B.; Li, Z.H.; Zhao, Y.; Xu, K. Early changes measured by CT perfusion imaging in tumor microcirculation following radiosurgery in rat C6 brain gliomas. J. Neurosurg. 2011, 114, 1672–1680. [Google Scholar] [CrossRef]
- Lu, N.; Di, Y.; Feng, X.Y.; Qiang, J.W.; Zhang, J.W.; Wang, Y.G.; Liu, Y. CT perfusion with acetazolamide challenge in C6 gliomas and angiogenesis. PLoS ONE 2015, 10, e0121631. [Google Scholar] [CrossRef]
- Qi, Q.; Yeung, T.P.; Lee, T.Y.; Bauman, G.; Crukley, C.; Morrison, L.; Hoffman, L.; Yartsev, S. Evaluation of CT Perfusion Biomarkers of Tumor Hypoxia. PLoS ONE 2016, 11, e0153569. [Google Scholar] [CrossRef] [PubMed]
- Ehling, J.; Theek, B.; Gremse, F.; Baetke, S.; Möckel, D.; Maynard, J.; Ricketts, S.A.; Grüll, H.; Neeman, M.; Knuechel, R.; et al. Micro-CT imaging of tumor angiogenesis: Quantitative measures describing micromorphology and vascularization. Am. J. Pathol. 2014, 184, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Ekdawi, S.N.; Stewart, J.M.; Dunne, M.; Stapleton, S.; Mitsakakis, N.; Dou, Y.N.; Jaffray, D.A.; Allen, C. Spatial and temporal mapping of heterogeneity in liposome uptake and microvascular distribution in an orthotopic tumor xenograft model. J. Control Release 2015, 207, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhou, J.; Li, J.; Zhang, L.; Zhang, P.; Liu, B. Evaluation of rat C6 malignant glioma using spectral computed tomography. Exp. Ther. Med. 2017, 14, 1037–1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, X.; Liang, X.; Zhang, Q.; Wang, D.; Liu, J.; Zhang, L.; Zhou, J. Quantifying the angiogenesis of C6 glioma in rats based on CT quantitative parameters. Acta Radiol. 2019, 60, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Karathanasis, E.; Chan, L.; Karumbaiah, L.; McNeeley, K.; D’Orsi, C.J.; Annapragada, A.V.; Sechopoulos, I.; Ballamkonda, R.V. Tumor vascular permeability to a nanoprobe correlates to tumor-specific expression levels of angiogenic markers. PLoS ONE 2009, 4, e5843. [Google Scholar] [CrossRef]
- Driscoll, B.; Keller, H.; Coolens, C. Development of a dynamic flow imaging phantom for dynamic contrast-enhanced CT. Med. Phys. 2011, 38, 4866–4880. [Google Scholar] [CrossRef]
- Knobloch, G.; Jost, G.; Huppertz, A.; Hamm, B.; Pietsch, H. Dual-energy computed tomography for the assessment of early treatment effects of regorafenib in a preclinical tumor model: Comparison with dynamic contrast-enhanced CT and conventional contrast-enhanced single-energy CT. Eur. Radiol. 2014, 24, 1896–1905. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.J.; Kim, S.H.; Bae, J.S.; Jeon, S.K.; Han, J.K. Can quantitative iodine parameters on DECT replace perfusion CT parameters in colorectal cancers? Eur. Radiol. 2018, 28, 4775–4782. [Google Scholar] [CrossRef]
- Brat, D.J.; Van Meir, E.G. Vaso-occlusive and prothrombotic mechanisms associated with tumor hypoxia, necrosis, and accelerated growth in glioblastoma. Lab. Investig. 2004, 84, 397–405. [Google Scholar] [CrossRef]
- Wippold, F.J., 2nd; Lämmle, M.; Anatelli, F.; Lennerz, J.; Perry, A. Neuropathology for the neuroradiologist: Palisades and pseudopalisades. AJNR Am. J. Neuroradiol. 2006, 27, 2037–2041. [Google Scholar]
- Xuesong, D.; Wei, X.; Heng, L.; Xiao, C.; Shunan, W.; Yu, G.; Weiguo, Z. Evaluation of neovascularization patterns in an orthotopic rat glioma model with dynamic contrast-enhanced MRI. Acta Radiol. 2017, 58, 1138–1146. [Google Scholar] [CrossRef] [PubMed]
- Hou, W.; Xue, Y.; Tang, W.; Pan, H.; Xu, M.; Li, X.; Bi, S.; Shen, Y.; Qian, Y.; Yu, Y. Evaluation of Tumor Hypoxia in C6 Glioma Rat Model With Dynamic Contrast-Enhanced Magnetic Resonance Imaging. Acad Radiol. 2019, 26, e224–e232. [Google Scholar] [CrossRef] [PubMed]
- Rosado-Méndez, I.; Palma, B.A.; Brandan, M.E. Analytical optimization of digital subtraction mammography with contrast medium using a commercial unit. Med. Phys. 2008, 35, 5544–5557. [Google Scholar] [CrossRef] [PubMed]
- Berumen, F.; Ayala-Domínguez, L.; Medina, L.A.; Brandan, M.E. A method to optimize the image acquisition protocol of a MicroCT unit for preclinical studies using contrast-enhanced digital subtraction. In AIP Conference Proceedings; AIP Publishing LLC: New York, NY, USA, 2016; Volume 1747, p. 080003. [Google Scholar]
- Castillo, J.P.; Corona-Nieblas, L.; Berumen, F.; Ayala-Domínguez, L.; Medina, L.A.; Brandan, M.E. Optimization of dual-energy subtraction for preclinical studies using a commercial MicroCT unit. In AIP Conference Proceedings; AIP Publishing LLC: New York, NY, USA, 2016; Volume 1747, p. 080005. [Google Scholar]
- Ayala-Domínguez, L.; Pérez-Cárdenas, E.; Medina, L.A.; Lizano, M.; Brandan, M.E. Contrast-enhanced microCT imaging in a tumor angiogenesis murine model. In AIP Conference Proceedings; AIP Publishing LLC: New York, NY, USA, 2019; Volume 2090, p. 030002. [Google Scholar]
- Holash, J.; Wiegand, S.J.; Yancopoulos, G.D. New model of tumor angiogenesis: Dynamic balance between vessel regression and growth mediated by angiopoietins and VEGF. Oncogene 1999, 18, 5356–5362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giakoumettis, D.; Kritis, A.; Foroglou, N. C6 cell line: The gold standard in glioma research. Hippokratia 2018, 22, 105–112. [Google Scholar]
- Carmeliet, P.; Jain, R.K. Molecular mechanisms and clinical applications of angiogenesis. Nature 2011, 473, 298–307. [Google Scholar] [CrossRef] [Green Version]
- Coomber, B.L.; Stewart, P.A.; Hayakawa, E.M.; Farrell, C.L.; Del Maestro, R.F. A quantitative assessment of microvessel ultrastructure in C6 astrocytoma spheroids transplanted to brain and to muscle. J. Neuropathol. Exp. Neurol. 1988, 47, 29–40. [Google Scholar] [CrossRef]
- Watanabe, K.; Sakamoto, M.; Somiya, M.; Amin, M.R.; Kamitani, H.; Watanabe, T. Feasibility and limitations of the rat model by C6 gliomas implanted at the subcutaneous region. Neurol. Res. 2002, 24, 485–490. [Google Scholar] [CrossRef]
- Lenting, K.; Verhaak, R.; Ter Laan, M.; Wesseling, P.; Leenders, W. Glioma: Experimental models and reality. Acta Neuropathol. 2017, 133, 263–282. [Google Scholar] [CrossRef] [Green Version]
- Hagiwara, A.; Fujita, S.; Ohno, Y.; Aoki, S. Variability and Standardization of Quantitative Imaging: Monoparametric to Multiparametric Quantification, Radiomics, and Artificial Intelligence. Investig. Radiol. 2020, 55, 601–616. [Google Scholar] [CrossRef] [PubMed]
- Alkadhi, H.; Euler, A. The Future of Computed Tomography: Personalized, Functional, and Precise. Investig. Radiol. 2020, 55, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.C.; Ashley, D.M.; López, G.Y.; Malinzak, M.; Friedman, H.S.; Khasraw, M. Management of glioblastoma: State of the art and future directions. CA Cancer J. Clin. 2020, 70, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Sharma, M.C.; Sarkar, C. Morphology of angiogenesis in human cancer: A conceptual overview, histoprognostic perspective and significance of neoangiogenesis. Histopathology 2005, 46, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Bolcaen, J.; Descamps, B.; Acou, M.; Deblaere, K.; den Broecke, C.V.; Boterberg, T.; Vanhove, C.; Goethals, I. In Vivo DCE-MRI for the Discrimination between Glioblastoma and Radiation Necrosis in Rats. Mol. Imaging Biol. 2017, 19, 857–866. [Google Scholar] [CrossRef] [PubMed]
- Zoula, S.; Hérigault, G.; Ziegler, A.; Farion, R.; Décorps, M.; Rémy, C. Correlation between the occurrence of 1H-MRS lipid signal, necrosis and lipid droplets during C6 rat glioma development. NMR Biomed. 2003, 16, 199–212. [Google Scholar] [CrossRef]
- Bradley, D.P.; Tessier, J.J.; Ashton, S.E.; Waterton, J.C.; Wilson, Z.; Worthington, P.L.; Ryan, A.J. Correlation of MRI biomarkers with tumor necrosis in Hras5 tumor xenograft in athymic rats. Neoplasia 2007, 9, 382–391. [Google Scholar] [CrossRef]
- Jiang, J.S.; Hua, Y.; Zhou, X.J.; Shen, D.D.; Shi, J.L.; Ge, M.; Geng, Q.N.; Jia, Z.Z. Quantitative Assessment of Tumor Cell Proliferation in Brain Gliomas with Dynamic Contrast-Enhanced MRI. Acad. Radiol. 2019, 26, 1215–1221. [Google Scholar] [CrossRef]
- Burgener, F.A.; Hamlin, D.J. Contrast enhancement in abdominal CT: Bolus vs. infusion. AJR Am J Roentgenol. 1981, 137, 351–358. [Google Scholar] [CrossRef]
- Ford, N.L.; Thornton, M.M.; Holdsworth, D.W. Fundamental image quality limits for microcomputed tomography in small animals. Med. Phys. 2003, 30, 2869–2877. [Google Scholar] [CrossRef]
- Evangelidis, G.D.; Psarakis, E.Z. Parametric image alignment using enhanced correlation coefficient maximization. IEEE Trans. Pattern Anal. Mach. Intell. 2008, 30, 1858–1865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, M.L.; Mainprize, J.G.; Mawdsley, G.E.; Yaffe, M.J. A solid iodinated phantom material for use in tomographic x-ray imaging. Med. Phys. 2009, 36, 4409–4420. [Google Scholar] [CrossRef] [PubMed]
- Amide Software. Available online: http://amide.sourceforge.net/ (accessed on 13 October 2020).
- Patlak, C.S.; Blasberg, R.G. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. Generalizations. J. Cereb. Blood Flow Metab. 1985, 5, 584–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ImageJ Software. Available online: https://imagej.nih.gov/ij/ (accessed on 13 October 2020).
- Weidner, N. Current pathologic methods for measuring intratumoral microvessel density within breast carcinoma and other solid tumors. Breast Cancer Res. Treat. 1995, 36, 169–180. [Google Scholar] [CrossRef] [PubMed]
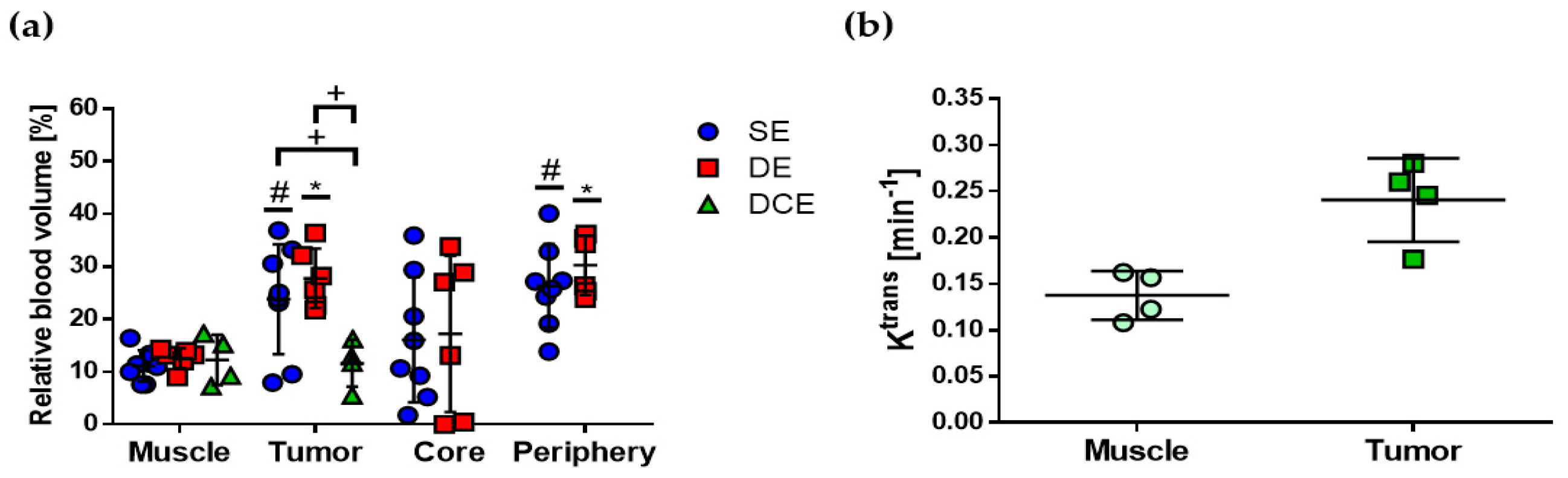
| Imaging Protocol | Imaging Parameter | Muscle | Tumor | Core | Periphery |
|---|---|---|---|---|---|
| SE (n = 8) | E (HU) | 35.5 ± 6.3 | 71.6 ± 16.3 * | 55.8 ± 17.9 * | 77.9 ± 16.1 * |
| CI (mg I/mL) | 0.72 ± 0.14 | 1.55 ± 0.37 * | 1.19 ± 0.41 | 1.69 ± 0.37 * | |
| rBV (%) | 11.1 ± 1.0 | 23.8 ± 3.6 * | 16.1 ± 4.2 | 26.3 ± 2.8 * | |
| DE (n = 6) | E (HU) | 27.2 ± 3.4 | 41.1 ± 3.3 | 23.4 ± 6.0 | 44.7 ± 4.6 |
| CI (mg I/mL) | 0.57 ± 0.10 | 1.17 ± 0.11 * | 0.56 ± 0.20 | 1.29 ± 0.16 * | |
| rBV (%) | 12.6 ± 0.7 | 27.7 ± 2.3 * | 17.2 ± 6.0 | 30.2 ± 2.2 * | |
| DCE (n = 4) | rBV (%) | 12.2 ± 2.3 | 11.6 ± 2.2 | ||
| Ktrans (min−1) | 0.13 ± 0.01 | 0.24 ± 0.02 |
| Imaging Protocol | Percent Necrosis (%) | Proliferation Index (%) | MVD (Vessels/HPF) |
|---|---|---|---|
| SE (n = 8) | 38.1 ± 10.5 | 68.7 ± 8.4 | 6.9 ± 1.9 |
| DE (n = 6) | 28.3 ± 7.6 | 70.8 ± 8.2 | 3.5 ± 1.0 |
| DCE (n = 4) | 26.2 ± 9.4 | 78.7 ± 6.5 | 3.9 ± 1.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ayala-Domínguez, L.; Pérez-Cárdenas, E.; Avilés-Salas, A.; Medina, L.A.; Lizano, M.; Brandan, M.-E. Quantitative Imaging Parameters of Contrast-Enhanced Micro-Computed Tomography Correlate with Angiogenesis and Necrosis in a Subcutaneous C6 Glioma Model. Cancers 2020, 12, 3417. https://doi.org/10.3390/cancers12113417
Ayala-Domínguez L, Pérez-Cárdenas E, Avilés-Salas A, Medina LA, Lizano M, Brandan M-E. Quantitative Imaging Parameters of Contrast-Enhanced Micro-Computed Tomography Correlate with Angiogenesis and Necrosis in a Subcutaneous C6 Glioma Model. Cancers. 2020; 12(11):3417. https://doi.org/10.3390/cancers12113417
Chicago/Turabian StyleAyala-Domínguez, Lízbeth, Enrique Pérez-Cárdenas, Alejandro Avilés-Salas, Luis Alberto Medina, Marcela Lizano, and María-Ester Brandan. 2020. "Quantitative Imaging Parameters of Contrast-Enhanced Micro-Computed Tomography Correlate with Angiogenesis and Necrosis in a Subcutaneous C6 Glioma Model" Cancers 12, no. 11: 3417. https://doi.org/10.3390/cancers12113417





