The Application of GHRH Antagonist as a Treatment for Resistant APL
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Peptides and Reagents
2.2. Cell Culture
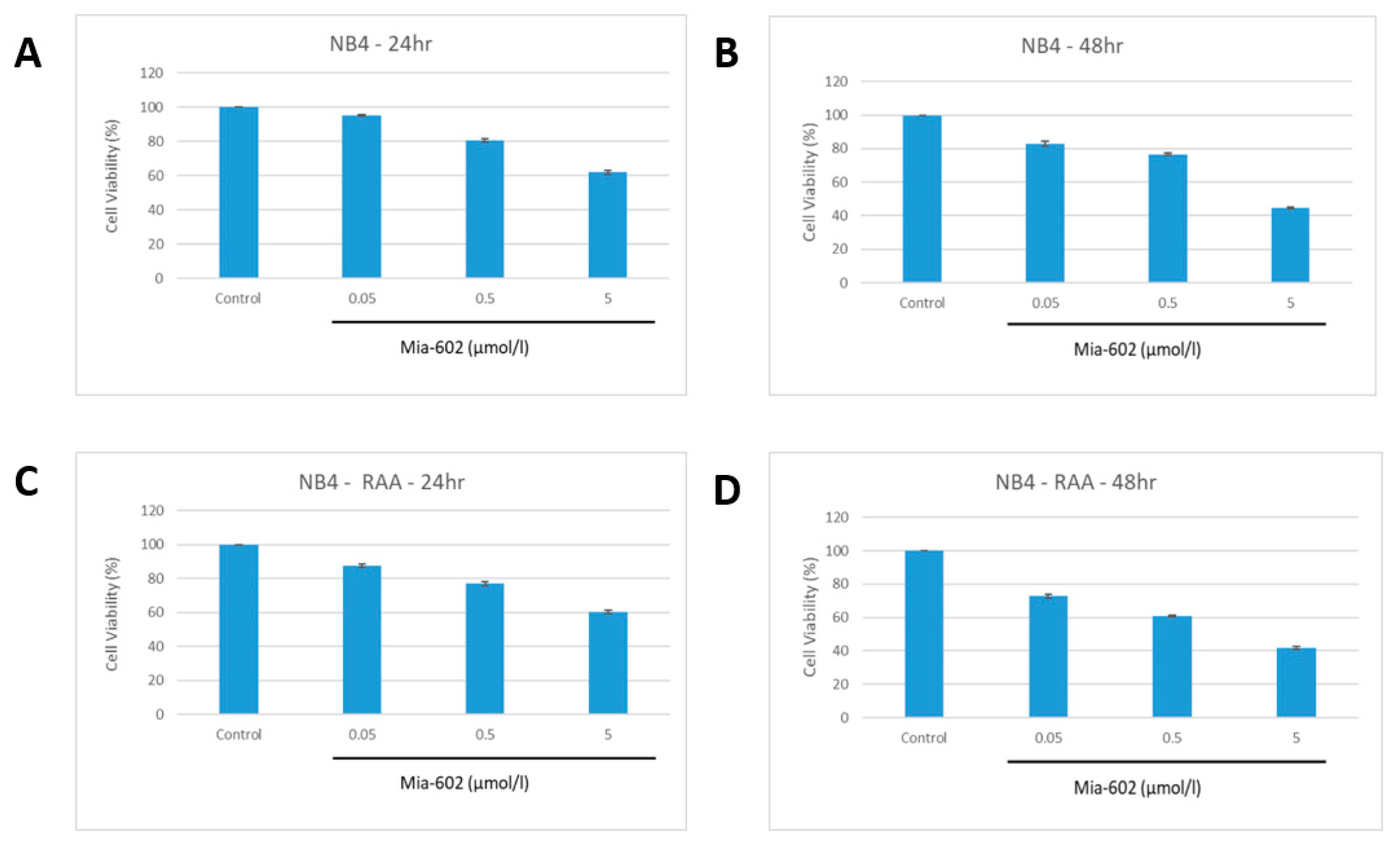
2.3. Cell Proliferation
2.4. Apoptosis Assay
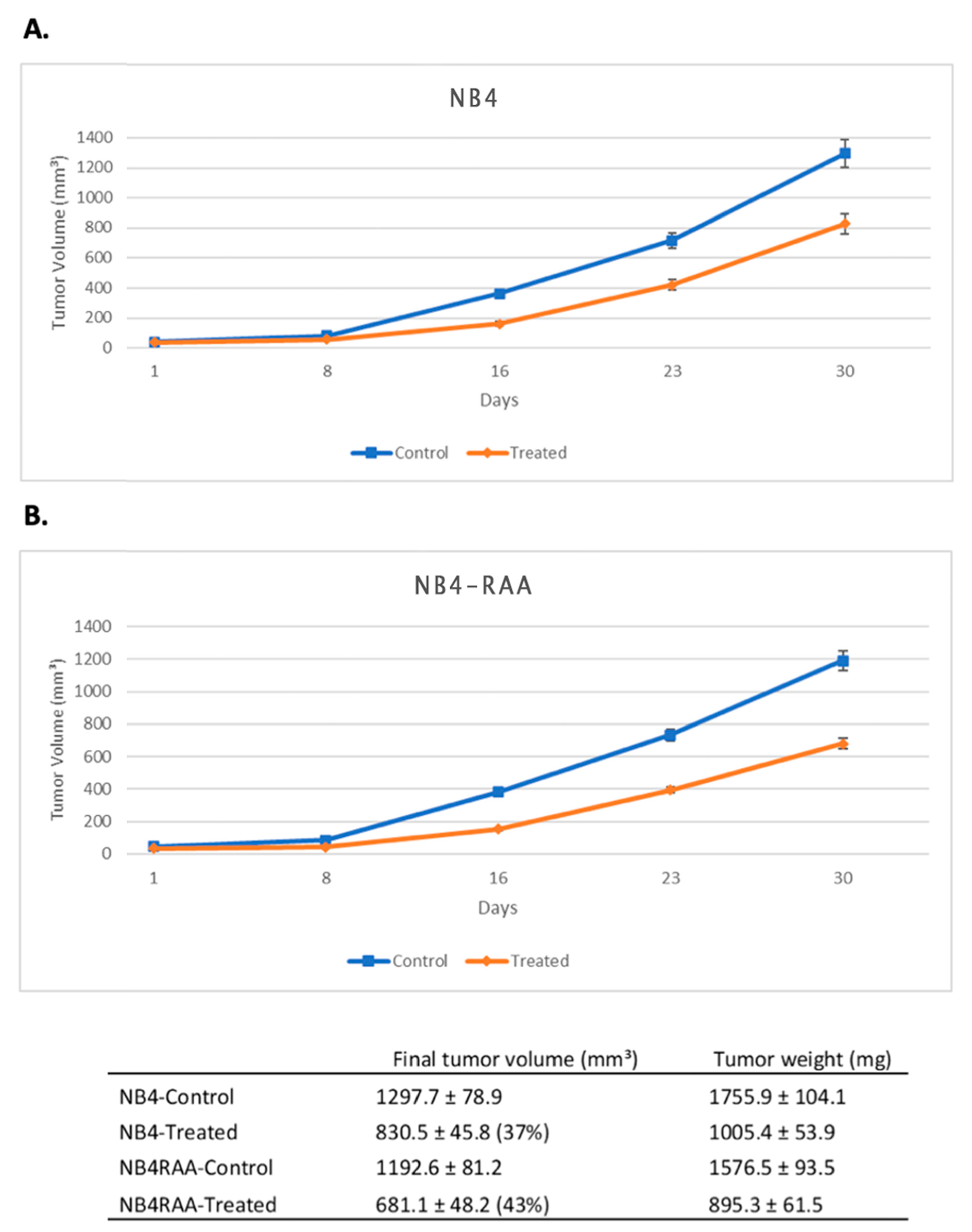
2.5. In Vivo Experiments in Mice
2.6. Western Blotting
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jimenez, J.J.; Chale, R.S.; Abad, A.C.; Schally, A.V. Acute promyelocytic leukemia (APL): A review of the literature. Oncotarget 2020, 11, 992–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coombs, C.C.; Tavakkoli, M.; Tallman, M.S. Acute promyelocytic leukemia: Where did we start, where are we now, and the future. Blood Cancer J. 2015, 5, e304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanz, M.A.; Fenaux, P.; Tallman, M.S.; Estey, E.H.; Lowenberg, B.; Naoe, T.; Lengfelder, E.; Dohner, H.; Burnett, A.K.; Chen, S.J.; et al. Management of acute promyelocytic leukemia: Updated recommendations from an expert panel of the European LeukemiaNet. Blood 2019, 133, 1630–1643. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.Y.; Gong, S.; Li, G.H.; Yao, Y.Z.; Zheng, Y.S.; Lu, X.H.; Wei, S.H.; Qin, W.W.; Liu, H.B.; Wang, M.C.; et al. An effective and chemotherapy-free strategy of all-trans retinoic acid and arsenic trioxide for acute promyelocytic leukemia in all risk groups (APL15 trial). Blood Cancer J. 2022, 12, 158. [Google Scholar] [CrossRef]
- Kutny, M.A.; Alonzo, T.A.; Abla, O.; Rajpurkar, M.; Gerbing, R.B.; Wang, Y.C.; Hirsch, B.A.; Raimondi, S.; Kahwash, S.; Hardy, K.K.; et al. Assessment of Arsenic Trioxide and All-trans Retinoic Acid for the Treatment of Pediatric Acute Promyelocytic Leukemia: A Report From the Children’s Oncology Group AAML1331 Trial. JAMA Oncol. 2022, 8, 79–87. [Google Scholar] [CrossRef]
- Cull, E.H.; Altman, J.K. Contemporary treatment of APL. Curr. Hematol. Malig. Rep. 2014, 9, 193–201. [Google Scholar] [CrossRef] [Green Version]
- Tobal, K.; Moore, H.; Macheta, M.; Yin, J.A. Monitoring minimal residual disease and predicting relapse in APL by quantitating PML-RARalpha transcripts with a sensitive competitive RT-PCR method. Leukemia 2001, 15, 1060–1065. [Google Scholar] [CrossRef] [Green Version]
- Montesinos, P.; Rayon, C.; Vellenga, E.; Brunet, S.; Gonzalez, J.; Gonzalez, M.; Holowiecka, A.; Esteve, J.; Bergua, J.; Gonzalez, J.D.; et al. Clinical significance of CD56 expression in patients with acute promyelocytic leukemia treated with all-trans retinoic acid and anthracycline-based regimens. Blood 2011, 117, 1799–1805. [Google Scholar] [CrossRef] [Green Version]
- Korninger, L.; Knobl, P.; Laczika, K.; Mustafa, S.; Quehenberger, P.; Schwarzinger, I.; Lechner, K.; Jaeger, U.; Mannhalter, C. PML-RAR alpha PCR positivity in the bone marrow of patients with APL precedes haematological relapse by 2–3 months. Br. J. Haematol. 1994, 88, 427–431. [Google Scholar] [CrossRef]
- Schachter-Tokarz, E.; Kelaidi, C.; Cassinat, B.; Chomienne, C.; Gardin, C.; Raffoux, E.; Dombret, H.; Fenaux, P.; Gallagher, R. PML-RARalpha ligand-binding domain deletion mutations associated with reduced disease control and outcome after first relapse of APL. Leukemia 2010, 24, 473–476. [Google Scholar] [CrossRef] [Green Version]
- Zak, P.; Koristek, Z. [Relapse in acute promyelocytic leukemia and the role of hematopoietic stem cell transplantation in the treatment of APL]. Vnitr. Lek. 2008, 54, 751–756. [Google Scholar] [PubMed]
- Stahl, M.; Tallman, M.S. Differentiation syndrome in acute promyelocytic leukaemia. Br. J. Haematol. 2019, 187, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.; Kantarjian, H.; Ravandi, F. Acute promyelocytic leukemia current treatment algorithms. Blood Cancer J. 2021, 11, 123. [Google Scholar] [CrossRef]
- Noguera, N.I.; Catalano, G.; Banella, C.; Divona, M.; Faraoni, I.; Ottone, T.; Arcese, W.; Voso, M.T. Acute Promyelocytic Leukemia: Update on the Mechanisms of Leukemogenesis, Resistance and on Innovative Treatment Strategies. Cancers 2019, 11, 1591. [Google Scholar] [CrossRef] [Green Version]
- Stahl, M.; Tallman, M.S. Acute promyelocytic leukemia (APL): Remaining challenges towards a cure for all. Leuk. Lymphoma 2019, 60, 3107–3115. [Google Scholar] [CrossRef] [PubMed]
- Russell, N.; Dillon, R. UK Experience of an Alternative ATO Dosing Regimen in APL. Front. Oncol. 2020, 10, 594129. [Google Scholar] [CrossRef] [PubMed]
- Van Acker, H.H.; Capsomidis, A.; Smits, E.L.; Van Tendeloo, V.F. CD56 in the Immune System: More Than a Marker for Cytotoxicity? Front. Immunol. 2017, 8, 892. [Google Scholar] [CrossRef] [Green Version]
- Sato, E.; Takaira, M.; Gohara, R.; Araki, N.; Masuoka, K.; Imamura, Y. CD 56-positive acute myeloid leukemia (AML-M 1) with t(16;21) (p11;q22) presenting an extramedullary tumor in the right breast at relapse. Rinsho Ketsueki 2002, 43, 560–566. [Google Scholar]
- Ando, T.; Mitani, N.; Matsui, K.; Yamashita, K.; Nomiyama, J.; Tsuru, M.; Yujiri, T.; Tanizawa, Y. Recurrent extramedullary relapse of acute myelogenous leukemia after allogeneic hematopoietic stem cell transplantation in a patient with the chromosomal abnormality t(8;21) and CD56-positivity. Int. J. Hematol. 2009, 90, 374–377. [Google Scholar] [CrossRef]
- Vance, M.L. Growth-hormone-releasing hormone. Clin. Chem. 1990, 36, 415–420. [Google Scholar] [CrossRef]
- Jimenez, J.J.; DelCanto, G.M.; Popovics, P.; Perez, A.; Vila Granda, A.; Vidaurre, I.; Cai, R.Z.; Rick, F.G.; Swords, R.T.; Schally, A.V. A new approach to the treatment of acute myeloid leukaemia targeting the receptor for growth hormone-releasing hormone. Br. J. Haematol. 2018, 181, 476–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chu, W.K.; Law, K.S.; Chan, S.O.; Yam, J.C.; Chen, L.J.; Zhang, H.; Cheung, H.S.; Block, N.L.; Schally, A.V.; Pang, C.P. Antagonists of growth hormone-releasing hormone receptor induce apoptosis specifically in retinoblastoma cells. Proc. Natl. Acad. Sci. USA 2016, 113, 14396–14401. [Google Scholar] [CrossRef] [Green Version]
- Havt, A.; Schally, A.V.; Halmos, G.; Varga, J.L.; Toller, G.L.; Horvath, J.E.; Szepeshazi, K.; Koster, F.; Kovitz, K.; Groot, K.; et al. The expression of the pituitary growth hormone-releasing hormone receptor and its splice variants in normal and neoplastic human tissues. Proc. Natl. Acad. Sci. USA 2005, 102, 17424–17429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarandi, M.; Cai, R.; Kovacs, M.; Popovics, P.; Szalontay, L.; Cui, T.; Sha, W.; Jaszberenyi, M.; Varga, J.; Zhang, X.; et al. Synthesis and structure-activity studies on novel analogs of human growth hormone releasing hormone (GHRH) with enhanced inhibitory activities on tumor growth. Peptides 2017, 89, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Stangelberger, A.; Schally, A.V.; Djavan, B. New treatment approaches for prostate cancer based on peptide analogues. Eur. Urol. 2008, 53, 890–900. [Google Scholar] [CrossRef]
- Schally, A.V. New approaches to the therapy of various tumors based on peptide analogues. Horm. Metab. Res. 2008, 40, 315–322. [Google Scholar] [CrossRef]
- Lozzio, B.B.; Lozzio, C.B.; Bamberger, E.G.; Feliu, A.S. A multipotential leukemia cell line (K-562) of human origin. Proc. Soc. Exp. Biol. Med. 1981, 166, 546–550. [Google Scholar] [CrossRef]
- Lanotte, M.; Martin-Thouvenin, V.; Najman, S.; Balerini, P.; Valensi, F.; Berger, R. NB4, a maturation inducible cell line with t(15;17) marker isolated from a human acute promyelocytic leukemia (M3). Blood 1991, 77, 1080–1086. [Google Scholar] [CrossRef] [Green Version]
- Cassinat, B.; Chomienne, C. Biological features of primary APL blasts: Their relevance to the understanding of granulopoiesis, leukemogenesis and patient management. Oncogene 2001, 20, 7154–7160. [Google Scholar] [CrossRef] [Green Version]
- Khanna-Gupta, A.; Kolibaba, K.; Zibello, T.A.; Berliner, N. NB4 cells show bilineage potential and an aberrant pattern of neutrophil secondary granule protein gene expression. Blood 1994, 84, 294–302. [Google Scholar] [CrossRef] [Green Version]
- Gan, J.; Ke, X.; Jiang, J.; Dong, H.; Yao, Z.; Lin, Y.; Lin, W.; Wu, X.; Yan, S.; Zhuang, Y.; et al. Growth hormone-releasing hormone receptor antagonists inhibit human gastric cancer through downregulation of PAK1-STAT3/NF-kappaB signaling. Proc. Natl. Acad. Sci. USA 2016, 113, 14745–14750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yin, X.J.; Wang, R.; Shen, H.S.; Jin, J.; Zhu, H.H. At What Point Are Long-Term (>5 Years) Survivors of APL Safe? A Study from the SEER Database. Cancers 2023, 15, 575. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chale, R.S.; Almeida, S.M.; Rodriguez, M.; Jozic, I.; Gaumond, S.I.; Schally, A.V.; Jimenez, J.J. The Application of GHRH Antagonist as a Treatment for Resistant APL. Cancers 2023, 15, 3104. https://doi.org/10.3390/cancers15123104
Chale RS, Almeida SM, Rodriguez M, Jozic I, Gaumond SI, Schally AV, Jimenez JJ. The Application of GHRH Antagonist as a Treatment for Resistant APL. Cancers. 2023; 15(12):3104. https://doi.org/10.3390/cancers15123104
Chicago/Turabian StyleChale, Ravinder S., Stephanie M. Almeida, Mario Rodriguez, Ivan Jozic, Simonetta I. Gaumond, Andrew V. Schally, and Joaquin J. Jimenez. 2023. "The Application of GHRH Antagonist as a Treatment for Resistant APL" Cancers 15, no. 12: 3104. https://doi.org/10.3390/cancers15123104





