Information on COVID-19 and Psychological Distress in a Sample of Non-Health Workers during the Pandemic Period
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Measuring Instruments
2.3. Procedure and Sample
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. Sociodemographic Data and Psychological Distress
3.2. Beliefs about the Outbreak and Psychological Distress among Non-Health Workers
3.3. Accessibility, Quantity, Quality, and Usefulness of Media and Official Information Sources on COVID-19, and Level of Psychological Distress
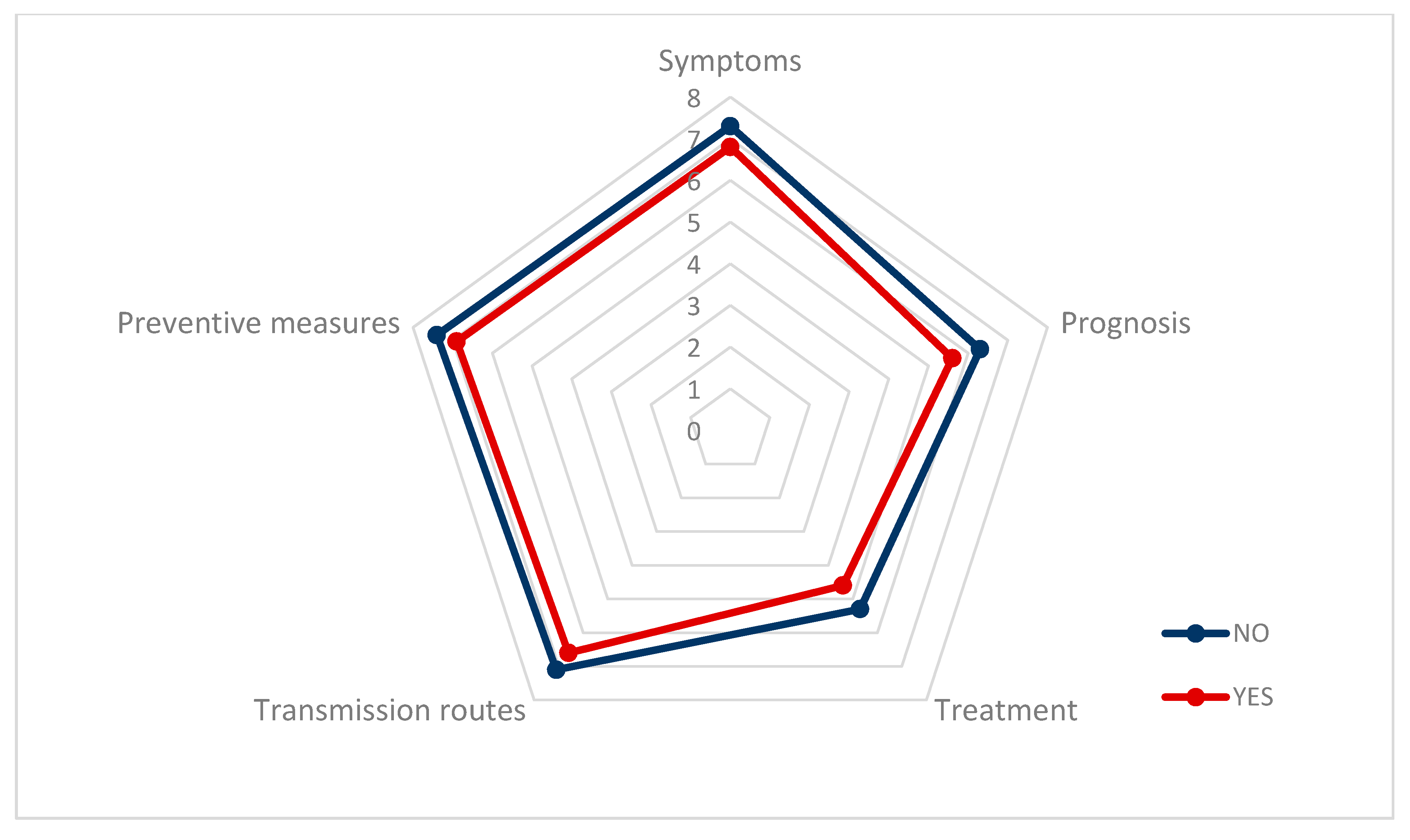
3.4. Sources of Information, Time Spent Receiving Information, and Psychological Distress
3.5. Media or Platforms to Receive Information about the COVID-19 Pandemic
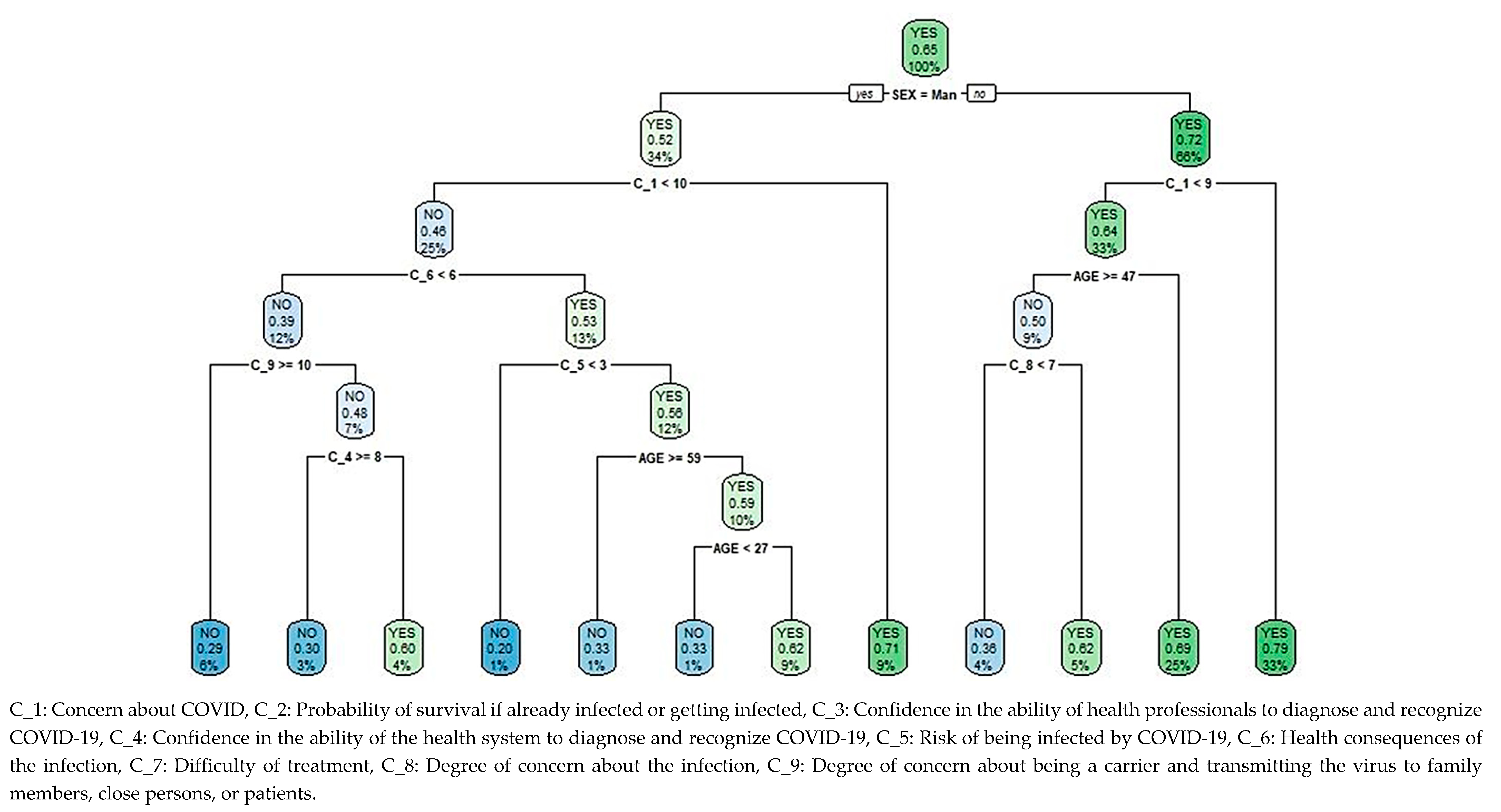
3.6. Classification and Regression Tree for the Level of Psychological Distress Based on Beliefs Regarding the Pandemic
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Novel Coronavirus (2019-nCoV) Situation Report 1. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf (accessed on 5 August 2020).
- Ciotti, M.; Angeletti, S.; Minieri, M.; Giovannettie, M.; Benvenuto, D.; Pascarella, S.; Sagnelli, C.; Bianchi, M.; Bernardini, S.; Ciccozzi, M. COVID-19 Outbreak: An Overview. Chemotherapy 2019, 64, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Ahn, D.G.; Shin, H.J.; Kim, M.H.; Lee, S.; Kim, H.S.; Myoung, J.; Kim, B.T.; Kim, S.J. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J. Microbiol. Biotechnol. 2020, 30, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sohrabia, C.; Alsafi, Z.; O’Neilla, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decisionmakers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 102211. [Google Scholar] [CrossRef]
- Gobierno de España. Ministerio de la Presidencia. Real Decreto 463/2020. Volume 67, Boletín Oficial del Estado. 2020. Available online: https://www.boe.es/buscar/pdf/2020/BOE-A-2020-3692-consolidado.pdf (accessed on 26 August 2020).
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. Situation Report-195. 2020. Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200802-covid-19-sitrep-195.pdf?sfvrsn=5e5da0c5_2 (accessed on 26 August 2020).
- Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins. Available online: https://coronavirus.jhu.edu/map.html (accessed on 26 August 2020).
- Gobierno de España. Ministerio de la Presidencia. Real Decreto-Ley 10/2020. Boletín Oficial del Estado. 2020. Available online: https://www.boe.es/buscar/pdf/2020/BOE-A-2020-4166-consolidado.pdf (accessed on 26 August 2020).
- Kimhi, S.; Eshel, Y.; Marciano, H.; Adini, B. Distress and Resilience in the Days of COVID-19: Comparing Two Ethnicities. Int. J. Environ. Res. Public Health 2020, 17, 3956. [Google Scholar] [CrossRef]
- Germani, A.; Buratta, L.; Delvecchio, E.; Mazzeschi, C. Emerging Adults and COVID-19: The Role of Individualism-Collectivism on Perceived Risks and Psychological Maladjustment. Int. J. Environ. Res. Public Health 2020, 17, 3497. [Google Scholar] [CrossRef]
- Mijiritsky, E.; Hamama-Raz, Y.; Liu, F.; Datarkar, A.N.; Mangani, L.; Caplan, J.; Shacham, A.; Kolerman, R.; Mijiritsky, O.; Ben-Ezra, M.; et al. Subjective Overload and Psychological Distress among Dentists during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 5074. [Google Scholar] [CrossRef]
- American Psychological Association. APA Dictionary of Psychology. Available online: https://dictionary.apa.org/psychological-distress (accessed on 6 August 2020).
- Chen, Y.; Jin, Y.L.; Zhu, L.J.; Fang, Z.M.; Wu, N.; Du, M.X.; Jiang, M.M.; Wang, J.; Yao, Y.S. The Network Investigation on Knowledge, Attitude and Practice about COVID-19 of the Residents in Anhui Province. Zhonghua Yu Fang Yi Xue Za Zhi 2020, 54, 367–373. [Google Scholar] [CrossRef]
- Rolison, J.J.; Hanoch, Y. Knowledge and risk perceptions of the Ebola virus in the United States. Prev. Med. Rep. 2015, 2, 262–264. [Google Scholar] [CrossRef] [Green Version]
- Videgaard, N. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020. [Advance online publication]. [Google Scholar] [CrossRef]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literatura. Asian J. Psychiatry 2020, 52, 102066. [Google Scholar] [CrossRef] [PubMed]
- Losada-Baltar, A.; Jiménez-Gonzalo, L.; Gallego-Alberto, L.; Pedroso-Chaparro, M.; Fernandes-Pires, J.; Márquez-González, M. “We’re staying at home.” Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry. Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Agüero, F.; Adell, M.N.; Giménez, A.P.; Medina, M.J.L.; Continente, X.G. Adoption of preventive measures during and after the 2009 influenza A (H1N1) virus pandemic peak in Spain. Prev. Med. 2011, 53, 203–206. [Google Scholar] [CrossRef]
- Lin, Y.; Huang, L.; Nie, S.; Liu, Z.; Yu, H.; Yan, W.; Xu, Y. Knowledge, attitudes and practices (KAP) related to the pandemic (H1N1) 2009 among Chinese general population: A telephone survey. BMC Infect. Dis. 2011, 11, 128. [Google Scholar] [CrossRef] [Green Version]
- Patel, N.; Anees, M.; Kola, R.; Acuña, J.; de la Vega, P.R.; Castro, G.; Ruiz, J.G.; Rojas, P. Association between Knowledge of Zika Transmission and Preventative Measures among Latinas of Childbearing Age in Farm-Working Communities in South Florida. Int. J. Environ. Res. Public Health 2019, 16, 1257. [Google Scholar] [CrossRef] [Green Version]
- Lau, J.T.; Griffiths, S.; Choi, K.C.; Tsui, H.Y. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infect. Dis. 2010, 10, 139. [Google Scholar] [CrossRef] [Green Version]
- Wester, M.; Giesecke, J. Ebola and healthcare worker stigma. Scand. J. Public Health 2019, 47, 99–104. [Google Scholar] [CrossRef]
- Del Vicario, M.; Bessi, A.; Zolloa, F.; Petroni, F.; Scala, A.; Caldarelli, G.; Eugene Stanley, H.; Quattrociocchi, W. The spreading of misinformation online. Proc. Natl. Acad. Sci. USA 2016, 113, 554–559. [Google Scholar] [CrossRef] [Green Version]
- Oyeyemi, S.O.; Gabarron, E.; Wynn, R. Ebola, Twitter, and misinformation: A dangerous combination? BMJ 2014, 349, g6178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venkatraman, A.; Mukhija, D.; Kumar, N.; Nagpal, S.J.S. Zika virus misinformation on the internet. Travel. Med. Infect. Dis. 2016, 14, 421–422. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.G.; Surian, D.; Leask, J.; Dey, A.; Mandl, K.D.; Coiera, E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine 2017, 35, 3033–3040. [Google Scholar] [CrossRef]
- AVAAZ. How Facebook can flatten the Curve of the Coronavirus Infodemic: Study Indicates Facebook is Rife with Bogus Cures and Conspiracy Theories that Remain on the Platform Long Enough to Put Millions of People at Risk. Report Published by AVAAZ, London. 2020. Available online: https://secure.avaaz.org/campaign/en/facebook_coronavirus_misinformation/ (accessed on 26 August 2020).
- Allington, D.; Duffy, B.; Wessely, S.; Dhavan, N.; Rubin, J. Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency. Psychol. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Hernández-García, I.; Giménez Júlvez, T. Assessment of Health Information about COVID-19 Prevention on the Internet: Infodemiological Study. JMIR Public Health Surveill 2020, 6, e18717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- International Labour Organization. COVID-19 and the World of Work. Available online: https://www.ilo.org/global/topics/coronavirus/lang--en/index.htm (accessed on 26 August 2020).
- Gobierno de España. Ministerio de Sanidad. Enfermedad por Nuevo Coronavirus COVID-19. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov-China/home.htm (accessed on 26 August 2020).
- MDPI. COVID-19 Academic Resources Center. Available online: https://www.mdpi.com/covid-19 (accessed on 9 August 2020).
- Elsevier. Novel Coronavirus Information Center. Elsevier’s Free Health and Medical Research on the Novel Coronavirus (SARS-CoV-2) and COVID-19. Available online: https://www.elsevier.com/connect/coronavirus-information-center (accessed on 6 August 2020).
- The Lancet COVID-19 Resource Centre. Available online: https://www.journals.elsevier.com/the-lancet-microbe/news/the-lancet-covid-19-resource-centre (accessed on 23 September 2020).
- Goldberg, D.P.; Gater, R.; Sartorius, N.; Ustun, T.B.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef]
- Tam, C.W.C.; Pang, E.P.F.; Lam, L.C.W.; Chiu, H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004, 34, 1197–1204. [Google Scholar] [CrossRef]
- Shultz, J.M.; Baingana, F.; Neria, Y. The 2014 Ebola outbreak and mental health: Current status and recommended response. JAMA 2015, 313, 567–568. [Google Scholar] [CrossRef] [Green Version]
- Shultz, J.M.; Cooper, J.L.; Baingana, F.; Oquendo, M.A.; Espinel, Z.; Althouse, B.M.; Marcelin, L.H.; Towers, S.; Espinola, M.; McCoy, C.B.; et al. The Role of Fear-Related Behaviors in the 2013-2016 West Africa Ebola Virus Disease Outbreak. Curr. Psychiatry Rep. 2016, 18, 104. [Google Scholar] [CrossRef]
- Abdelhafiz, A.S.; Mohammed, Z.; Ibrahim, M.E.; Ziady, H.H.; Alorabi, M.; Ayyad, M.; Sultan, E.A. Knowledge, Perceptions, and Attitude of Egyptians Towards the Novel Coronavirus Disease (COVID-19). J. Community Health 2020, 45, 881–890. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Cuan-Baltazar, J.Y.; Muñoz-Perez, M.J.; Robledo-Vega, C.; Pérez-Zepeda, M.F.; Soto-Vega, E. Misinformation of COVID-19 on the Internet: Infodemiology Study. JMIR Public Health Surveill 2020, 6, e18444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rahman, A.; Sathi, N.J. Knowledge, Attitude, and Preventive Practices toward COVID-19 among Bangladeshi Internet Users. Electron. J. Gen. Med. 2020, 17, em245. [Google Scholar] [CrossRef]
- Zhao, Y.; Cheng, S.; Yu, X.; Xu, H. Chinese Public’s Attention to the COVID-19 Epidemic on Social Media: Observational Descriptive Study. J. Med. Internet Res. 2020, 22, e18825. [Google Scholar] [CrossRef]
- Abd-Alrazaq, A.; Alhuwail, D.; Househ, M.; Hamdi, M.; Shah, Z. Top Concerns of Tweeters during the COVID-19 Pandemic: Infoveillance Study. J. Med. Internet Res. 2020, 22, e19016. [Google Scholar] [CrossRef] [Green Version]
- Teixeira da Silva, J.A. An Alert to COVID-19 Literature in Predatory Publishing Venues. J. Acad. Librariansh. 2020, 46, 102187. [Google Scholar] [CrossRef]
- Grudniewicz, A.; Moher, D.; Cobey, K.D.; Bryson, G.L.; Cukier, S.; Allen, K.; Ardern, C.; Balcom, L.; Barros, T.; Berger, M.; et al. Predatory journals: No definition, no defence. Nature 2019, 576, 210–212. [Google Scholar] [CrossRef] [Green Version]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, E37–E38. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Wang, Y.; Xue, J.; Zhao, N.; Zhu, T. The Impact of COVID-19 Epidemic Declaration on Psychological Consequences: A Study on Active Weibo Users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [Green Version]
- Cori, L.; Bianchi, F.; Cadum, E.; Anthonj, C. Risk Perception and COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3114. [Google Scholar] [CrossRef]
- Wolf, M.S.; Serper, M.; Opsasnick, L.; O’Conor, R.M.; Curtis, L.M.; Benavente, J.Y.; Wismer, G.; Batio, S.; Eifler, M.; Zheng, P.; et al. Awareness, Attitudes, and Actions Related to COVID-19 Among Adults with Chronic Conditions at the Onset of the U.S. Outbreak: A Cross-sectional Survey. Ann. Intern. Med. 2020, 173, 100–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhong, B.L.; Luo, W.; Li, H.M.; Zhang, Q.Q.; Liu, X.G.; Li, W.T.; Li, Y. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int. J. Biol. Sci. 2020, 16, 1745–1752. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Röhr, S.; Müller, F.; Jung, F.; Apfelbacher, C.; Seidler, A.; Riedel-Heller, S.G. Psychosocial Impact of Quarantine Measures During Serious Coronavirus Outbreaks: A Rapid Review. Psychiatr. Prax. 2020, 47, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact of COVID-19 in Spain: Early data report. Psychol. Trauma 2020, 12, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Atanes, M.; Recio-Barbero, M.; Saenz-Herrero, M. Are women still “the other”? Gendered mental health interventions for health care workers in Spain during COVID-19. Psychol. Trauma 2020, 12, S243–S244. [Google Scholar] [CrossRef] [PubMed]
- Leung, T.Y.; Sharma, P.; Adithipyangkul, P.; Hosie, P. Gender equity and public health outcomes: The COVID-19 experience. J. Bus Res. 2020, 116, 193–198. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Liu, T.; Liang, W.; Zhong, H.; He, J.; Chen, Z.; He, G.; Song, T.; Chen, S.; Wang, P.; Li, J.; et al. Risk factors associated with COVID-19 infection: A retrospective cohort study based on contacts tracing. Emerg. Microbes Infect. 2020, 9, 1546–1553. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, X.; Feng, Q.; Liu, L.; Yao, Y.; Shi, J. Psychological assistance during the coronavirus disease 2019 outbreak in China. J. Health Psychol. 2020, 25, 733–737. [Google Scholar] [CrossRef]
| Non-Health Workers (n = 1089) | Non-Health Workers Working Away from Home (n = 492) | Non-Health Workers Working from Home (n = 597) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GHQ12 | GHQ12 | GHQ12 | |||||||||||||
| M (SD) | NO (n = 380) | YES (n = 709) | Statistics | p | M (SD) | NO (n = 161) | YES (n = 331) | Statistics | p | M (SD) | NO | YES | Statistics | p | |
| Concern about COVID (C_1) | 8.17 (1.73) | 7.70 (1.87) | 8.42 (1.60) | 6.696 | <0.001 ** | 8.17 (1.76) | 7.83 (1.79) | 8,34 (1.72) | −3.072 | 0.002 ** | 8.17 (1.71) | 7.61 (1.92) | 8.49 (1.49) | −5.901 | <0.001 ** |
| Probability in surviving if already infected or getting infected (C_2) | 8.10 (1.84) | 8.34 (1.78) | 7.97 (1.86) | −3.137 | 0.002 ** | 8.03 (1.82) | 8.36 (1.73) | 7.87 (1.84) | 2.828 | 0.005 ** | 8.16 (1.85) | 8.32 (1.82) | 8.07 (1.87) | 1.642 | 0.101 |
| Confidence in the ability of health professionals to diagnose and recognize COVID-19 (C_3) | 8.28 (1.84) | 8.44 (1.78) | 8.20 (1.87) | −2.047 | 0.041 * | 8.28 (1.89) | 8.47 (1.81) | 8.18 (1.92) | 1.606 | 0.109 | 8.29 (1.80) | 8.42 (1.76) | 8.22 (1.83) | 1.297 | 0.195 |
| Confidence in the ability of the health system to diagnose and recognize COVID-19 (C_4) | 6.96 (2.25) | 7.26 (2.18) | 6.80 (2.27) | −3.263 | 0.001 ** | 6.82 (2.33) | 7.17 (2.22) | 6.64 (2.36) | 2.398 | 0.017 * | 7.08 (2.18) | 7.32 (2.15) | 6.93 (2.19) | 2.126 | 0.034 * |
| Risk of being infected by COVID-19 (C_5) | 5.39 (2.38) | 5.06 (2.42) | 5.57 (2.35) | 3.387 | 0.001 ** | 5.75 (2.37) | 5.35 (2.42) | 5.94 (2.32) | −2.617 | 0.009 ** | 5.10 (2.36) | 4.85 (2.39) | 5.25 (2.33) | −1.998 | 0.046 * |
| Health consequences of the infection (C_6) | 5.92 (2.39) | 5.71 (2.44) | 6.03 (2.36) | 2.115 | 0.035 * | 5.93 (2.39) | 5.73 (2.39) | 6.03 (2.39) | −1.308 | 0.192 | 5.91 (2.39) | 5.70 (2.47) | 6.03 (2.33) | −1.657 | 0.098 |
| Difficulty of treatment (C_7) | 6.89 (2.08) | 6.69 (2.14) | 7.00 (2.03) | 2.295 | 0.022 * | 6.98 (2.11) | 6.87 (2.12) | 7.03 (2.11) | −0.791 | 0.429 | 6.82 (2.05) | 6.57 (2.16) | 6.97 (1.97) | −2.266 | 0.024 * |
| Degree of concern about the infection (C_8) | 7.33 (2.37) | 6.83 (2.40) | 7.60 (2.31) | 5.113 | <0.001 ** | 7.47 (2.40) | 7.21 (2.25) | 7.59 (2.46) | −1.706 | 0.089 | 7.22 (2.35) | 6.56 (2.48) | 7.60 (2.18) | −5.182 | <0.001 ** |
| Degree of concern about being a carrier and transmitting the virus to family members, close persons, or patients (C_9) | 9.01 (1.70) | 8.83 (1.79) | 9.10 (1.64) | 2.45 | 0.015 * | 9.19 (1.46) | 9.27 (1.20) | 9.15 (1.58) | 0.846 | 0.398 | 8.86 (1.85) | 8.51 (2.06) | 9.06 (1.68) | −3.347 | 0.001 ** |
| MEDIA | OFFICIAL INFORMATION | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % GHQ12 | % GHQ12 | ||||||||||||
| n (%) | NO | YES | χ2 | p | n (%) | NO | YES | χ2 | p | χ2 | p | ||
| (n = 380) | (n = 709) | (n = 380) | (n = 709) | ||||||||||
| Accessibility | Very low | 25 (2.30) | 3.16 | 1.83 | 7.065 | 0.132 | 56 (5.14) | 3.68 | 5.92 | 5.953 | 0.203 | 442.394 | <0.001 ** |
| Low | 54 (4.96) | 3.42 | 5.78 | 128 (11.75) | 11.32 | 11.99 | |||||||
| Intermediate | 198 (18.18) | 20.00 | 17.21 | 380 (34.89) | 32.37 | 36.25 | |||||||
| High | 438 (40.22) | 41.58 | 39.49 | 382 (35.08) | 38.42 | 33.29 | |||||||
| Very high | 374 (34.34) | 31.84 | 35.68 | 143 (13.13) | 14.21 | 12.55 | |||||||
| Quantity | Very low | 15 (1.38) | 2.11 | 0.99 | 4.066 | 0.397 | 35 (3.21) | 2.89 | 3.39 | 7.530 | 0.110 | 305.737 | <0.001 ** |
| Low | 29 (2.66) | 2.89 | 2.54 | 123 (11.29) | 10.53 | 11.71 | |||||||
| Intermediate | 117 (10.74) | 10.26 | 11.00 | 396 (36.36) | 31.84 | 38.79 | |||||||
| High | 304 (27.92) | 30.00 | 26.80 | 384 (35.26) | 39.47 | 33.00 | |||||||
| Very high | 624 (57.30) | 54.74 | 58.67 | 151 (13.87) | 15.26 | 13.12 | |||||||
| Quality | Very low | 110 (10.10) | 9.74 | 10.30 | 2.606 | 0.626 | 135 (12.40) | 11.32 | 12.98 | 5.074 | 0.280 | 451.026 | <0.001 ** |
| Low | 254 (23.32) | 21.05 | 24.54 | 220 (20.20) | 18.68 | 21.02 | |||||||
| Intermediate | 543 (49.86) | 50.79 | 49.37 | 428 (39.30) | 39.47 | 39.21 | |||||||
| High | 162 (14.88) | 16.58 | 13.96 | 263 (24.15) | 25.00 | 23.70 | |||||||
| Very high | 20 (1.84) | 1.84 | 1.83 | 43 (3.95) | 5.53 | 3.10 | |||||||
| Usefulness | Very low | 75 (6.89) | 7.11 | 6.77 | 6.156 | 0.188 | 108 (9.92) | 8.42 | 10.72 | 6.945 | 0.139 | 541.742 | <0.001 ** |
| Low | 210 (19.28) | 16.05 | 21.02 | 196 (18.00) | 17.11 | 18.48 | |||||||
| Intermediate | 532 (48.85) | 48.68 | 48.94 | 428 (39.30) | 37.11 | 40.48 | |||||||
| High | 246 (22.59) | 25.00 | 21.30 | 290 (26.63) | 29.47 | 25.11 | |||||||
| Very high | 26 (2.39) | 3.16 | 1.97 | 67 (6.15) | 7.89 | 5.22 | |||||||
| Non-Health Workers (n = 1089) | Non-Health Workers Working Away from Home (n = 492) | Non-Health Workers Working from Home (n = 597) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GHQ12 | GHQ12 | GHQ12 | |||||||||||||
| M (SD) | NO (n = 380) | YES (n = 709) | Statistics | p | M (SD) | NO (n = 161) | YES (n = 331) | Statistics | p | M (SD) | NO (n = 219) | YES (n = 378) | Statistics | p | |
| No of sources | 3.37 (1.98) | 3.29 (1.94) | 3.41 (2.00) | 0.994 | 0.321 | 3.25 (1.98) | 3.29 (1.93) | 3.23 (2.00) | −0.328 | 0.743 | 3.47 (1.98) | 3.29 (1.96) | 3.58 (1.99) | 1.718 | 0.086 |
| n. hours daily | 2.84 (2.53) | 2.48 (1.98) | 3.04 (2.76) | 3.861 | <0.001 | 2.97 (2.50) | 2.73 (2.17) | 3.09 (2.64) | 1.519 | 0.129 | 2.74 (2.55) | 2.30 (1.82) | 2.99 (2.86) | 3.637 | <0.001 |
| Information on COVID-19 * | |||||||||||||||
| Symptoms | 7.05 (2.35) | 7.36 (2.30) | 6.88 (2.37) | −3.241 | 0.001 | 6.83 (2.43) | 6.99 (2.44) | 6.75 (2.43) | −1.033 | 0.302 | 7.23 (2.27) | 7.64 (2.16) | 7.00 (2.31) | −3.353 | 0.001 |
| Prognosis | 5.79 (2.38) | 6.30 (2.37) | 5.52 (2.34) | −5.173 | <0.001 | 5.57 (2.38) | 5.94 (2.38) | 5.39 (2.37) | −2.422 | 0.016 | 5.98 (2.36) | 6.56 (2.33) | 5.64 (2.31) | −4.652 | <0.001 |
| Treatment | 4.79 (2.45) | 5.28 (2.58) | 4.52 (2.33) | −4.753 | <0.001 | 4.57 (2.41) | 5.00 (2.49) | 4.36 (2.35) | −2.781 | 0.006 | 4.96 (2.46) | 5.48 (2.63) | 4.66 (2.31) | −3.809 | <0.001 |
| Transmission routes | 6.82 (2.45) | 7.17 (2.35) | 6.63 (2.48) | −3.430 | 0.001 | 6.63 (2.54) | 6.81 (2.52) | 6.54 (2.55) | −1.117 | 0.264 | 6.98 (2.36) | 7.42 (2.19) | 6.72 (2.41) | −3.570 | <0.001 |
| Preventive measures | 6.99 (2.47) | 7.36 (2.30) | 6.79 (2.54) | −3.731 | <0.001 | 6.75 (2.60) | 7.12 (2.38 | 6.56 (2.69) | −2.317 | 0.021 | 7.19 (2.35) | 7.53 (2.24) | 6.99 (2.39) | −2.749 | 0.006 |
| Clear and precise information offered by department, service, unit, company * | 6.16 (2.89) | 6.54 (2.76) | 5.95 (2.94) | −3.274 | 0.001 | 5.87 (2.99) | 6.11 (2.79) | 5.75 (3.08) | −1.290 | 0.209 | 6.39 (2.79) | 6.85 (2.71) | 6.12 (2.80) | −3.106 | 0.002 |
| Means or Platforms through Which Information on the COVID-19 Pandemic is Made Accessible | No of Cases | Percentage |
|---|---|---|
| Social media (WhatsApp, Facebook, Instagram, etc.) | 843 | 77.41 |
| Television | 695 | 63.82 |
| Friends or relatives | 461 | 42.33 |
| Webpages of official organisms or scientific societies | 447 | 41.05 |
| Papers (online or paper) | 436 | 40.04 |
| Google or other search engines | 309 | 28.37 |
| Radio | 297 | 27.27 |
| Mobile phones or apps for official information | 131 | 12.03 |
| Other (professional bodies, companies, …) | 52 | 4.78 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Frutos, C.; Ortega-Moreno, M.; Dias, A.; Bernardes, J.M.; García-Iglesias, J.J.; Gómez-Salgado, J. Information on COVID-19 and Psychological Distress in a Sample of Non-Health Workers during the Pandemic Period. Int. J. Environ. Res. Public Health 2020, 17, 6982. https://doi.org/10.3390/ijerph17196982
Ruiz-Frutos C, Ortega-Moreno M, Dias A, Bernardes JM, García-Iglesias JJ, Gómez-Salgado J. Information on COVID-19 and Psychological Distress in a Sample of Non-Health Workers during the Pandemic Period. International Journal of Environmental Research and Public Health. 2020; 17(19):6982. https://doi.org/10.3390/ijerph17196982
Chicago/Turabian StyleRuiz-Frutos, Carlos, Mónica Ortega-Moreno, Adriano Dias, João Marcos Bernardes, Juan Jesús García-Iglesias, and Juan Gómez-Salgado. 2020. "Information on COVID-19 and Psychological Distress in a Sample of Non-Health Workers during the Pandemic Period" International Journal of Environmental Research and Public Health 17, no. 19: 6982. https://doi.org/10.3390/ijerph17196982
APA StyleRuiz-Frutos, C., Ortega-Moreno, M., Dias, A., Bernardes, J. M., García-Iglesias, J. J., & Gómez-Salgado, J. (2020). Information on COVID-19 and Psychological Distress in a Sample of Non-Health Workers during the Pandemic Period. International Journal of Environmental Research and Public Health, 17(19), 6982. https://doi.org/10.3390/ijerph17196982









