Abstract
The COVID-19 pandemic itself and related public health measurements have had substantial impacts on individual social lives and psychological and mental health, all to the detriment of health-related quality of life (HRQoL). There have been extensive studies investigating the mental health of people in different populations during the COVID-19 pandemic. However, few studies have explored the impact of COVID-19 and its association with HRQoL. To fill this research gap and provide further empirical evidence, this study examined the impact of COVID-19 on Hong Kong people and evaluated its association with HRQoL. A total of 500 participants were randomly recruited to complete an online questionnaire on their concerns related to COVID-19. This entailed responding to the World Health Organization Quality of Life-BREF instrument. Data were collected between 24 April and 3 May 2020. Independent t-tests and multiple linear regressions were used to examine the association between the impact of COVID-19 and HRQoL. Overall, 69.6% of participants were worried about contracting COVID-19, and 41.4% frequently suspected themselves of being infected. Furthermore, 29.0% were concerned by the lack of disinfectants. All of these findings were associated with poorer HRQoL in the physical and psychological health, social relationships, and environment domains. On the other hand, 47.4% of participants were concerned that they may lose their job because of the pandemic, while 39.4% were bothered by the insufficient supply of surgical masks. These two factors were associated with poorer HRQoL in the physical and psychological health and environment domains. The adverse impact of COVID-19 on individuals is multifactorial, affecting all aspects of HRQoL. In addition to enhancing anti-epidemic efforts, it is equally important to implement public health and social welfare measures, thereby diminishing the adverse impact of COVID-19 on overall well-being.
1. Introduction
In December 2019, the highly contagious coronavirus disease COVID-19 emerged in Wuhan City, China [1]. The initial outbreak rapidly evolved into an explosive global pandemic [2], affecting more than 180 countries and regions [3]. With the number of confirmed COVID-19 cases surging past 10 million globally as of 15 July 2020 [3], there seems to be no end in sight to the health crisis. Since learning of the viral outbreak in January 2020, the Hong Kong government has implemented precautionary measures to attenuate the spread of infection, such as physical distancing rules, mandatory quarantine, travel restrictions, and temporary closure of schools and certain entertainment establishments [4,5,6,7]. Although these preventative measures played a role in averting a major local epidemic [5], these tough controls, coupled with the health threats from COVID-19, may lead to detrimental effects on individuals’ health-related quality of life (HRQoL) [8].
The World Health Organization has conceptualized HRQoL as an individual’s perception of his or her health and health-related domains of well-being [9]. HRQoL is dynamic, subjective and multidimensional. The dimensions include physical, social, psychological and environmental factors [9,10]. HRQoL is an important clinical outcome because poor HRQoL is associated with adverse clinical outcomes. For example, a study among Scottish adults found that physical aspects of HRQoL could predict all-cause death, incident cancer and coronary heart disease [11]. A study of Spanish older adults also found that changes in HRQoL could predict mortality [12]. Another study also found that a decrease in HRQoL has been significantly associated with increased odds of negative outcomes, including the inability to work due to health, hospitalization at one year and mortality [13].
With respect to the psychological impact of COVID-19, it has been found that the viral outbreak has had a substantial effect on people’s mental health [4,14,15,16]. Apart from the fear of direct health threats, psychosocial stressors, such as severe disruptions to routines, shortages of daily necessities, overwhelming amounts of health information related to COVID-19, and uncertainty over the outbreak could all be associated with heightened levels of anxiety and depression [14,17,18]. Concerning social factors, the lack of face-to-face social interaction could compromise social well-being despite the use of digital communications. It is suggested that social isolation and loneliness could pose diverse health risks to individuals, and in particular, lead to lower resilience to stress [19], higher risk of depression [20], less effective immune responses [20], and a decline in cognitive function [21]. Amid the pandemic, border shutdowns, travel restrictions, and quarantine policies have caused widespread economic aftershocks [22]. Nearly all sectors, especially hospitality, aviation, and the tourism industry, have faced an unprecedented economic crisis, resulting in a record-high unemployment rate in Hong Kong. Accordingly, income instability could undermine the HRQoL of individuals [23].
For most Hong Kong people, the COVID-19 pandemic reminded them of the difficult time in 2003, when severe acute respiratory syndrome (SARS) took the lives of nearly 300 local citizens [24]. Hence, at the very beginning of the current pandemic, the public stocked up surgical marks, disinfectants, and other cleaning products as precautions. Together with the public health measures imposed by the local government, this had certainly affected people’s HRQoL. However, there is little information on this aspect to date [25], as existing studies have mainly focused on the impact of COVID-19 and its associations with depression, anxiety, and fear [4,26]. In view of this, to supplement previous studies and provide a more holistic view of the adverse impact of COVID-19, this study aimed to investigate the impact of the viral outbreak on Hong Kong people and to evaluate its association with HRQoL. Assessing HRQoL during the COVID-19 pandemic helps identify the impacts of the pandemic on people’s everyday lives. Therefore, clinicians, social workers and other healthcare professionals can develop appropriate psychosocial interventions to alleviate the impacts of the pandemic on people’s well-being and daily lives.
2. Materials and Methods
2.1. Study Design
This was a cross-sectional study.
2.2. Setting and Participants
This study was a community-based study, which was carried out in Hong Kong. To be eligible, study participants would need to be (i) currently living in Hong Kong, (ii) able to read and understand Chinese, and (iii) aged 18 years or older.
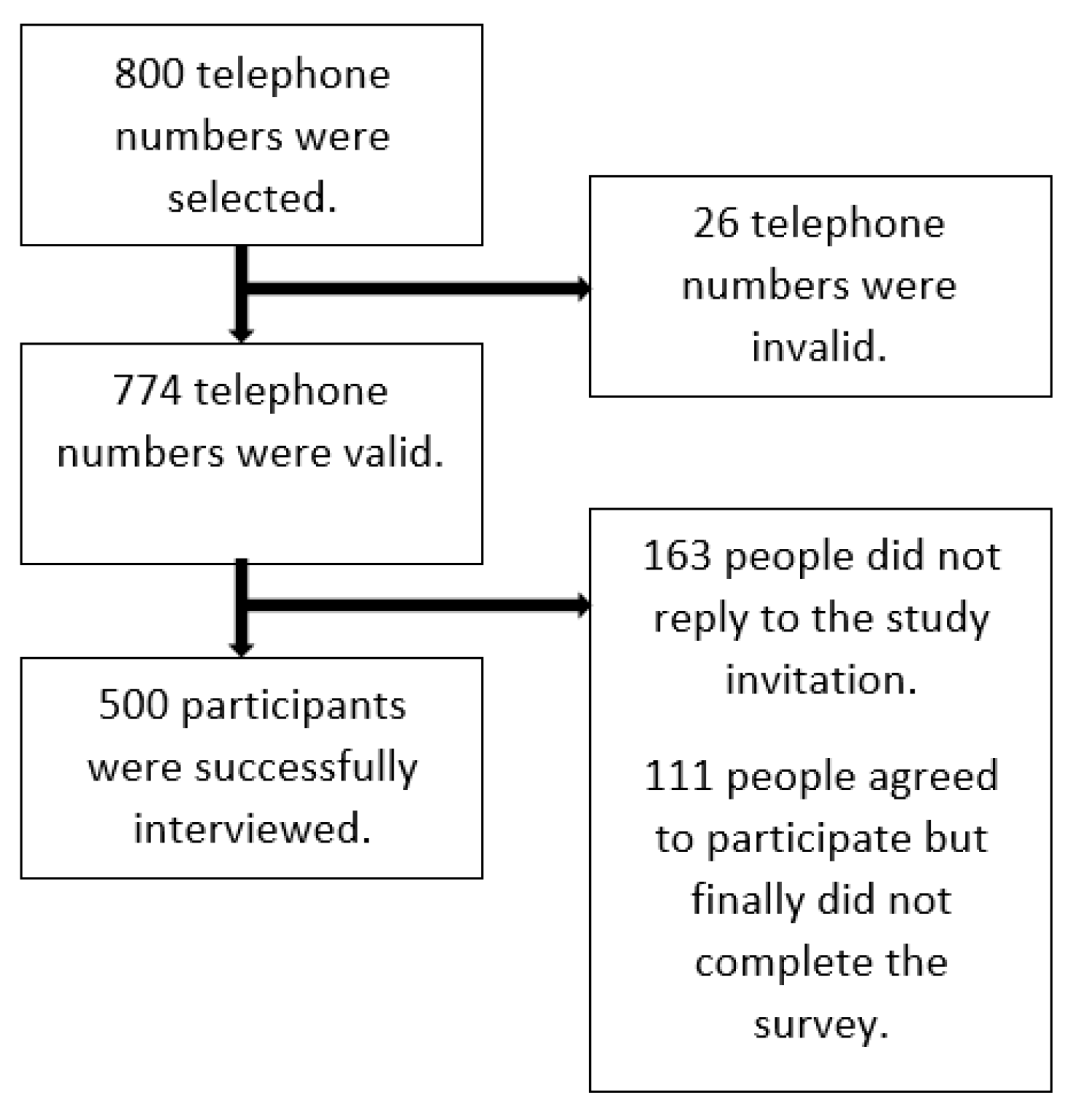
A mobile phone-based random sampling approach was used to recruit study participants. The random list of mobile phone numbers was generated through the numbering plan for telecommunication services in Hong Kong provided by the Office of the Communications Authority. Mobile text messages were sent to randomly selected study participants to invite them to take part. After they had agreed to complete the questionnaire study, a link to a self-administered online survey was sent to them. The data collection period was between 24 April and 3 May 2020 in Hong Kong, which was approximately three months after the first local COVID-19 case was reported. Figure 1 shows the flow diagram of recruitment.
Figure 1.
The flow diagram of recruitment.
2.3. Study Instruments
The World Health Organization Quality of Life-BREF (WHOQOL-BREF) was used to measure the generic HRQoL in the study [27]. The WHOQOL-BREF consists of 24 questions in four domains, namely physical health (seven items), psychological health (six items), social relationships (three items), and environment (eight items). Each question w rated on a 5-point Likert scale. The scores within each domain are averaged. These average domain scores are multiplied by 4 to obtain transformed scores on a scale of 4–20 according to the guideline of the study instrument. Finally, the transformed domain scores are transformed linearly to a 0–100 scale [28,29,30], with a higher score indicating better HRQoL. The instrument has been validated among Chinese individuals living in Hong Kong [31]. Permission to use this instrument was obtained from the World Health Organization.
To assess the impact of COVID-19 on individuals’ HRQoL, the following statements were developed for the present study:
- (i)
- I feel worried that I will be infected with COVID-19;
- (ii)
- I feel worried that my family members will be infected with COVID-19;
- (iii)
- I feel bothered because I often suspect that I have COVID-19 symptoms;
- (iv)
- I feel bothered because I do not have enough surgical masks;
- (v)
- I feel bothered because I do not have enough disinfectant supplies at home;
- (vi)
- I feel worried that I may lose my job because of COVID-19.
The recall period for these five statements was two weeks, and a 4-point Likert scale was used (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day).
These items about the impact of COVID-19 were developed by the investigation team based on the pandemic situation from January 2020 to March 2020 in Hong Kong. The items were piloted on five people before we rolled out the study.
Participants also had to answer questions on sociodemographics, including gender, age, marital status, educational attainment, employment status, and income.
2.4. Statistical Analysis
First, descriptive statistics, such as mean and standard deviation (SD), were used to summarize the domain scores of the WHOQOL-BREF as well as sociodemographic characteristics. Second, we dichotomized the responses of the 6 statements related to COVID-19. Study participants who answered “0 = not at all” were coded as “no”, while study participants who answered “1 = several days”, “2 = more than half the days”, or “3 = nearly every day” were coded as “yes”. Independent t-tests were used to compare the mean HRQoL score of four domains between two groups (“yes” vs. “no”). Cohen’s d was also calculated, which classifies effect sizes as small (d = 0.2), medium (d = 0.5), and large (d = 0.8) [32]. Third, multiple linear regression analysis was used to test the robustness of the relationship between the impact of COVID-19 and the four domains of HRQoL after controlling for the sociodemographic factors.
The program Statistical Package for the Social Sciences (version 25) was used for data analysis. p-values < 0.05 indicated statistical significance.
2.5. Ethics
Ethics approval was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB). Reference: UW20-217.
Electronic informed consent was obtained for each participant.
3. Results
3.1. Sample Characteristics
The mean age was 47.26 years (SD = 15.82), with 274 (54.8%) females and 226 males. 336 participants (67.2%) were currently married, and 281 participants (56.2%) had a full-time job. There were 159 participants (31.8%) with a bachelor’s degree or above, while 339 participants (67.8%) had a monthly personal income less than Hong Kong Dollar (HKD$) 20,001. Table 1 presents the sociodemographic characteristics of the study participants.

Table 1.
Demographics of the participants.
3.2. Impact of COVID-19
Overall, 348 participants (69.6%) were worried about contracting COVID-19, while 371 participants (74.2%) were worried that their family members would be infected by COVID-19. We found that 207 participants (41.4%) often suspected themselves of being infected. Furthermore, 197 participants (39.4%) feared that they would run out of surgical masks, and 145 participants (29.0%) were bothered by not having enough disinfectant supplies at home. Finally, 237 participants (47.4%) were concerned that they might lose their job because of COVID-19. Table 1 presents the descriptive statistics for the impact of COVID-19 on study participants.
3.3. HRQOL Scores
Compared with participants who at ease with the risk of infection, those who worried about contracting COVID-19 had poorer HRQoL across the four domains. We also found that those who worried that their family members would be infected with COVID-19 had poorer physical aspects of HRQoL only.
For participants, who often suspected themselves of being infected, and therefore, feeling worried had poorer HRQoL across the four domains than those who were not. Participants who were bothered by the insufficient supply of surgical masks had poorer HRQoL in three of the four domains than those who were not worried: physical health, psychological health and environment.
Participants who were concerned about the lack of enough insufficient disinfectant supplies had poorer HRQoL in all four domains. Finally, participants who were worried about job loss due to COVID-19 had poorer HRQoL in physical health, psychological health and environment domains.
Table 2 presents the results of the independent t-tests. The association between the impact of COVID and HRQoL remained statistically significant in multiple linear regressions after controlling for the sociodemographic factors. Table 3 shows the results of the multiple linear regression analysis.

Table 2.
Results of independent t-tests.

Table 3.
Results of multiple linear regressions.
4. Discussion
Many participants were worried that they would be infected with COVID-19. There are some possible explanations. First, Hong Kong is not far from Wuhan, China, where the initial outbreak of COVID-19 is thought to have occurred [33]. Moreover, the viral outbreak occurred shortly before the Chinese New Year, when crowds of people traveled back to the hometowns or other parts of the country (including Hong Kong) to gather with their family. Hong Kong citizens worried that there would be a huge surge of new imported COVID-19 cases from other parts of China, giving rise to active community transmission within Hong Kong.
We found that the fear of infection was associated with poorer HRQoL. Fear and anxiety related to COVID-19 are known to be common stressors during the COVID-19 pandemic. Excessive stress can cause psychological and physiological disruption, leading to fatigue, poor performance, and emotional control problems [34]. A review suggests that stress affects the immune system, gastrointestinal function, and endocrine system [35]. For instance, psychological stress may interfere with the immune function through direct innervation of lymphatic tissue, through the release of hypothalamic-pituitary-adrenocortical axis and sympathetic-adrenal-medullary hormones that bind to and alter the functions of immunologically active cells, or through stress-induced behavioral changes [36]. Furthermore, psychological stress may also influence physical health through its effects on other systems. For example, psychological stress was found to impair vagal tone, leading to an increased risk of cardiovascular diseases [36,37].
In addition, the fear of acquiring COVID-19 disease has led to a significant decrease in group gatherings and trips outside the home. The public is encouraged to reduce social contact and maintain physical distance to minimize the risk of transmission among the community. In spite of the use of digital communications, social relationships could be compromised due to the lack of face-to-face social interaction. Social isolation and loneliness are also found to be closely correlated with poorer physical [38] and psychological health [20].
Our findings showed that more than 40% of the study participants often suspected themselves of having COVID-19. As most people with mild COVID-19 would experience flu-like symptoms, the most common being mild fever, cough, fatigue, and diarrhea [39,40], it is understandable that some of them would think that they were infected. Besides, the result could also be explained by Barsky and Wyshak’s (1990) model of hypochondriasis and somatosensory amplification [41]. During the COVID-19 pandemic, there is ample evidence to suggest that people suffered from stress [42], fear [26], a high level of anxiety and depression [4], and hypochondriasis. When a hypochondriac is sick, he/she may pay more attention to bodily processes and misattribute a broad range of somatic sensations and misattribute them to serious diseases, which is COVID-19 in this case [43]. Consequently, it would heighten their stress level, and in turn, affect their physical and psychological health. Nonetheless, to supplement our quantitative findings, further qualitative studies should be conducted to understand why people often suspected themselves of having COVID-19.
Amid the pandemic, people more often seek out COVID-19-related health information more frequently so as to gain better insight and understanding of the latest development [44,45]. A study in mainland China found that a higher social media exposure during COVID-19 was associated with higher odds of anxiety (odds ratio = 1.72) and a combination of depression and anxiety (odds ratio = 1.91) [46]. Furthermore, people are likely to be exposed to misleading content on social media platforms, either through disinformation or misinformation [44,47]. Their anxiety might be exacerbated when the situation is exaggerated, and consequences are overestimated. In addition, harmless bodily sensations and changes may also be misinterpreted as signs of infection, which results in distress and worsens people’s psychological and physical health [43]. This explains why we found that people who had constant suspicion of being infected with COVID-19 had poorer HRQoL, particularly in the physical and psychological domains.
Furthermore, our study found that the lack of surgical masks and disinfectant supplies at home troubled nearly 40% and 30% of participants, respectively. After the SARS outbreak in 2003, most people in Hong Kong have realized the significance of protection provided surgical masks and proper hand hygiene. Moreover, to fight COVID-19, the Hong Kong government also recommends wearing a surgical mask when taking public transport or staying in crowded places and performing hand hygiene frequently [48]. Understanding the efficacy and importance of surgical masks and disinfectants, Hong Kong people flocked to stock up on these protective and cleaning supplies during the COVID-19 pandemic. However, at the very beginning of the pandemic, there was a shortage and a general price rise for such products [4]. With panic-buying sprees, many struggled to obtain sufficient disinfectant supplies. The sight of empty shelves in stores could cause widespread consternation, and those who could not obtain enough facemasks and disinfectants might be worried that they were at higher risk of infection. In addition to the fear of contracting the virus, poorer psychosocial health could be associated with unjustified public fear. Due to fear and bias, people not wearing masks are often discriminated against in Hong Kong, as they are viewed as egocentric and inconsiderate for exposing others to the risk of infection. Therefore, people who were bothered by not having enough surgical masks and disinfectant supplies had poorer HRQoL in the physical, psychological, and environmental aspects.
Lastly, almost half of the study participants were scared about losing their job. Market instability and lockdown induced by the ongoing COVID-19 pandemic may increase the likelihood of a global economic downturn [22]. With the pandemic disrupting almost all economic activities, business plummeted in nearly all sectors, especially the hospitality, aviation, and tourism industries, which are the major pillars of Hong Kong’s economy. Many employees in Hong Kong are prone to salary reduction and dismissal. According to the statistics from the Census and Statistics Department, the seasonally adjusted unemployment rate has been surging for the past 9 months, climbing to its highest level in 15 years at 5.9% (as of May 2020) [49]. Therefore, it is reasonable to fear redundancies. Income instability and fear of dismissals could lead to economic insecurity, which is found to be associated with poorer self-rated health and a number of health issues, for example, back problems, muscular pain, overall fatigue, and insomnia [50]. Apart from these adverse impacts on physical health, uncertainty about future finance and employment may also be a source of psychological stress on people [51]. Existing studies have found that job insecurity is negatively related to overall marital and family functioning, as well as mental health [50,51,52].
Limitations
It is prudent to highlight a number of limitations of the present study. First, the temporal relationship between COVID-19 and HRQoL cannot be explored due to the cross-sectional design. Second, all outcomes were self-reported, and the findings may be affected by reporting bias. Third, there could be sampling bias from the use of an online survey in the current study; people with lower computer literacy or lower socioeconomic status may be underrepresented in the current study. However, due to the pandemic, it is not feasible to conduct a household survey. Fourth, the study findings may not be generalizable to other populations. Differences in mortality rate, incidence rates, government policy, and even the public’s belief and attitudes toward the use of surgical masks may affect how people perceive the impact of COVID-19 on their lives and daily activities. Fifth, a generic HRQoL instrument was used in the study, which may not be specific and sensitive enough to capture the impact of COVID-19 on HRQoL. Sixth, only six self-developed items were used to capture the impacts of COVID-19 in the current study. We acknowledged that these items were not representative enough to capture the worry and fear related to COVID-19 as the pandemic evolves. Nonetheless, the items were very relevant to people in Hong Kong at that particular period of time. Seventh, other important information such as health status and the number of family members were not collected. Future studies should collect the information and explore its association with HRQoL.
5. Conclusions
The present study found that almost 70% of the participants were worried about contracting COVID-19. Approximately 40% of participants often suspected themselves of being infected with COVID-19 and were bothered by the lack of sufficient surgical masks and job insecurity. All these negative effects of COVID-19 were associated with poorer HRQoL across different domains. Therefore, in addition to enhancing anti-epidemic measures through physical distancing, border closure, and active surveillance of COVID-19 cases, it is equally important to implement public health and social welfare policies to diminish the adverse impact of COVID-19 on the overall well-being.
Author Contributions
E.P.H.C. design of the work, acquisition of data, data analysis, interpretation of data and writing the manuscript; B.P.H.H. design of the work, interpretation of data and writing the manuscript; E.Y.F.W. design of the work, data analysis, interpretation of data and revising the manuscript; J.Y.Y.K. conceptualization of the study and critical review of the manuscript T.H.L.T. writing the manuscript; C.W. writing the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the LKS Faculty of Medicine, The University of Hong Kong.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB) (protocol code UW 20-217 and date of approval: 18 March 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
We would like to thank Social Policy Research Limited for data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. Who Declares Covid-19 a Pandemic? Acta Bio Med. Atenei Parm. 2020, 91, 157–160. [Google Scholar]
- Johns Hopkins University. Covid-19 Dashboard. Available online: https://coronavirus.jhu.edu/map.html (accessed on 15 July 2020).
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in hong kong during covid-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef] [PubMed]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.; Tsang, T.K.; Li, J.C.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Law, S.; Leung, A.W.; Xu, C. Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): From causes to preventions in hong kong. Int. J. Infect. Dis. 2020, 94, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Kwok, K.O.; Li, K.K.; Chan, H.H.; Yi, Y.Y.; Tang, A.; Wei, W.I.; Wong, S.Y. Community responses during early phase of covid-19 epidemic, hong kong. Emerg. Infect. Dis. 2020, 26, 1575–1579. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, Z.F. Impact of the covid-19 pandemic on mental health and quality of life among local residents in liaoning province, china: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef]
- Bakas, T.; McLennon, S.M.; Carpenter, J.S.; Buelow, J.M.; Otte, J.L.; Hanna, K.M.; Ellett, M.L.; Hadler, K.A.; Welch, J.L. Systematic review of health-related quality of life models. Health Qual. Life Outcomes 2012, 10, 1–12. [Google Scholar] [CrossRef]
- Haas, B.K. A multidisciplinary concept analysis of quality of life. West. J. Nurs. Res. 1999, 21, 728–742. [Google Scholar] [CrossRef] [PubMed]
- Ul-Haq, Z.; Mackay, D.F.; Pell, J.P. Association between physical and mental health-related quality of life and adverse outcomes; a retrospective cohort study of 5272 scottish adults. BMC Public Health 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Otero-Rodríguez, A.; León-Muñoz, L.M.; Balboa-Castillo, T.; Banegas, J.R.; Rodríguez-Artalejo, F.; Guallar-Castillón, P. Change in health-related quality of life as a predictor of mortality in the older adults. Qual. Life Res. 2010, 19, 15–23. [Google Scholar] [CrossRef]
- Bjorner, J.B.; Wallenstein, G.V.; Martin, M.C.; Lin, P.; Blaisdell-Gross, B.; Tak Piech, C.; Mody, S.H. Interpreting score differences in the sf-36 vitality scale: Using clinical conditions and functional outcomes to define the minimally important difference. Curr. Med. Res. Opin. 2007, 23, 731–739. [Google Scholar] [CrossRef]
- Mamun, M.A.; Griffiths, M.D. First COVID-19 suicide case in bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J. Psychiatry 2020, 51, 102073. [Google Scholar] [CrossRef]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and psychometric evaluation of the italian version of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 2020, 1–10. [Google Scholar] [CrossRef]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S. The Psychology of Pandemics: Preparing for the Next Global Outbreak of Infectious Diseas; Cambridge Scholars Publishing: Newcastle upon Tyne, UK, 2019. [Google Scholar]
- Fiorillo, A.; Gorwood, P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 2020, 63, e32. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Cacioppo, S.; Capitanio, J.P.; Cole, S.W. The neuroendocrinology of social isolation. Annu. Rev. Psychol. 2015, 66, 733–767. [Google Scholar] [CrossRef] [PubMed]
- Matthews, T.; Danese, A.; Wertz, J.; Odgers, C.L.; Ambler, A.; Moffitt, T.E.; Arseneault, L. Social isolation, loneliness and depression in young adulthood: A behavioural genetic analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 339–348. [Google Scholar] [CrossRef]
- Shankar, A.; Hamer, M.; McMunn, A.; Steptoe, A. Social isolation and loneliness: Relationships with cognitive function during 4 years of follow-up in the english longitudinal study of ageing. Psychosomat. Med. 2013, 75, 161–170. [Google Scholar] [CrossRef]
- Fernandes, N. Economic Effects of Coronavirus Outbreak (COVID-19) on the World Economy. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3557504 (accessed on 15 July 2020).
- Davalos, M.E.; French, M.T. This recession is wearing me out! Health-related quality of life and economic downturns. J. Ment. Health Policy Econ. 2011, 14, 61–72. [Google Scholar] [PubMed]
- Leung, G.; Ho, L.; Lam, T.; Hedley, A. Epidemiology of sars in the 2003 Hong Kong epidemic. Hong Kong Med. J. 2009, 15, 12–16. [Google Scholar] [PubMed]
- Algahtani, F.D.; Hassan, S.-u.-N.; Alsaif, B.; Zrieq, R. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the kingdom of saudi arabia. Int. J. Environ. Res. Public Health 2021, 18, 847. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.-Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef]
- Group, W. Development of the world health organization whoqol-bref quality of life assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- Gholami, A.; Jahromi, L.M.; Zarei, E.; Dehghan, A. Application of whoqol-bref in measuring quality of life in health-care staff. Int. J. Prev. Med. 2013, 4, 809. [Google Scholar]
- Choi, E.P.; Wong, J.Y.; Fong, D.Y. Mental health and health-related quality of life of chinese college students who were the victims of dating violence. Qual. Life Res. 2017, 26, 945–957. [Google Scholar] [CrossRef]
- Chew, B.-H.; Mohd-Sidik, S.; Shariff-Ghazali, S. Negative effects of diabetes–related distress on health-related quality of life: An evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in malaysia. Health Qual. Life Outcomes 2015, 13, 187. [Google Scholar] [CrossRef] [PubMed]
- Leung, K.; Wong, W.; Tay, M.; Chu, M.; Ng, S. Development and validation of the interview version of the hong kong chinese whoqol-bref. Qual. Life Res. 2005, 14, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and anovas. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Heymann, D.L. Data sharing and outbreaks: Best practice exemplified. Lancet 2020, 395, 469–470. [Google Scholar] [CrossRef]
- Kowalski, K.C.; Crocker, P.R. Development and validation of the coping function questionnaire for adolescents in sport. J. Sport Exerc. Psychol. 2001, 23, 136–155. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Panahi, Y.; Sahraei, H.; Johnston, T.P.; Sahebkar, A. The impact of stress on body function: A review. EXCLI J. 2017, 16, 1057. [Google Scholar]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W. Cardiac vagal tone: A physiological index of stress. Neurosci. Biobehav. Rev. 1995, 19, 225–233. [Google Scholar] [CrossRef]
- Pressman, S.D.; Cohen, S.; Miller, G.E.; Barkin, A.; Rabin, B.S.; Treanor, J.J. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychol. 2005, 24, 297. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Mu, M.; Yang, P.; Sun, Y.; Wang, R.; Yan, J.; Li, P.; Hu, B.; Wang, J.; Hu, C. Clinical characteristics of COVID-19 patients with digestive symptoms in hubei, china: A descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020, 115, 766–773. [Google Scholar] [CrossRef]
- Singhal, T. A review of coronavirus disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 1–6. [Google Scholar] [CrossRef]
- Barsky, A.J.; Wyshak, G.; Klerman, G.L. The somatosensory amplification scale and its relationship to hypochondriasis. J. Psychiatr. Res. 1990, 24, 323–334. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in china. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Rief, W.; Broadbent, E. Explaining medically unexplained symptoms-models and mechanisms. Clin. Psychol. Rev. 2007, 27, 821–841. [Google Scholar] [CrossRef]
- Cuan-Baltazar, J.Y.; Muñoz-Perez, M.J.; Robledo-Vega, C.; Pérez-Zepeda, M.F.; Soto-Vega, E. Misinformation of COVID-19 on the internet: Infodemiology study. JMIR Public Health Surveill. 2020, 6, e18444. [Google Scholar] [CrossRef]
- Hernández-García, I.; Giménez-Júlvez, T. Assessment of health information about covid-19 prevention on the internet: Infodemiological study. JMIR Public Health Surveill. 2020, 6, e18717. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 0020764020915212. [Google Scholar] [CrossRef]
- Feng, S.; Shen, C.; Xia, N.; Song, W.; Fan, M.; Cowling, B.J. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020, 8, 434–436. [Google Scholar] [CrossRef]
- Census and Statistics Department The HKSAR. Labour Force. Available online: https://www.censtatd.gov.hk/hkstat/sub/sp200.jsp?tableID=006&ID=0&productType=8 (accessed on 15 July 2020).
- Caroli, E.; Godard, M. Does job insecurity deteriorate health? Health Econ. 2016, 25, 131–147. [Google Scholar] [CrossRef]
- Bünnings, C.; Kleibrink, J.; Weßling, J. Fear of unemployment and its effect on the mental health of spouses. Health Econ. 2017, 26, 104–117. [Google Scholar] [CrossRef] [PubMed]
- McDonough, P. Job insecurity and health. Int. J. Health Serv. 2000, 30, 453–476. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).