Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging
Abstract
:1. Introduction
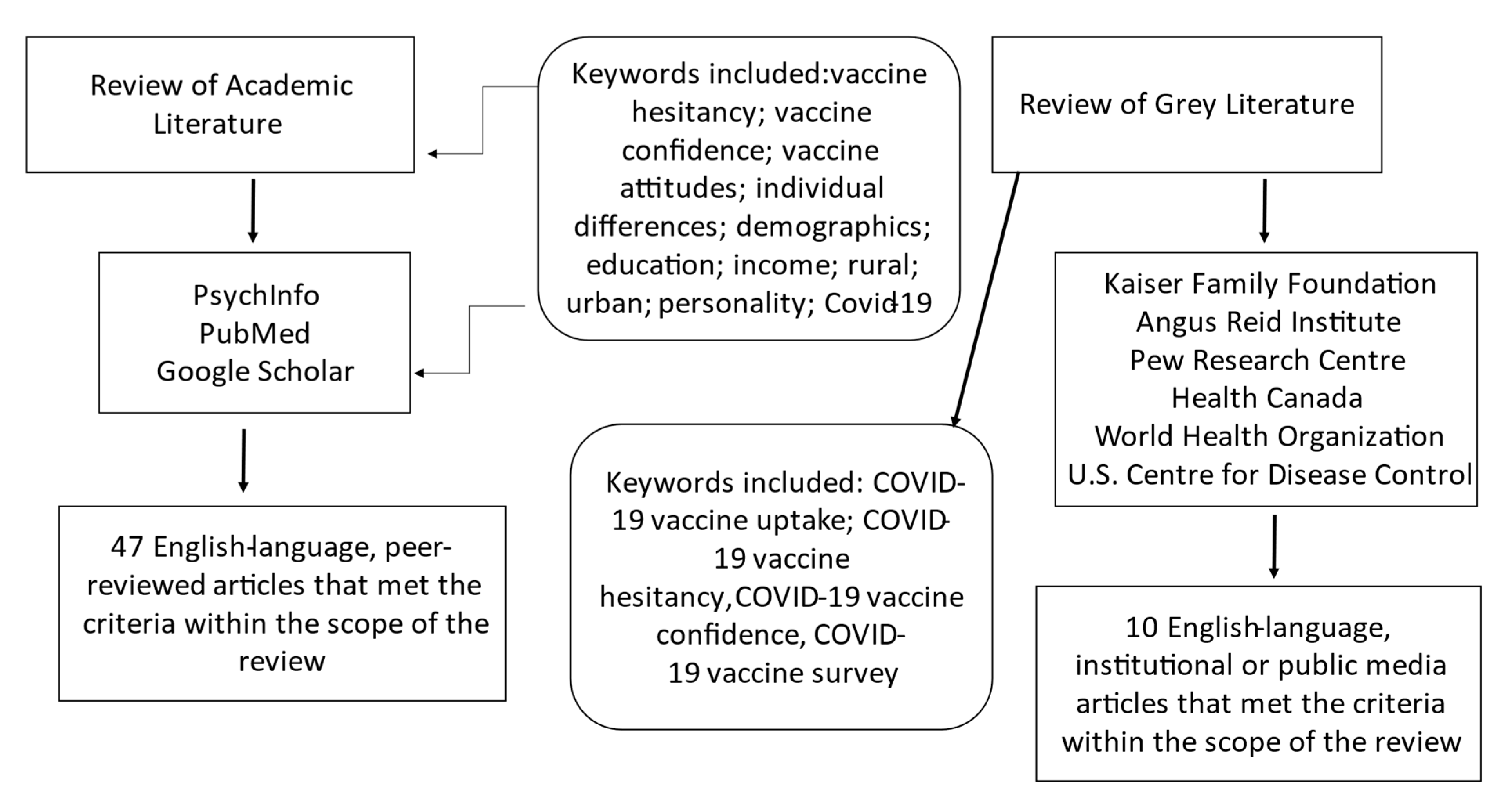
2. Method
3. Results and Discussion
3.1. Age
3.2. Socioeconomic Status
3.3. Education and Health Literacy
3.4. Parental Status
3.5. Rurality
3.6. Mistrust in Authority
3.7. Disgust Sensitivity
3.8. Risk Aversion
3.9. Limitations and Future Directions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO) Epidemiological Report 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update---1-december-2020 (accessed on 28 March 2021).
- Health Canada. Covid-19 Outbreak Updates 2021. Available online: https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html (accessed on 28 March 2021).
- Walensky, R.P.; Del Rio, C. From mitigation to containment of the COVID-19 pandemic: Putting the SARS-CoV-2 genie back in the bottle. JAMA 2020, 323, 1889–1890. [Google Scholar] [CrossRef]
- Wilder-Smith, A.; Freedman, D.O. Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 2020, 27, taaa020. [Google Scholar] [CrossRef] [PubMed]
- Health Canada. Vaccines and Treatments for Covid-19: Vaccine Rollout 2021. Available online: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/covid-19-vaccine-treatment/vaccine-rollout.html (accessed on 28 March 2021).
- Jacobson, R.M.; Sauver, J.L.S.; Rutten, L.J.F. Vaccine Hesitancy. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2015; pp. 1562–1568. [Google Scholar]
- Heininger, U.; Bachtiar, N.S.; Bahri, P.; Dana, A.; Dodoo, A.; Gidudu, J.; Matos dos Santos, E. The concept of vaccination failure. Vaccine 2012, 30, 1265–1268. [Google Scholar] [CrossRef]
- Health Canada. Moderna Covid-19 Vaccine: What You Should Know 2021. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/moderna.html#a3-Canada.ca (accessed on 28 March 2021).
- Health Canada. Pfizer-BioNTech COVID-19 Vaccine: What You Should Know 2021. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/covid19-industry/drugs-vaccines-treatments/vaccines/pfizer-biontech.html (accessed on 28 March 2021).
- Harrison, E.A.; Wu, J.W. Vaccine confidence in the time of COVID-19. Eur. J. Epidemiol. 2020, 35, 325–330. [Google Scholar] [CrossRef] [Green Version]
- Conrod, P.J.; O’Leary-Barrett, M.; Newton, N.; Topper, L.; Castellanos-Ryan, N.; Mackie, C.; Girard, A. Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry 2013, 70, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Hudson, A.; Thompson, K.; MacNevin, P.D.; Ivany, M.; Teehan, M.; Stuart, H.; Stuart, H.S. University students’ perceptions of links between substance use and mental health: A qualitative focus group study. Emerg. Adulthood 2018, 6, 399–410. [Google Scholar] [CrossRef]
- Funk, C.; Tyson, A. Intent to Get a COVID-19 Vaccine Rises to 60% as Confidence in Research and Development Process Increases. Pew Res. Center 2020, 3, 1–45. [Google Scholar]
- Greenberg, J.; Dubé, E.; Driedger, M. Vaccine hesitancy: In search of the risk communication comfort zone. PLoS Curr. 2017, 9. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Ten Threats to Public Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 28 March 2021).
- Gates, B. Responding to Covid-19—A once-in-a-century pandemic? NEJM 2020. [Google Scholar] [CrossRef]
- Wu, S.; Su, J.; Yang, P.; Zhang, H.; Li, H.; Chu, Y.; Hua, W.; Li, C.; Tang, Y.; Wang, Q. Factors associated with the uptake of seasonal influenza vaccination in older and younger adults: A large, population-based survey in Beijing, China. BMJ Open 2017, 7, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Luyten, J.; Bruyneel, L.; van Hoek, A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine 2019, 37, 2494–2501. [Google Scholar] [CrossRef] [PubMed]
- Opel, D.J.; Taylor, J.A.; Mangione-Smith, R.; Solomon, C.; Zhao, C.; Catz, S.; Martin, D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011, 29, 6598–6605. [Google Scholar] [CrossRef] [PubMed]
- Azizi, F.S.M.; Kew, Y.; Moy, F.M. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine 2017, 35, 2955–2961. [Google Scholar] [CrossRef] [PubMed]
- Mitra, T.; Counts, S.; Pennebaker, J. Understanding anti-vaccination attitudes in social media. In Proceedings of the International AAAI Conference on Web and Social Media; AAAI Press: Palo Alto, CA, USA, 2016. [Google Scholar]
- Volkman, J.E.; Hokeness, K.L.; Morse, C.R.; Viens, A.; Dickie, A. Information source’s influence on vaccine perceptions: An exploration into perceptions of knowledge, risk and safety. J. Commun. Heal. 2021, 14, 50–60. [Google Scholar] [CrossRef]
- Fietkiewicz, K.J.; Lins, E.; Baran, K.S.; Stock, W.G. Inter-generational comparison of social media use: Investigating the online behavior of different generational cohorts. In Proceedings of the 49th Hawaii International Conference on System Sciences, Koloa, HI, USA, 5–8 January 2016; pp. 3829–3838. [Google Scholar]
- Wei, F.; Mullooly, J.P.; Goodman, M.; Mccarty, M.C.; Hanson, A.M.; Crane, B.; Nordin, J. Identification and characteristics of vaccine refusers. BMC Pediatrics 2009, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Luthy, K.E.; Beckstrand, R.L.; Callister, L.C. Parental hesitation in immunizing children in Utah. Public Health Nurs. 2010, 27, 25–31. [Google Scholar] [CrossRef]
- Sia, D.; Fournier, P.; Kobiané, J.F.; Sondo, B.K. Rates of coverage and determinants of complete vaccination of children in rural areas of Burkina Faso (1998–2003). BMC Public Health 2009, 9, 1–10. [Google Scholar] [CrossRef]
- Wu, A.C.; Wisler-Sher, D.J.; Griswold, K.; Colson, E.; Shapiro, E.D.; Holmboe, E.S.; Benin, A.L. Postpartum mothers’ attitudes, knowledge, and trust regarding vaccination. Matern. Child. Health J. 2008, 12, 766–773. [Google Scholar] [CrossRef]
- Ambwani, S.; Sellinger, G.; Rose, K.L.; Richmond, T.K.; Sonneville, K.R. “It’s healthy because it’s natural.” Perceptions of “clean” eating among US adolescents and emerging adults. Nutrients 2020, 12, 1708. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, J. Vaccine hesitancy: A growing concern. Pediatric Drugs 2020, 22, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Carpiano, R.M.; Polonijo, A.N.; Gilbert, N.; Cantin, L.; Dubé, E. Socioeconomic status differences in parental immunization attitudes and child immunization in Canada: Findings from the 2013 Childhood National Immunization Coverage Survey (CNICS). Prev. Med. 2019, 123, 278–287. [Google Scholar] [CrossRef]
- Danis, K.; Georgakopoulou, T.; Stavrou, T.; Laggas, D.; Panagiotopoulos, T. Socioeconomic factors play a more important role in childhood vaccination coverage than parental perceptions: A cross-sectional study in Greece. Vaccine 2010, 28, 1861–1869. [Google Scholar] [CrossRef]
- Larson, H.J.; De Figueiredo, A.; Zhao, X.; Schulz, W.S.; Verger, P.; Johnston, I.; Cook, A.; Jones, N.S. The state of vaccine confidence 2016: Global insights through a 67-country survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Vikram, K.; Vanneman, R.; Desai, S. Linkages between maternal education and childhood immunization in India. Soc. Sci. Med. 2012, 75, 331–339. [Google Scholar] [CrossRef] [Green Version]
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of vaccine Hesitancy across five low- and middle-income countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montelpare, W.J. Principles of Health- or what the health are you thinking? Epidemics Pandemics Spread Illn. 2021, in press. [Google Scholar]
- Burton, D.R. Antibodies, viruses and vaccines. Nat. Rev. Immunol. 2002, 2, 706–713. [Google Scholar] [CrossRef]
- Hoffmann, A.R.; Proctor, L.M.; Surette, M.G.; Suchodolski, J.S. The microbiome: The trillions of microorganisms that maintain health and cause disease in humans and companion animals. Vet. Pathol. 2016, 53, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Gangarosa, E.J.; Galazka, A.M.; Wolfe, C.R.; Phillips, L.M.; FRCPath, E.M.; Chen, R.T.; Gangarosa, R.E. Impact of anti-vaccine movements on pertussis control: The untold story. Lancet 1998, 351, 356–361. [Google Scholar] [CrossRef]
- Abdel-Latif, M.M. The enigma of health literacy and COVID-19 pandemic. Public Health 2020, 185, 95–96. [Google Scholar] [CrossRef]
- Olisarova, V.; Kaas, J.; Staskova, V.; Bartlova, S.; Papp, K.; Nagorska, M.; Korucova, R.; Reifsnider, E. Health literacy and behavioral health factors in adults. Public Health 2021, 190, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Bundt, T.S.; Hu, H.M. National examination of compliance predictors and the immunization status of children: Precursor to a developmental model for health systems. Mil. Med. 2004, 169, 795–803. [Google Scholar] [CrossRef] [Green Version]
- Mergler, M.J.; Omer, S.B.; Pan, W.K.; Navar-Boggan, A.M.; Orenstein, W.; Marcuse, E.K.; Taylor, J.; Dehart, M.P.; Carter, T.C.; Damico, A.; et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine 2013, 31, 4591–4595. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.L.; Huang, Z.; Ren, J.; Laffoon, M.; Ji, M.; Pinckney, L.C.; Sun, X.; Prosser, L.A.; Boulton, M.L.; Zikmund-Fisher, B.J. Vaccine hesitancy and concerns about vaccine safety and effectiveness in Shanghai, China. Am. J. Prev. Med. 2020, 60, 77–86. [Google Scholar] [CrossRef]
- Hamel, L.; Kirzinger, A.; Munana, C.; Brodie, M. KFF COVID-19 Vaccine Monitor December 2020. Available online: www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/ (accessed on 1 March 2021).
- Freeman, D.; Waite, F.; Rosebrock, L.; Petit, A.; Causier, C.; East, A.; Jenner, L.; Teale, A.L.; Carr, L.; Mulhall, S.; et al. Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 2020, 1–13. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 1–15. [Google Scholar] [CrossRef]
- Douglas, K.M.; Uscinski, J.E.; Sutton, R.M.; Cichocka, A.; Nefes, T.; Ang, C.S.; Deravi, F. Understanding conspiracy theories. Political Psychol. 2019, 40, 3–35. [Google Scholar] [CrossRef] [Green Version]
- Reuben, R.; Aitken, D.; Freedman, J.L.; Einstein, G. Mistrust of the medical profession and higher disgust sensitivity predict parental vaccine hesitancy. PLoS ONE 2020, 15, e0237755. [Google Scholar] [CrossRef]
- Jones, A.M.; Omer, S.B.; Bednarczyk, R.A.; Halsey, N.A.; Moulton, L.H.; Salmon, D.A. Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv. Prev. Med. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Jolley, D.; Douglas, K.M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS ONE 2014, 9, e89177. [Google Scholar] [CrossRef]
- Greer, A.M.; Amlani, A.; Burmeister, C.; Scott, A.; Newman, C.; Lampkin, H.; Pauly, B.; Buxton, J.A. Peer engagement barriers and enablers: Insights from people who use drugs in British Columbia, Canada. Can. J. Public Health 2019, 110, 227–235. [Google Scholar] [CrossRef]
- Tybur, J.M.; Lieberman, D.; Griskevicius, V. Microbes, mating, and morality: Individual differences in three functional domains of disgust. J. Personal. Soc. Psychol. 2019, 97, 1–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clifford, S.; Wendell, D.G. How disgust influences health purity attitudes. Political Behav. 2016, 38, 155–178. [Google Scholar] [CrossRef]
- Amin, A.B.; Bednarczyk, R.A.; Ray, C.E.; Melchiori, K.J.; Graham, J.; Huntsinger, J.R.; Omer, S.B. Association of moral values with vaccine hesitancy. Nat. Hum. Behav. 2017, 1, 873–880. [Google Scholar] [CrossRef] [PubMed]
- Horne, Z.; Powell, D.; Hummel, J.E.; Holyoak, K.J. Countering antivaccination attitudes. Proc. Natl. Acad. Sci. USA 2015, 112, 10321–10324. [Google Scholar] [CrossRef] [Green Version]
- Charpentier, C.J.; Aylward, J.; Roiser, J.P.; Robinson, O.J. Enhanced risk aversion, but not loss aversion, in unmedicated pathological anxiety. Biol. Psychiatry 2017, 81, 1014–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benin, A.L.; Wisler-Scher, D.J.; Colson, E.; Shapiro, E.D.; Holmboe, E.S. Qualitative analysis of mothers’ decision-making about vaccines for infants: The importance of trust. Pediatrics 2006, 117, 1532–1541. [Google Scholar] [CrossRef]
- Noyman-Veksler, G.; Greenberg, D.; Grotto, I.; Shahar, G. Parents’ malevolent personification of mass vaccination solidifies vaccine hesitancy. J. Heal. Psychol. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.F.; Wang, R.H.; Schneider, J.K.; Tsai, C.T.; Jiang, D.D.S.; Hung, M.N.; Lin, L.J. Using the health belief model to understand caregiver factors influencing childhood influenza vaccinations. J. Community Health Nurs. 2011, 28, 29–40. [Google Scholar] [CrossRef]
- Shapiro, G.K.; Tatar, O.; Dube, E.; Amsel, R.; Knauper, B.; Naz, A.; Perez, S.; Rosberger, Z. The vaccine hesitancy scale: Psychometric properties and validation. Vaccine 2018, 36, 660–667. [Google Scholar] [CrossRef]
- Bhopal, S.; Nielsen, M. Vaccine hesitancy in low-and middle-income countries: Potential implications for the COVID-19 response. Arch. Dis. Child. 2020, 106, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Zajenkowski, M.; Jonason, P.K.; Leniarska, M.; Kozakiewicz, Z. Who complies with the restrictions to reduce the spread of COVID-19: Personality and perceptions of the COVID-19 situation. Pers. Individ. Differ. 2020, 166, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Burki, T. Understanding variants of SARS-CoV-2. Lancet 2021, 397, 462. [Google Scholar] [CrossRef]
- Navin, M.C.; Wasserman, J.A.; Ahmad, M.; Bies, S. Vaccine education, reasons for refusal, and vaccination behavior. Am. J. Prev. Med. 2019, 56, 359–367. [Google Scholar] [CrossRef]
| Predictors of Vaccine Hesitancy | Population | Key Findings |
|---|---|---|
| Older and younger adults in China | Reasons for vaccinating varied by age with susceptibility to disease predicting influenza vaccine uptake in older adults and perceived effectiveness predicting vaccination in younger adults [17]. | |
| Age | Adults and young adults in the U.K. | Vaccine attitudes differed across age groups, with adults 50 to 59 reporting more confidence in vaccines than adults 20 to 29 [18] |
| Parents in the U.S.; Parents in Malaysia | Younger parental age was associated with vaccine hesitancy as measured by the Parent Attitudes about Childhood Vaccines Questionnaire [19,20] | |
| Adults in the U.S.; Adults in Germany | Increased social media use contributed to negative vaccine attitudes, and centennials and millennials were the primary users of social media platforms [21–23] | |
| Implications: Observed age group differences in vaccine hesitancy have connotations for developing effective vaccination campaigns. Findings of increased hesitancy among young adults indicate a need for communications targeted at those cohorts (i.e., sharing evidence-based content over social media). | ||
| Socioeconomic Status | Families in the U.S. with children under 6 | Families who refused vaccines for their children were more likely to reside in higher-income communities than families who vaccinated [24] |
| Parents of dependent children in the U.S. | Parents of under-immunized children were largely middle-class and college-educated [25] | |
| Families with infants aged 12–23 months in West Africa | Standard of living was associated with the vaccination status of children, with well-off families being more likely to have children who were vaccinated than families living in poverty [26] | |
| Postpartum mothers in the U.S. | Low income was associated with less trustful attitudes toward vaccination [27] | |
| Implications: Vaccine campaigns should not be reduced to targeting communities based on SES, as vaccine hesitancy is an issue across social classes. Future research is required to explain why income relates differently to vaccination behaviours and attitudes in different samples. | ||
| Education | Canadian parents | Higher educational attainment related to fewer concerns over vaccine safety, according to results of the National Childhood Immunization Coverage Survey [30] |
| Greek parents of 6-year-old children | Paternal education of high school or higher predicted age-appropriate immunizations of children [31] | |
| Families in the U.S. with children under 6 | Families who refused vaccines for their children tended to reside in communities with higher educational attainment, based on census data [24] | |
| Mothers from several low- to middle-income countries | Education was unrelated to vaccine hesitancy in a multi-ethnic sample, using the WHO Vaccine Hesitancy Scale [34] | |
| Implications: Educational campaigns may be effective means for addressing knowledge gaps and correcting misinformation. Public education should explain the mechanisms of action of vaccines using everyday terminology and plain language. Education on the history of transmissible disease and the role of vaccination programs in controlling outbreaks will create pertinent conversations in combatting the COVID-19 pandemic. Vaccine uptake strategies geared toward individuals with adequate education and health literacy should depart from educational agendas and, instead, focus on perceived risks and fears. | ||
| Parental Status | British adults responding to an adapted WHO Vaccine Hesitancy Scale | Participants with young children experienced the most aversion to potential side effects and risks of vaccines [18] |
| Parents in Malaysia | The most common reason for vaccine hesitancy among parents with young children was concern over side effects [20] | |
| Parents in West Africa; Parents in the U.S.; Parents in Greece | Family size was a consistent predictor of vaccine uptake, and families with 3+ children were more likely to refuse immunizations [26,31,41] | |
| Postpartum mothers in the U.S.; Parents in the U.S. | Parental vaccine decisions were strongly linked to health care provider recommendations. Parents who were vaccine-hesitant were more likely to have care providers who questioned the overuse of immunizations [25,27,42] | |
| Implications: Findings highlight the importance of knowledge sharing between health care providers and parents. Parent-centred information on vaccines should be distributed by primary care providers in ways that are efficient and effective. Brochures, pamphlets, and web-based aids for parents are all evidence-based outlets shown to positively affect parents’ intent to vaccinate. Much of this research has taken place with parents of young children, representing a notable knowledge gap given that age guidelines are currently 12+ for the Pfizer/BioNTech vaccine and 18+ for the Moderna vaccine. a | ||
| Rurality | Parents in Greece | Longer travel time to vaccine administration sites has been cited as a barrier to being vaccinated [31] |
| Mothers in rural and urban areas of China | Mothers from rural regions report significantly lower vaccination rates for their children compared to mothers in urban areas [43] | |
| Adults in the U.K. | Vaccine confidence was stronger among urban residents than individuals residing in rural areas in the U.K [18] | |
| Adults in the U.S. | Surveys completed in December 2020 revealed greater vaccine hesitancy among rural respondents than the general population, with 35% of rural participants indicating that they would probably not or definitely not get a COVID-19 vaccine [44] | |
| Implications: Discrepancies in rural versus urban settings need to be addressed by efforts to boost vaccine confidence in rural regions and by attempts to decentralize vaccination clinics. Otherwise, geographical differences in vaccine hesitancy could lead to disparities in vaccination coverage and localized COVID-19 outbreaks for the foreseeable future. | ||
| Mistrust in Authority | Parents in Canada, the U.S., the U.K. | Mistrust in the medical profession predicted vaccine hesitancy in parents in Canada, the U.S., and the U.K [47] |
| Parents in the U.S. | Individuals who lacked trust in their family physician were more likely to consult the Internet for advice on vaccinations, which, in turn, negatively affected vaccination attitudes and behaviours [48] | |
| Adults in the U.S. | Mistrust was a common reason for not planning to get a COVID-19 vaccine. Fifty-five percent of survey respondents stated they lacked trust in the government to ensure vaccine safety and effectiveness [44] | |
| Adults in the U.K.; Adults in Ireland | Adults who self-identified as vaccine-hesitant on a COVID-19 vaccine survey reported mistrust in authorities and a reluctance to obtain information from traditional sources [45] | |
| Implications: One strategy for addressing mistrust is to share knowledge through relatable sources (i.e., peers). Other areas of public health, such as substance use prevention and intervention, have emphasized peer-led initiatives. Individuals experiencing mistrust in government or the health system may be more responsive to members of the public sharing their intentions to immunize or providing information they receive from credible sources. Incorporating a community voice and highlighting collaboration between experts, leaders, and peers could help build vaccine confidence among this population. | ||
| Disgust Sensitivity | Parents in the U.S., U.K., and Canada | Respondents who scored higher on global measures of disgust sensitivity were more vaccine-hesitant, as per scores on the Parent Attitudes about Childhood Vaccines Scale [47] |
| Undergraduate university students in the U.S. | Positive associations have been found between pathogen disgust sensitivity and vaccine hesitancy among university students [52] | |
| Parents in the U.S. | Purity values (another measure of disgust sensitivity) were associated with high levels of vaccine hesitancy among parents. High-hesitancy respondents were over twice as likely to endorse strong purity values [53] | |
| Implications: Associations between disgust sensitivity and vaccine hesitancy highlight a need to integrate broader themes into vaccine discussions. Disgust-sensitive individuals may respond better to content that uses technical and logical terms and avoids potential triggers for disgust, such as images of needles puncturing skin. Emphasizing the vaccine’s mechanism for building immunity as a natural bodily response may resonate with individuals with strong purity values. | ||
| Risk Aversion | Israeli Parents | Trait anxiety is closely linked to risk aversion, and individuals high in anxiety have been found to experience greater levels of vaccine hesitancy [55,57] |
| Mothers with young infants | Qualitative research has provided insight into a preference for passive risk (i.e., not vaccinating) over taking a risk through active behaviour, in a phenomenon known as the omission bias [56] | |
| Adults in low- and middle-income countries | Studies using the WHO Vaccine Hesitancy Scale have found that a majority of people believe new vaccines carry more risk than older vaccines [34] | |
| Parents and caregivers in Taiwan | Fear and risk aversion can promote vaccination when individuals perceive the vaccine-preventable disease as being prevalent and/or dangerous [58] | |
| Implications: Building a sense of safety among the public will be essential to addressing the outlined fears. Work is needed to ensure that transportation to vaccine clinics and the clinics themselves are organized in a way that limits the opportunity for transmission, which will help address some concerns. Accurate information around the outcomes and risks of the disease versus outcomes and risks of vaccination should be provided to encourage individuals to accurately calculate risk and make informed decisions. Public health communications must acknowledge that decision making is not purely cognitive but driven heavily by emotions, especially fear. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudson, A.; Montelpare, W.J. Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. Int. J. Environ. Res. Public Health 2021, 18, 8054. https://doi.org/10.3390/ijerph18158054
Hudson A, Montelpare WJ. Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. International Journal of Environmental Research and Public Health. 2021; 18(15):8054. https://doi.org/10.3390/ijerph18158054
Chicago/Turabian StyleHudson, Amanda, and William J. Montelpare. 2021. "Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging" International Journal of Environmental Research and Public Health 18, no. 15: 8054. https://doi.org/10.3390/ijerph18158054
APA StyleHudson, A., & Montelpare, W. J. (2021). Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. International Journal of Environmental Research and Public Health, 18(15), 8054. https://doi.org/10.3390/ijerph18158054





