Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review
Abstract
:1. Introduction
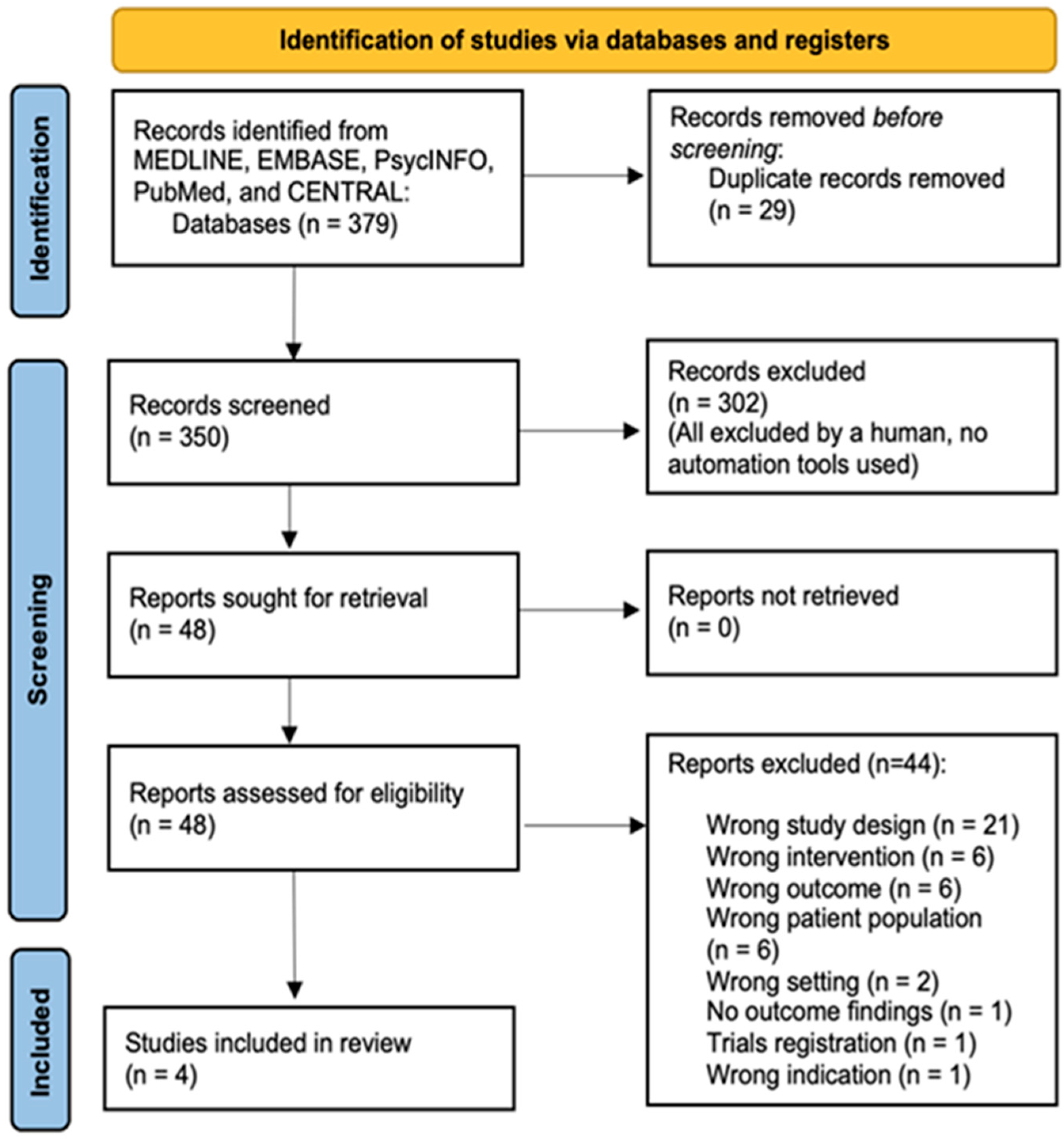
2. Material and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Selection Process
2.4. Methodological Quality
2.5. Selection Process
2.6. Data Extraction
2.7. Methodological Quality
2.8. Data Synthesis
3. Results
Study Characteristics
4. Discussion
4.1. The Role of 360° Virtual Tour in Psychological Stress Reduction
4.2. VR Video Games as a Form of Recreational Use during the Lockdown
4.3. Meditative Effect of 3D vs. 2D Format
4.4. The VR Program Implemented in COVID-19 Recovery Unit (CRU)
4.5. Shared Elements for VR in the Psychological Intervention for a Patient with Mental Health Problems
4.6. Limitations of VR as a Digital Health Intervention: For Patients and the Healthcare Staff
4.7. Strength and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A. Modified McMaster Critical Review Form
| Domains | Yes | No | Not Addressed | Not Applicable |
|---|---|---|---|---|
| Study purpose | Yes | No | Na | NA |
| 1. Was the purpose stated clearly? | ||||
| Literature review | Yes | No | Na | NA |
| 2. Was relevant background literature reviewed? | ||||
| Sample | Yes | No | Na | NA |
| 3. Was the sample described in detail? | ||||
| 4. Was sample size justified? | ||||
| 5. Were the groups randomized? | ||||
| 6. Was randomization appropriately done? | ||||
| Outcome | Yes | No | Na | NA |
| 7. Were the outcome measures reliable? | ||||
| 8. Were the outcome measures valid? | ||||
| Results | Yes | No | Na | NA |
| 9. Were results reported in terms of statistical significance? | ||||
| 10. Were the analysis of method(s) appropriate? | ||||
| 11. Was clinical importance reported? | ||||
| 12. Were drop-outs reported? | ||||
| Conclusions | Yes | No | Na | NA |
| 13. Were conclusions appropriate, given study methods and results? |
References
- Kumar, A.; Singh, R.; Kaur, J.; Pandey, S.; Sharma, V.; Thakur, L.; Sati, S.; Mani, S.; Asthana, S.; Sharma, T.K.; et al. Wuhan to World: The COVID-19 Pandemic. Front. Cell. Infect. Microbiol. 2021, 11, 596201. [Google Scholar] [CrossRef]
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19); StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- New Straits Times. COVID-19: Movement Control Order Imposed with Only Essential Sectors Operating. 2020. Available online: https://web.archive.org/web/20200316224520/https://www.nst.com.my/news/nation/2020/03/575177/covid-19-movement-control-order-imposed-only-essential-sectors-operating (accessed on 3 December 2021).
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Chi, X.; Becker, B.; Yu, Q.; Willeit, P.; Jiao, C.; Huang, L.; Hossain, M.M.; Grabovac, I.; Yeung, A.; Lin, J.; et al. Prevalence and Psychosocial Correlates of Mental Health Outcomes among Chinese College Students during the Coronavirus Disease (COVID-19) Pandemic. Front. Psychiatry 2020, 7, 803. [Google Scholar] [CrossRef]
- da Silva, F.C.T.; Neto, M.L.R. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2020, 104, 110057. [Google Scholar] [CrossRef]
- South China Morning Post. Coronavirus: Malaysia in Partial Lockdown from March 18 to Limit Outbreak. Available online: https://www.scmp.com/week-asia/health-environment/article/3075456/coronavirus-malaysias-prime-minister-muhyiddin-yassin (accessed on 10 November 2021).
- Berge, L.I.; Gedde, M.H.; Husebo, B.S.; Erdal, A.; Kjellstadli, C.; Vahia, I.V. Age and Emotional Distress during COVID-19: Findings from Two Waves of the Norwegian Citizen Panel. Int. J. Environ. Res. Public Health 2021, 18, 9568. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef]
- Cai, H.Z.; Tu, B.R.; Ma, J.; Chen, L.M.; Fu, L.; Jiang, Y.F.; Zhuang, Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of Coronavirus Disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 2020, 26, e924171-1–e924171-16. [Google Scholar]
- Liu, X.; Luo, W.T.; Li, Y.; Li, C.N.; Hong, Z.S.; Chen, H.L.; Xiao, F.; Xia, J.Y. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 2020, 9, 58. [Google Scholar] [CrossRef]
- Liu, S.; Yang, L.; Zhang, C.; Xiang, Y.T.; Liu, Z.; Hu, S.; Zhang, B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e17–e18. [Google Scholar] [CrossRef]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. Social Capital and Sleep Quality in Individuals Who Self-Isolated for 14 Days during the Coronavirus Disease 2019 (COVID-19) Outbreak in January 2020 in China. Med. Sci. Monit. 2020, 26, e923921. [Google Scholar] [CrossRef]
- Forte, G.; Favieri, F.; Tambelli, R.; Casagrande, M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int. J. Environ. Res. Public Health 2020, 17, 4151. [Google Scholar] [CrossRef]
- Sundarasen, S.; Chinna, K.; Kamaludin, K.; Nurunnabi, M.; Mohammad Baloch, G.; Khoshaimet, H.B.; Abid Hossain, S.F.; Sukayt, A. Psychological impact of COVID-19 and lockdown among university students in Malaysia: Implications and policy recommendations. Int. J. Environ. Res. Public Health 2020, 17, 6206. [Google Scholar] [CrossRef]
- Zhai, K.; Dilawar, A.; Yousef, M.S.; Holroyd, S.; El-Hammali, H.; Abdelmonem, M. Virtual Reality Therapy for Depression and Mood in Long-Term Care Facilities. Geriatrics 2021, 6, 58. [Google Scholar] [CrossRef]
- Valmaggia, L.R.; Latif, L.; Kempton, M.J.; Rus-Calafell, M. Virtual reality in the psychological treatment for mental health problems: An systematic review of recent evidence. Psychiatry Res. 2016, 236, 189–195. [Google Scholar] [CrossRef] [Green Version]
- Dellazizzo, L.; Potvin, S.; Luigi, M.; Dumais, A. Evidence on Virtual Reality-Based Therapies for Psychiatric Disorders: Meta-Review of Meta-Analyses. J. Med. Internet Res. 2020, 22, e20889. [Google Scholar] [CrossRef]
- Tashjian, V.C.; Mosadeghi, S.; Howard, A.R.; Lopez, M.; Dupuy, T.; Reid, M.; Martinez, B.; Ahmed, S.; Dailey, F.; Robbins, K.; et al. Virtual reality for management of pain in hospitalized patients: Results of a controlled trial. JMIR Ment. Health 2017, 4, e7387. [Google Scholar] [CrossRef]
- Bani Mohammad, E.; Ahmad, M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: A randomized control trial. Palliat. Support. Care 2019, 17, 29–34. [Google Scholar] [CrossRef]
- Pourmand, A.; Davis, S.; Marchak, A.; Whiteside, T.; Sikka, N. Virtual reality as a clinical tool for pain management. Curr. Pain Headache Rep. 2018, 15, 53. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Cohen, J.F.; Deeks, J.J.; Hooft, L.; Salameh, J.P.; Korevaar, D.A.; Gatsonis, C.; Hopewell, S.; Hunt, H.A.; Hyde, C.J.; Leeflang, M.M.; et al. Preferred reporting items for journal and conference abstracts of systematic reviews and meta-analyses of diagnostic test accuracy studies (PRISMA-DTA for Abstracts): Checklist, explanation, and elaboration. BMJ 2021, 372, n265. [Google Scholar] [CrossRef]
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 20 February 2022).
- Law, M.; Stewart, D.; Letts, L.; Pollock, N.; Bosch, J.; Westmorland, M. Guidelines for Critical Review of Qualitative Studies. 1998. Available online: https://medfac.tbzmed.ac.ir/Uploads/3/cms/user/File/10/Pezeshki_Ejtemaei/conferance/dav.pdf (accessed on 20 January 2022).
- Barratt, A.; Ragg, M.; Irwig, L.; Swinburne, L.; Chapman, S. How to Prepare and Present Evidence-Based Information for Consumers of Health Services: A Literature Review; National Medical Health and Medical Research Council: Canberra, Australia, 1999. Available online: https://www.nhmrc.gov.au/sites/default/files/2018-03/How-to-prepare-and-present-evidence-based-info-for-consumers-of-health-services.pdf (accessed on 20 February 2022).
- Waller, M.; Mistry, D.; Jetly, R.; Frewen, P. Meditating in Virtual Reality 3: 360° Video of Perceptual Presence of Instructor. Mindfulness 2021, 12, 1424–1437. [Google Scholar] [CrossRef]
- Siani, A.; Marley, S.A. Impact of the recreational use of virtual reality on physical and mental wellbeing during the COVID-19 lockdown. Health Technol. 2021, 11, 425–435. [Google Scholar] [CrossRef]
- Kolbe, L.; Jaywant, A.; Gupta, A.; Vanderlind, W.M.; Jabbour, G. Use of virtual reality in the inpatient rehabilitation of COVID-19 patients. Gen. Hosp. Psychiatry 2021, 71, 76–81. [Google Scholar] [CrossRef]
- Yang, T.; Lai, I.K.W.; Fan, Z.B.; Mo, Q.M. The impact of a 360° virtual tour on the reduction of psychological stress caused by COVID-19. Technol. Soc. 2021, 64, 101514. [Google Scholar] [CrossRef]
- Kim, D.; Ko, Y.J. The impact of virtual reality (VR) technology on sport spectators’ flow experience and satisfaction. Comput. Hum. Behav. 2019, 93, 346–356. [Google Scholar] [CrossRef]
- Kim, M.J.; Hall, C.M. A hedonic motivation model in virtual reality tourism: Comparing visitors and non-visitors. Int. J. Inf. Manag. 2019, 46, 236–249. [Google Scholar] [CrossRef]
- Kimiecik, J.C.; Harris, A.T. What is enjoyment? A conceptual/definitional analysis with implications for sport and exercise psychology. J. Sport Exerc. Psychol. 1996, 18, 247–263. [Google Scholar] [CrossRef]
- Dębska, M.; Polechoński, J.; Mynarski, A.; Polechoński, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef] [Green Version]
- Van Damme, K.; All, A.; De Marez, L.; Van Leuven, S. 360° Video journalism: Experimental study on the effect of immersion on news experience and distant suffering. J. Stud. 2019, 20, 2053–2076. [Google Scholar] [CrossRef]
- Alyan, E.; Combe, T.; Rambli, D.R.A.; Sulaiman, S.; Merienne, F.; Diyana, N. The Influence of Virtual Forest Walk on Physio-logical and Psychological Responses. Int. J. Environ. Res. Public Health 2021, 18, 11420. [Google Scholar] [CrossRef]
- Kefaliakos, A.; Pliakos, I.; Kiekkas, P.; Charalampidou, M.; Diomidous, M. Virtual reality in the rehabilitation of patients with neurological disorders. Stud. Health Technol. Inform. 2016, 226, 45–47. [Google Scholar]
- O’Neil, O.; Fernandez, M.M.; Herzog, J.; Beorchia, M.; Gower, V.; Gramatica, F.; Starrost, K.; Kiwull, L. Virtual reality for neurorehabilitation: Insights from 3 European clinics. PM&R 2018, 10, S198–S206. [Google Scholar] [CrossRef]
- Gupta, A.; Scott, K.; Dukewich, M. Innovative technology using virtual reality in the treatment of pain: Does it reduce pain via distraction, or is there more to it? Pain Med. 2018, 19, 151–159. [Google Scholar] [CrossRef] [Green Version]
- Zeidan, F.; Vago, D.R. Mindfulness meditation-based pain relief: A mechanistic account. Ann. N. Y. Acad. Sci. 2016, 1373, 114–127. [Google Scholar] [CrossRef]
- Zeidan, F.; Grant, J.A.; Brown, C.A.; McHaffie, J.G.; Coghill, R.C. Mindfulness meditation related pain relief: Evidence for unique brain mechanisms in the regulation of pain. Neurosci. Lett. 2012, 520, 165–173. [Google Scholar] [CrossRef] [Green Version]
- Hwang, N.K.; Shim, S.H. Use of Virtual Reality Technology to Support the Home Modification Process: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11096. [Google Scholar] [CrossRef]
- Alvarez-Lopez, F.; Maina, M.F.; Saigí-Rubió, F. Use of a Low-Cost Portable 3D Virtual Reality Gesture-Mediated Simulator for Training and Learning Basic Psychomotor Skills in Minimally Invasive Surgery: Development and Content Validity Study. J. Med. Internet Res. 2020, 22, e17491. [Google Scholar] [CrossRef]
- Hatta, M.H.; Sidi, H.; Sharip, S.; Das, S.; Saini, S.M. The Role of Virtual Reality as a Psychological Intervention for Mental Health Disturbances during the COVID-19 Pandemic: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 2390. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]

| Study by Authors | Type of Study | Sample Size | Age | Country | Setting | Inclusion Criteria | Exclusion Criteria | Intervention | Exposure Measurement Scale | Outcome Measurement | Comparator/ Control | Statistics (e.g., OR/RR, p-Value, 95% CI) | VR-Based Intervention (Outcome) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Waller 2021 [27] | RCT | 32 | 17–28 | Canada | Setting was not defined | Not defined | Respondents were not controlled. The respondents underwent evaluation for life events, childhood events, traumatic events, PTSD, and life experiences before commencing the study | The non-VR group was exposed to (1) conventional face-to-face (in vivo (IV) method), (2) pre-recorded 360° video viewed by a standard laptop computer monitor (2D format), and (3) pre-recorded 360° video viewed through an HMD (VR condition; 3D format) | A revised evaluation of the emotional questionnaire, Buddhist Affective States, Meditation Breath Attention Scores, and Meditative Experience Questionnaire | Encountering relaxation, less distractibility from the process of breathing, and being less fatigue | 3D (VR) vs. 2D format | Qualitative thematic analysis | ↑ When compared to the 2D format, VR meditations were associated with a more significant outcome |
| Siani 2021 [28] | Cross-sectional | 646 | 18–40 | UK-based with multiple countries’ participation | Online survey on researcher’s personal Facebook and Twitter, Facebook group (Virtual Reality Society, Oculus Virtual Reality), and Reddit channels | Not defined | Not defined | Mainly VR-video games play | N/A | Increased use of VR during quarantine, to study the impact on mental health, devices type, and fitness intensity | Control (waiting list) vs. Two-Group Random Assignment Pretest–Posttest Design | Majority were positive about the usefulness of VR for fitness (χ2 = 185.21,df = 4, p < 0.001) and mental health (χ2 = 416.27, df = 4, p < 0.001). The majority of both VR (48.4%) and console (42.1%) users engaged with moderate intensity. A greater proportion of VR users engage in vigorous activity (43.0%) than mild activity (8.6%), a trend which is reversed in console users (38.0% mild, 19.8% vigorous) | ↑ |
| Kolbe 2021 [29] | Cross-sectional | 24 (13 patients and 11 staff from COCID-19 Rehabilitation Unit (CRU), respectively | N/A | USA | COCID-19 Rehabilitation Unit (CRU) | (1) Hospitalized patients with +ve COVID-19 PCR test (2) Medical team deems the patient physically stable and has ongoing medical and rehabilitative needs (3) Able to tolerate >30+ min physical therapy (PT)/occupational therapy (OT) each daily (4) PT or OT recommendation for acute/subacute rehabilitation at the time of discharge (5) Anticipation of remaining in hospital/rehabilitation for ≥1 week | (1) Sexually not active, severe dementia and active delirium, or 1:1 sitter (2) must have non-invasive O2 needs of 6 L or fewer, or in case of tracheostomy patients have achieved “trach collaring” with anticipated ability to downsize/ decannulate | (1) Guided meditation, (2) exploration of natural environments, (3) cognitive stimulation game | A yes or no simple rating scale of 1–10 scores where 10 indicates the highest satisfaction and highest recommendation | Satisfaction, perceived enhancement | CRU inpatients and staff | For patients: 100% of patients answered “yes” to recommending the therapy to others, and 92.3% answered “yes” to the perceived enhancement of their treatment; For staff: 100% of staff answered “yes” to recommending the therapy to others, and 100% answered “yes” to perceived enhancement of their wellbeing | ↑ The use of VR led to significant decreases in participants’ psychological stress |
| Yang 2021 [30] | Cross-sectional | 235 | >18 | China | Local populace (in a shopping mall in Zhuhai City) | Not defined | Not defined | Validation of a theoretical model of the 360 degrees VR: A theoretical construct comprising the following factors: EN, IN, SA, SP, SR, TP are strongly related to each other and may help reduce stress from the COVID-19 pandemic | A newly designed questionnaire (translated and back-translated from English to Chinese) on the following features: (1) Introduction to the 360◦ virtual tours, and then the respondents were asked to watch a short video of the 360° virtual tours; (2) Measurement on the stress reduction of the research model; (3) Recorded the respondents’ demographic characteristics such as gender, age, marital status, education, income, occupation, and so on; (4) Measuring stress reduction as a result of using the 360° virtual tours | Enjoyment (EN) Involvement (IN) Satisfaction (SA) Sense of presence (SA) Stress Reduction (SR) Telepresence (TP) factors | No control group defined | PLS-SEM: The sense of presence (SP) and their level of enjoyment (EN) (β = 0.221, t-statistics (t) = 2.256), (SP) with involvement (IN) (β = 0.250, t-statistics = 3.224), SA and SP (β = 0.289, t = 4.099) TP to EN (β = 0.528, t = 5.411) TP to IN(β = 0.466, t = 6.028), TP to SA (β = 0.235, t = 3.246), path coefficients: EN to SA to stress reduction of COVID 0.268 (t = 4.345) and 0.474 (t = 5.904), respectively. 0.164 IN to stress reduction of COVID-19 (t = 2.626) and 0.158 (t = 2.093), SA to stress reduction from COVID-19, respectively: 0.196 (t = 3.116) | ↑ Satisfaction with the 360° virtual tour experience and stress reduction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hatta, M.H.; Sidi, H.; Siew Koon, C.; Che Roos, N.A.; Sharip, S.; Abdul Samad, F.D.; Wan Xi, O.; Das, S.; Mohamed Saini, S. Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5389. https://doi.org/10.3390/ijerph19095389
Hatta MH, Sidi H, Siew Koon C, Che Roos NA, Sharip S, Abdul Samad FD, Wan Xi O, Das S, Mohamed Saini S. Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(9):5389. https://doi.org/10.3390/ijerph19095389
Chicago/Turabian StyleHatta, Muhammad Hizri, Hatta Sidi, Chong Siew Koon, Nur Aishah Che Roos, Shalisah Sharip, Farah Deena Abdul Samad, Ong Wan Xi, Srijit Das, and Suriati Mohamed Saini. 2022. "Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 9: 5389. https://doi.org/10.3390/ijerph19095389
APA StyleHatta, M. H., Sidi, H., Siew Koon, C., Che Roos, N. A., Sharip, S., Abdul Samad, F. D., Wan Xi, O., Das, S., & Mohamed Saini, S. (2022). Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review. International Journal of Environmental Research and Public Health, 19(9), 5389. https://doi.org/10.3390/ijerph19095389







