Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning
Abstract
1. Introduction
2. Methods
2.1. MARS
2.2. CART
2.3. RF
2.4. XGBoost
2.5. Model Implementation
3. Empirical Study
3.1. Dataset and Performance Criteria
3.2. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fang, Y.T.; Chou, Y.J.; Pu, C.; Lin, P.J.; Liu, T.L.; Huang, N.; Chou, P. Prescription of atropine eye drops among children diagnosed with myopia in Taiwan from 2000 to 2007: A nationwide study. Eye 2013, 27, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.C.; Huang, H.M.; Yu, H.J. Epidemiology of Myopia. Asia Pac. J. Ophthalmol. 2016, 5, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Michalski, A.; Rogaczewska, M.; Maleszka-Kurpiel, M.; Stopa, M. Pharmacological Myopia Control Influence on Quality of Life and Psyche among Adolescents. J. Clin. Med. 2020, 9, 3920. [Google Scholar] [CrossRef]
- Health Promotion Administration, Ministry of Health and Welfare for the Taiwan. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=45 (accessed on 29 June 2020).
- Upadhyay, A.; Beuerman, R.W. Biological Mechanisms of Atropine Control of Myopia. Eye Contact Lens 2020, 46, 129–135. [Google Scholar] [CrossRef]
- Chia, A.; Chua, W.H.; Cheung, Y.B.; Wong, W.L.; Lingham, A.; Fong, A.; Tan, D. Atropine for the treatment of childhood myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 2012, 119, 347–354. [Google Scholar] [CrossRef]
- Chia, A.; Lu, Q.S.; Tan, D. Five-year clinical trial on atropine for the treatment of myopia 2: Myopia control with atropine 0.01% eyedrops. Ophthalmology 2016, 123, 391–399. [Google Scholar] [CrossRef]
- Gong, Q.; Janowski, M.; Luo, M.; Wei, H.; Chen, B.; Yang, G.; Liu, L. Efficacy and adverse effects of atropine in childhood myopia: A meta-analysis. JAMA Ophthalmol. 2017, 135, 624–630. [Google Scholar] [CrossRef]
- Pineles, S.L.; Kraker, R.T.; VanderVeen, D.K.; Hutchinson, A.K.; Galvin, J.A.; Wilson, L.B.; Lambert, S.R. Atropine for the prevention of myopia progression in children: A report by the American Academy of Ophthalmology. Ophthalmology 2017, 124, 1857–1866. [Google Scholar] [CrossRef]
- Wu, P.C.; Chuang, M.N.; Choi, J.; Chen, H.; Wu, G.; Ohno-Matsui, K. Update in myopia and treatment strategy of atropine use in myopia control. Eye 2019, 33, 3–13. [Google Scholar] [CrossRef]
- McCrann, S.; Flitcroft, I.; Strang, N.C.; Saunders, K.J.; Logan, N.S.; Lee, S.S. Myopia Outcome Study of Atropine in Children (MOSAIC): An investigator-led, double-masked, placebo-controlled, randomised clinical trial protocol. HRB Open Res. 2019, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Sacchi, M.; Serafino, M.; Villani, E.; Tagliabue, E.; Luccarelli, S.; Bonsignore, F.; Nucci, P. Efficacy of atropine 0.01% for the treatment of childhood myopia in European patients. Acta Ophthalmol. 2019, 97, 1136–1140. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.Y.; Mackey, D.A.; Lingham, G.; Crewe, J.M.; Richards, M.D.; Chen, F.K. Western Australia Atropine for the Treatment of Myopia (WA-ATOM) study: Rationale, methodology and participant baseline characteristics. Clin. Exp. Ophthalmol. 2020, 48, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Fan, L.; Tao, J.; Hua, R.; Yang, Q.; Gu, H. Use of Topical 0.01% Atropine for Controlling Near Work-Induced Transient Myopia: A Randomized, Double-Masked, Placebo-Controlled Study. J. Ocul. Pharmacol. Ther. 2020, 36, 97–101. [Google Scholar] [CrossRef]
- Zhu, Q.; Tang, Y.; Guo, L.; Tighe, S.; Zhou, Y.; Zhang, X. Efficacy and Safety of 1% Atropine on Retardation of Moderate Myopia Progression in Chinese School Children. Int. J. Med. Sci. 2020, 17, 176–181. [Google Scholar] [CrossRef]
- Yam, J.C.; Jiang, Y.; Tang, S.M.; Law, A.K.; Chan, J.J.; Wong, E. Low-concentration atropine for myopia progression (LAMP) study: A randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology 2019, 126, 113–124. [Google Scholar] [CrossRef]
- Yam, J.C.; Li, F.F.; Zhang, X.; Tang, S.M.; Yip, B.H.; Kam, K.W. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: Phase 2 report. Ophthalmology 2020, 127, 910–919. [Google Scholar] [CrossRef]
- Kim, J.; Lim, D.H.; Han, S.H.; Chung, T.Y. Predictive factors associated with axial length growth and myopia progression in orthokeratology. PLoS ONE 2019, 14, e0218140. [Google Scholar] [CrossRef]
- Lee, Y.C.; Wang, J.H.; Chiu, C.J. Effect of Orthokeratology on myopia progression: Twelve-year results of a retrospective cohort study. BMC Ophthalmol. 2017, 17, 243. [Google Scholar] [CrossRef]
- Anstice, N.S.; Phillips, J.R. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 2011, 118, 1152–1161. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Holden, B.; Smith, E., 3rd; Naduvilath, T.; Chen, X.; de la Jara, P.L.; Martinez, A. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: One-year results. Investig. Ophthalmol. Visual Sci. 2011, 52, 9362–9367. [Google Scholar] [CrossRef] [PubMed]
- Gong, C.R.; Troilo, D.; Richdale, K. Accommodation and phoria in children wearing multifocal contact lenses. Optom. Vision Sci. 2017, 94, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Walline, J.J.; Greiner, K.L.; McVey, M.E.; Jones-Jordan, L.A. Multifocal contact lens myopia control. Optom. Vision Sci. 2013, 90, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Przekoracka, K.; Michalak, K.; Olszewski, J.; Zeri, F.; Michalski, A.; Paluch, J.; Przekoracka-Krawczyk, A. Contrast sensitivity and visual acuity in subjects wearing multifocal contact lenses with high additions designed for myopia progression control. Contact Lens Anter. Eye 2020, 43, 33–39. [Google Scholar] [CrossRef]
- Kropacz-Sobkowiak, S.; Przekoracka-Krawczyk, A.; Michalak, K.; Michalski, A.; Kujawa, K.; Olszewski, J. The influence of high addition soft multifocal contact lenses on visual performance. Klin. Oczna Acta Ophthalmol. Pol. 2020, 122, 92–99. [Google Scholar] [CrossRef]
- Wagner, R.S. Treatment of progressive myopia in the pediatric population. J. Pediatr. Ophthalmol. Strabismus 2019, 56, 72. [Google Scholar] [CrossRef]
- Saw, S.M.; Matsumura, S.; Hoang, Q.V. Prevention and management of myopia and myopic pathology. Investig. Ophthalmol. Visual Sci. 2019, 60, 488–499. [Google Scholar] [CrossRef]
- Wu, T.E.J.; Yang, C.C.; Chen, H.S. Does atropine use increase intraocular pressure in myopic children? Optom. Vision Sci. 2012, 89, E161–E167. [Google Scholar] [CrossRef]
- Ho, M.C.; Hsieh, Y.T.; Shen, E.P.; Hsu, W.C.; Cheng, H.C. Short-term refractive and ocular parameter changes after topical atropine. Taiwan J. Ophthalmol. 2020, 10, 111–115. [Google Scholar]
- Rengstorff, R.H.; Doughty, C.B. Mydriatic and cycloplegic drugs: A review of ocular and systemic complications. Am. J. Optom. Physiol. Opt. 1982, 59, 162–177. [Google Scholar] [CrossRef]
- Lee, C.Y.; Sun, C.C.; Lin, Y.F.; Lin, K.K. Effects of topical atropine on intraocular pressure and myopia progression: A prospective comparative study. BMC Ophthalmol. 2016, 16, 114. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-González, J.M.; De-Hita-Cantalejo, C.; Baustita-Llamas, M.J.; Sánchez-González, M.C.; Capote-Puente, R. The Combined Effect of Low-dose Atropine with Orthokeratology in Pediatric Myopia Control: Review of the Current Treatment Status for Myopia. J. Clin. Med. 2020, 9, 2371. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.Z.; Syn, N.; Li, S.; Barathi, V.A.; Tong, L.; Neo, J. The penetration and distribution of topical atropine in animal ocular tissues. Acta Ophthalmol. 2019, 97, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Vutipongsatorn, K.; Yokoi, T.; Ohno-Matsui, K. Current and emerging pharmaceutical interventions for myopia. Br. J. Ophthalmol. 2019, 103, 1539–1548. [Google Scholar] [CrossRef]
- Chan, L.W.; Hsieh, Y.T.; Hsu, W.C.; Cheng, H.C.; Shen, E.P. Optic Disc Parameters of Myopic Children with Atropine Treatment. Curr. Eye Res. 2017, 42, 1614–1619. [Google Scholar] [CrossRef]
- Weng, J.; Tsai, I.L.; Kuo, L.L.; Tsai, C.Y.; Woung, L.C.; Hsiao, Y.C. Intraocular pressure monitoring by rebound tonometry in children with myopia. Taiwan J. Ophthalmol. 2017, 7, 149–154. [Google Scholar]
- Friedman, J.H. Multivariate adaptive regression splines. Ann. Stat. 1991, 19, 1–67. [Google Scholar] [CrossRef]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees; Wadsworth, Champman &Hall/CRC: New York, NY, USA, 1984. [Google Scholar]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Probst, P.; Wright, M.N.; Boulesteix, A.L. Hyperparameters and tuning strategies for random forest. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 2019, 9, e1301. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016. [Google Scholar]
- Milborrow, S.; Hastie, T.; Tibshirani, R. Earth: Multivariate Adaptive Regression Splines. R Package Version 5.1.2. Available online: https://www.rdocumentation.org/packages/earth (accessed on 1 August 2020).
- Therneau, T.; Atkinson, B.; Ripley, B. Rpart: Recursive Partitioning and Regression Trees. R Package Version, 4.1-15. Available online: https://www.rdocumentation.org/packages/rpart/versions/4.1-15 (accessed on 1 August 2020).
- Liaw, A.; Wiener, M. RandomForest: Breiman and Cutler’s Random Forests for Classification and Regression. R Package Version, 4.6.14. Available online: https://www.rdocumentation.org/packages/randomForest (accessed on 1 August 2020).
- Chen, T.; He, T.; Benesty, M. XGboost: Extreme Gradient Boosting. R Package Version 0.90.0.2. Available online: https://www.rdocumentation.org/packages/XGboost (accessed on 1 August 2020).
- Yan, Y. MLmetrics: Machine Learning Evaluation Metrics. R Package Version, 1.1.1. Available online: https://www.rdocumentation.org/packages/MLmetrics/versions/1.1.1 (accessed on 1 August 2020).
- Hamner, B.; Frasco, M.; LeDell, E. Metrics: Evaluation Metrics for Machine Learning. R Package Version 0.1.4. Available online: https://www.rdocumentation.org/packages/Metrics/versions/0.1.4 (accessed on 1 August 2020).
- Kuhn, M.; Wing, J.; Weston, S.; Williams, A.; Keefer, C.; Engelhardt, A.; Kenkel, B. Caret: Classification and Regression Training. R Package Version 6.0-84. Available online: https://www.rdocumentation.org/packages/caret (accessed on 1 August 2020).
- Sihota, R.; Tuli, D.; Dada, T.; Gupta, V.; Sachdeva, M.M. Distribution and determinants of intraocular pressure in a normal pediatric population. J. Pediatr. Ophthalmol. Strabismus. 2006, 43, 14–18. [Google Scholar] [CrossRef]
- Lomoriello, D.S.; Lombardo, M.; Tranchina, L.; Oddone, F.; Serrao, S.; Ducoli, P. Repeatability of intra-ocular pressure and central corneal thickness measurements provided by a non-contact method of tonometry and pachymetry. Graefe Arch. Clin. Exp. Ophthalmol. 2011, 249, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Camburu, G.; Zemba, M.; Purcărea, V.L. Is Central Corneal Thickness a reliable independent factor in decision-making regarding the management of patients with high IOP? Rom. J. Ophthalmol. 2020, 64, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.G.; Kim, J.H.; Kim, N.R.; Kim, C.Y.; Lee, E.S. Comparison between Tonopachy and other tonometric and pachymetric devices. Optom. Vision Sci. 2011, 88, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.C.; Wu, T.E.; Wang, Y.S.; Cheng, S.F.; Liou, S.W. A STROBE-compliant case–control study: Effects of cumulative doses of topical atropine on intraocular pressure and myopia progression. Medicine 2020, 99, e22745. [Google Scholar] [CrossRef]

| Metrics | Description | Calculation * |
|---|---|---|
| MAPE | Mean Absolute Percentage Error | |
| SMAPE | Symmetric Mean Absolute Percentage Error | |
| RAE | Relative Absolute Error | |
| RRSE | Root Relative Squared Error | |
| RMSE | Root Mean Squared Error |
| Variables | Description | Unit | |
|---|---|---|---|
| X1: | Sex | Male/Female | - |
| X2: | Age | Age in years | - |
| X3: | Base IOP | Baseline intraocular pressure measured | mm-Hg |
| X4: | Base Spherical | Baseline myopic power | Diopter (D) |
| X5: | Base SE | Baseline spherical equivalent | Diopter (D) |
| X6 | End Spherical | Endpoint myopic power | Diopter (D) |
| X7 | End SE | Endpoint spherical equivalent | Diopter (D) |
| X8 | Total Duration | Total duration from first to last visit | month |
| X9 | Total Cumulative Dosage | Total cumulative dosage of topical atropine | mg |
| X10 | Total Average Dosage per month | Average dosage per month from the first visit to the last visit | mg/month |
| X11 | Total Prescribed Bottles | Number of prescription bottles of atropine | bottles |
| X12 | Previous Duration | The duration from the first visit to the recruitment date | month |
| X13 | Previous Cumulative Dosage | Cumulative dosage of topical atropine from the first visit to the recruitment date | mg |
| X14 | Previous Average Dosage Per Month | Average dosage per month from the first visit to the recruitment date | mg/month |
| X15 | Recruit Duration | The duration from the recruitment date to the last visit | month |
| X16 | Recruit Cumulative Dosage | Cumulative dosage of topical atropine from the recruitment date to the last visit | mg |
| X17 | Recruit Average Dosage Per Month | Average dosage per month from the recruitment date to the last visit | mg/month |
| X18 | Last Dosage | The prescribed dosage of atropine on the last visit | mg |
| X19 | Last Frequency | The prescribed frequency of atropine on the last visit | - |
| Y | End IOP | Endpoint intraocular pressure measured | mm-Hg |
| Characteristics | Mean ± SD | |
|---|---|---|
| X2 | Age | 10.53 ± 2.54 |
| X3 | Base IOP (mm-Hg) | 14.51 ± 2.69 |
| X4 | Base Spherical (Diopter (D) | −1.95 ± 1.45 |
| X5 | Base SE (Diopter (D) | −2.48 ± 1.57 |
| X6 | End Spherical (Diopter (D) | −2.39 ± 1.68 |
| X7 | End SE (Diopter (D) | −2.94 ± 1.86 |
| X8 | Total Duration (month) | 20.02 ± 12.01 |
| X11 | Total Prescribed Bottles | 6.47 ± 5.54 |
| X12 | Previous Duration (mg) | 14.07 ± 12.14 |
| X15 | Recruit Duration (month) | 5.96 ± 3.83 |
| Y | End IOP (mm-Hg) | 15.08 ± 2.86 |
| Median (IQR) | ||
| X9 | Total Cumulative Dosage (mg) | 75.00 (37.5–150) |
| X10 | Total Average Dosage per Month (mg/month) | 4.35 (2.66–7.87) |
| X13 | Previous Cumulative Dosage (mg) | 45.00 (25–87.5) |
| X14 | Previous Average Dosage Per Month (mg/month) | 6.42 (2.34–15.99) |
| X16 | Recruit Cumulative Dosage (mg) | 12.50 (0–55) |
| X17 | Recruit Average Dosage Per Month (mg/month) | 2.35 (0–11.93) |
| X1 | Sex | n (%) |
| Male | 813 (52.6%) | |
| Female | 732 (47.4%) | |
| X18 | Last Dosage (mg) | n (%) |
| 0 | 4 (0.3%) | |
| 5 | 619 (40.1%) | |
| 12.5 | 718 (46.5%) | |
| 25 | 146 (9.4%) | |
| 50 | 58 (3.8%) | |
| X19 | Last Frequency | n (%) |
| QN | 1191 (77.1%) | |
| QON | 238 (15.4%) | |
| BIW | 80 (5.2%) | |
| QW | 32 (2.1%) | |
| 0 | 4 (0.3%) |
| Methods | MAPE | SMAPE | RAE | RRSE | RMSE |
|---|---|---|---|---|---|
| LR | 0.1266 | 0.1226 | 0.8235 | 0.8458 | 2.3283 |
| MARS | 0.1259 | 0.1219 | 0.8228 | 0.8409 | 2.3149 |
| CART | 0.1341 | 0.1298 | 0.8666 | 0.8835 | 2.4323 |
| RF | 0.1271 | 0.1229 | 0.8222 | 0.8331 | 2.2934 |
| XGBoost | 0.1182 | 0.1155 | 0.7783 | 0.8211 | 2.2604 |
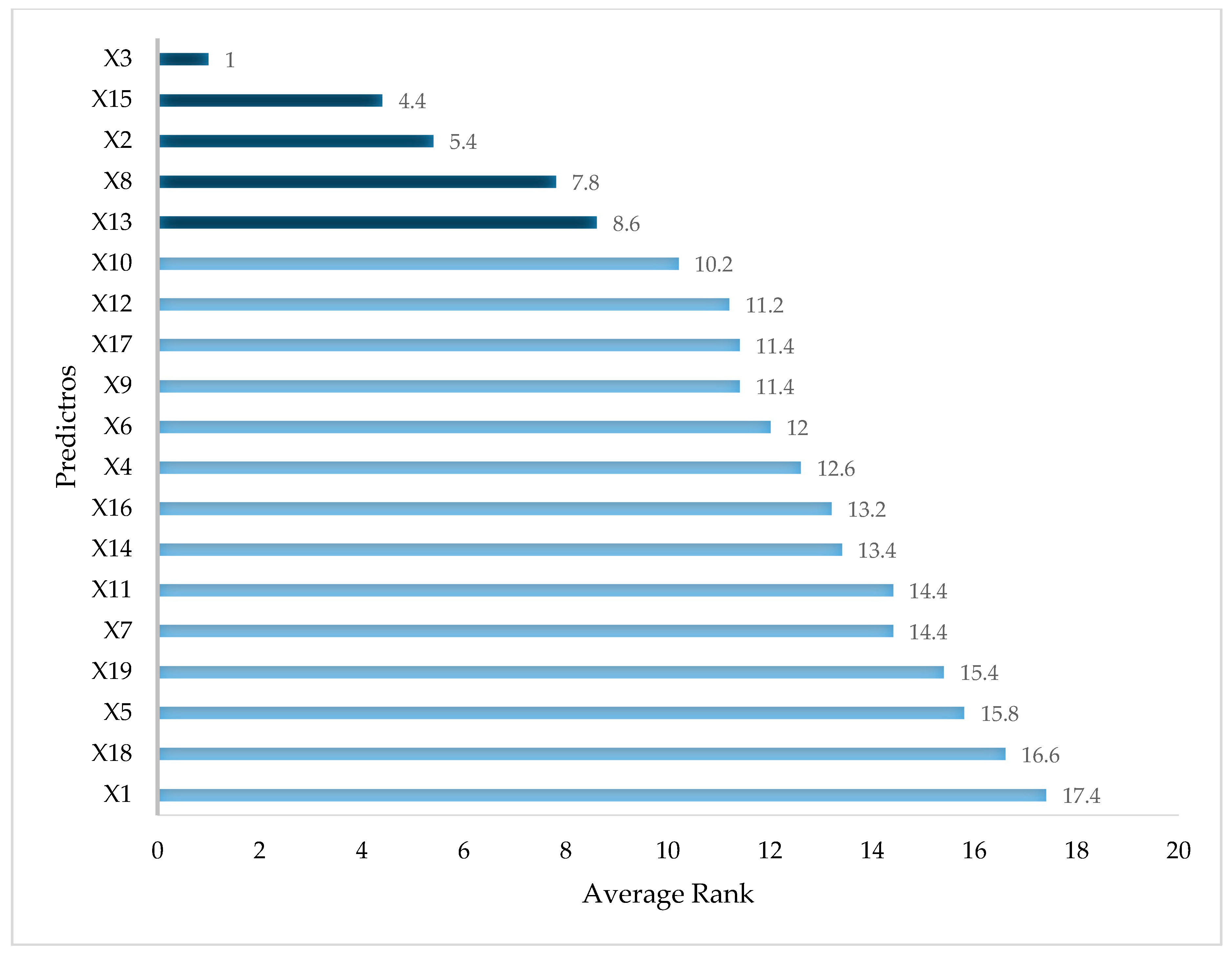
| Predictors | LR | MARS | CART | RF | XGBoost | Average Rank |
|---|---|---|---|---|---|---|
| X1 Sex | 11 | 19 | 19 | 19 | 19 | 17.4 |
| X2 Age | 16 | 4 | 2 | 3 | 2 | 5.4 |
| X3 Base IOP | 1 | 1 | 1 | 1 | 1 | 1 |
| X4 Base Spherical | 12 | 5 | 19 | 14 | 13 | 12.6 |
| X5 Base SE | 14 | 19 | 19 | 13 | 14 | 15.8 |
| X6 End Spherical | 8 | 5 | 19 | 11 | 17 | 12 |
| X7 End SE | 13 | 19 | 19 | 12 | 9 | 14.4 |
| X8 Total Duration | 5 | 19 | 5 | 4 | 6 | 7.8 |
| X9 Total Cumulative Dosage | 2 | 19 | 19 | 6 | 11 | 11.4 |
| X10 Total Average Dosage per month | 15 | 19 | 4 | 8 | 5 | 10.2 |
| X11 Total Prescribed Bottles | 9 | 19 | 19 | 10 | 15 | 14.4 |
| X12 Previous Duration | 5 | 19 | 19 | 5 | 8 | 11.2 |
| X13 Previous Cumulative Dosage | 3 | 19 | 7 | 2 | 12 | 8.6 |
| X14 Previous Average Dosage Per Month | 19 | 19 | 19 | 7 | 3 | 13.4 |
| X15 Recruit Duration | 4 | 2 | 3 | 9 | 4 | 4.4 |
| X16 Recruit Cumulative Dosage | 19 | 3 | 19 | 15 | 10 | 13.2 |
| X17 Recruit Average Dosage Per Month | 7 | 19 | 6 | 18 | 7 | 11.4 |
| X18 Last Dosage | 10 | 19 | 19 | 17 | 18 | 16.6 |
| X19 Last Frequency | 19 | 7 | 19 | 16 | 16 | 15.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, T.-E.; Chen, H.-A.; Jhou, M.-J.; Chen, Y.-N.; Chang, T.-J.; Lu, C.-J. Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning. J. Clin. Med. 2021, 10, 111. https://doi.org/10.3390/jcm10010111
Wu T-E, Chen H-A, Jhou M-J, Chen Y-N, Chang T-J, Lu C-J. Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning. Journal of Clinical Medicine. 2021; 10(1):111. https://doi.org/10.3390/jcm10010111
Chicago/Turabian StyleWu, Tzu-En, Hsin-An Chen, Mao-Jhen Jhou, Yen-Ning Chen, Ting-Jen Chang, and Chi-Jie Lu. 2021. "Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning" Journal of Clinical Medicine 10, no. 1: 111. https://doi.org/10.3390/jcm10010111
APA StyleWu, T.-E., Chen, H.-A., Jhou, M.-J., Chen, Y.-N., Chang, T.-J., & Lu, C.-J. (2021). Evaluating the Effect of Topical Atropine Use for Myopia Control on Intraocular Pressure by Using Machine Learning. Journal of Clinical Medicine, 10(1), 111. https://doi.org/10.3390/jcm10010111







