Development of a Complex Intervention for Effective Management of Type 2 Diabetes in a Developing Country
Abstract
:1. Introduction
2. Materials and Methods
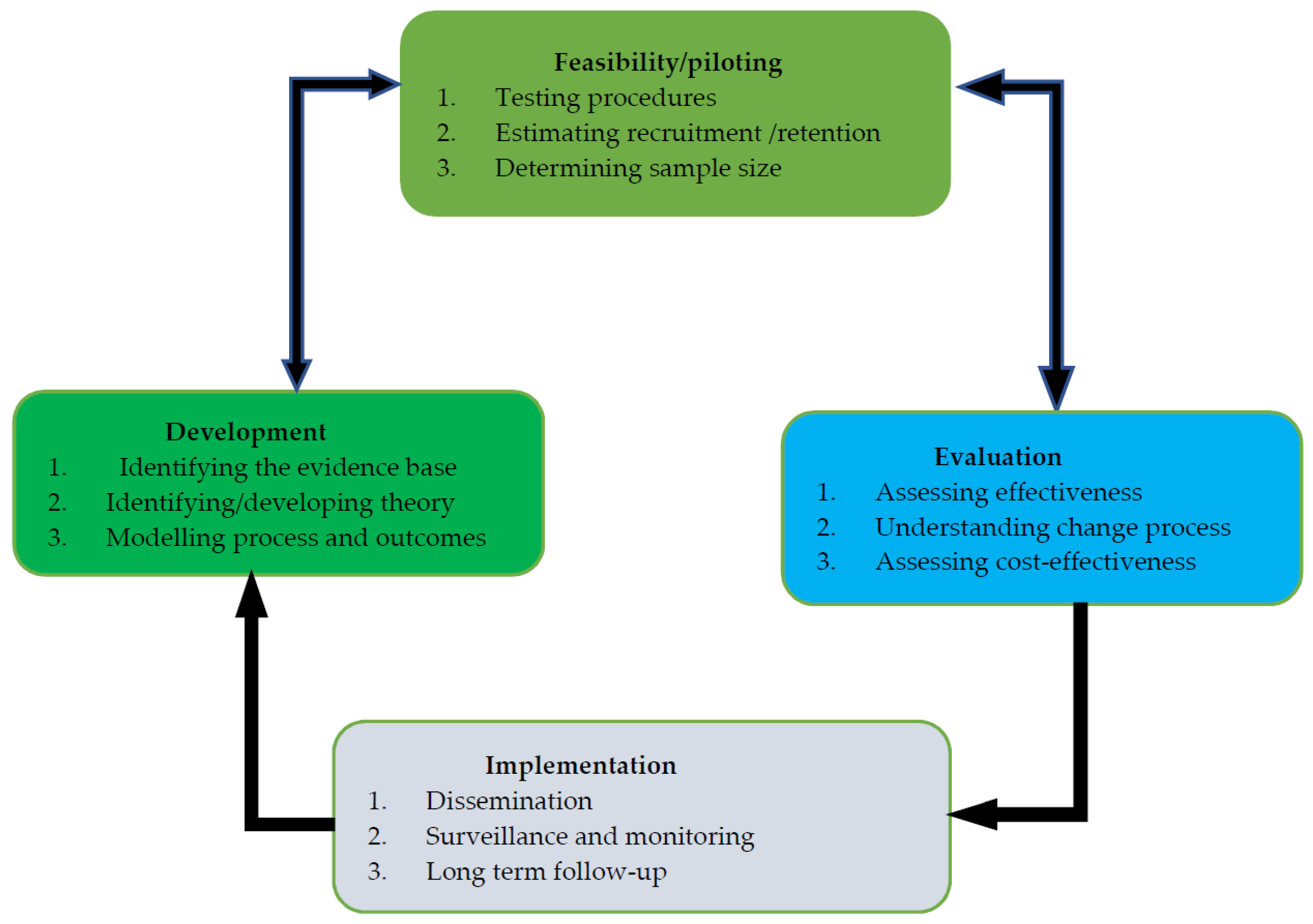
2.1. Developing a Complex Intervention
2.2. Identifying the Evidence Base
2.3. Identifying and Developing Theory
2.3.1. Workshop I
2.3.2. Workshop II
2.3.3. Workshop III
- Who needs to perform the behaviour?
- What do they need to do differently to achieve the desired change?
- When do they need to do it?
- Where do they need to do it?
- How often do they need to do it?
- With whom do they need to do it?
Stage One
Stage Two
- Decide what ‘intervention functions’ to apply: education, persuasion, incentivisation, coercion, training, restriction, environmental restructuring, modelling, and enablement;
- Select implementation strategy: fiscal policy, legislation, regulation, environmental planning, communications, service provision, and guidelines development.
Stage Three
- Create the detailed intervention specification covering all aspects of content and delivery of the intervention structured around the chosen BCTs and modes of delivery.
2.4. Modelling and Creating a Complex Intervention
3. Results
3.1. Study Participants
3.2. Step One: Define the Health Problem in Behavioural Terms
3.3. Step Two: Select the Target Behaviour
- Lack of resources, such as medications, laboratory, and diagnostic tests;
- Lack of continuity of care, such as prolonged follow up clinic visits;
- Lack of knowledge and awareness of patients about type 2 diabetes and its complications;
- Lack of self-care activities;
- Low level of type 2 diabetes education and counselling services;
- Low competence and experience of health professionals providing diabetes care;
- Inefficient collaboration among health professionals (nurses, physicians, and pharmacists) in the care of type 2 diabetes;
- Absence of involvement of clinical pharmacists, dietitians or nutritionists, and psychologists in the care of type 2 diabetes.
- Provide structured diabetes education and counselling with competent health professionals;
- Enable collaborative care of type 2 diabetes;
- Involve clinical pharmacists, dietitians or nutritionists, and psychologists in the care of type 2 diabetes as members of the collaborative care team;
- Improve health professionals’ competency, commitment, and professional ethics through trainings.
- Ensure continuous availability of medications;
- Ensure continuous availability of laboratory and diagnostic tests;
- Involve clinical pharmacists, dietitians or nutritionists, and psychologists in the care of type 2 diabetes as members of the collaborative care team;
- Enable collaborative care of type 2 diabetes;
- Integrate all type 2 diabetes care services at the diabetes centre.
3.4. Step Three: Specify the Target Behaviour
3.5. Step Four: Identify What Needs to Change
3.5.1. Structured Type 2 Diabetes Education and Counselling
3.5.2. Collaborative Care
3.6. Step Five: Identify Intervention Functions
3.6.1. Intervention Functions for the COM-B Components of the Target Behaviour Provision of Structured Diabetes Education and Counselling
3.6.2. Intervention Functions for the COM-B Components of The Target Behaviour in Collaborative Care of Type 2 Diabetes
3.7. Step Six: Identifying Policy Categories for the Target Behaviours’ Provision of Structured Diabetes Education, Counselling, and Collaborative Care of Type 2 Diabetes
3.8. Step Seven: Identifying Behaviour Change Techniques
- Feedback on behaviour;
- Self-monitoring of behaviour;
- Prompt/cues;
- Salience of consequences;
- Instruction on how to perform the behaviour;
- Demonstration of the behaviour;
- Restructuring the physical environment;
- Restructuring the social environment;
- Adding objects to the environment;
- Goal setting behaviour;
- Action planning;
- Social support (unspecified).
3.9. Step Eight: Mode of Delivery and Development of the Complex Intervention
- Self-monitoring of behaviour;
- Prompt/cues;
- Feedback on behaviour;
- Instruction on how to perform the behaviour;
- Restructuring the physical environment;
- Restructuring the social environment;
- Adding objects to the environment;
- Demonstration of the behaviour;
- Goal setting behaviour;
- Action planning;
- Social support (unspecified);
- Social support (practical);
- Problem solving.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, F.B. Globalisation of diabetes: The role of diet, lifestyle, and genes. Diabetes Care 2011, 34, 1249–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bloomgarden, Z.T. Cardiovascular disease in diabetes. Diabetes Care 2008, 31, 1260–1266. [Google Scholar] [CrossRef] [Green Version]
- International Diabetes Federation. International Diabetes Federation Diabetes Atlas, 8th ed.; International Diabetes Federation: Brussels, Belgium, 2017. [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas, 9th ed.; International Diabetes Federation: Brussels, Belgium, 2019. [Google Scholar]
- Kim, S. Burden of shospitalisations primarily due to uncontrolled diabetes: Implications of inadequate primary health care in the United States. Diabetes Care 2007, 30, 1281–1282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cramer, J.A.; Benedict, Á.; Muszbek, N.; Keskinaslan, A.; Khan, Z.M. The significance of compliance and persistence in the treatment of diabetes, hypertension and dyslipidaemia: A review. Int. J. Clin. Pr. 2007, 62, 76–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Inzucchi, S.E.; Bergenstal, R.M.; Buse, J.; Diamant, M.; Ferrannini, E.; Nauck, M.; Peters, A.; Tsapas, A.; Wender, R.; Matthews, D.R. Management of hyperglycaemia in type 2 diabetes: A patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2012, 55, 1577–1596. [Google Scholar] [CrossRef]
- Azevedo, M.; Alla, S. Diabetes in Sub-Saharan Africa: Kenya, Mali, Mozambique, Nigeria, South Africa and Zambia. Int. J. Diabetes Dev. Ctries. 2008, 28, 101–108. [Google Scholar] [CrossRef] [Green Version]
- Gill, G.V.; Mbanya, J.-C.; Ramaiya, K.L.; Tesfaye, S. A sub-Saharan African perspective of diabetes. Diabetologia 2009, 52, 8–16. [Google Scholar] [CrossRef] [Green Version]
- Pastakia, S.D.; Pekny, C.R.; Manyara, S.M.; Fischer, L. Diabetes in sub-Saharan Africa—From policy to practice to progress: Targeting the existing gaps for future care for diabetes. Diabetes Metab. Syndr. Obes. 2017, 10, 247–263. [Google Scholar] [CrossRef] [Green Version]
- Shimels, T.; Abebaw, M.; Bilal, A.I.; Tesfaye, T. Treatment Pattern and Factors Associated with Blood Pressure and Fasting Plasma Glucose Control among Patients with Type 2 Diabetes Mellitus in Police Referral Hospital in Ethiopia. Ethiop. J. Health Sci. 2018, 28, 461–472. [Google Scholar] [CrossRef]
- Gudina, E.K.; Amade, S.T.; Tesfamichael, F.A.; Ram, R. Assessment of quality of care given to diabetic patients at Jimma University Specialized Hospital diabetes follow-up clinic, Jimma, Ethiopia. BMC Endocr. Disord. 2011, 11, 19. [Google Scholar] [CrossRef] [Green Version]
- Yigazu, D.M.; Desse, T.A. Glycemic control and associated factors among type 2 diabetic patients at Shanan Gibe Hospital, Southwest Ethiopia. BMC Res. Notes 2017, 10, 597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atun, R.; Davies, J.I.; Gale, E.A.M.; Bärnighausen, T.; Beran, D.; Kengne, A.P.; Levitt, N.; Mangugu, F.W.; Nyirenda, M.J.; Ogle, G.D.; et al. Diabetes in sub-Saharan Africa: From clinical care to health policy. Lancet Diabetes Endocrinol. 2017, 5, 622–667. [Google Scholar] [CrossRef] [Green Version]
- Mobula, L.M.; Sarfo, F.S.; Carson, K.A.; Burnham, G.; Arthur, L.; Ansong, D.; Sarfo-Kantanka, O.; Plange-Rhule, J.; Ofori-Adjei, D. Predictors of glycemic control in type-2 diabetes mellitus: Evidence from a multicenter study in Ghana. Transl. Metab. Syndr. Res. 2018, 1, 1–8. [Google Scholar] [CrossRef]
- Nuche-Berenguer, B.; Kupfer, L.E. Readiness of Sub-Saharan Africa Healthcare Systems for the New Pandemic, Diabetes: A Systematic Review. J. Diabetes Res. 2018, 2018, 9262395. [Google Scholar] [CrossRef] [Green Version]
- Bhagavathula, A.S.; Gebreyohannes, E.A.; Abegaz, T.M.; Abebe, T.B. Perceived Obstacles Faced by Diabetes Patients Attending University of Gondar Hospital, Northwest Ethiopia. Front. Public Health 2018, 6, 81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nigatu, T. Epidemiology, complications and management of diabetes in Ethiopia: A systematic review. J. Diabetes 2012, 4, 174–180. [Google Scholar] [CrossRef]
- Yimama, M.; Jarso, H.; Desse, T.A. Determinants of drug-related problems among ambulatory type 2 diabetes patients with hypertension comorbidity in Southwest Ethiopia: A prospective cross sectional study. BMC Res. Notes 2018, 11, 679. [Google Scholar] [CrossRef]
- Kiflie, Y.; Jira, C.; Nigussie, D. The quality of care provided to patients with chronic non-communicable diseases: A Retrospective multi-set up study in Jimma Zone, southwest Ethiopia. Ethiop. J. Health Sci. 2011, 21, 119–130. [Google Scholar] [CrossRef]
- Bekele, A.; Getachew, T.; Amenu, K.; Defar, A.; Teklie, H.; Gelibo, T.; Taddesse, M.; Assefa, Y.; Kebede, A.; Feleke, Y. Service availability and readiness for diabetes care at health facilities in Ethiopia. Ethiop. J. Health Dev. 2017, 31, 110–118. [Google Scholar]
- Habte, B.M.; Kebede, T.; Fenta, T.G.; Boon, H. Ethiopian patients’ perceptions of anti-diabetic medications: Implications for diabetes education. J. Pharm. Policy Pr. 2017, 10, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, M.; Alemu, T.; Sada, O. Medication adherence and its associated factors among diabetic patients at Zewditu Memorial Hospital, Addis Ababa, Ethiopia. BMC Res. Notes 2017, 10, 676. [Google Scholar] [CrossRef]
- Esterson, Y.B.; Carey, M.; Piette, J.D.; Thomas, N.; Hawkins, M. A Systematic Review of Innovative Diabetes Care Models in Low-and Middle-Income Countries (LMICs). J. Health Care Poor Underserved 2014, 25, 72–93. [Google Scholar] [CrossRef] [PubMed]
- Glazier, R.H.; Bajcar, J.; Kennie, N.R.; Willson, K. A Systematic Review of Interventions to Improve Diabetes Care in Socially Disadvantaged Populations. Diabetes Care 2006, 29, 1675–1688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pinchevsky, Y.; Butkow, N.; Chirwa, T.; Raal, F. Treatment Gaps Found in the Management of Type 2 Diabetes at a Community Health Centre in Johannesburg, South Africa. J. Diabetes Res. 2017, 2017, 9536025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atlantis, E.; Fahey, P.; Foster, J. Collaborative care for comorbid depression and diabetes: A systematic review and meta-analysis. BMJ Open 2014, 4, e004706. [Google Scholar] [CrossRef] [Green Version]
- Powers, M.A.; Bardsley, J.K.; Cypress, M.; Funnell, M.M.; Harms, D.; Hess-Fischl, A.; Hooks, B.; Isaacs, D.; Mandel, E.D.; Maryniuk, M.D.; et al. Diabetes Self-management Education and Support in Adults with Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. J. Am. Assoc. Nurse Pr. 2020, 43, 1636–1649. [Google Scholar]
- Beck, J.; Greenwood, D.A.; Blanton, L.; Bollinger, S.T.; Butcher, M.K.; Condon, J.E.; Cypress, M.; Faulkner, P.; Fischl, A.H.; Francis, T.; et al. 2017 National Standards for Diabetes Self-Management Education and Support. Diabetes Care 2017, 40, 1409–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desse, T.A.; Vakil, K.; Mc Namara, K.; Manias, E. Impact of clinical pharmacy interventions on health and economic outcomes in type 2 diabetes: A systematic review and meta-analysis. Diabet. Med. 2021, 38, e14526. [Google Scholar] [CrossRef]
- Habte, B.M.; Kebede, T.; Fenta, T.G.; Boon, H. Barriers and facilitators to adherence to anti-diabetic medications: Ethiopian patients’ perspectives. Afr. J. Prim. Health Care Fam. Med. 2017, 9, 9. [Google Scholar] [CrossRef]
- Ethiopian Public Health Institute. Services Availability and Readiness Assessment (SARA); Ethiopian Public Health Institute: Addis Ababa, Ethiopia, 2018. [Google Scholar]
- Cheneke, W.; Suleman, S.; Yemane, T.; Abebe, G. Assessment of glycemic control using glycated hemoglobin among diabetic patients in Jimma University sspecialised hospital, Ethiopia. BMC Res. Notes 2016, 9, 96. [Google Scholar] [CrossRef] [Green Version]
- Abebe, N.; Kebede, T.; Addise, D. Diabetes in Ethiopia 2000–2016—Prevalence and related acute and chronic complications; a systematic review. Afr. J. Diabetes Med. 2017, 25, 7–12. [Google Scholar]
- Fiseha, T.; Alemayehu, E.; Kassahun, W.; Adamu, A.; Gebreweld, A. Factors associated with glycemic control among diabetic adult out-patients in Northeast Ethiopia. BMC Res. Notes 2018, 11, 316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tekalegn, Y.; Addissie, A.; Kebede, T.; Ayele, W. Magnitude of glycemic control and its associated factors among patients with type 2 diabetes at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. PLoS ONE 2018, 13, e0193442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Desse, T.A.; Eshetie, T.C.; Gudina, E.K. Predictors and treatment outcome of hyperglycemic emergencies at Jimma University Specialized Hospital, southwest Ethiopia. BMC Res. Notes 2015, 8, 553. [Google Scholar] [CrossRef] [Green Version]
- Reba, K.; Argaw, Z.; Walle, B.; Gutema, H. Health-related quality of life of patients with diagnosed type 2 diabetes in Felege Hiwot Referral Hospital, North West Ethiopia: A cross-sectional study. BMC Res. Notes 2018, 11, 544. [Google Scholar] [CrossRef]
- Zimmermann, M.; Bunn, C.; Namadingo, H.; Gray, C.M.; Lwanda, J. Experiences of type 2 diabetes in sub-Saharan Africa: A scoping review. Glob. Health Res. Policy 2018, 3, 25. [Google Scholar] [CrossRef] [Green Version]
- Godman, B.; Basu, D.; Pillay, Y.; Mwita, J.C.; Rwegerera, G.M.; Paramadhas, B.D.A.; Tiroyakgosi, C.; Okwen, P.M.; Niba, L.L.; Nonvignon, J.; et al. Review of Ongoing Activities and Challenges to Improve the Care of Patients With Type 2 Diabetes Across Africa and the Implications for the Future. Front. Pharmacol. 2020, 11, 108. [Google Scholar] [CrossRef]
- Yifter, H.; Reja, A.; Ahmed, A.; Narayan, K.M.V.; Amogne, W. Achievement of diabetes care goals at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiop. Med. J. 2020, 58, 125–130. [Google Scholar]
- Desse, T.A.; Namara, K.M.; Yifter, H.; Manias, E. Current practices and future preferences of type 2 diabetes care in a developing country: A qualitative study of patient, health professional, and policymaker perspectives. 2021. [Google Scholar]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: An introduction to the new Medical Research Council guidance. Evid.-Based Public Health 2009, 337, a1655. [Google Scholar] [CrossRef]
- Murphy, M.E.; Byrne, M.; Zarabzadeh, A.; Corrigan, D.; Fahey, T.; Smith, S.M. Development of a complex intervention to promote appropriate prescribing and medication intensification in poorly controlled type 2 diabetes mellitus in Irish general practice. Implement. Sci. 2017, 12, 115. [Google Scholar] [CrossRef] [Green Version]
- Francis, J.J.; Eccles, M.P.; Johnston, M.; Whitty, P.; Grimshaw, J.M.; Kaner, E.F.; Smith, L.; Walker, A. Explaining the effects of an intervention designed to promote evidence-based diabetes care: A theory-based process evaluation of a pragmatic cluster randomised controlled trial. Implement. Sci. 2008, 3, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel. A Guide to Designing Interventions; Silverback Publishing: Sutton, UK, 2014. [Google Scholar]
- Sinnott, C.; Mercer, S.W.; Payne, R.A.; Duerden, M.; Bradley, C.P.; Byrne, M. Improving medication management in multimorbidity: Development of the MultimorbiditY COllaborative Medication Review And DEcision Making (MY COMRADE) intervention using the Behaviour Change Wheel. Implement. Sci. 2015, 10, 132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smits, S.; McCutchan, G.; Wood, F.; Edwards, A.; Lewis, I.; Robling, M.; Paranjothy, S.; Carter, B.; Townson, J.; Brain, K. Development of a Behavior Change Intervention to Encourage Timely Cancer Symptom Presentation Among People Living in Deprived Communities Using the Behavior Change Wheel. Ann. Behav. Med. 2018, 52, 474–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sargent, L.; McCullough, A.; Del Mar, C.; Lowe, J. Using theory to explore facilitators and barriers to delayed prescribing in Australia: A qualitative study using the Theoretical Domains Framework and the Behaviour Change Wheel. BMC Fam. Pr. 2017, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Mangurian, C.; Niu, G.C.; Schillinger, D.; Newcomer, J.W.; Dilley, J.; Handley, M.A. Utilisation of the Behavior Change Wheel framework to develop a model to improve cardiometabolic screening for people with severe mental illness. Implement. Sci. 2017, 12, 134. [Google Scholar] [CrossRef] [Green Version]
- Steinmo, S.; Fuller, C.C.; Stone, S.P.; Michie, S. Characterising an implementation intervention in terms of behaviour change techniques and theory: The ‘Sepsis Six’ clinical care bundle. Implement. Sci. 2015, 10, 111. [Google Scholar] [CrossRef] [Green Version]
- Jackson, C.; Eliasson, L.; Barber, N.; Weinman, J. Applying COM-B to medication adherence: A suggested framework for research and interventions. Eur. Health Psychol. 2014, 16, 7–17. [Google Scholar]
- Leykum, L.K.; Pugh, J.; Lawrence, V.; Parchman, M.; Noël, P.H.; Cornell, J.; McDaniel, R.R. Organisational interventions employing principles of complexity science have improved outcomes for patients with Type II diabetes. Implement. Sci. 2007, 2, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, M.E.; Byrne, M.; Galvin, R.; Boland, F.; Fahey, T.; Smith, S. Improving risk factor management for patients with poorly controlled type 2 diabetes: A systematic review of healthcare interventions in primary care and community settings. BMJ Open 2017, 7, e015135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Renders, C.M.; Valk, G.D.; Griffin, S.J.; Wagner, E.H.; Eijk van, J.T.; Assendelft, W.J. Interventions to Improve the Management of Diabetes in Primary Care, Outpatient, and Community Settings. Diabetes Care 2001, 24, 1821–1833. [Google Scholar] [CrossRef] [Green Version]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Rowlands, G.; Sims, J.; Kerry, S. A lesson learnt: The importance of modelling in srandomised controlled trials for complex interventions in primary care. Fam. Pract. 2005, 22, 132–139. [Google Scholar] [CrossRef] [Green Version]
- Ogrinc, G.; Davies, L.; Goodman, D.; Batalden, P.; Davidoff, F.; Stevens, D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 2016, 25, 986. [Google Scholar] [CrossRef] [Green Version]
- Yimam, M.; Desse, T.A.; Hebo, H.J. Glycemic control among ambulatory type 2 diabetes patients with hypertension Co-morbidity in a developing country: A cross sectional study. Heliyon 2020, 6, e05671. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, M.; Blue, A.; Aschenbrener, C.A.; Viggiano, T.R. Core competencies for interprofessional collaborative practice: Reforming health care by transforming health professionals’ education. Acad. Med. 2011, 86, 1351. [Google Scholar] [CrossRef] [PubMed]
- Gucciardi, E.; Espin, S.; Morganti, A.; Dorado, L. Exploring interprofessional collaboration during the integration of diabetes teams into primary care. BMC Fam. Pr. 2016, 17, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Erturkmen, G.B.; Yuksel, M.; Sarigul, B.; Arvanitis, T.N.; Lindman, P.; Chen, R.; Zhao, L.; Sadou, E.; Bouaud, J.; Traore, L.; et al. A Collaborative Platform for Management of Chronic Diseases via Guideline-Driven Individualized Care Plans. Comput. Struct. Biotechnol. J. 2019, 17, 869–885. [Google Scholar] [CrossRef]
- Phelps, K.W.; Howell, C.D.; Hill, S.G.; Seemann, T.S.; Lamson, A.L.; Hodgson, J.L.; Smith, D.A. A collaborative care model for patients with Type-2 diabetes. Fam. Syst. Health 2009, 27, 131–140. [Google Scholar] [CrossRef]
- Johnson, J.; Carragher, R. Interprofessional collaboration and the care and management of type 2 diabetic patients in the Middle East: A systematic review. J. Interprof. Care 2018, 32, 621–628. [Google Scholar] [CrossRef]
- Presseau, J.; Ivers, N.M.; Newham, J.J.; Knittle, K.; Danko, K.J.; Grimshaw, J.M. Using a behaviour change techniques taxonomy to identify active ingredients within trials of implementation interventions for diabetes care. Implement. Sci. 2015, 10, 55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartholomew, L.K.; Mullen, P.D. Five roles for using theory and evidence in the design and testing of behavior change interventions. J. Public Health Dent. 2011, 71, S20–S33. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From Theory to Intervention: Mapping Theoretically Derived Behavioural Determinants to Behaviour Change Techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Whitford, D.L.; Roberts, S.H.; Griffin, S. Sustainability and effectiveness of comprehensive diabetes care to a district population. Diabet. Med. 2004, 21, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Barrera-Cancedda, A.E.; Riman, K.A.; Shinnick, J.E.; Buttenheim, A.M. Implementation strategies for infection prevention and control promotion for nurses in Sub-Saharan Africa: A systematic review. Implement. Sci. 2019, 14, 111. [Google Scholar] [CrossRef] [Green Version]
- Opiyo, N.; Ciapponi, A.; Dudley, L.; Gagnon, M.-P.; Herrera, C.; Lewin, S.; Martí, S.G.; Oxman, A.D.; Paulsen, E.; Penaloza, B.; et al. Implementation strategies for health systems in low-income countries: An overview of systematic reviews. Cochrane Database Syst. Rev. 2014, 9, CD011086. [Google Scholar] [CrossRef] [Green Version]
- Johnson, L.G.; Armstrong, A.; Joyce, C.M.; Teitelman, A.M.; Buttenheim, A.M. Implementation strategies to improve cervical cancer prevention in sub-Saharan Africa: A systematic review. Implement. Sci. 2018, 13, 28. [Google Scholar] [CrossRef] [Green Version]
- Elwyn, G.; Scholl, I.; Tietbohl, C.; Mann, M.; Edwards, A.G.K.; Clay, C.; Légaré, F.; Van Der Weijden, T.; Lewis, C.L.; Wexler, R.M.; et al. “Many miles to go …”: A systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med. Inform. Decis. Mak. 2013, 13, S14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scholl, I.; LaRussa, A.; Hahlweg, P.; Kobrin, S.; Elwyn, G. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them—A scoping review. Implement. Sci. 2018, 13, 40. [Google Scholar] [CrossRef] [Green Version]
- Joseph-Williams, N.; Lloyd, A.; Edwards, A.; Stobbart, L.; Tomson, D.; Macphail, S.; Dodd, C.; Brain, K.; Elwyn, G.; Thomson, R. Implementing shared decision making in the NHS: Lessons from the MAGIC programme. BMJ 2017, 357, j1744. [Google Scholar] [CrossRef] [Green Version]
- Yapa, H.M.; Bärnighausen, T. Implementation science in resource-poor countries and communities. Implement. Sci. 2018, 13, 154. [Google Scholar] [CrossRef] [PubMed]
- Eccles, M.P.; Mittman, B.S. Welcome to Implementation Science. Implement. Sci. 2006, 1, 13. [Google Scholar] [CrossRef] [Green Version]
- Kalbarczyk, A.; Davis, W.; Kalibala, S.; Geibel, S.; Yansaneh, A.; Martin, N.A.; Weiss, E.; Kerrigan, D.; Manabe, Y.C. Research Capacity Strengthening in Sub-Saharan Africa: Recognising the Importance of Local Partnerships in Designing and Disseminating HIV Implementation Science to Reach the 90-90-90 Goals. AIDS Behav. 2019, 23 (Suppl. 2), 206–213. [Google Scholar] [CrossRef] [Green Version]
- Osanjo, G.O.; Oyugi, J.O.; Kibwage, I.O.; Mwanda, W.O.; Ngugi, E.N.; Otieno, F.C.; Ndege, W.; Child, M.; Farquhar, C.; Penner, J.; et al. Building capacity in implementation science research training at the University of Nairobi. Implement. Sci. 2015, 11, 30. [Google Scholar] [CrossRef] [Green Version]
- Iwelunmor, J.; Blackstone, S.; Veira, D.; Nwaozuru, U.; Airhihenbuwa, C.; Munodawafa, D.; Kalipeni, E.; Jutal, A.; Shelley, D.; Ogedegebe, G. Toward the sustainability of health interventions implemented in sub-Saharan Africa: A systematic review and conceptual framework. Implement. Sci. 2015, 11, 43. [Google Scholar] [CrossRef] [Green Version]
- World Bank Group. Africa’s Pulse, No. 16; World Bank: Washington, DC, USA, 2017. [Google Scholar]
- WHO. The Abuja Declaration: Ten Years On; WHO: Geneva, Switzerland, 2011.
- The Federal Democratic Republic of Ethiopia Ministry of Health. Health Sector Transformation Plan: 2015/16–2019/20; The Federal Democratic Republic of Ethiopia Ministry of Health: Addis Ababa, Ethiopia, 2015.
- Ministry of Health of Ethiopia. Ethiopian National Health Care Quality Strategy: 2016–2020; Ministry of Health of Ethiopia: Addis Ababa, Ethiopia, 2016.
- Ministry of Health of Ethiopia. Essential Health Services Package of Ethiopia; Ministry of Health of Ethiopia: Addis Ababa, Ethiopia, 2019.
- Manyazewal, T.; Matlakala, M. Implementing health care reform: Implications for performance of public hospitals in central Ethiopia. J. Glob. Health 2018, 8, 010403. [Google Scholar] [CrossRef]
- Walker, R.J.; Smalls, B.L.; Bonilha, H.S.; Campbell, J.A.; Egede, L.E. Behavioral interventions to improve glycemic control in African Americans with type 2 diabetes: A systematic review. Ethn. Dis. 2013, 23, 401–408. [Google Scholar]
- Flood, D.; Hane, J.; Dunn, M.; Brown, S.J.; Wagenaar, B.H.; Rogers, E.A.; Heisler, M.; Rohloff, P.; Chopra, V. Health system interventions for adults with type 2 diabetes in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2020, 17, e1003434. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Ivers, N.M.; Grimshaw, J.; Moher, D.; Turner, L.; Galipeau, J.; Halperin, I.; Vachon, B.; Ramsay, T.; Manns, B.; et al. Effectiveness of quality improvement strategies on the management of diabetes: A systematic review and meta-analysis. Lancet 2012, 379, 2252–2261. [Google Scholar] [CrossRef]
- Murphy, A.L.; Gardner, D.M.; Kutcher, S.P.; Martin-Misener, R. A theory-informed approach to mental health care capacity building for pharmacists. Int. J. Ment. Health Syst. 2014, 8, 46. [Google Scholar] [CrossRef] [Green Version]
- Hood, K.K.; Hilliard, M.; Piatt, G.A.; Ievers-Landis, C.E. Effective strategies for encouraging behavior change in people with diabetes. Diabetes Manag. 2015, 5, 499–510. [Google Scholar] [CrossRef]
- Cadogan, C.A.; Ryan, C.; Francis, J.J.; Gormley, G.J.; Passmore, P.; Kerse, N.; Hughes, C.M. Improving appropriate polypharmacy for older people in primary care: Selecting components of an evidence-based intervention to target prescribing and dispensing. Implement. Sci. 2015, 10, 161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chauhan, B.F.; Jeyaraman, M.; Mann, A.S.; Lys, J.; Skidmore, B.; Sibley, K.M.; Abou-Setta, A.M.; Zarychanksi, R. Behavior change interventions and policies influencing primary healthcare professionals’ practice—An overview of reviews. Implement. Sci. 2017, 12, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nielsen, K.; Abildgaard, J.S. Organisational interventions: A research-based framework for the evaluation of both process and effects. Work Stress 2013, 27, 278–297. [Google Scholar] [CrossRef]
- Clement, M.; Filteau, P.; Harvey, B.; Jin, S.; Laubscher, T.; Mukerji, G.; Sherifali, D. Organization of Diabetes Care. Can. J. Diabetes 2018, 42, S27–S35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Association of Diabetes Educators. An Effective Model of Diabetes Care and Education: Revising the AADE7 Self-Care Behaviors®. Diabetes Educ. 2020, 46, 139–160. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Bardram, J.E.; Bækgaard, P.; Cramer-Petersen, C.L.; Skinner, T.; Vrangbæk, K.; Starr, L.; Nørgaard, K.; Lind, N.; Christensen, M.B.; et al. Integrated spersonalised diabetes management goes Europe: A multi-disciplinary approach to innovating type 2 diabetes care in Europe. Prim. Care Diabetes 2021, 15, 360–364. [Google Scholar] [CrossRef]
- Mercer, T.; Chang, A.C.; Fischer, L.; Gardner, A.; Kerubo, I.; Tran, D.N.; Laktabai, J.; Pastakia, S. Mitigating The Burden Of Diabetes in Sub-Saharan Africa Through an Integrated Diagonal Health Systems Approach. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 2261–2272. [Google Scholar] [CrossRef] [Green Version]
- Mohan, V.; Khunti, K.; Chan, S.P.; Filho, F.F.; Tran, N.Q.; Ramaiya, K.; Joshi, S.; Mithal, A.; Mbaye, M.N.; Nicodemus, N.J.; et al. Management of Type 2 Diabetes in Developing Countries: Balancing Optimal Glycaemic Control and Outcomes with Affordability and Accessibility to Treatment. Diabetes Ther. 2020, 11, 15–35. [Google Scholar] [CrossRef] [Green Version]
- Hellquist, K.; Bradley, R.; Grambart, S.; Kapustin, J.; Loch, J. Collaborative Practice Benefits Patients: An Examination of Interprofessional Approaches to Diabetes Care. Health Interprof. Pract. 2012, 1, eP1017. [Google Scholar] [CrossRef]
- Lankhof, B. Perceptions of Collaboration and Mutual Respect Among Members of Interprofessional Teams. Ph.D. Thesis, Walden University, Minneapolis, MN, USA, 2018. [Google Scholar]
- Yorke, E.; Atiase, Y. Impact of structured education on glucose control and hypoglycaemia in Type-2 diabetes: A systematic review of srandomised controlled trials. Ghana Med. J. 2018, 52, 41–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chrvala, C.A.; Sherr, D.; Lipman, R.D. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ. Couns. 2016, 99, 926–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Chu, L. Effectiveness of Systematic Health Education Model for Type 2 Diabetes Patients. Int. J. Endocrinol. 2018, 2018, 6530607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohamed, A.; Staite, E.; Ismail, K.; Winkley, K. A systematic review of diabetes self-management education interventions for people with type 2 diabetes mellitus in the Asian Western Pacific (AWP) region. Nurs. Open 2019, 6, 1424–1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Do Rosario Pinto, M.; Parreira, P.; Basto, M.L.; Dos Santos Mendes Monico, L. Impact of a structured multicomponent educational intervention program on metabolic control of patients with type 2 diabetes. BMC Endocr. Disord. 2017, 17, 77. [Google Scholar] [CrossRef] [Green Version]




| Components of the Complex Intervention (VICKY) | Intervention Plan and Activities | |
|---|---|---|
| 1 | Patient-centred collaborative care by a team of physicians, clinical pharmacists, nurses, dietitians or nutritionists, psychologists, and policymakers. |
|
| 2 | Referral system for patients across transition of care between different health professionals of the diabetes care team (physicians, clinical pharmacists, nurses, dietitians or nutritionists, psychologists, and policymakers). | |
| 3 | Tools for provision of collaborative care and documentation for the care provided. |
|
| 4 | Evidence-based structured diabetes education and counselling by a team of trained physician, nurse, clinical pharmacist, dietitian or nutritionist, and expert patient. |
|
| 5 | Educational materials and documentation tools for structured diabetes education and counselling. | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desse, T.A.; Namara, K.M.; Yifter, H.; Manias, E. Development of a Complex Intervention for Effective Management of Type 2 Diabetes in a Developing Country. J. Clin. Med. 2022, 11, 1149. https://doi.org/10.3390/jcm11051149
Desse TA, Namara KM, Yifter H, Manias E. Development of a Complex Intervention for Effective Management of Type 2 Diabetes in a Developing Country. Journal of Clinical Medicine. 2022; 11(5):1149. https://doi.org/10.3390/jcm11051149
Chicago/Turabian StyleDesse, Tigestu Alemu, Kevin Mc Namara, Helen Yifter, and Elizabeth Manias. 2022. "Development of a Complex Intervention for Effective Management of Type 2 Diabetes in a Developing Country" Journal of Clinical Medicine 11, no. 5: 1149. https://doi.org/10.3390/jcm11051149
APA StyleDesse, T. A., Namara, K. M., Yifter, H., & Manias, E. (2022). Development of a Complex Intervention for Effective Management of Type 2 Diabetes in a Developing Country. Journal of Clinical Medicine, 11(5), 1149. https://doi.org/10.3390/jcm11051149






