Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution’s Experience from an Endemic Area
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design—Settings
2.1.1. Variables of the Participants
2.1.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turgut, A.T.; Altin, L.; Topçu, S.; Kiliçoğlu, B.; Altinok, T.; Kaptanoğlu, E.; Karademir, A.; Kosar, U. Unusual imaging characteristics of complicated hydatid disease. Eur. J. Radiol. 2007, 63, 84–93. [Google Scholar] [CrossRef]
- Safioleas, M.C.; Misiakos, E.P.; Kouvaraki, M.; Stamatakos, M.K.; Manti, C.P.; Felekouras, E.S. Hydatid Disease of the Liver: A Continuing Surgical Problem. Arch. Surg. 2006, 141, 1101–1108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuxun, T.; Zhang, J.-H.; Zhao, J.-M.; Tai, Q.-W.; Abudurexti, M.; Ma, H.-Z.; Wen, H. World review of laparoscopic treatment of liver cystic echinococcosis—914 patients. Int. J. Infect. Dis. 2014, 24, 43–50. [Google Scholar] [CrossRef] [Green Version]
- Agayev, R.M.O. Diagnosis and surgical treatment of complicated liver echinococcosis. Turk. J. Gastroenterol. 2002, 13, 11–16. [Google Scholar]
- Yağmur, Y.; Akbulut, S.; Gümüs, S.; Babür, M.; Can, M.A. Laparoscopic management of hydatid cyst of the liver. S. Afr. J. Surg. 2016, 54, 14–17. [Google Scholar]
- Smego, R.A.; Sebanego, P. Treatment options for hepatic cystic echinococcosis. Int. J. Infect. Dis. 2005, 9, 69–76. [Google Scholar] [CrossRef] [Green Version]
- Shaw, J.M.; Bornman, P.C.; Krige, J.E.J. Hydatid disease of the liver. S. Afr. J. Surg. 2006, 44, 70–72, 74–77. [Google Scholar] [PubMed]
- Da Silva, A.M. Human Echinococcosis: A Neglected Disease. Gastroenterol. Res. Pract. 2010, 583297, 9. [Google Scholar] [CrossRef] [PubMed]
- Darbari, A.; Jauhari, A.; Shrivastava, A. Management of hepatic hydatidosis by open versus laparoscopic surgery. Int. J. Res. Med. Sci. 2014, 2, 1371. [Google Scholar] [CrossRef] [Green Version]
- Malik, A.A.; Bari, S.U.; Amin, R.; Jan, M. Surgical management of complicated hydatid cysts of the liver. World J. Gastrointest. Surg. 2010, 2, 78–84. [Google Scholar] [CrossRef]
- Acarli, K. Controversies in the laparoscopic treatment of hepatic hydatid disease. HPB 2004, 6, 213–221. [Google Scholar] [CrossRef] [Green Version]
- Soliman, H.E.M.; Shoreem, H.A.; Abdelsallam, O.H.; Saleh, S.M.; Badawey, M.T.; Sallam, A.N.; Ayoub, I.A.; Gad, E.H.; Yaseen, T.E.; Lasheen, H.Z.; et al. Laparoscopic management of parasitic liver cysts: A retrospective, comparative study. Saudi Surg. J. 2017, 5, 35. [Google Scholar] [CrossRef]
- Anand, S.; Rajagopalan, B.S.; Mohan, R. Management of liver hydatid cysts-current perspectives. Med. J. Armed Forces India 2012, 68, 304–309. [Google Scholar] [CrossRef] [Green Version]
- Busić, Z.; Cupurdija, K.; Servis, D.; Kolovrat, M.; Cavka, V.; Boras, Z.; Busic, D.; Kristek, J.; Tucak, A.; Busic, N. Surgical Treatment of Liver Echinococcosis-Open or Laparoscopic Surgery? Coll. Antropol. 2012, 36, 1363–1366. [Google Scholar]
- WHO Echinococcosis, Fact Sheet. Available online: http://www.who.int/mediacentre/factsheets/fs377/en/ (accessed on 28 August 2017).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sotiraki, S.; Chaligiannis, I. Cystic echinococcosis in Greece. Past and present. Parasite 2010, 17, 205–210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Budke, C.; Deplazes, P.; Torgerson, P.R. Global Socioeconomic Impact of Cystic Echinococcosis. Emerg. Infect. Dis. 2006, 12, 296–303. [Google Scholar] [CrossRef]
- Torgerson, P.R. Economic Effects of Echinococcosis. Acta Trop. 2003, 85, 113–118. [Google Scholar] [CrossRef]
- Muftuoglu, M.A.T.; Koksal, N.; Topaloglu, U. The role of omentoplasty in the surgical management of remnant cavity in hepatic hydatid cyst. HPB 2005, 7, 231–234. [Google Scholar] [CrossRef] [Green Version]
- Martin, R.M.; Colebrook, A.L.; Gasser, R.B.; Lightowlers, M.W. Antibody responses of patients with cystic hydatid disease to recombinant myophilin of Echinococcus granulosus. Acta Trop. 1996, 61, 307–314. [Google Scholar] [CrossRef]
- Refik, M.; Mehmet, N.; Durmaz, R. Postoperative changes in serum cytokines profile and nitric oxide levels in patients with cystic echinococcosis. Parasite 2005, 12, 265–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Filippou, D.; Tselepis, D.; Filippou, G.; Papadopoulos, V. Advances in Liver Echinococcosis: Diagnosis and Treatment. Clin. Gastroenterol. Hepatol. 2007, 5, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Galati, G.; Sterpetti, A.V.; Caputo, M.; Adduci, M.; Lucandri, G.; Brozzetti, S.; Bolognese, A.; Cavallaro, A. Endoscopic retrograde cholangiography for intrabiliary rupture of hydatid cyst. Am. J. Surg. 2006, 191, 206–210. [Google Scholar] [CrossRef]
- Akcakaya, A.; Sahin, M.; Karakelleoglu, A.; Okan, I. Endoscopic stenting for selected cases of biliary fistula after hepatic hydatid surgery. Surg. Endosc. 2006, 20, 1415–1418. [Google Scholar] [CrossRef] [PubMed]
- Saritas, Ü.; Parlak, E.; Akoglu, M.; Sahin, B. Effectiveness of Endoscopic Treatment Modalities in Complicated Hepatic Hydatid Disease after Surgical Intervention. Endoscopy 2001, 33, 858–863. [Google Scholar] [CrossRef]
- Dziri, C.; Haouet, K.; Fingerhut, A. Treatment of Hydatid Cyst of the Liver: Where Is the Evidence? World J. Surg. 2004, 28, 731–736. [Google Scholar] [CrossRef]
- Yol, S.; Kartal, A.; Tavli, S.; Sahin, M.; Vatansev, C.; Karahan, O.; Belviranli, M. Open drainage versus overlapping method in the treatment of hepatic hydatid cyst cavities. Int. Surg. 1999, 84, 139–143. [Google Scholar]
- Katsinelos, P.; Paroutoglou, G.; Chatzimavroudis, G.; Beltsis, A.; Mimidis, K.; Katsinelos, T.; Pilpilidis, I.; Papaziogas, B. Successful treatmne tof intractable bronchobiliary fistula using long-term biliary stenting. Surg. Laparosc. Endosc. Percutan. Tech. 2007, 17, 206–209. [Google Scholar] [CrossRef]
- Patrinou, V.; Dougenis, D.; Kritikos, N.; Polydorou, A.; Vagianos, C. Treatment of postoperative bronchobiliary fistula by nasobiliary drainage. Surg. Endosc. 2001, 15, 758. [Google Scholar] [CrossRef]
| Value/Group | Complicated HD (18) N (%) | Uncomplicated HD (32) N (%) | p-Value |
|---|---|---|---|
| Age (mean, range) | 56.3 (25–82) | 55.1 (23–81) | 0.875 |
| Male gender | 14 (78%) | 26 (81%) | 0.479 |
| Previous medical advice | 9 (50%) | 17 (53%) | 0.831 |
| Missed diagnosis | 7 (39%) | 10 (31%) | |
| Known hydatid disease | 2 (11%) | 7 (22%) | |
| Co-morbidities | 13 (72%) | 20 (63%) | 0.486 |
| Cardiovascular | 5 (28%) | 10 (31%) | |
| Respiratory | 4 (22%) | 7 (22%) | |
| Diabetes mellitus | 2 (11%) | 3 (9%) | |
| >1 co-morbidities | 6 (33%) | 12 (60%) | |
| Clinical presentation | |||
| Non-specific | 18 (100%) | 29 (91%) | |
| Nausea, vomiting | 17 (94%) | 22 (69%) | |
| RUQ tenderness | 16 (88%) | 25 (78%) | |
| Fever | 14 (78%) | 7 (22%) | |
| Yellow sputum | 2 (11%) | 0 | |
| Acute cholangitis | 2 (11%) | 0 | |
| Acute abdomen | 1 (0.5%) | 0 | |
| Cyst characteristics | |||
| Number of cysts (mean, range) | 1.3 (1–4) | 1 (1–3) | 0.148 |
| Maximum diameter (mean, range) | 9.6 (4.5–20) | 7.6 (4–18) | 0.097 |
| Elevated Biochemical Values | Intra-Operative Diagnosis (N%) | |||||
|---|---|---|---|---|---|---|
| Biliary Tree Rupture (6) | Biliary Tree Communication (6) | Broncho-Biliary Fistula (2) | Rupture in the Peritoneal Cavity (2) | Abscess Formation (2) | Total (18) | |
| Bilirubin | 2/6 (33%) | 0/6 (0%) | 0/2 (0%) | 0/2 (0%) | 0/2 (0%) | 2/18 (11%) |
| ALP/γGT | 4/6 (66%) | 4/6 (66%) | 2/2 (100%) | 1/2 (50%) | 0/2 (0%) | 11/18 (61%) |
| CRP | 5/6 (83%) | 1/6 (17%) | 2/2 (100%) | 2/2 (100%) | 2/2 (100%) | 12/18 (67%) |
| Eosinophiles | 2/6 (33%) | 2/6 (33%) | 2/2 (100%) | 2/2 (100%) | 2/2 (100%) | 10/18 (56%) |
| Intra-Operative Diagnosis (N%) | ||||||
|---|---|---|---|---|---|---|
| Biliary Tree Rupture (6) | Biliary Tree Communication (6) | Broncho-Biliary Fistula (2) | Rupture in the Peritoneal Cavity (2) | Abscess Formation (2) | Total (18) | |
| Ultrasonography | 2/6 (33%) | 2/6 (33%) | Not performed | 0/2 (0%) | 0/2 (0%) | 4/16 (25%) |
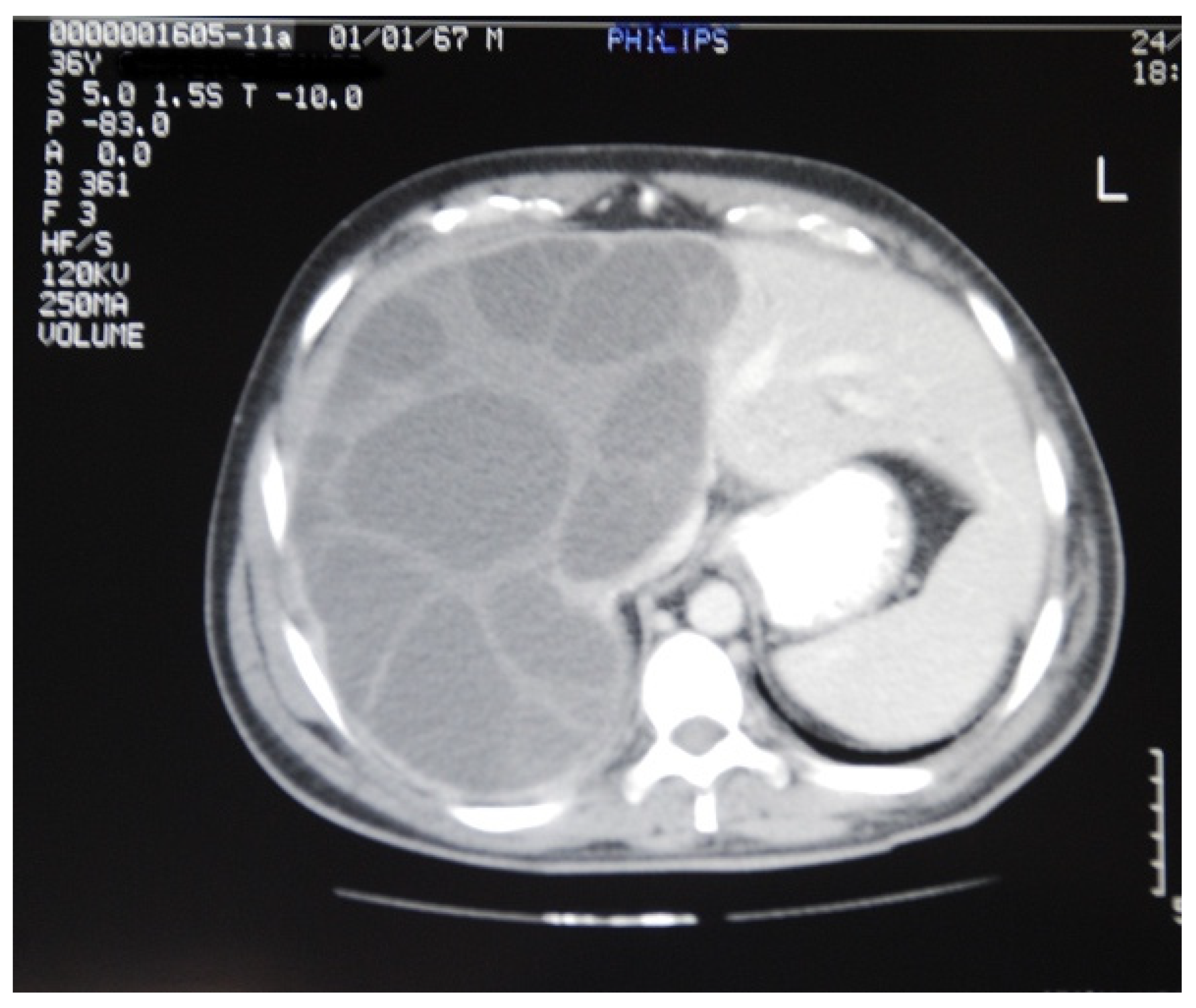
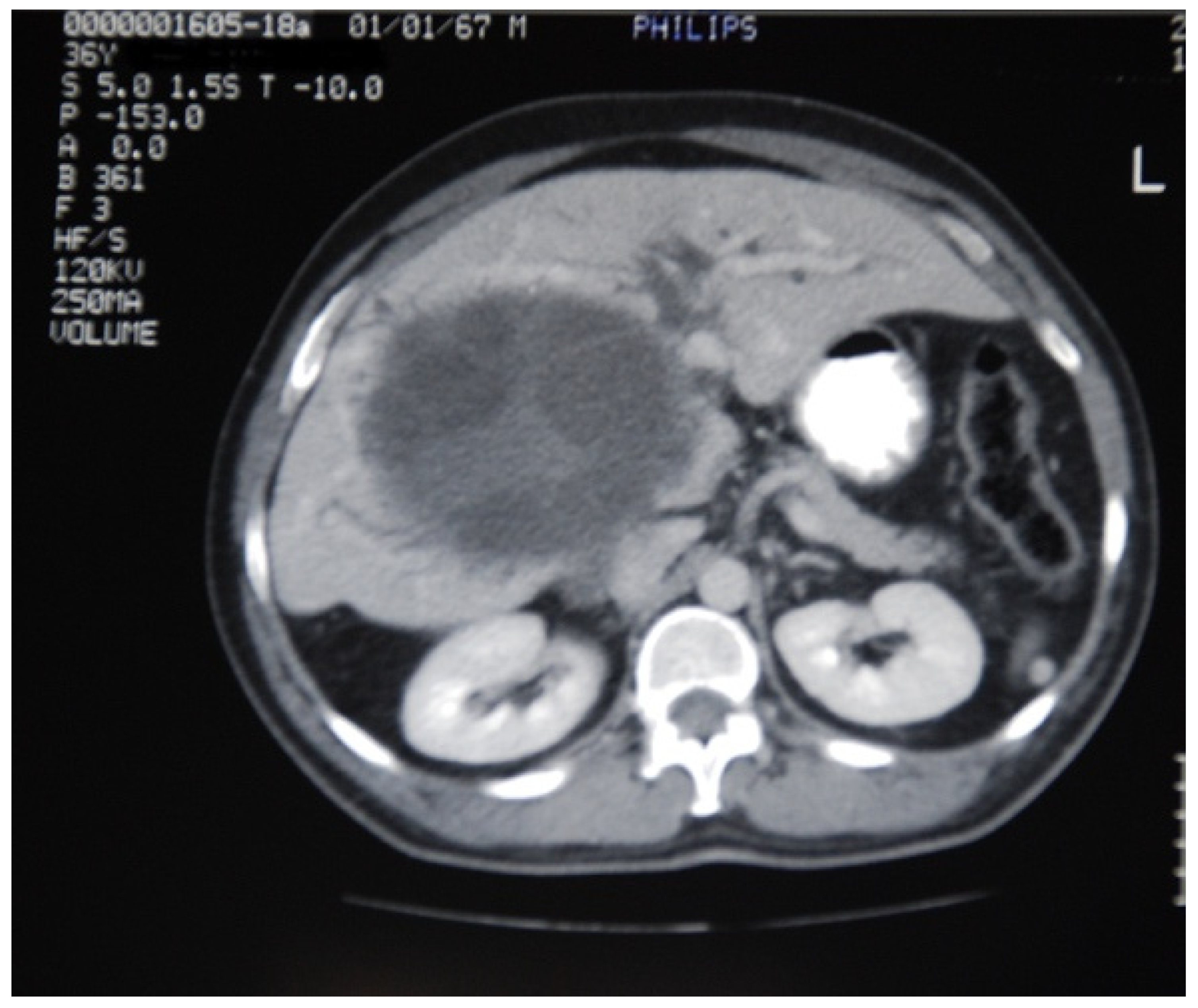
| Computer Tomography | 2/6 (33%) | 1/6 (17%) | 2/2 (100%) | 2/2 (100%) | 1/2 (50%) | 8/18 (44%) |
| Magnetic Resonance Imaging | 2 (100%) | Not performed | Not performed | Not performed | Not performed | 2/2 (100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christodoulidis, G.; Samara, A.A.; Diamantis, A.; Floros, T.; Sgantzou, I.-K.; Karakantas, K.-S.; Zotos, P.-A.; Koutras, A.; Janho, M.B.; Tepetes, K. Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution’s Experience from an Endemic Area. Medicina 2021, 57, 1210. https://doi.org/10.3390/medicina57111210
Christodoulidis G, Samara AA, Diamantis A, Floros T, Sgantzou I-K, Karakantas K-S, Zotos P-A, Koutras A, Janho MB, Tepetes K. Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution’s Experience from an Endemic Area. Medicina. 2021; 57(11):1210. https://doi.org/10.3390/medicina57111210
Chicago/Turabian StyleChristodoulidis, Gregory, Athina A. Samara, Alexandros Diamantis, Theodoros Floros, Ioanna-Konstantina Sgantzou, Kostas-Sotirios Karakantas, Prokopis-Andreas Zotos, Antonios Koutras, Michel B. Janho, and Konstantinos Tepetes. 2021. "Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution’s Experience from an Endemic Area" Medicina 57, no. 11: 1210. https://doi.org/10.3390/medicina57111210
APA StyleChristodoulidis, G., Samara, A. A., Diamantis, A., Floros, T., Sgantzou, I. -K., Karakantas, K. -S., Zotos, P. -A., Koutras, A., Janho, M. B., & Tepetes, K. (2021). Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution’s Experience from an Endemic Area. Medicina, 57(11), 1210. https://doi.org/10.3390/medicina57111210







