A Rare Case of Prostatic Utricle with Crossover Vas Deferens in Children
Abstract
:1. Introduction
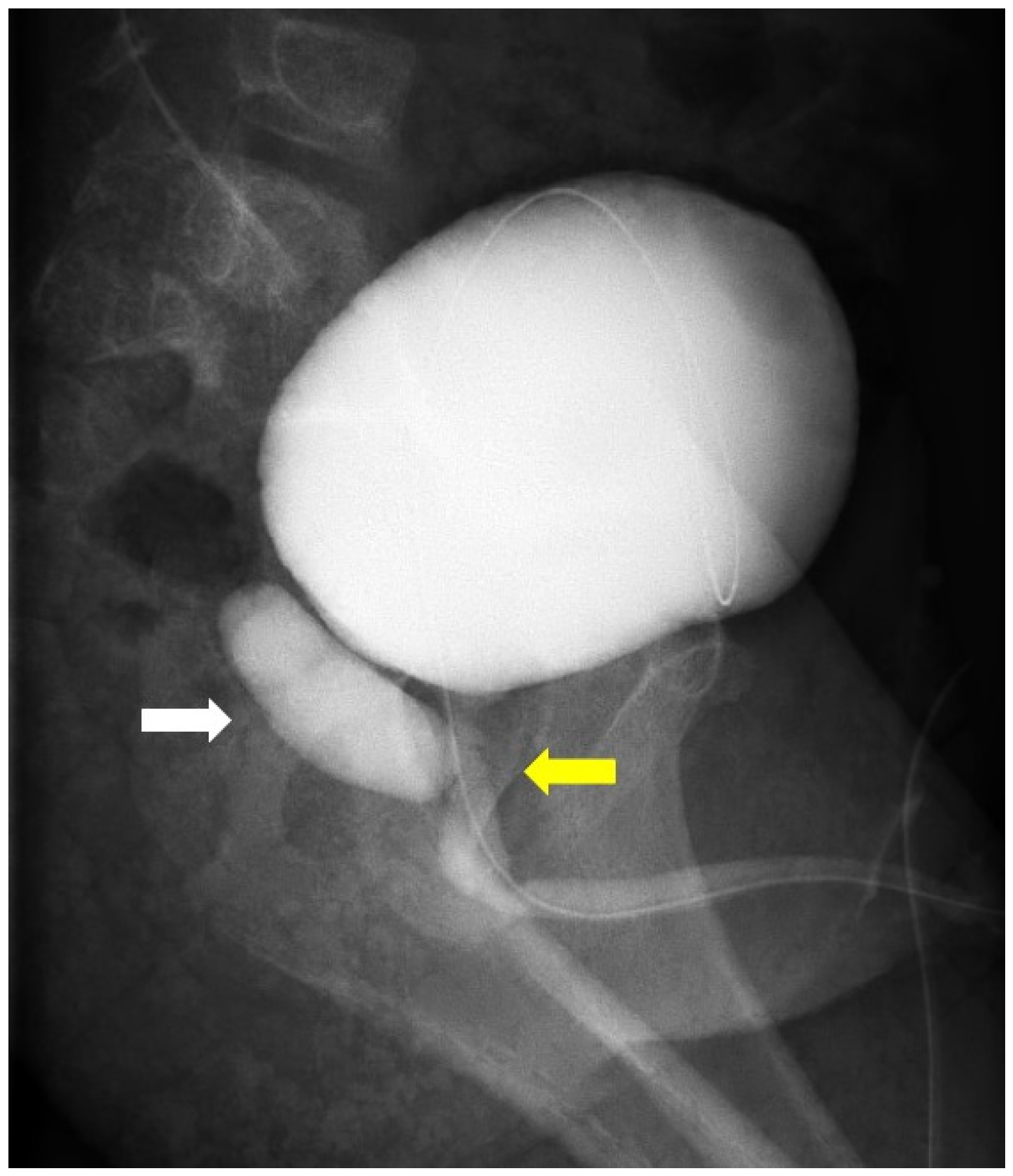
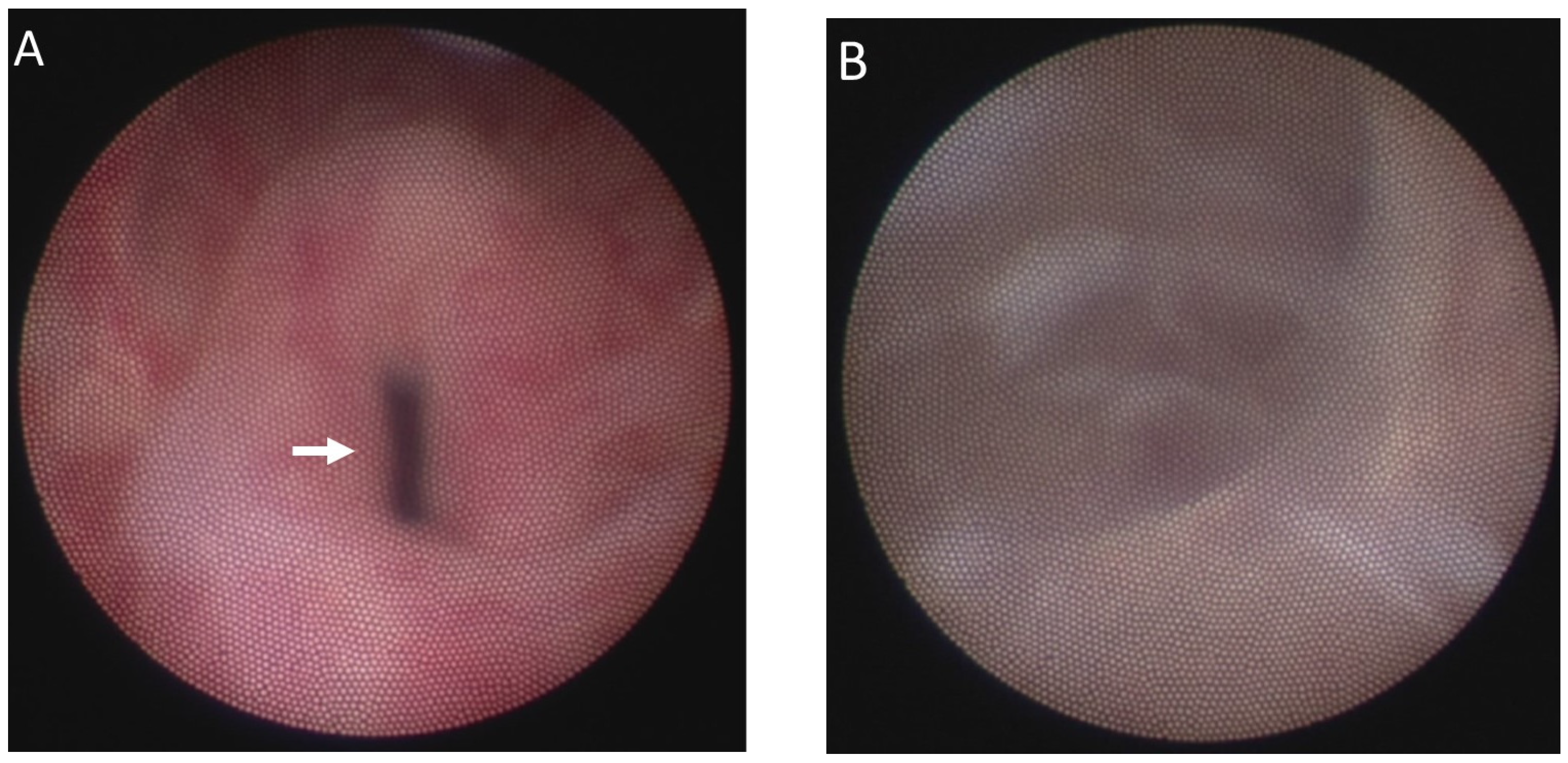
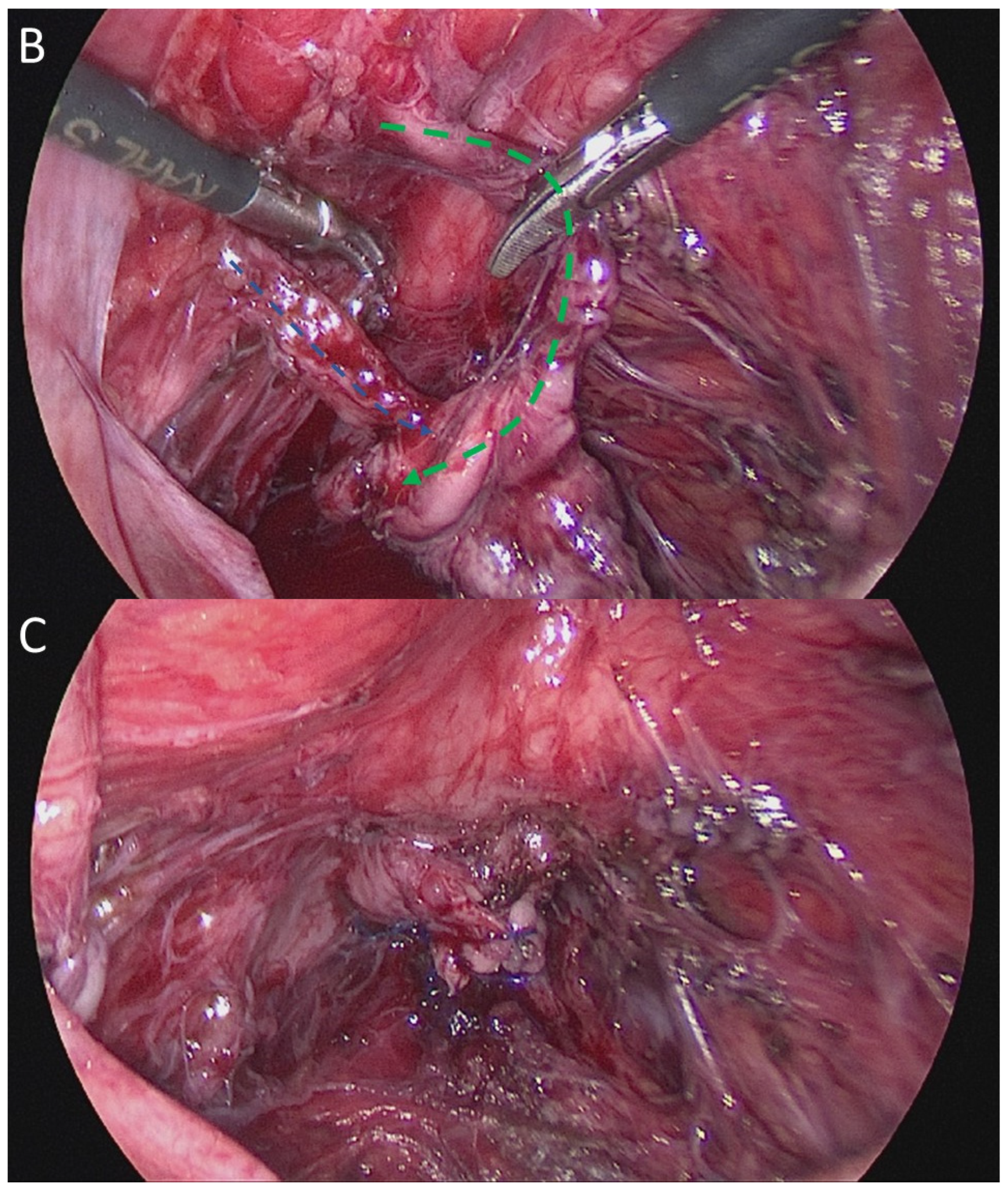
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Yeung, C.; Sihoe, J.; Tam, Y.; Lee, K. Laparoscopic excision of prostatic utricles in children. BJU Int. 2001, 87, 505–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Di Benedetto, V.; Bagnara, V.; Guys, J.; Meyrat, J.; Monfort, G. A transvesical approach to mullerian duct remnants. Pediatric Surg. Int. 1997, 12, 151–154. [Google Scholar] [CrossRef]
- Picard, J.-Y.; Cate, R.L.; Racine, C.; Josso, N. The persistent Müllerian duct syndrome: An update based upon a personal experience of 157 cases. Sex. Dev. 2017, 11, 109–125. [Google Scholar] [CrossRef] [PubMed]
- Devine, C.J., Jr.; Gonzalez-Serva, L.; Stecker, J.F., Jr.; Devine, P.C.; Horton, C.E. Utricular configuration in hypospadias and intersex. J. Urol. 1980, 123, 407–411. [Google Scholar] [CrossRef]
- Ikoma, F.; Shima, H.; Yabumoto, H.; Mori, Y. Surgical treatment for enlarged prostatic utricle and vagina masculina in patients with hypospadias. Br. J. Urol. 1986, 58, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Hendry, W.; Pryor, J. Müllerian duct (prostatic utricle) cyst: Diagnosis and treatment in subfertile males. Br. J. Urol. 1992, 69, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Schuhrke, T.D.; Kaplan, G.W. Prostatic utricle cysts (müllerian duct cysts). J. Urol. 1978, 119, 765–767. [Google Scholar] [CrossRef]
- Jia, W.; Liu, G.-C.; Zhang, L.-Y.; Wen, Y.-Q.; Fu, W.; Hu, J.-H.; Xia, H.-M. Comparison of laparoscopic excision versus open transvesical excision for symptomatic prostatic utricle in children. J. Pediatr. Surg. 2016, 51, 1597–1601. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, I.A.; Woodward, M.N.; Shalaby, M.S. Cystoscopic-assisted laparoscopic excision of prostatic utricle. J. Pediatr. Urol. 2018, 14, 77–78. [Google Scholar] [CrossRef] [PubMed]
- Meisheri, I.; Motiwale, S.; Sawant, V. Surgical management of enlarged prostatic utricle. Pediatr. Surg. Int. 2000, 16, 199–203. [Google Scholar] [CrossRef] [PubMed]
- McDougall, E.M.; Clayman, R.V.; Bowles, W.T. Laparoscopic excision of müllerian duct remnant. J. Urol. 1994, 152, 482–484. [Google Scholar] [CrossRef]
- Lima, M.; Maffi, M.; Di Salvo, N.; Ruggeri, G.; Libri, M.; Gargano, T.; Lardy, H. Robotic removal of Müllerian duct remnants in pediatric patients: Our experience and a review of the literature. Pediatr. Med. Chir. 2018, 40, 27–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, T.-H.; Hsu, Y.-J.; Chin, T.-W.; Fu, Y.-W. A Rare Case of Prostatic Utricle with Crossover Vas Deferens in Children. Medicina 2022, 58, 40. https://doi.org/10.3390/medicina58010040
Wu T-H, Hsu Y-J, Chin T-W, Fu Y-W. A Rare Case of Prostatic Utricle with Crossover Vas Deferens in Children. Medicina. 2022; 58(1):40. https://doi.org/10.3390/medicina58010040
Chicago/Turabian StyleWu, Tsung-Heng, Yao-Jen Hsu, Tai-Wai Chin, and Yu-Wei Fu. 2022. "A Rare Case of Prostatic Utricle with Crossover Vas Deferens in Children" Medicina 58, no. 1: 40. https://doi.org/10.3390/medicina58010040
APA StyleWu, T. -H., Hsu, Y. -J., Chin, T. -W., & Fu, Y. -W. (2022). A Rare Case of Prostatic Utricle with Crossover Vas Deferens in Children. Medicina, 58(1), 40. https://doi.org/10.3390/medicina58010040





