Combined Positive Score for Programmed Death Ligand-1 Expression and Inflammatory Microenvironment in Gastrointestinal Stromal Tumors
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Patient and Tumor Characteristics
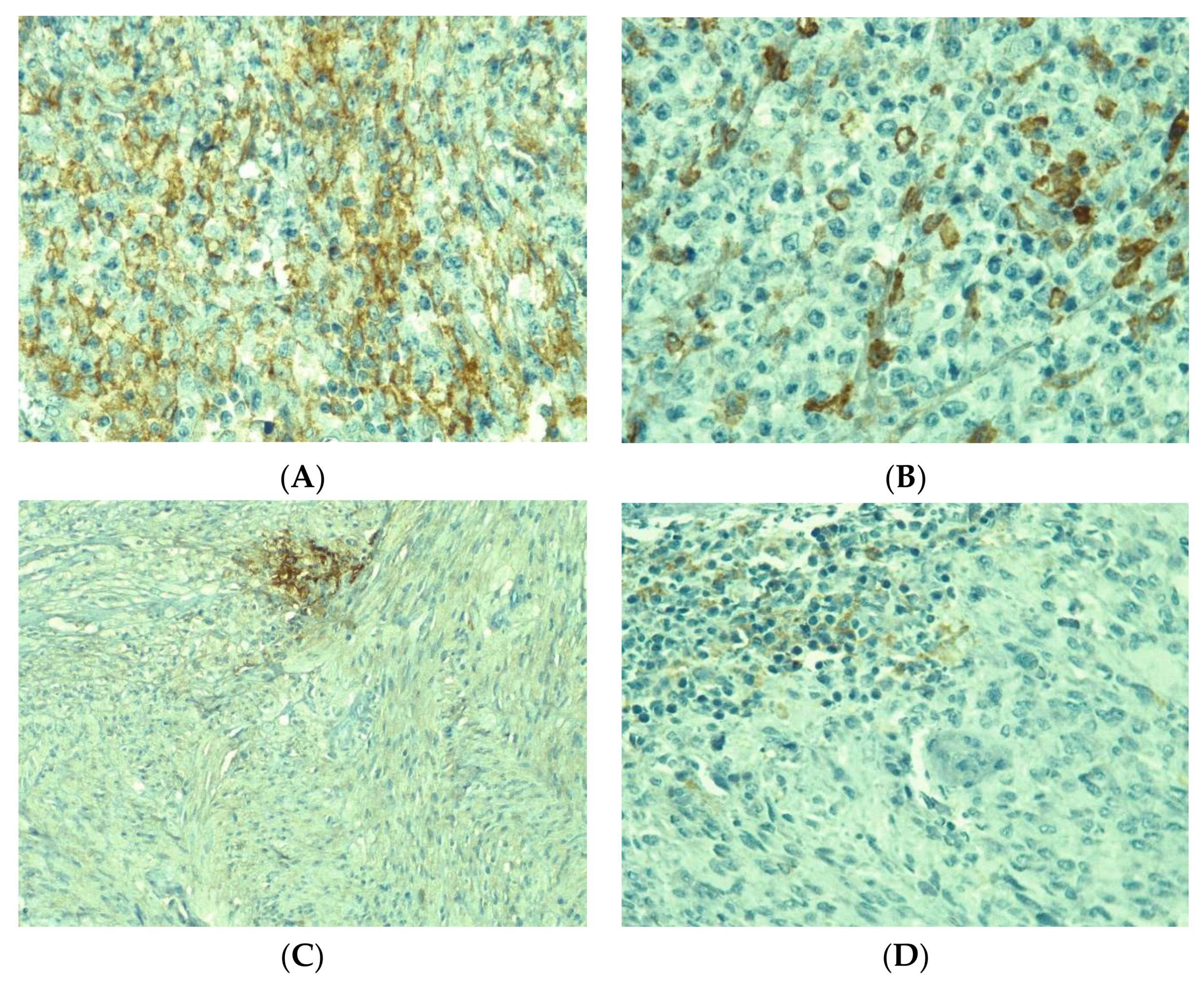
3.2. PD-L1 Expression
3.3. Immune Cells
3.4. Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akahoshi, K.; Oya, M.; Koga, T.; Shiratsuchi, Y. Current clinical management of gastrointestinal stromal tumor. World J. Gastroenterol. 2018, 24, 2806–2817. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-J.; Zhang, Z.-Z.; Xu, J.; Wang, M.; Zhao, W.-Y.; Tu, L.; Zhuang, C.; Liu, Q.; Shen, Y.-Y.; Cao, H.; et al. SLITRK3 expression correlation to gastrointestinal stromal tumor risk rating and prognosis. World J. Gastroenterol. 2015, 21, 8398–8407. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, N.; Sharma, A.; Iqbal, N. Clinicopathological and treatment analysis of 13 stromal tumors of mesentery and retroperitoneum. Ann. Gastroenterol. 2015, 28, 105–108. [Google Scholar] [PubMed]
- Zhou, J.; Yan, T.; Huang, Z.; Zhao, J.; Bi, X.; Zhao, H.; Zhang, Y.-F.; Cai, J. Clinical features and prognosis of extragastrointestinal stromal tumors. Int. J. Clin. Exp. Med. 2016, 9, 16367–16372. [Google Scholar]
- Feng, F.; Feng, B.; Liu, S.; Liu, Z.; Xu, G.; Guo, M. Clinicopathological features and prognosis of mesenteric gastrointestinal stromal tumor: Evaluation of a pooled case series. Oncotarget 2017, 8, 46514–46522. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fletcher, C.D.; Berman, J.J.; Corless, C.; Gorstein, F.; Lasota, J.; Longley, B.; Miettinen, M.; O’Leary, T.J.; Remotti, H.; Rubin, B.P.; et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum. Pathol. 2002, 33, 459–465. [Google Scholar] [CrossRef] [Green Version]
- Miettinen, M.; Lasota, J. Gastrointestinal stromal tumors: Pathology and prognosis at different sites. Semin. Diagn. Pathol. 2006, 23, 70–83. [Google Scholar] [CrossRef]
- Herlea, V.; Roşulescu, A.; Iorgescu, A.; Dima, S.O.; Dumitraşcu, T.; Braşoveanu, V.; Stroescu, C.; Vasilescu, C.; Popescu, I. The Immune Response in Gastrointestinal Stromal Tumors. J. Cancer Res. Immunooncol. 2020, 6, 125. [Google Scholar]
- Mansuri, N.; Birkman, E.M.; Heuser, V.D.; Lintunen, M.; Algars, A.; Sundstrom, J.; Ristamäki, R.; Lehtinen, L.; Carpén, O. Association of tumor-infiltrating T lymphocytes with intestinal-type gastric cancer molecular subtypes and outcome. Virchows Archiv. 2021, 478, 707–717. [Google Scholar] [CrossRef]
- Stanton, S.E.; Adams, S.; Disis, M.L. Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: A systematic review. JAMA Oncol. 2016, 2, 1354–1360. [Google Scholar] [CrossRef]
- Van Dongen, M.; Savage, N.D.; Jordanova, E.S.; Briaire-de Bruijn, I.H.; Walburg, K.V.; Ottenhoff, T.H.; Hogendoorn, P.C.W.; van der Burg, S.H.; Gelderblom, H.; van Hall, T. Anti-inflammatory M2 type macrophages characterize metastasized and tyrosine kinase inhibitor-treated gastrointestinal stromal tumors. Int. J. Cancer. 2010, 127, 899–909. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Garcia-Buitrago, M.T.; Trent, J.C.; Rosenberg, A.E. The immune system and gastrointestinal stromal tumor: A wealth of opportunities. Curr. Opin. Oncol. 2015, 27, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Däster, S.; Eppenberger-Castori, S.; Mele, V.; Schäfer, H.M.; Schmid, L.; Weixler, B.; Soysal, S.D.; Droeser, R.A.; Spagnoli, G.C.; Kettelhack, C.; et al. Low Expression of Programmed Death 1 (PD-1), PD-1 Ligand1 (PD-L1), and low CD8+ T Lymphocyte Infiltration Identify a Subgroup of Patients with Gastric and Esophageal Adenocarcinoma with Severe Prognosis. Front. Med. 2020, 7, 144. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Ericsson, P.I.; Stovgaard, E.S.; Sua, L.F.; Reisenbichler, E.; Kos, Z.; Carter, J.M.; Michiels, S.; Le Quesne, J.; Nielsen, T.O.; Lænkholm, A.-V. International Immuno-Oncology Biomarker Working Group. The path to a better biomarker: Application of a risk management framework for the implementation of PD-L1 and TILs as immuno-oncology biomarkers into breast cancer clinical trials and daily practice. J. Pathol. 2020, 250, 667–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lien, H.C.; Lee, Y.H.; Chen, I.C.; Lin, C.H.; Chen, T.W.; Lu, Y.T.; Lu, Y.S. Tumor-infiltrating lymphocyte abundance and programmed death-ligand 1 expression in metaplastic breats carcinoma: Implications for distinct immune microenvironments in different metaplastic components. Virchows Archiv. 2021, 478, 669–678. [Google Scholar] [CrossRef] [PubMed]
- Kulangara, K.; Zhang, N.; Corigliano, E.; Guerrero, L.; Waldroup, S.; Jaiswal, D.; Ms, M.J.; Shah, S.; Hanks, D.; Wang, J.; et al. Clinical Utility of the Combined Positive Score for Programmed Death Ligand-1 Expression and the Approval of Pembrolizumab for Treatment of Gastric Cancer. Arch. Pathol. Lab. Med. 2019, 143, 330–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, M.A.; Ramos, M.F.K.P.; Dias, A.R.; Ribeiro, R.; Cardili, L.; Zilberstein, B. Scoring systems for PD-L1 expression and their prognostic impact in patients with resectable gastric cancer. Virchows Arch. 2021, 478, 1039–1048. [Google Scholar] [CrossRef]
- Gallo, G.; Vescio, G.; de Paola, G.; Sammarco, G. Therapeutic Targets and Tumor Microenvironment in Colorectal Cancer. J. Clin. Med. 2021, 10, 2295. [Google Scholar] [CrossRef]
- Ju, X.; Zhang, H.; Zhou, Z.; Wang, Q. Regulation of PD-L1 expression in cancer and clinical implications in immunotherapy. Am. J. Cancer Res. 2020, 10, 1–11. [Google Scholar]
- Chae, Y.K.; Pan, A.; Davis, A.A.; Raparia, K.; Mohindra, N.A.; Matsangou, M.; Giles, F.J. Biomarkers for PD-1/PD-L1 Blockade Therapy in Non-Small-cell Lung Cancer: Is PD-L1 Expression a Good Marker for Patient Selection? Clin. Lung Cancer 2016, 17, 350–361. [Google Scholar] [CrossRef]
- Carbognin, L.; Pilotto, S.; Milella, M.; Vaccaro, V.; Brunelli, M.; Caliò, A.; Cuppone, F.; Sperduti, I.; Giannarelli, D.; Chilosi, M.; et al. Differential Activity of Nivolumab, Pembrolizumab and MPDL3280A according to the Tumor Expression of Programmed Death-Ligand-1 (PD-L1): Sensitivity Analysis of Trials in Melanoma, Lung and Genitourinary Cancers. PLoS ONE 2015, 10, e0130142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, R.; Song, Y.; Wang, Y.; Huang, Y.; Li, Z.; Cui, Y.; Yi, M.; Xia, L.; Zhuang, W.; Wu, X.; et al. PD-1/PD-L1 blockade rescue exhausted CD8+ T cells in gastrointestinal stromal tumours via the PI3K/Akt/mTOR signalling pathway. Cell Prolif. 2019, 52, e12571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bertucci, F.; Finetti, P.; Mamessier, E.; Pantaleo, M.A.; Astolfi, A.; Ostrowski, J.; Birnbaum, D. PDL1 expression is an independent prognostic factor in localized GIST. OncoImmunology 2015, 4, 8. [Google Scholar] [CrossRef] [Green Version]
- Seifert, A.M.; Zeng, S.; Zhang, J.Q.; Kim, T.S.; Cohen, N.A.; Beckman, M.J.; Medina, B.D.; Maltbaek, J.H.; Loo, J.K.; DeMatteo, R.P.; et al. PD-1/PD-L1 Blockade Enhances T-cell Activity and Antitumor Efficacy of Imatinib in Gastrointestinal Stromal Tumors. Clin. Cancer Res. 2017, 23, 454–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoemig-Markiefka, B.; Eschbach, J.; Scheel, A.H.; Pamuk, A.; Rueschoff, J.; Zander, T.; Buettner, R.; Schroeder, W.; Bruns, C.J.; Loeser, H.; et al. Optimized PD-L1 scoring of gastric cancer. Gastric Cancer 2021, 24, 1115–1122. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Sun, J.; Yuan, W.; Gao, X.; Fu, M.; Xue, A.; Li, H.; Shu, P.; Fang, Y.; Hou, Y.; et al. Immune Cell Infiltration and the Expression of PD-1 and PD-L1 in Primary PDGFRA-Mutant Gastrointestinal Stromal Tumors. J. Gastrointest. Surg. 2021, 25, 2091–2100. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Ding, J.; Cheng, X.; Xiong, M. Hypoxia-Related Gene-Based Signature Can Evaluate the Tumor Immune Microenvironment and Predict the Prognosis of Colon Adenocarcinoma Patients. Int. J. Gen. Med. 2021, 14, 9853–9862. [Google Scholar] [CrossRef]
- Pantaleo, M.A.; Tarantino, G.; Agostinelli, C.; Urbini, M.; Nannini, M.; Saponara, M.; Castelli, C.; Stacchiotti, S.; Fumagalli, E.; Gatto, L. Immune microenvironment profiling of gastrointestinal stromal tumors (GIST) shows gene expression patterns associated to immune checkpoint inhibitors response. OncoImmunology 2019, 8, e1617588. [Google Scholar] [CrossRef] [Green Version]
- Cameron, S.; Gieselmann, M.; Blaschke, M.; Ramadori, G.; Fuzesi, L. Immune cells in primary and metastatic gastrointestinal stromal tumors (GIST). Int. J. Clin. Exp. Pathol. 2014, 7, 3563–3579. [Google Scholar]
- Wang, J.; Ren, H.; Wu, W.; Zeng, Q.; Chen, J.; Han, J.; Lin, M.; Zhang, C.; He, Y.; Lee, M. Immune Infiltration, Cancer Stemness, and Targeted Therapy in Gastrointestinal Stromal Tumor. Front. Immunol. 2021, 12, 691713. [Google Scholar] [CrossRef]
- Poveda, A.; del Muro, X.G.; López-Guerrero, J.A.; Cubedo, R.; Martínez, V.; Romero, I.; Serrano, C.; Valverde, C.; Martín-Broto, J. GEIS guidelines for gastrointestinal sarcomas (GIST). Cancer Treat. Rev. 2017, 55, 107–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siozopoulou, V.; Domen, A.; Zwaenepoel, K.; van Beeck, A.; Smits, E.; Pauwels, P.; Marcq, E. Immune Checkpoint Inhibitory Therapy in Sarcomas: Is There Light at the End of the Tunnel? Cancers 2021, 13, 360. [Google Scholar] [CrossRef] [PubMed]
- Fudalej, M.M.; Badowska-Kozakiewicz, A.M. Improved understanding of gastrointestinal stromal tumors biology as a step for developing new diagnostic and therapeutic schemes. Oncol. Lett. 2021, 21, 417. [Google Scholar] [CrossRef] [PubMed]





| Antibody | Dilution | Clone | Producer |
|---|---|---|---|
| PD-L1 | 1:50 | ZR3 | Cell Marque (USA) |
| Ki67 | 1:250 | SP6 | Cell Marque (USA) |
| CD3 | Ready to use | MRQ-39 | Cell Marque (USA) |
| CD20 | 1:250 | L26 | Cell Marque (USA) |
| CD4 | 1:50 | SP35 | Cell Marque (USA) |
| CD8 | 1:50 | C8/144B | Cell Marque (USA) |
| CD68 | 1:250 | Kp-1 | Cell Marque (USA) |
| Patient Characteristic | N (%) |
|---|---|
| Age, mean (sd) | 57.8 (11.4) |
| Gender | |
| Female | 29 (44.6) |
| Male | 36 (55.4) |
| Tumor location | |
| Colon | 2 (3.1) |
| Small bowel | 11 (16.9) |
| Gastric | 30 (46.1) |
| Rectum | 2 (3.1) |
| EGIST | 7 (10.8) |
| Local recurrence | 6 (9.2) |
| Metastasis | 7 (10.8) |
| Tumor dimension (cm), mean (sd) | 7.1 (4.8) |
| Colon | 10 (2.8) |
| Small bowel | 5.0 (2.8) |
| Gastric | 7.2 (5.0) |
| Rectum | 5.2 (6.7) |
| EGIST | 9 (6.3) |
| Local recurrence | 8.7 (3.0) |
| Metastasis | 6.5 (6.1) |
| Risk of disease progression | |
| Very low | 5 (9.8) |
| Low | 24 (47.1) |
| Moderate | 6 (11.8) |
| High | 16 (31.4) |
| Mitotic rate | |
| ≤5/50 HPFs | 39 (60.9) |
| >5/50 HPFs | 25 (39.1) |
| Cell type | |
| Spindle | 41 (63.1) |
| Epithelioid | 3 (4.6) |
| Mixed | 21 (32.3) |
| CD117 | |
| Negative | 5 (7.7) |
| Positive | 60 (92.3) |
| Ki67 (range) | 1–75 |
| <50% | 59 (90.8) |
| ≥50% | 6 (9.2) |
| PD-L1 CPS | p | ||||
|---|---|---|---|---|---|
| Location of the Tumor N (%) | ≤1 24 (36.9) | 2–10 17 (26.1) | 11–50 12 (18.5) | >50 12 (18.5) | |
| Colon | 2 (100) | 0 | 0 | 0 | 0.586 |
| Small bowel | 5 (45.3) | 2 (18.9) | 2 (18.9) | 2 (18.9) | |
| Gastric | 9 (30.0) | 9 (30.0) | 4 (13.3) | 8 (26.7) | |
| Rectum | 1 (50.0) | 0 | 0 | 1 (50.0) | |
| EGIST | 3 (42.9) | 3 (42.9) | 1 (14.2) | 0 | |
| Local recurrence | 1 (16.7) | 1 (16.7) | 3 (50.0) | 1 (16.7) | |
| Metastasis | 3 (42.8) | 2 (28.6) | 2 (28.6) | 0 | |
| Recurrence | |||||
| No | 19 (33.9) | 14 (25.0) | 11 (19.6) | 12 (21.5) | 0.331 |
| Yes | 5 (55.6) | 3 (33.3) | 1 (11.1) | 0 | |
| Metastasis | |||||
| No | 19 (39.7) | 11 (22.9) | 9 (18.7) | 9 (18.7) | 0.776 |
| Yes | 5 (29.5) | 6 (35.3) | 3 (17.6) | 3 (17.6) | |
| Factors | Negative PDL-1 | Positive PDL-1 | p * |
|---|---|---|---|
| Sex, N(%) | |||
| Females | 11 (37.9) | 18 (62.1) | 0.796 |
| Males | 12 (33.3) | 24 (66.7) | |
| Age | |||
| Mean ± sd | 54.3 ± 10.7 | 59.7 ± 11.4 | 0.068 ** |
| Median (range) | 57 (35–72) | 62 (28–78) | |
| Tumor size, N (%) | |||
| ≤5 cm | 10 (31.2) | 22 (68.8) | 0.606 |
| >5 cm | 13 (39.4) | 20 (60.6) | |
| Cell type, N (%) | |||
| Epithelioid and mixed | 8 (33.3) | 16 (66.7) | 1.000 |
| Spindle | 15 (36.6) | 26 (63.4) | |
| Mitotic rate, N (%) | |||
| ≤5 | 15 (38.5) | 24 (61.5) | 0.431 |
| >5 | 7 (28.0) | 18 (72.0) | |
| Risk of disease progression, N (%) | |||
| Very low and Low | 12 (41.4) | 17 (58.6) | 0.566 |
| Intermediate and High | 7 (37.2) | 15 (62.8) | |
| Cell Type (n = 65) | PDL-1 Negative (n = 23) | PDL-1 Positive (n = 42) | p * | All Patients |
|---|---|---|---|---|
| Median(range)-No.of cells/HPF | ||||
| CD3 | 21 (3–95) | 37 (5–217) | 0.032 | 31 (3–217) |
| CD4 | 28 (3–109) | 41.5 (0–119) | 0.091 | 36 (0–119) |
| CD8 | 13 (0–119) | 23 (4–161) | 0.066 | 19 (0–161) |
| CD20 | 7 (0–230) | 15 (0–168) | 0.051 | 13 (0–230) |
| CD68 | 21 (2–80) | 38 (2–222) | 0.008 | 34 (2–222) |
| H&E | 124 (31–460) | 172.5 (42–729) | 0.011 | 148 (31–729) |
| N (%) | No. Events | Median OS | p * | |
|---|---|---|---|---|
| Gender | ||||
| Female | 29 (44.6) | 9 | 48 | 0.711 |
| Male | 36 (55.4) | 10 | 36 | |
| PDL-1 | ||||
| Negative | 23 (35.4) | 8 | 36 | 0.492 |
| Positive | 42 (64.6) | 11 | 48 | |
| KI67 | ||||
| <50 | 59 (90.8) | 15 | 48 | 0.008 |
| ≥50 | 6 (9.2) | 4 | 22 | |
| Multifocal tumor | ||||
| No | 48 (73.8) | 8 | 48 | 0.0001 |
| Yes | 17 (26.1) | 11 | 25 | |
| Location of the tumor | ||||
| Colon | 2 (3.1) | 0 | 42 | 0.301 |
| Small bowel | 11 (16.9) | 4 | 60 | |
| Stomach | 30 (46.1) | 8 | 36 | |
| Rectum | 2 (3.1) | 1 | 18.5 | |
| EGIST | 7 (10.8) | 4 | 25 | |
| Recurrences | 6 (9.2) | 1 | 66 | |
| Metastases | 7 (10.8) | 1 | 60 |
| Factors | HR (95% CI) | p-Value * |
|---|---|---|
| Risk of disease progression Very low and Low Intermediate and High | Reference 4.46 (0.64–30.90) | 0.130 |
| Tumor size ≤5 cm >5 cm | Reference 2.30 (0.33–16.08) | 0.400 |
| PDL-1 Negative Positive | Reference 0.71 (0.21–2.38) | 0.579 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herlea, V.; Roșulescu, A.; Calotă, V.C.; Croitoru, V.; Stoica Mustafa, E.; Vasilescu, C.; Alexandrescu, S.; Dumitrașcu, T.; Popescu, I.; Dima, S.O.; et al. Combined Positive Score for Programmed Death Ligand-1 Expression and Inflammatory Microenvironment in Gastrointestinal Stromal Tumors. Medicina 2022, 58, 174. https://doi.org/10.3390/medicina58020174
Herlea V, Roșulescu A, Calotă VC, Croitoru V, Stoica Mustafa E, Vasilescu C, Alexandrescu S, Dumitrașcu T, Popescu I, Dima SO, et al. Combined Positive Score for Programmed Death Ligand-1 Expression and Inflammatory Microenvironment in Gastrointestinal Stromal Tumors. Medicina. 2022; 58(2):174. https://doi.org/10.3390/medicina58020174
Chicago/Turabian StyleHerlea, Vlad, Alexandra Roșulescu, Violeta Claudia Calotă, Vlad Croitoru, Elena Stoica Mustafa, Cătălin Vasilescu, Sorin Alexandrescu, Traian Dumitrașcu, Irinel Popescu, Simona Olimpia Dima, and et al. 2022. "Combined Positive Score for Programmed Death Ligand-1 Expression and Inflammatory Microenvironment in Gastrointestinal Stromal Tumors" Medicina 58, no. 2: 174. https://doi.org/10.3390/medicina58020174
APA StyleHerlea, V., Roșulescu, A., Calotă, V. C., Croitoru, V., Stoica Mustafa, E., Vasilescu, C., Alexandrescu, S., Dumitrașcu, T., Popescu, I., Dima, S. O., & Sajin, M. (2022). Combined Positive Score for Programmed Death Ligand-1 Expression and Inflammatory Microenvironment in Gastrointestinal Stromal Tumors. Medicina, 58(2), 174. https://doi.org/10.3390/medicina58020174







