The Feasibility of a Machine Learning Approach in Predicting Successful Ventilator Mode Shifting for Adult Patients in the Medical Intensive Care Unit
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.1.1. Data Source
2.1.2. Participants
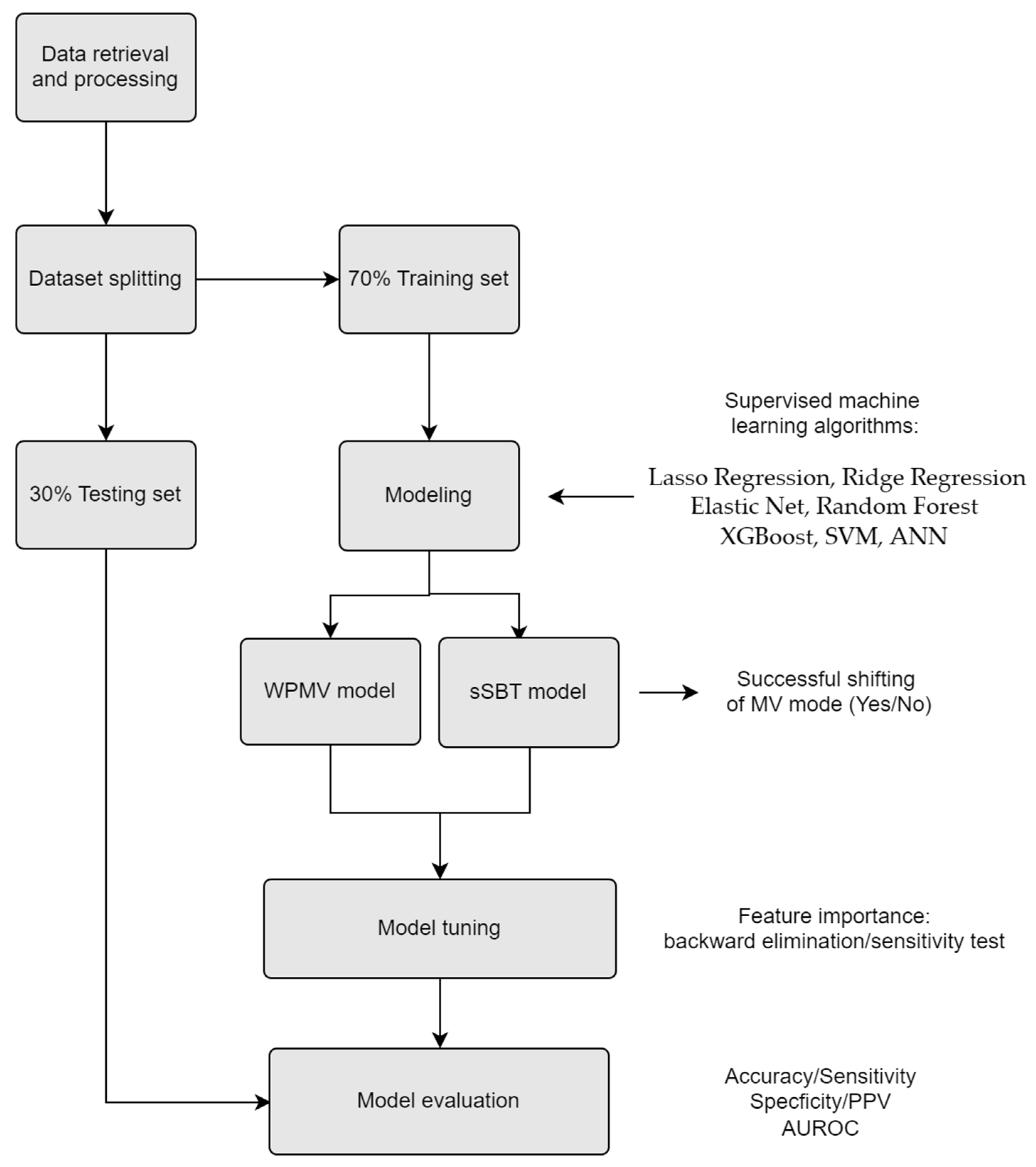
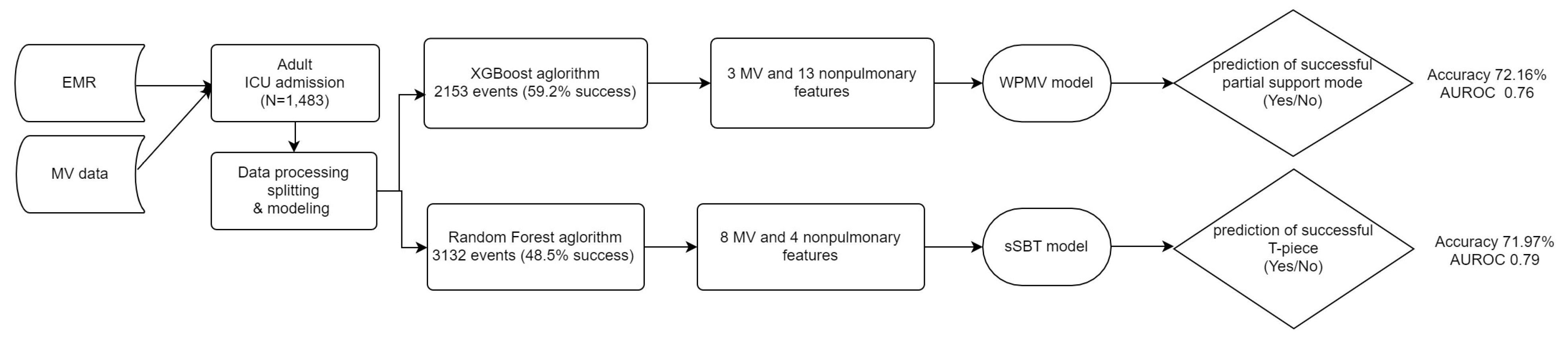
2.2. Predicting Models
Outcomes
2.3. Candidate Predictors
2.4. Missing Data
2.5. Data Mining
2.6. Modeling
3. Results
3.1. Participants and Outcomes
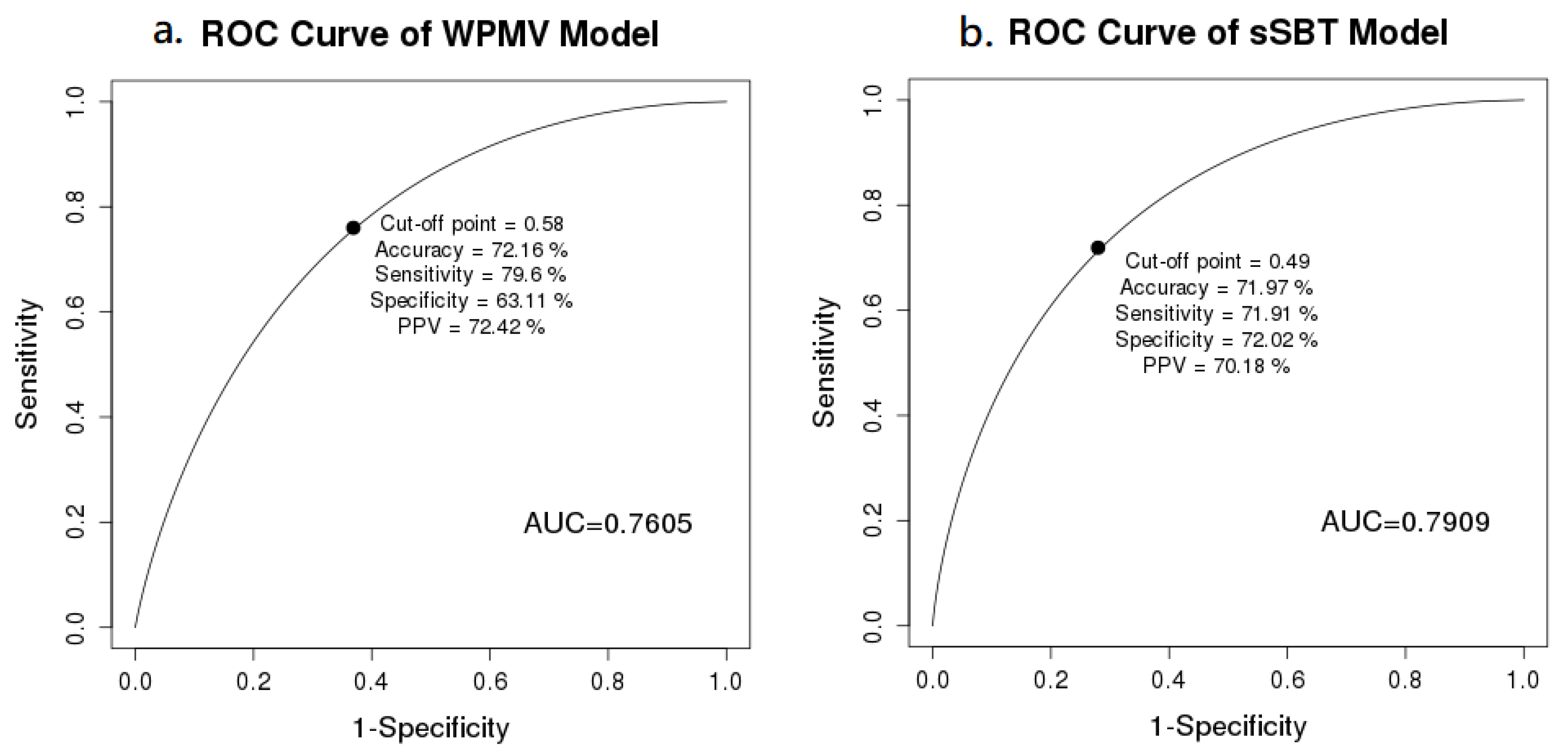
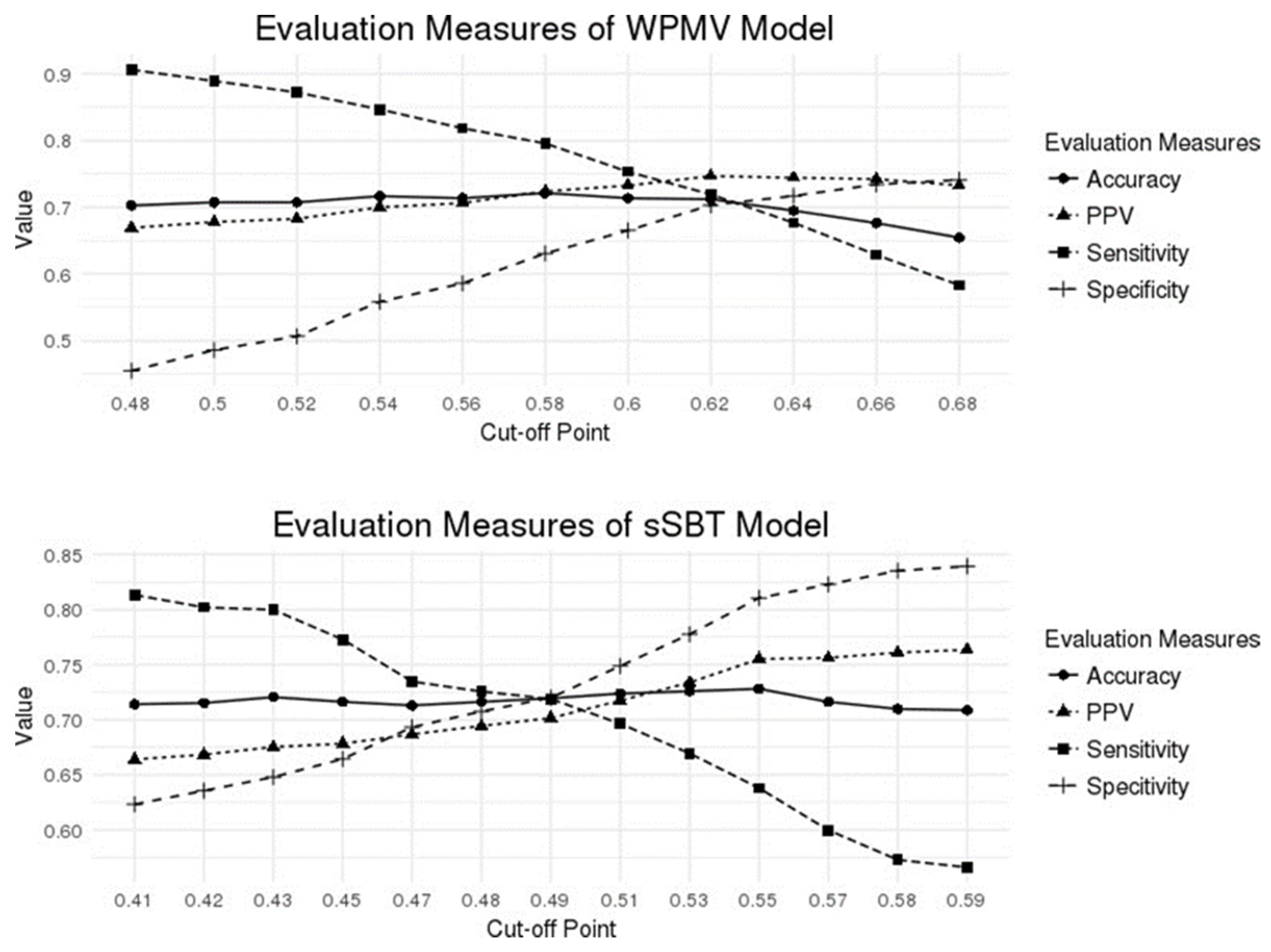
3.2. Model Performance
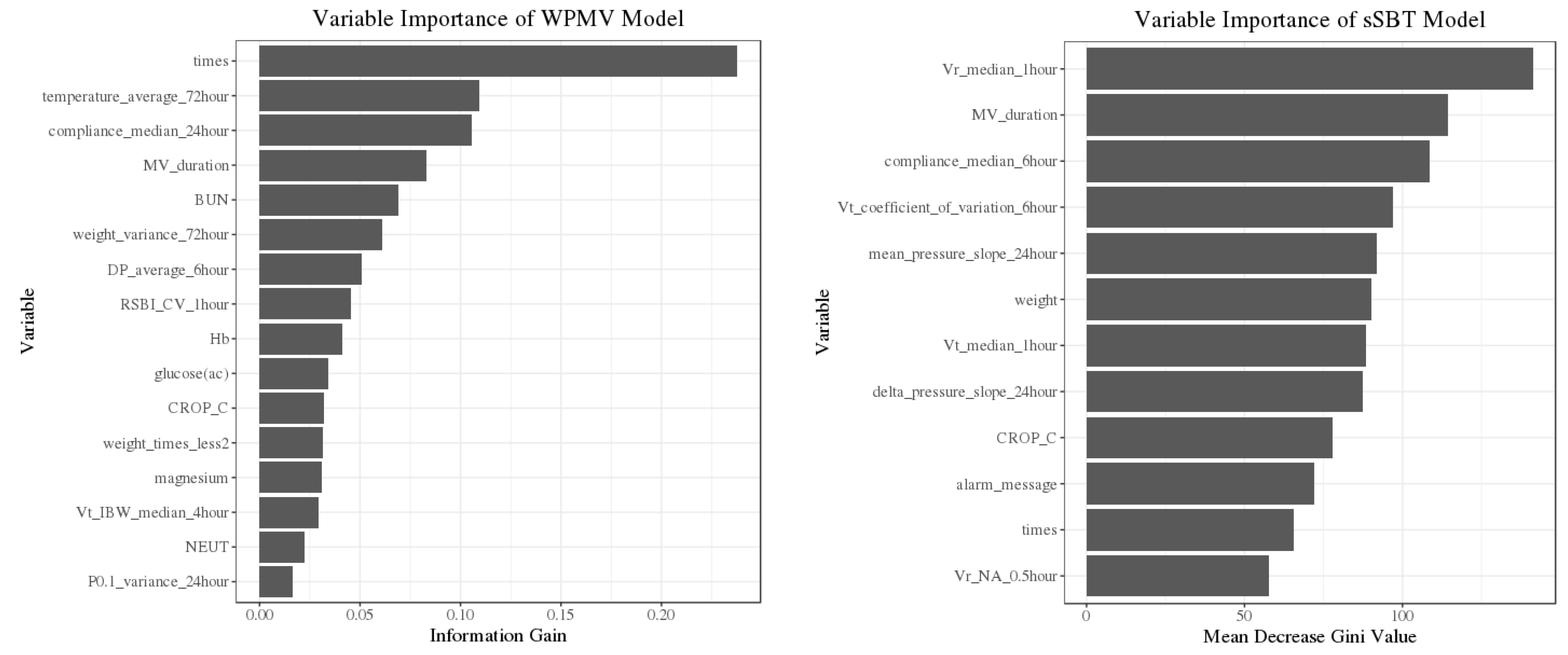
3.3. Predictor Importance
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jaber, S.; Chanques, G.; Matecki, S.; Ramonatxo, M.; Vergne, C.; Souche, B.; Perrigault, P.F.; Eledjam, J.J. Post-extubation stridor in intensive care unit patients. Risk factors evaluation and importance of the cuff-leak test. Intensive Care Med. 2003, 29, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Sue, R.D.; Susanto, I. Long-term complications of artificial airways. Clin. Chest Med. 2003, 24, 457–471. [Google Scholar] [CrossRef]
- Carden, K.A.; Boiselle, P.M.; Waltz, D.A.; Ernst, A. Tracheomalacia and tracheobronchomalacia in children and adults: An in-depth review. Chest 2005, 127, 984–1005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, A.-C.; Cheng, K.-C.; Chen, C.-M.; Hsing, S.-C.; Sung, M.-Y. The outcome and predictors of failed extubation in intensive care patients—The elderly is an important predictor. Int. J. Gerontol. 2011, 5, 206–211. [Google Scholar] [CrossRef] [Green Version]
- Yang, K.L.; Tobin, M.J. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. New Engl. J. Med. 1991, 324, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Boles, J.M.; Bion, J.; Connors, A.; Herridge, M.; Marsh, B.; Melot, C.; Pearl, R.; Silverman, H.; Stanchina, M.; Vieillard-Baron, A.; et al. Weaning from mechanical ventilation. Eur. Respir. J. 2007, 29, 1033–1056. [Google Scholar] [CrossRef]
- Heunks, L.M.; van der Hoeven, J.G. Clinical review: The ABC of weaning failure--a structured approach. Crit. Care 2010, 14, 245. [Google Scholar] [CrossRef] [Green Version]
- Kuo, H.J.; Chiu, H.W.; Lee, C.N.; Chen, T.T.; Chang, C.C.; Bien, M.Y. Improvement in the Prediction of Ventilator Weaning Outcomes by an Artificial Neural Network in a Medical ICU. Respir. Care 2015, 60, 1560–1569. [Google Scholar] [CrossRef] [Green Version]
- Kwong, M.T.; Colopy, G.W.; Weber, A.M.; Ercole, A.; Bergmann, J.H. The efficacy and effectiveness of machine learning for weaning in mechanically ventilated patients at the intensive care unit: A systematic review. Bio-Des. Manuf. 2019, 2, 31–40. [Google Scholar] [CrossRef] [Green Version]
- Todorova, L.; Temelkov, A. Weaning from long-term mechanical ventilation: A nonpulmonary weaning index. J. Clin. Monit. Comput. 2004, 18, 275–281. [Google Scholar] [CrossRef]
- Wu, Y.K.; Kao, K.C.; Hsu, K.H.; Hsieh, M.J.; Tsai, Y.H. Predictors of successful weaning from prolonged mechanical ventilation in Taiwan. Respir. Med. 2009, 103, 1189–1195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Datta, D.; Foley, R.; Wu, R.; Grady, J.; Scalise, P. Can creatinine height index predict weaning and survival outcomes in patients on prolonged mechanical ventilation after critical illness? J. Intensive Care Med. 2018, 33, 104–110. [Google Scholar] [CrossRef]
- Esteban, A.; AlÍa, I.; Tobin, M.J.; Gil, A.; Gordo, F.; VallverdÚ, I.; Blanch, L.; Bonet, A.; VÁzquez, A.; de PABLO, R. Effect of spontaneous breathing trial duration on outcome of attempts to discontinue mechanical ventilation. Am. J. Respir. Crit. Care Med. 1999, 159, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.; Guyatt, G.; Cook, D.; Griffith, L.; Sinuff, T.; Kergl, C.; Mancebo, J.; Esteban, A.; Epstein, S. Predicting success in weaning from mechanical ventilation. Chest 2001, 120, 400S–424S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, M.H.; Hsieh, M.J.; Cheng, A.C.; Chen, C.M.; Hsieh, C.C.; Chao, C.M.; Lai, C.C.; Cheng, K.C.; Chou, W. Predicting weaning difficulty for planned extubation patients with an artificial neural network. Medicine 2019, 98, e17392. [Google Scholar] [CrossRef] [PubMed]
- Giraldo, B.; Garde, A.; Arizmendi, C.; Jane, R.; Benito, S.; Diaz, I.; Ballesteros, D. Support vector machine classification applied on weaning trials patients. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2006, 2006, 5587–5590. [Google Scholar] [CrossRef] [PubMed]
- Garde, A.; Schroeder, R.; Voss, A.; Caminal, P.; Benito, S.; Giraldo, B.F. Patients on weaning trials classified with support vector machines. Physiol. Meas. 2010, 31, 979–993. [Google Scholar] [CrossRef]
- Beduneau, G.; Pham, T.; Schortgen, F.; Piquilloud, L.; Zogheib, E.; Jonas, M.; Grelon, F.; Runge, I.; Nicolas, T.; Grange, S.; et al. Epidemiology of Weaning Outcome according to a New Definition. The WIND Study. Am. J. Respir. Crit. Care Med. 2017, 195, 772–783. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM Sigkdd International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Epstein, C.D.; Peerless, J.R. Weaning readiness and fluid balance in older critically ill surgical patients. Am. J. Crit. Care 2006, 15, 54–64. [Google Scholar] [CrossRef]
- Vieira, J.M., Jr.; Castro, I.; Curvello-Neto, A.; Demarzo, S.; Caruso, P.; Pastore, L., Jr.; Imanishe, M.H.; Abdulkader, R.C.; Deheinzelin, D. Effect of acute kidney injury on weaning from mechanical ventilation in critically ill patients. Crit. Care Med. 2007, 35, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.-C.; Ruan, S.-Y.; Huang, C.-T.; Kuo, P.-H.; Yu, C.-J. Hemoglobin levels and weaning outcome of mechanical ventilation in difficult-to-wean patients: A retrospective cohort study. PLoS ONE 2013, 8, e73743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, Y.-L.; Perrodeau, E.; Guidet, B.; Trinquart, L.; Richard, J.-C.M.; Mercat, A.; Jolliet, P.; Ravaud, P.; Brochard, L. Mechanical ventilation and clinical practice heterogeneity in intensive care units: A multicenter case-vignette study. Ann. Intensive Care 2014, 4, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Category | Candidate Predictors (Abbreviation Used throughout This Study) | Range of the Outliers (Unit) |
|---|---|---|
| Ventilator information | Tidal Volume (Vt) | Vt < 1 or Vt > 1260 (mL) |
| Ventilation Rate (Vr) | Vr < 1 or Vr > 50 (breath per minute) | |
| airway occlusion pressure (P0.1) | nil | |
| Dynamic Compliance | nil | |
| Mean Pressure | mean_pressure < 0.1 or >28.2 (cm H2O) | |
| Resistance | Resistance < 0 or >30 (cm H2O/L/s) | |
| fraction of inspired oxygen (FiO2) | FiO2 < 21% or FiO2 > 100% | |
| positive end expiratory pressure (PEEP) | nil | |
| alveolar oxygen partial pressure (PAO2) | nil | |
| number of transitions from full to partial-support mode during weaning (numbers of WPMV) | nil | |
| numbers of transitions from partial-support mode to full-support mode or T-P during weaning (numbers of SBT) | nil | |
| Accumulated total time of using mechanical ventilator (MV_duration) | nil | |
| Numbers of alarm message per minute on MV (alarm_message) | nil | |
| Arterial Blood Gas | Arterial carbon dioxide partial pressure (PaCO2) | nil |
| arterial oxygen partial pressure (PaO2) | PaO2 < 23.1 or >480 (mmHg) | |
| arterial oxygen saturation (SaO2) | SaO2 < 39.7 or >100 (%) | |
| base excess (BE) | BE < −27.7 or BE ≥ 93.5 (mEq/L) | |
| potential of hydrogen (pH) | nil | |
| Laboratory data | Albumin, Blood Urea Nitrogen (BUN) | nil |
| Creatinine | nil | |
| Glucose | nil | |
| Hemoglobin (Hb) | nil | |
| white blood cell (WBC) | nil | |
| differential count: Neutrophil (NEUT) | nil | |
| Vital Sign | Glasgow Coma Scale (GCS) | GCS < 3 or GCS > 15 |
| Diastolic Blood Pressure (DP) | DP ≤ 0 or DP ≥ 150 (mmHg) | |
| Systolic Blood Pressure (SP) | SP ≤ 0 or SP ≥ 268 (mmHg) | |
| Pulse | Pulse < 30 or > 235 (beat per minute) | |
| Temperature | Temperature < 32 or >42 (°C) | |
| Demographic data | Age | nil |
| Gender | nil | |
| Patient’s weight (weight) | nil |
| Characteristic | Statistical Analysis |
| General | |
| Gender | |
| male | 927 (62.5%) |
| female | 556 (37.5%) |
| Age | 66.88 ± 15.42 |
| APACHE II score | 21 (17–27) |
| In-ICU days | 7 (3–12) |
| MV day | 3.91 (1.67–8.73) |
| Count of shifting between full mode and partial mode | 1 (1–2) |
| Count of shifting between partial mode and SBT | 1 (1–2) |
| Diagnostics/Diseases | |
| Cause of respiratory failure | |
| Pulmonary edema | 18 (1.2%) |
| Systolic congestive heart failure | 460 (29.6%) |
| Acute myocardial infraction | 63 (4.0%) |
| Chronic obstructive pulmonary disease | 43 (2.8%) |
| Asthma | 33 (2.1%) |
| Pneumonia | 289 (18.6%) |
| Bronchopneumonia | 20 (1.3%) |
| Urinary tract infection | 77 (4.9%) |
| Sepsis | 505 (32.5%) |
| Toxicity of carbon monoxide | 40 (2.6%) |
| Comorbidity | |
| Diabetes mellitus | 368 (23.7%) |
| Brain related (infarction/hemorrhage) | 501 (32.2%) |
| Kidney related (ESRD, acute/chronic kidney disease) | 149 (9.6%) |
| Liver related (alcoholic cirrhosis, HBV/HCV cirrhosis) | 95 (6.1%) |
| Lung related (tuberculosis) | 2 (0.1%) |
| Malignancy (all types) | 133 (8.5%) |
| Predictors (Unit) | Successful Event | Unsuccessful Event | p-Value |
|---|---|---|---|
| WPMV model | |||
| Numbers of WPMV (count) | 1 (1–2) | 2 (1–4) | <0.01 |
| temperature_average_72hour (°C) | 36.99 ± 0.61 | 37.15 ± 0.65 | <0.01 |
| compliance_median_24hour (mL/cm H2O) M | 52.65 ± 28.20 | 43.37 ± 24.41 | <0.01 |
| MV_duration (hour) | 48.0 (21.1–98.6) | 88.49 (40.4–164.2) | <0.01 |
| Blood Urea Nitrogen (mg/dL) | 38.70 ± 32.24 | 47.87 ± 34.03 | <0.01 |
| weight_variance_72hour (kg) | 0.15 ± 2.67 | 0.03 ± 0.15 | 0.357 |
| DiastoicPressure_average_6hour (mmHg) | 67.50 ± 11.95 | 65.67 ± 12.07 | <0.01 |
| RSBI_CV_1hour (breaths/min/mL) M | 0.66 ± 0.43 | 0.72 ± 0.47 | 0.017 |
| Hemoglobin (g/dL) | 10.47 ± 2.00 | 10.33 ± 1.94 | 0.137 |
| Glucose (mg/dL) | 166.27 ± 87.57 | 166.31 ± 103.31 | 0.995 |
| CROP_C | 0.02 ± 0.02 | 0.01 ± 0.02 | 0.01 |
| numbers of weight records < 2 before partial mode (%) | 212 (16.6) | 103 (11.7) | 0.002 |
| magnesium (mg/dL) | 2.14 ± 0.48 | 2.19 ± 0.47 | 0.076 |
| Vt_weight_median_4hour (mL/kg) M | 8.39 ± 1.88 | 8.50 ± 2.18 | 0.256 |
| Neutrophil (%) | 80.62 ± 10.66 | 80.33 ± 10.53 | 0.5598 |
| P0.1_variance_24hour (cm H2O) M | 1.08 ± 3.78 | 2.25 ± 12.16 | 0.136 |
| sSBT model | |||
| Vr_median_1hour (breaths/min) M | 19.85 ± 8.00 | 21.07 ± 10.49 | 0.002 |
| MV_duration (hour) | 49.08 (20.0–109.2) | 79.14 (35.2–154.2) | <0.01 |
| compliance_median_6hour (mL/cm H2O) M | 67.58 ± 39.60 | 59.04 ± 50.17 | <0.01 |
| Vt_CV_6hour (mL) M | 0.40 ± 0.25 | 0.39 ± 0.22 | 0.253 |
| mean_pressure_slope_24hour (cm H2O) M | −0.00 ± 0.01 | 0.00 ± 0.04 | 0.183 |
| weight (kg) | 60.87 ± 14.19 | 61.08 ± 14.44 | 0.69 |
| Vt_median_1hour (mL) M | 415.93 ± 186.20 | 417.13 ± 189.43 | 0.868 |
| delta_pressure_slope_24hour (cm H2O) M | −0.00 ± 0.02 | −0.01 ± 0.18 | 0.1 |
| CROP_C | 0.03 ± 0.08 | 0.02 ± 0.04 | 0.213 |
| alarm_message (count) M | 0 (0–5) | 4 (0–13) | <0.01 |
| Numbers of SBT (count) | 1 (1–2) | 2 (1–3) | <0.01 |
| No Vr change in 0.5hour (%)(Vr_NA_0.5hour = 1) M | 973 (64.0) | 496 (30.8) | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, K.-H.; Tan, M.-C.; Chang, Y.-J.; Lin, C.-W.; Lin, Y.-H.; Chang, T.-M.; Kuo, L.-K. The Feasibility of a Machine Learning Approach in Predicting Successful Ventilator Mode Shifting for Adult Patients in the Medical Intensive Care Unit. Medicina 2022, 58, 360. https://doi.org/10.3390/medicina58030360
Cheng K-H, Tan M-C, Chang Y-J, Lin C-W, Lin Y-H, Chang T-M, Kuo L-K. The Feasibility of a Machine Learning Approach in Predicting Successful Ventilator Mode Shifting for Adult Patients in the Medical Intensive Care Unit. Medicina. 2022; 58(3):360. https://doi.org/10.3390/medicina58030360
Chicago/Turabian StyleCheng, Kuang-Hua, Mei-Chu Tan, Yu-Jen Chang, Cheng-Wei Lin, Yi-Han Lin, Tzu-Min Chang, and Li-Kuo Kuo. 2022. "The Feasibility of a Machine Learning Approach in Predicting Successful Ventilator Mode Shifting for Adult Patients in the Medical Intensive Care Unit" Medicina 58, no. 3: 360. https://doi.org/10.3390/medicina58030360
APA StyleCheng, K.-H., Tan, M.-C., Chang, Y.-J., Lin, C.-W., Lin, Y.-H., Chang, T.-M., & Kuo, L.-K. (2022). The Feasibility of a Machine Learning Approach in Predicting Successful Ventilator Mode Shifting for Adult Patients in the Medical Intensive Care Unit. Medicina, 58(3), 360. https://doi.org/10.3390/medicina58030360






