Impact of COVID-19 Pandemic on the Quality of Life of IBD Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Ethical Aspects
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/who-director-general-s-special-envoys-on-covid-19-preparedness-and-response (accessed on 21 February 2022).
- Available online: https://www.worldometers.info/coronavirus/ (accessed on 21 February 2022).
- Available online: https://www.worldometers.info/coronavirus/coronavirus-death-rate/ (accessed on 21 February 2022).
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef]
- Fekadu, G.; Bekele, F.; Tolossa, T.; Fetensa, G.; Turi, E.; Getachew, M.; Abdisa, E.; Assefa, L.; Afeta, M.; Demisew, W.; et al. Impact of COVID-19 pandemic on chronic diseases care follow-up and current perspectives in low resource settings: A narrative review. Int. J. Physiol. Pathophysiol. Pharmacol. 2021, 13, 86–93. [Google Scholar] [PubMed]
- Kumric, M.; TicinovicKurir, T.; Martinovic, D.; Zivkovic, P.M.; Bozic, J. Impact of the COVID-19 pandemic on inflammatory bowel disease patients: A review of the current evidence. World J. Gastroenterol. 2021, 27, 3748–3761. [Google Scholar] [CrossRef] [PubMed]
- Viganò, C.; Mulinacci, G.; Palermo, A.; Barisani, D.; Pirola, L.; Fichera, M.; Invernizzi, P.; Massironi, S. Impact of COVID-19 on inflammatory bowel disease practice and perspectives for the future. World J. Gastroenterol. 2021, 7, 5520–5535. [Google Scholar] [CrossRef]
- Ungaro, R.C.; Kappelman, M.D.; Rubin, D.T.; Colombel, J.F. COVID-19 and Inflammatory Bowel Disease: Lessons Learned, Practical Recommendations, and Unanswered Questions. Gastroenterology 2021, 160, 1447–1451. [Google Scholar] [CrossRef]
- Lee, J.W.; Song, E.M.; Jung, S.A.; Jung, S.H.; Kim, K.W.; Koh, S.J.; Lee, H.J.; Hong, S.W.; Park, J.H.; Hwang, S.W.; et al. Clinical Course of COVID-19 in Patients with Inflammatory Bowel Disease in Korea: A KASID Multicenter Study. J. Korean Med. Sci. 2021, 36, e336. [Google Scholar] [CrossRef] [PubMed]
- D’amico, F.; Danese, S.; Peyrin-Biroulet, L. Systematic Review on Inflammatory Bowel Disease Patients with Coronavirus Disease 2019: It Is Time to Take Stock. Clin. Gastroenterol. Hepatol. 2020, 18, 2689–2700. [Google Scholar] [CrossRef]
- BSG Expanded Consensus Advice for the Management of IBD during the COVID-19 Pandemic. Available online: https://www.bsg.org.uk/covid-19-advice/bsg-advice-for-management-of-inflammatory-bowel-diseases-during-the-covid-19-pandemic (accessed on 21 February 2022).
- Singh, A.K.; Jena, A.; Kumar, M.P.; Sharma, V.; Sebastian, S. Risk and outcomes of coronavirus disease in patients with inflammatory bowel disease: A systematic review and meta-analysis. UEG J. 2021, 9, 159–176. [Google Scholar] [CrossRef]
- Alyammahi, S.K.; Abdin, S.M.; Alhamad, D.W.; Elgendy, S.M.; Altell, A.T.; Omar, H.A. The dynamic association between COVID-19 and chronic disorders: An updated insight into prevalence, mechanisms and therapeutic modalities. Infect. Genet. Evol. 2021, 87, 104647. [Google Scholar] [CrossRef]
- Saqib, M.A.N.; Siddiqui, S.; Qasim, M.; Jamil, M.A.; Rafique, I.; Awan, U.A.; Ahmad, H.; Afzal, M.S. Effect of COVID-19 lockdown on patients with chronic diseases. Diabetes Metab. Syndr. 2020, 14, 1621–1623. [Google Scholar] [CrossRef]
- Trindade, I.A.; Ferreira, N.B. COVID-19 pandemic’s effects on disease and psychological outcomes of people with inflammatory bowel disease in Portugal: A preliminary research. Inflamm. Bowel. Dis. 2020, 27, 1224–1229. [Google Scholar] [CrossRef]
- Wang, H.; Tu, L.; Li, Y.; Bai, T.; Zou, K.; Xiao, F.; Li, J.; Chen, M.; Zhang, H.; Li, G.; et al. The symptoms and medications of patients with inflammatory bowel disease in hubei province after COVID-19 Epidemic. J. Immunol. Res. 2020, 2020, 2847316. [Google Scholar] [CrossRef]
- Azzam, N.A.; Aljebreen, A.; Almuhareb, A.; Almadi, M.A. Disability and quality of life before and during the COVID-19 outbreak: A cross-sectional study in inflammatory bowel disease patients. Saudi J. Gastroenterol. 2020, 26, 256–262. [Google Scholar] [CrossRef]
- Gavrilescu, O.; Prelipcean, C.C.; Dranga, M.; Soponaru, C.; Mihai, C. The specialized educational and psychological counseling in inflammatory bowel disease patients-a target or a challenge? Turk. J. Gastroenterol. 2020, 31, 760–766. [Google Scholar] [CrossRef]
- Guyatt, G.; Mitchell, A.; Irvine, E.J.; Singer, J.; Williams, N.; Goodacre, R.; Tompkins, C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology 1989, 96, 804–810. [Google Scholar] [CrossRef]
- Atkinson, L.; Kite, C.; McGregor, G.; James, T.; Clark, C.C.; Randeva, H.S.; Kyrou, I. Uncertainty, Anxiety and Isolation: Experiencing the COVID-19 Pandemic and Lockdown as a Woman with Polycystic Ovary Syndrome (PCOS). J. Pers. Med. 2021, 11, 952. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Knowles, S.R.; Keefer, L.; Wilding, H.; Hewitt, C.; Graff, L.A.; Mikocka-Walus, A. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses. Part II. Inflamm. Bowel. Dis. 2018, 24, 966–976. [Google Scholar] [CrossRef] [PubMed]
- Del Hoyo, J.; Aguas, M. Implementing telemedicine in inflammatory bowel disease: Is COVID-19 the definitive trigger? Gastroenterol. Hepatol. 2020, 43, 415–417. [Google Scholar] [CrossRef]
- Janowitz, T.; Gablenz, E.; Pattinson, D.; Wang, T.C.; Conigliaro, J.; Tracey, K.; Tuveson, D. Famotidine use and quantitative symptom tracking for COVID-19 in non-hospitalised patients: A case series. Gut 2020, 69, 1592–1597. [Google Scholar] [CrossRef]
- Mariotti, A. The effects of chronic stress on health: New insights into the molecular mechanisms of brain-body communication. Future Sci. OA 2015, 1, FSO23. [Google Scholar] [CrossRef] [Green Version]
- de Bock, E.; Filipe, M.D.; Meij, V.; Oldenburg, B.; van Schaik, F.D.; Bastian, O.W.; Fidder, H.F.; Vriens, M.R.; Richir, M.C. Quality of life in patients with IBD during the COVID-19 pandemic in the Netherlands. BMJ Open Gastroenterol. 2021, 8, e000670. [Google Scholar] [CrossRef]
- Nass, B.Y.S.; Dibbets, P.; Markus, C.R. Impact of the COVID-19 pandemic on inflammatory bowel disease: The role of emotional stress and social isolation. Stress Health 2021, 38, 222–233. [Google Scholar] [CrossRef]
- Clair, R.; Gordon, M.; Kroon, M.; Reilly, C. The effects of social isolation on well-being and life satisfaction during pandemic. Humanit. Soc. Sci. Commun. 2021, 8, 28. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 23, 2769–2778. [Google Scholar] [CrossRef]
- Ghoshal, U.C.; Sahu, S.; Biswas, S.N.; Singh, P.; Chaudhary, M.; Ghoshal, U.; Tiwari, P.; Rai, S.; Mishra, S.K. Care of inflammatory bowel disease patients during coronavirus disease-19 pandemic using digital health-care technology. JGH Open 2021, 5, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Li, L.; Xie, R.; Wang, B.; Jiang, K.; Cao, H. Stress Triggers Flare of Inflammatory Bowel Disease in Children and Adults. Front. Pediatr. 2019, 7, 432. [Google Scholar] [CrossRef]
- Herrera-de Guise, C.; Mayorga Ayala, L.F.; Serra Ruiz, X.; Robles Alonso, V.; BorruelSainz, N.; Ibarz, A.; Pérez Martínez, Z.; Casellas, F. Health-related quality of life decline in clinically stable inflammatory bowel disease patients during the COVID-19 outbreak. Rev. Esp. De Enferm. Dig. Organo Of. De La Soc. Esp. De Patol. Dig. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Brzozowski, B.; Mazur-Bialy, A.; Pajdo, R.; Kwiecien, S.; Bilski, J.; Zwolinska-Wcislo, M.; Mach, T.; Brzozowski, T. Mechanisms by which Stress Affects the Experimental and Clinical Inflammatory Bowel Disease (IBD): Role of Brain-Gut Axis. Curr. Neuropharmacol. 2016, 14, 892–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neuendorf, R.; Harding, A.; Stello, N.; Hanes, D.; Wahbeh, H. Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. J. Psychosom. Res. 2016, 87, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Stapersma, L.; van den Brink, G.; van der Ende, J.; Bodelier, A.G.; van Wering, H.M.; Hurkmans, P.C.W.M.; Mearin, M.L.; van der Meulen-de Jong, A.E.; Escher, J.C.; Utens, E.M.W.J. Illness Perceptions and Depression Are Associated with Health-Related Quality of Life in Youth with Inflammatory Bowel Disease. Int. J. Behav. Med. 2019, 26, 415–426. [Google Scholar] [CrossRef] [Green Version]
- Liang, S.W.; Chen, R.N.; Liu, L.L.; Li, X.G.; Chen, J.B.; Tang, S.Y.; Zhao, J.B. The Psychological Impact of the COVID-19 Epidemic on Guangdong College Students: The Difference between Seeking and Not Seeking Psychological Help. Front. Psychol. 2020, 4, 2231. [Google Scholar] [CrossRef]
| Total n = 90 | 2018 Group n = 45 | 2021 Group n = 45 | p | |
|---|---|---|---|---|
| Mean age ± SD years (median/interval) | 43.77 ± 12.76 44/19–70 | 43.80 ± 12.91 44/19–70 | 43.73 ± 12.75 44/19–70 | 0.980 t |
| Male, n(%) | 58 (64.4%) | 27 (60.0%) | 31 (68.9%) | 0.583 C |
| ≥45 years, n (%) | 46 (51.1%) | 23 (51.1%) | 23 (51.1%) | 1.000 C |
| Urban, n (%) | 66 (73.3%) | 31 (68.9%) | 35 (77.8%) | 0.339 C |
| Disorder, n (%) | 0.171 C | |||
| UC | 62 (68.9%) | 34 (75.6%) | 28 (62.2%) | |
| CD | 28 (31.1%) | 11 (24.4%) | 17 (37.8%) | |
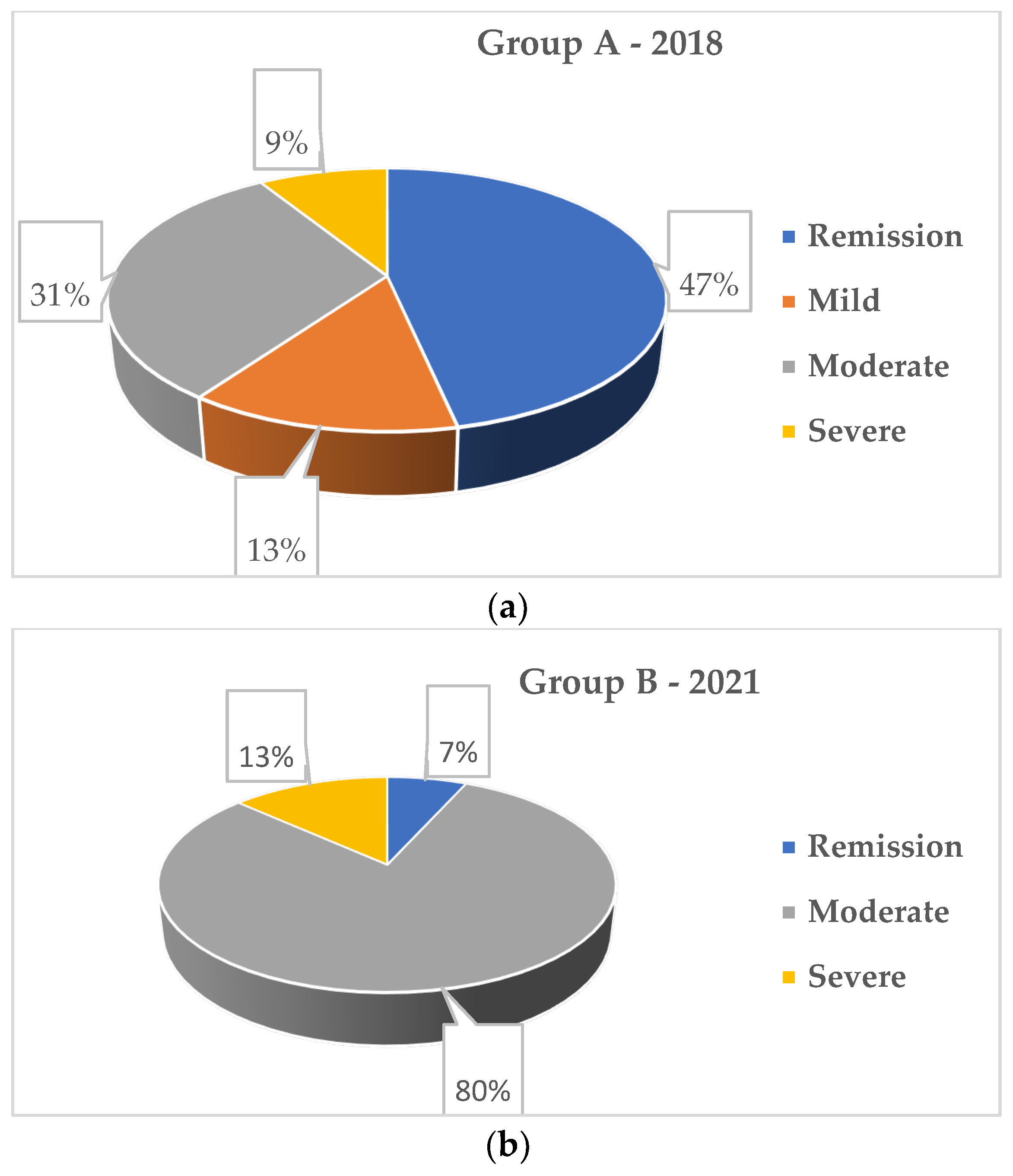
| Activity, n (%) | 0.001 C | |||
| mild | 6 (6.7%) | 6 (13.3%) | 0 (0.0%) | |
| moderate | 50 (55.6%) | 14 (31.3%) | 36 (80.0%) | |
| severe | 10 (11.1%) | 4 (8.9%) | 6 (13.3%) | |
| Remission, n (%) | 24 (26.7%) | 21 (46.7%) | 3 (6.7%) | 0.001 C |
| Mesalamines, n (%) | 31 (34.4%) | 16 (35.6%) | 15 (33.3%) | 0.825 C |
| Immunosupressants, n(%) | 19 (21.1%) | 9 (20.0%) | 10 (22.2%) | 0.797 C |
| Corticosteroids, n (%) | 8 (8.9%) | 3 (6.7%) | 5 (11.1%) | 0.461 C |
| Biologicals, n (%) | 32 (35.6%) | 17 (37.8%) | 15 (33.3%) | 0.661 C |
| Score | 2018 Group n = 45 | 2021 Group n = 45 | Statistical Test | p | Liniar Regression | |||
|---|---|---|---|---|---|---|---|---|
| Standardized Coefficients | Sig. | |||||||
| (Constant) | Year | Activity | ||||||
| IBDQ | 145.56 ± 32.00 | 128.33 ± 34.76 | t-Student | 0.016 | 153.50 | 5.50 | −18.50 | 0.018 |
| IBDQ-1 | 49.51 ± 13.13 | 43.24 ± 15.76 | t-Student | 0.043 | 53.15 | 3.41 | −8.49 | 0.018 |
| IBDQ-2 | 23.84 ± 7.03 | 20.67 ± 6.95 | t-Student | 0.034 | 22.32 | 1.84 | −2.78 | 0.090 |
| IBDQ-3 | 52.07 ± 16.46 | 45.20 ± 15.62 | t-Student | 0.045 | 62.50 | −3.44 | −5.36 | 0.210 |
| IBDQ-4 | 22.11 ± 5.93 | 19.22 ± 6.12 | t-Student | 0.025 | 27.05 | 0.63 | −4.39 | 0.003 |
| Score | Disease Activity | Statistical Test | p | ||
|---|---|---|---|---|---|
| Mild | Moderate | Severe | |||
| 2018 Sample | |||||
| IBDQ | 133.75 ± 8.44 | 122.43 ± 28.80 | 119.33 ± 24.99 | F ANOVA | 0.674 |
| IBDQ-1 | 43.75 ± 3.95 | 37.43 ± 11.13 | 44.67 ± 14.01 | F ANOVA | 0.350 |
| IBDQ-2 | 18.50 ± 1.73 | 18.57 ± 5.87 | 19.67 ± 6.74 | F ANOVA | 0.918 |
| IBDQ-3 | 55.75 ± 10.34 | 49.64 ± 19.01 | 42.17 ± 18.97 | F ANOVA | 0.499 |
| IBDQ-4 | 15.75 ± 4.03 | 19.79 ± 5.04 | 20.33 ± 6.86 | F ANOVA | 0.376 |
| 2021 Sample | |||||
| IBDQ | - | 121.39 ± 24.21 p = 0.144 | 67.67 ± 20.40 p= 0.001 | F ANOVA | 0.001 |
| IBDQ-1 | - | 35.97 ± 13.23 p = 0.067 | 22.67 ± 12.74 p= 0.014 | F ANOVA | 0.001 |
| IBDQ-2 | - | 18.03 ± 6.63 p = 0.231 | 14.17 ± 4.54 p = 0.110 | F ANOVA | 0.001 |
| IBDQ-3 | - | 48.25 ± 12.24 p = 0.760 | 19.50 ± 10.35 p= 0.001 | F ANOVA | 0.001 |
| IBDQ-4 | - | 18.14 ± 5.52 p = 0.836 | 11.33 ± 4.08 p = 0.131 | F ANOVA | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gavrilescu, O.; Prelipcean, C.C.; Dranga, M.; Popa, I.V.; Mihai, C. Impact of COVID-19 Pandemic on the Quality of Life of IBD Patients. Medicina 2022, 58, 562. https://doi.org/10.3390/medicina58050562
Gavrilescu O, Prelipcean CC, Dranga M, Popa IV, Mihai C. Impact of COVID-19 Pandemic on the Quality of Life of IBD Patients. Medicina. 2022; 58(5):562. https://doi.org/10.3390/medicina58050562
Chicago/Turabian StyleGavrilescu, Otilia, Cristina Cijevschi Prelipcean, Mihaela Dranga, Iolanda Valentina Popa, and Cătălina Mihai. 2022. "Impact of COVID-19 Pandemic on the Quality of Life of IBD Patients" Medicina 58, no. 5: 562. https://doi.org/10.3390/medicina58050562
APA StyleGavrilescu, O., Prelipcean, C. C., Dranga, M., Popa, I. V., & Mihai, C. (2022). Impact of COVID-19 Pandemic on the Quality of Life of IBD Patients. Medicina, 58(5), 562. https://doi.org/10.3390/medicina58050562






