Long-Term Results of Posterior Vertebral Column Resection for Severe Thoracolumbar Kyphosis with Achondroplastic Patients: A Case Series
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Case 1—16-Year-Old Girl, Achondroplasia, Thoracolumbar Kyphosis 126°
3.1.1. Patient History
3.1.2. Physical Examination
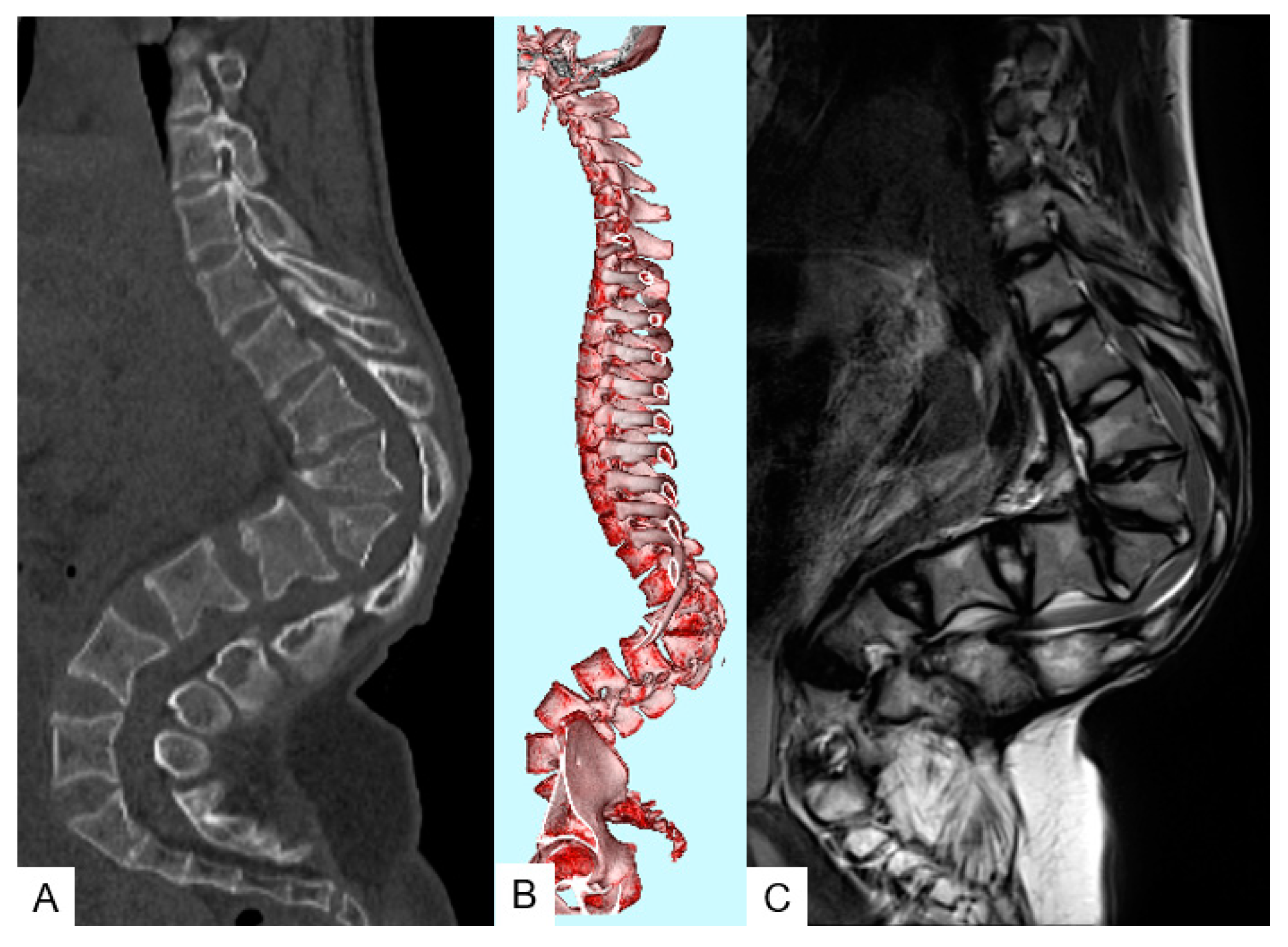
3.1.3. Preoperative Imaging
3.1.4. Surgery
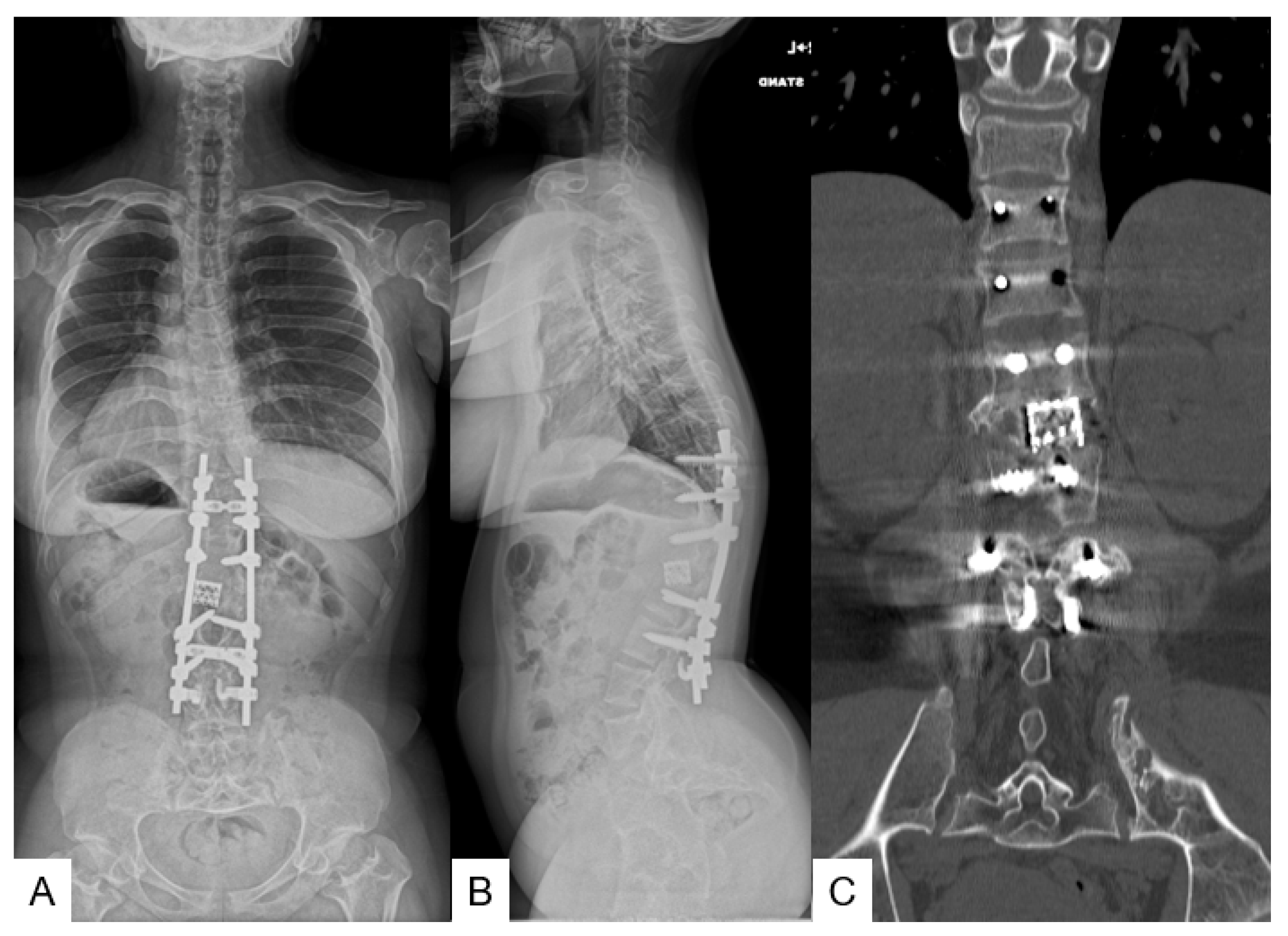
3.1.5. Postoperative Imaging
3.1.6. Follow-Up Results
3.2. Case 2—25-Year-Old Man, Achondroplasia, Thoracolumbar Kyphosis 123°
3.2.1. Patient History
3.2.2. Physical Examination
3.2.3. Preoperative Imaging
3.2.4. Surgery
3.2.5. Postoperative Imaging
3.2.6. Follow-Up Results
3.3. Case 3—26-Year-Old Man, Achondroplasia, Thoracolumbar Kyphosis 103°
3.3.1. Patient History
3.3.2. Physical Examination
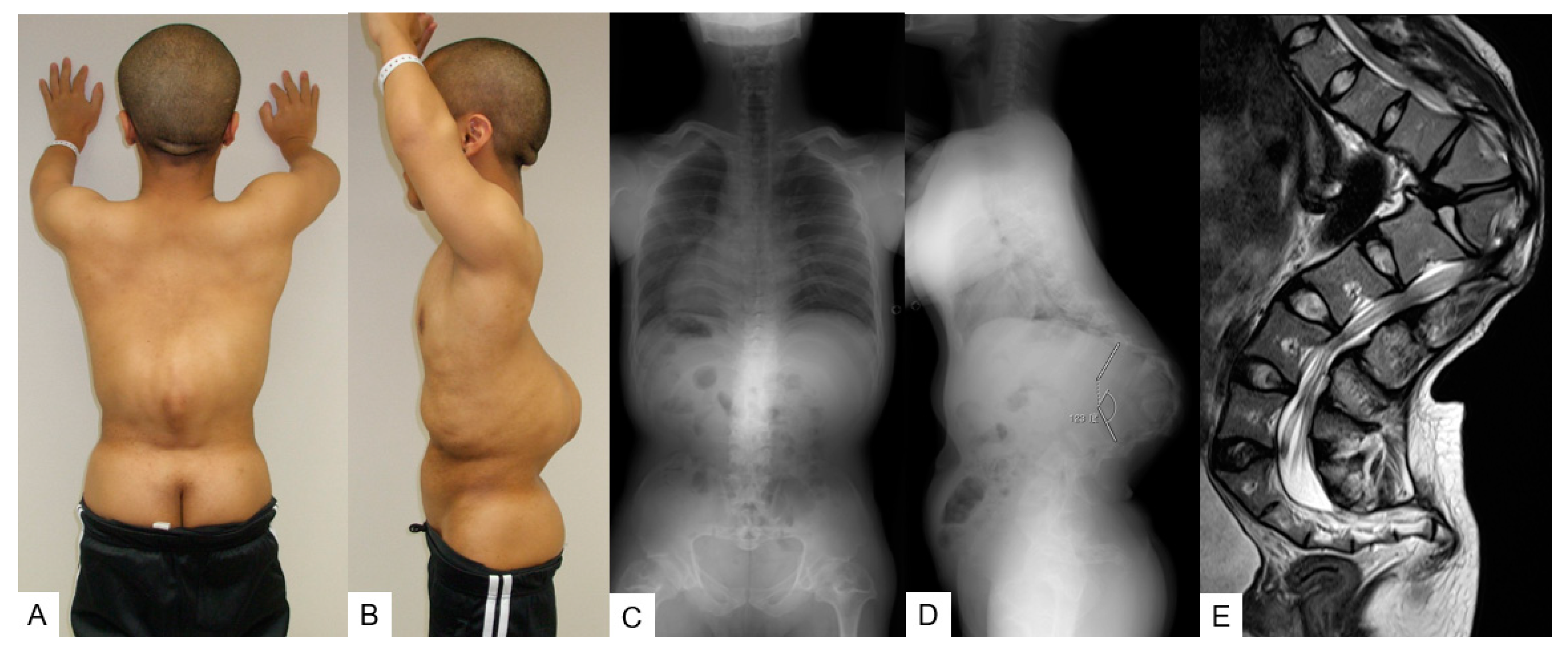
3.3.3. Preoperative Imaging
3.3.4. Surgery
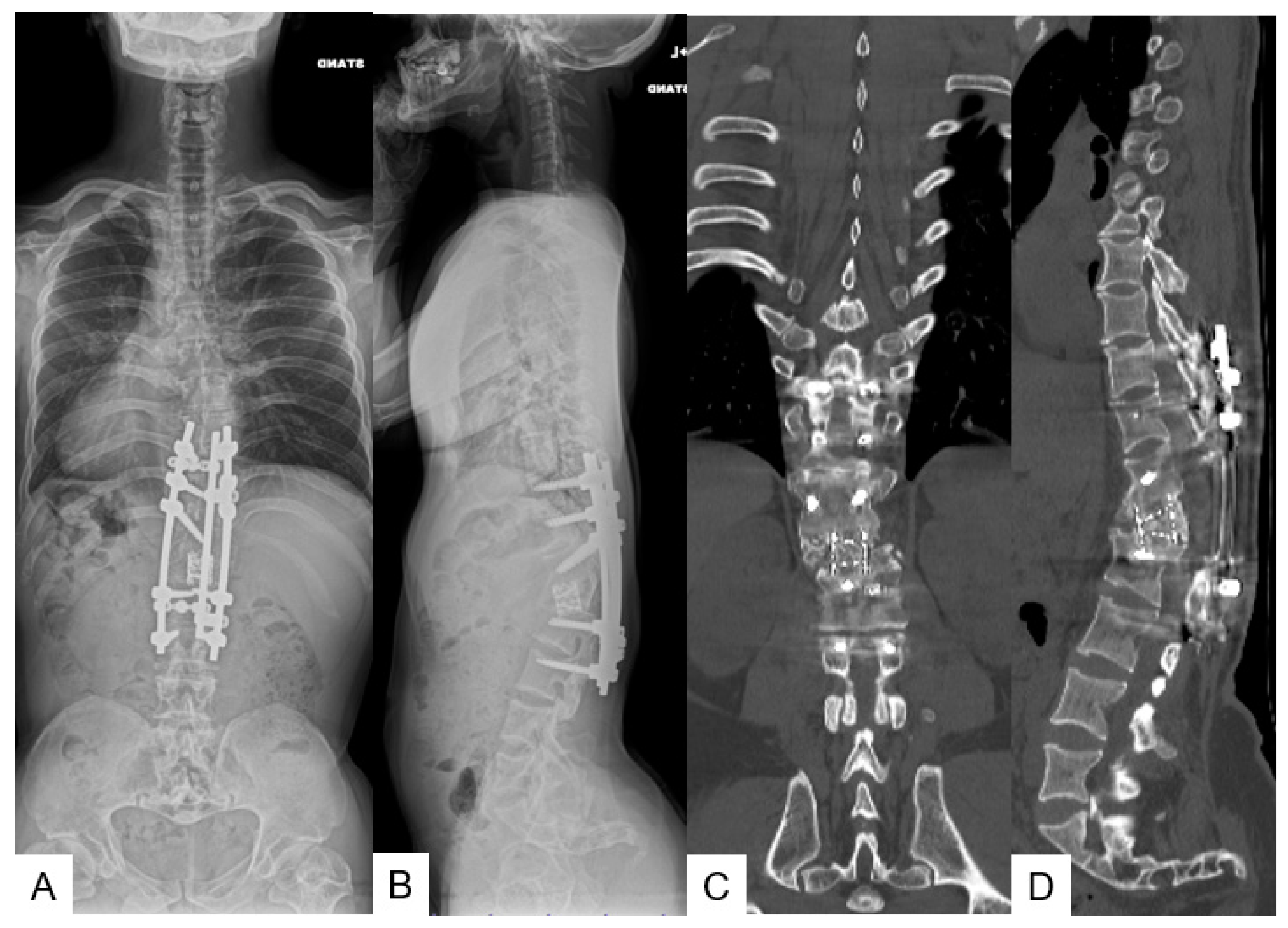
3.3.5. Postoperative Imaging
3.3.6. Follow-Up Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rousseau, F.; Bonaventure, J.; Legeai-Mallet, L.; Pelet, A.; Rozet, J.M.; Maroteaux, P.; Merrer, M.; Munnich, A. Mutations in the gene encoding fibroblast growth factor receptor-3 in achondroplasia. Nature 1994, 371, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Clair, A.; Francomano, C.A. The Genetic Basis of Dwarfism. N. Engl. J. Med. 1995, 332, 58–59. [Google Scholar]
- Srikumaran, U.; Woodard, E.J.; Leet, A.I.; Rigamonti, D.; Sponseller, P.D.; Ain, M.C. Pedicle and spinal canal parameters of the lower thoracic and lumbar vertebrae in the achondroplast population. Spine 2007, 32, 2423–2431. [Google Scholar] [CrossRef] [PubMed]
- Fredwall, S.O.; Steen, U.; de Vries, O.; Rustad, C.F.; Eggesbø, H.B.; Weedon-Fekjær, H.; Lidal, I.; Savarirayan, R.; Manum, G. High prevalence of symptomatic spinal stenosis in Norwegian adults with achondroplasia: A population-based study. Orphanet. J. Rare Dis. 2020, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Wynne-Davies, R.; Walsh, W.K.; Gormley, J. Achondroplasia and hypochondroplasia. Clinical variation and spinal stenosis. J. Bone Jt. Surg. Ser. B 1981, 63, 508–515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bethem, D.; Winter, R.B.; Lutter, L.; Moe, J.; Bradford, D.; .Lonstein, J.; Langer, L. Spinal disorders of dwarfism. Review of the literature and report of eighty cases. J. Bone Jt. Surg. Ser. A 1981, 63, 1412–1425. [Google Scholar] [CrossRef]
- Thomasen, E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin. Orthop. Relat. Res. 1985, 194, 142–152. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, J.H.; Kim, W.J.; Lee, S.M.; Chung, E.R.; Nah, K.H. Posterior vertebral column resection for severe spinal deformities. Spine 2002, 27, 2374–2382. [Google Scholar] [CrossRef]
- Tanaka, M.; Fujiwara, Y.; Uotani, K.; Yamauchi, T.; Misawa, H. C-arm Free Anterior Correction for Adolescent Idiopathic Scoliosis (Lenke type 5C): Analysis of Early Outcomes and Complications. World Neurosurg. 2021, 18, S1878-875000428-9. [Google Scholar] [CrossRef]
- Tanaka, M.; Uotani, K.; Fujiwara, Y.; Yamane, K.; Sonawane, S.; Arataki, S.; Yamauchi, T. Navigated Lateral Osteotomy for Adult Spinal Deformity: A Technical Note. World Neurosurg. 2021, 150, 56–63. [Google Scholar] [CrossRef]
- Okenfuss, E.; Moghaddam, B.; Avins, A.L. Natural history of achondroplasia: A retrospective review of longitudinal clinical data. Am. J. Med. Genet. Part. A 2020, 182A, 2540–2551. [Google Scholar] [CrossRef] [PubMed]
- Cabrera, G.; Boling, M.D. BRDC-C. Achondroplasia. In CINAHL Nursing Guide; Pravikoff, D.R.P.F., Ed.; EBSCO Publishing: Ipswich, MA, USA, 2018. [Google Scholar]
- Bodensteiner, J.B. Neurological Manifestations of Achondroplasia. Curr. Neurol. Neurosci. Rep. 2019, 19, 105. [Google Scholar] [CrossRef] [PubMed]
- Waller, D.; Correa, A.; Vo, T.M.; Wang, Y.; Hobbs, C.; Langlois, P.; Pearson, K.; Romitti, P.; Shaw, G.; Hecht, J. The population-based prevalence of achondroplasia and thanatophoric dysplasia in selected regions of the US. Am. J. Med. Genet. 2008, 146A, 2385–2389. [Google Scholar] [CrossRef]
- Vajo, Z.; Francomano, C.A.; Wilkin, D.J. The molecular and genetic basis of fibroblast growth factor receptor 3 disorders: The achondroplasia family of skeletal dysplasias, Muenke craniosynostosis, and Crouzon syndrome with acanthosis nigricans. Endocr. Rev. 2000, 21, 23–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kubota, T.; Adachi, M.; Kitaoka, T.; Hasegawa, K.; Ohata, Y.; Fujiwara, M.; Michigami, T.; Mochizuki, H.; Ozono, K. Clinical Practice Guidelines for Achondroplasia. Clin. Pediatr. Endocrinol. 2020, 29, 25–42. [Google Scholar] [CrossRef] [Green Version]
- Hecht, J.T.; Francomano, C.A.; Horton, W.A.; Annegers, J.F. Mortality in achondroplasia. Am. J. Hum. Genet. 1987, 41, 454–464. [Google Scholar]
- Hecht, J.T.; Nelson, F.W.; Butler, I.J.; Horton, W.; Scott, C., Jr.; Wassman, E.; Mehringer, C.; Rimoin, D.; Pauli, R. Computerized tomography of the foramen magnum: Achondroplastic values compared to normal standards. Am. J. Med. Genet. 1985, 20, 355–360. [Google Scholar] [CrossRef]
- Pauli, R.M.; Breed, A.; Horton, V.K.; Glinski, L.P.; Reiser, C.A. Prevention of fixed, angular kyphosis in achondroplasia. J. Pediatr. Orthop. 1997, 17, 726–733. [Google Scholar] [CrossRef]
- Richard, M.P. Achondroplasia: A comprehensive clinical review. Orphanet J. Rare Dis. 2019, 14, 1–49. [Google Scholar] [CrossRef] [Green Version]
- Margalit, A.; McKean, G.; Lawing, C.; Galey, S.; Ain, M.C. Walking Out of the Curve: Thoracolumbar Kyphosis in Achondroplasia. J. Pediatric Orthop. 2018, 38, 491–497. [Google Scholar] [CrossRef]
- Kei, A.; Kazuyoshi, K.; Hiroaki, N.; Machino, M.; Ito, S.; Kanbara, S.; Inoue, T.; Segi, N.; Koshimizu, H.; Imagama, S. Sagittal alignment at 3 years old determines future thoracolumbar kyphosis in achondroplasia: A prospective study with minimum 5-year follow-up from infancy. North Am. Spine Soc. J. 2021, 6, 100070. [Google Scholar] [CrossRef]
- Kopits, S.E. Thoracolumbar kyphosis and lumbosacral hyperlordosis in achondroplastic children. Basic Life Sci. 1988, 48, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Li, Y.; Sheng, F.; Xia, C.; Qiu, Y.; Zhu, Z. The Efficacy of Brace Treatment for Thoracolumbar Kyphosis in Patients With Achondroplasia. Spine 2018, 43, 1133–1138. [Google Scholar] [CrossRef] [PubMed]
- Misra, S.N.; Morgan, H.W. Thoracolumbar spinal deformity in achondroplasia. Neurosurg. Focus 2003, 14, e4. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.; El-Makhy, M.; Grevitt, M. The natural history of thoracolumbar kyphosis in achondroplasia. Eur. Spine J. 2019, 28, 2602–2607. [Google Scholar] [CrossRef] [PubMed]
- Ain, M.; Shirley, E.; Pirouzmanesh, A.; Hariri, A.; Carson, B. Postlaminectomy Kyphosis in the Skeletally Immature Achondroplast. Spine 2006, 31, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Şarlak, A.Y.; Buluç, L.; Anık, Y.; Memişoğlu, K.; Kurtgöz, B. Treatment of fixed thoracolumbar kyphosis in immature achondroplastic patient: Posterior column resection combined with segmental pedicle screw fixation and posterolateral fusion. Eur. Spine J. 2004, 13, 458–461. [Google Scholar] [CrossRef] [Green Version]
- Shaffrey, C.I. Expert’s comment concerning Grand Rounds case entitled “Surgical treatment of a 180° thoracolumbar fixed kyphosis in a young achondroplastic patient: A one stage ‘in situ’ combined fusion and spinal cord translocation” (by Aurégan, J.C.; Odent, T.; Zerah, M.; Padovani, J.-P.; Glorion, C.). Eur. Spine J. 2010, 19, 1812–1814. [Google Scholar]
- Pyeritz, R.E.; Sack, G.H., Jr.; Udvarhelyi, G.B. Thoracolumbosacral laminectomy in achondroplasia: Long-term results in 22 patients. Am. J. Med. Genet. 1987, 28, 433–444. [Google Scholar] [CrossRef]
- Ain, M.C.; Browne, J.A. Spinal arthrodesis with instrumentation for thoracolumbar kyphosis in pediatric achondroplasia. Spine 2004, 15, 2075–2080. [Google Scholar] [CrossRef]
- Qi, X.; Matsumoto, M.; Ishii, K.; Nakamura, M.; Chiba, K.; Toyama, Y. Posterior osteotomy and instrumentation for thoracolumbar kyphosis in patients with achondroplasia. Spine 2006, 31, E606–E610. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, S.; Wu, N.; Wang, S.; Qiu, G.; Zhang, J. Posterior Vertebral Column Resection (pVCR) for Severe Thoracolumbar Kyphosis in Patients With Achondroplasia. Global Spine J. 2021, 2192568221989291. [Google Scholar] [CrossRef] [PubMed]
- Ain, M.C.; Chang, T.L.; Schkrohowsky, J.G.; Carlisle, E.S.; Hodor, M.; Rigamonti, D. Rates of perioperative complications associated with laminectomies in patients with achondroplasia. J Bone Jt. Surg Am. 2008, 90, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.J.; Lenke, L.G.; Kim, Y.C.; Koester, L.A.; Blanke, K.M. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine 2014, 39, 1899–1904. [Google Scholar] [CrossRef]
- De Fernando, B.O.R.; De Alderico, G.C.B.; Juan, D.P.A.; Da Rodrigo, J.F.C.; Da Luis, E.C.T.S. Evaluation of Rod Breakage After Three-Column Osteotomy. Coluna/Columna 2020, 19, 44–47. [Google Scholar] [CrossRef] [Green Version]








| No. | JOA Scores Pre-Op | JOA Scores F/U | Years Of FU Post Op | Kyphosis Cobb Pre-Op | Kyphosis Cobb Post-Op | Correction Rate | Fusion Level | p-VCR | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 7 | 11 | 10 | 126 | 14 | 89% | T9-L3 | T12,L1 | SSI (day 10) |
| 2 | 8 | 10 | 9 | 123 | 38 | 69% | T9-L3 | T12,L1 | Rod breakage (2 years) |
| 3 | 9 | 11 | 9 | 103 | 57 | 47% | T9-L3 | T12, L1 | Rod breakage (1 year) SSI (3 years) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, M.; Chan, T.-T.; Misawa, H.; Uotani, K.; Arataki, S.; Takigawa, T.; Mazaki, T.; Sugimoto, Y. Long-Term Results of Posterior Vertebral Column Resection for Severe Thoracolumbar Kyphosis with Achondroplastic Patients: A Case Series. Medicina 2022, 58, 605. https://doi.org/10.3390/medicina58050605
Tanaka M, Chan T-T, Misawa H, Uotani K, Arataki S, Takigawa T, Mazaki T, Sugimoto Y. Long-Term Results of Posterior Vertebral Column Resection for Severe Thoracolumbar Kyphosis with Achondroplastic Patients: A Case Series. Medicina. 2022; 58(5):605. https://doi.org/10.3390/medicina58050605
Chicago/Turabian StyleTanaka, Masato, Tsang-Tung Chan, Haruo Misawa, Koji Uotani, Shinaya Arataki, Tomoyuki Takigawa, Tetsuro Mazaki, and Yoshihisa Sugimoto. 2022. "Long-Term Results of Posterior Vertebral Column Resection for Severe Thoracolumbar Kyphosis with Achondroplastic Patients: A Case Series" Medicina 58, no. 5: 605. https://doi.org/10.3390/medicina58050605
APA StyleTanaka, M., Chan, T. -T., Misawa, H., Uotani, K., Arataki, S., Takigawa, T., Mazaki, T., & Sugimoto, Y. (2022). Long-Term Results of Posterior Vertebral Column Resection for Severe Thoracolumbar Kyphosis with Achondroplastic Patients: A Case Series. Medicina, 58(5), 605. https://doi.org/10.3390/medicina58050605







