One-Year Clinical Outcomes of Minimal-Invasive Dorsal Percutaneous Fixation of Thoracolumbar Spine Fractures
Abstract
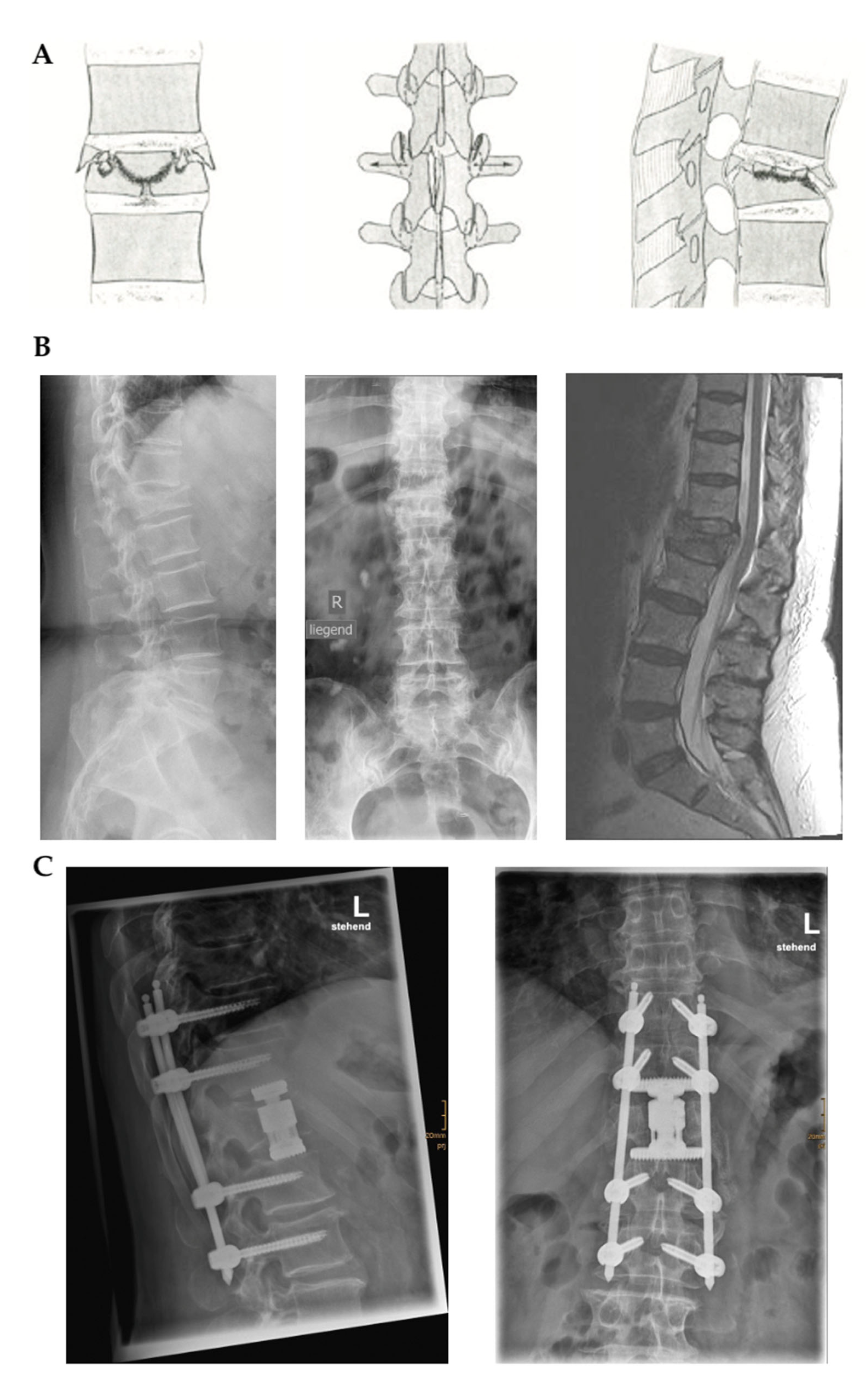
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Handling
2.3. Statistical Analysis
3. Results
3.1. Cohort Characteristics
3.2. Assessment of PROMs
3.3. Analysis of Association with PROMs
4. Discussion
4.1. Length of Stay
4.2. PROMs
4.3. Laboratory Data
4.4. Other Considerations
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wood, K.B.; Li, W.; Lebl, D.R.; Lebl, D.S.; Ploumis, A. Management of Thoracolumbar Spine Fractures. Spine J. 2014, 14, 145–164. [Google Scholar] [CrossRef]
- Couvertier, M.; Germaneau, A.; Saget, M.; Dupré, J.-C.; Doumalin, P.; Brémand, F.; Hesser, F.; Brèque, C.; Roulaud, M.; Monlezun, O.; et al. Biomechanical Analysis of the Thoracolumbar Spine under Physiological Loadings: Experimental Motion Data Corridors for Validation of Finite Element Models. Proc. Inst. Mech. Eng. H 2017, 231, 975–981. [Google Scholar] [CrossRef] [PubMed]
- Zileli, M.; Sharif, S.; Fornari, M. Incidence and Epidemiology of Thoracolumbar Spine Fractures: WFNS Spine Committee Recommendations. Neurospine 2021, 18, 704–712. [Google Scholar] [CrossRef]
- Bizimungu, R.; Sergio Alvarez, N.; Baumann, B.M.; Raja, A.S.; Mower, W.R.; Langdorf, M.I.; Medak, A.J.; Hendey, G.W.; Nishijima, D.; Rodriguez, R.M. Thoracic Spine Fracture in the Panscan Era. Ann. Emerg. Med. 2020, 76, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Katsuura, Y.; Osborn, J.M.; Cason, G.W. The Epidemiology of Thoracolumbar Trauma: A Meta-Analysis. J. Orthop. 2016, 13, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Zhu, Y.; Liu, S.; Chen, W.; Zhang, F.; Zhang, Y. National Incidence of Traumatic Spinal Fractures in China: Data from China National Fracture Study. Medicine 2018, 97, e12190. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Beck, C.; Yoganandan, N.; Rao, R.D. Incidence and Mechanism of Neurological Deficit after Thoracolumbar Fractures Sustained in Motor Vehicle Collisions. J. Neurosurg. Spine 2016, 24, 323–331. [Google Scholar] [CrossRef]
- Divi, S.N.; Schroeder, G.D.; Oner, F.C.; Kandziora, F.; Schnake, K.J.; Dvorak, M.F.; Benneker, L.M.; Chapman, J.R.; Vaccaro, A.R. AOSpine-Spine Trauma Classification System: The Value of Modifiers: A Narrative Review With Commentary on Evolving Descriptive Principles. Glob. Spine J. 2019, 9, 77S–88S. [Google Scholar] [CrossRef]
- Finkelstein, J.A.; Schwartz, C.E. Patient-Reported Outcomes in Spine Surgery: Past, Current, and Future Directions. J. Neurosurg. Spine 2019, 31, 155–164. [Google Scholar] [CrossRef]
- Reinhold, M.; Audigé, L.; Schnake, K.J.; Bellabarba, C.; Dai, L.-Y.; Oner, F.C. AO Spine Injury Classification System: A Revision Proposal for the Thoracic and Lumbar Spine. Eur. Spine J. 2013, 22, 2184–2201. [Google Scholar] [CrossRef]
- Kim, B.-G.; Dan, J.-M.; Shin, D.-E. Treatment of Thoracolumbar Fracture. Asian Spine J. 2015, 9, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Assaker, R. Minimal Access Spinal Technologies: State-of-the-Art, Indications, and Techniques. Jt. Bone Spine 2004, 71, 459–469. [Google Scholar] [CrossRef] [PubMed]
- Vu, C.; Gendelberg, D. Classifications in Brief: AO Thoracolumbar Classification System. Clin. Orthop. Relat. Res. 2020, 478, 434–440. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952, discussion 2952. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Vila-Casademunt, A.; Domingo-Sàbat, M.; Wunderlin, S.; Pellisé, F.; Bago, J.; Acaroglu, E.; Alanay, A.; Pérez-Grueso, F.S.; Obeid, I.; et al. The Core Outcome Measures Index (COMI) Is a Responsive Instrument for Assessing the Outcome of Treatment for Adult Spinal Deformity. Eur. Spine J. 2016, 25, 2638–2648. [Google Scholar] [CrossRef]
- Haefeli, M.; Elfering, A. Pain Assessment. Eur. Spine J. 2006, 15 (Suppl. 1), S17–S24. [Google Scholar] [CrossRef]
- Garratt, A.M.; Furunes, H.; Hellum, C.; Solberg, T.; Brox, J.I.; Storheim, K.; Johnsen, L.G. Evaluation of the EQ-5D-3L and 5L Versions in Low Back Pain Patients. Health Qual. Life Outcomes 2021, 19, 155. [Google Scholar] [CrossRef]
- Schwind, J.; Learman, K.; O’Halloran, B.; Showalter, C.; Cook, C. Different Minimally Important Clinical Difference (MCID) Scores Lead to Different Clinical Prediction Rules for the Oswestry Disability Index for the Same Sample of Patients. J. Man. Manip. Ther. 2013, 21, 71–78. [Google Scholar] [CrossRef]
- Luo, N.; Johnson, J.; Coons, S.J. Using Instrument-Defined Health State Transitions to Estimate Minimally Important Differences for Four Preference-Based Health-Related Quality of Life Instruments. Med. Care 2010, 48, 365–371. [Google Scholar] [CrossRef]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal Clinically Important Changes in Chronic Musculoskeletal Pain Intensity Measured on a Numerical Rating Scale. Eur. J. Pain 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Akoglu, H. User’s Guide to Correlation Coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Dickerman, R.D.; Reynolds, A.S.; Tackett, J.; Winters, K.; Alvarado, C. Percutaneous Pedicle Screws Significantly Decrease Muscle Damage and Operative Time: Surgical Technique Makes a Difference! Eur. Spine J. 2008, 17, 1398. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lendemans, S.; Hussmann, B.; Kauther, M.D.; Nast-Kolb, D.; Taeger, G. Minimally invasive dorsal stabilization of the thoracolumbar spine. Unfallchirurg 2011, 114, 149–159, quiz 160. [Google Scholar] [CrossRef] [PubMed]
- Hikmet Demirkol, Y.S. Minimally Invasive Stabilization for Thoracolumbar Fractures. J. Spine 2013, 5, 3. [Google Scholar] [CrossRef]
- Younus, A.; Kelly, A.; Lekgwara, P. An Institutional Review of Percutaneous Stabilization versus Open Stabilization of Unstable Thoracolumbar Fractures. Interdiscip. Neurosurg. 2020, 22, 100806. [Google Scholar] [CrossRef]
- Phan, K.; Rao, P.J.; Mobbs, R.J. Percutaneous versus Open Pedicle Screw Fixation for Treatment of Thoracolumbar Fractures: Systematic Review and Meta-Analysis of Comparative Studies. Clin. Neurol. Neurosurg. 2015, 135, 85–92. [Google Scholar] [CrossRef] [PubMed]
- de Jong, J.D.; Westert, G.P.; Lagoe, R.; Groenewegen, P.P. Variation in Hospital Length of Stay: Do Physicians Adapt Their Length of Stay Decisions to What Is Usual in the Hospital Where They Work? Health Serv. Res. 2006, 41, 374–394. [Google Scholar] [CrossRef] [PubMed]
- Englum, B.R.; Hui, X.; Zogg, C.K.; Chaudhary, M.A.; Villegas, C.; Bolorunduro, O.B.; Stevens, K.A.; Haut, E.R.; Cornwell, E.E.; Efron, D.T.; et al. Association Between Insurance Status and Hospital Length of Stay Following Trauma. Am. Surg. 2016, 82, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Sapkas, G.; Kateros, K.; Papadakis, S.A.; Brilakis, E.; Macheras, G.; Katonis, P. Treatment of Unstable Thoracolumbar Burst Fractures by Indirect Reduction and Posterior Stabilization: Short-Segment versus Long-Segment Stabilization. Open Orthop. J. 2010, 4, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, L. Comparison of Short-Segment versus Long-Segment Fixation for the Treatment of Thoracolumbar Burst Fracture: A Meta-Analysis. Int. J. Clin. Exp. Med. 2017, 10, 1750–1762. [Google Scholar]
- Serin, E.; Karakurt, L.; Yilmaz, E.; Belhan, O.; Varol, T. Effects of Two-Levels, Four-Levels, and Four-Levels plus Offset-Hook Posterior Fixation Techniques on Protecting the Surgical Correction of Unstable Thoracolumbar Vertebral Fractures: A Clinical Study. Eur. J. Orthop. Surg. Traumatol. 2004, 14, 1–6. [Google Scholar] [CrossRef]
- Altay, M.; Ozkurt, B.; Aktekin, C.N.; Ozturk, A.M.; Dogan, O.; Tabak, A.Y. Treatment of Unstable Thoracolumbar Junction Burst Fractures with Short- or Long-Segment Posterior Fixation in Magerl Type a Fractures. Eur. Spine J. 2007, 16, 1145–1155. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chen, C.-H.; Tsuang, F.-Y.; Lin, Y.-C.; Chiang, C.-J.; Kuo, Y.-J. The Stability of Long-Segment and Short-Segment Fixation for Treating Severe Burst Fractures at the Thoracolumbar Junction in Osteoporotic Bone: A Finite Element Analysis. PLoS ONE 2019, 14, e0211676. [Google Scholar] [CrossRef] [PubMed]
- Modi, H.N.; Chung, K.J.; Seo, I.W.; Yoon, H.S.; Hwang, J.H.; Kim, H.K.; Noh, K.C.; Yoo, J.H. Two Levels above and One Level below Pedicle Screw Fixation for the Treatment of Unstable Thoracolumbar Fracture with Partial or Intact Neurology. J. Orthop. Surg. Res. 2009, 4, 28. [Google Scholar] [CrossRef] [PubMed]
- Ugras, A.A.; Akyildiz, M.F.; Yilmaz, M.; Sungur, I.; Cetinus, E. Is It Possible to Save One Lumbar Segment in the Treatment of Thoracolumbar Fractures? Acta Orthop. Belg. 2012, 78, 87–93. [Google Scholar]
- Claus, C.F.; Tong, D.; Lytle, E.; Bahoura, M.; Garmo, L.; Li, C.; Park, P.; Carr, D.A.; Easton, R.; Abdulhak, M.; et al. Age as a Predictor for Complications and Patient-Reported Outcomes in Multilevel Transforaminal Lumbar Interbody Fusions: Analyses From the Michigan Spine Surgery Improvement Collaborative (MSSIC). Spine 2021, 46, 356–365. [Google Scholar] [CrossRef]
- Genov, P.G.; Timerbaev, V.K.; Dolgasheva, N.S.; Efanov, A.A.; Grin’, A.A.; Rebrova, O.Y. Prognostic models of the severity of acute dynamic pain on the first postoperative day and the likelihood of chronic postoperative pain in spine surgery. Zhurnal Vopr. Neirokhirurgii Im. NN Burd. 2018, 82, 29–35. [Google Scholar] [CrossRef]
- Merali, Z.G.; Witiw, C.D.; Badhiwala, J.H.; Wilson, J.R.; Fehlings, M.G. Using a Machine Learning Approach to Predict Outcome after Surgery for Degenerative Cervical Myelopathy. PLoS ONE 2019, 14, e0215133. [Google Scholar] [CrossRef]
- Lee, B.H.; Yang, J.H.; Lee, H.M.; Park, J.Y.; Park, S.E.; Moon, S.H. Surgical Outcome Predictor in Degenerative Lumbar Spinal Disease Based on Health Related Quality of Life Using Euro-Quality 5 Dimensions Analysis. Yonsei Med. J. 2016, 57, 1214–1221. [Google Scholar] [CrossRef]
- Hegarty, D.; Shorten, G. Multivariate Prognostic Modeling of Persistent Pain Following Lumbar Discectomy. Pain Physician 2012, 15, 421–434. [Google Scholar] [CrossRef]
- Khor, S.; Lavallee, D.; Cizik, A.M.; Bellabarba, C.; Chapman, J.R.; Howe, C.R.; Lu, D.; Mohit, A.A.; Oskouian, R.J.; Roh, J.R.; et al. Development and Validation of a Prediction Model for Pain and Functional Outcomes After Lumbar Spine Surgery. JAMA Surg. 2018, 153, 634–642. [Google Scholar] [CrossRef] [PubMed]
- McGirt, M.J.; Bydon, M.; Archer, K.R.; Devin, C.J.; Chotai, S.; Parker, S.L.; Nian, H.; Harrell, F.E.; Speroff, T.; Dittus, R.S.; et al. An Analysis from the Quality Outcomes Database, Part 1. Disability, Quality of Life, and Pain Outcomes Following Lumbar Spine Surgery: Predicting Likely Individual Patient Outcomes for Shared Decision-Making. J. Neurosurg. Spine 2017, 27, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.P.; Price, A.J.; Beard, D.J.; Hadfield, S.G.; Arden, N.K.; Murray, D.W.; Field, R.E. The Effects of Age on Patient-Reported Outcome Measures in Total Knee Replacements. Bone Jt. J. 2013, 95-B, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.N.; van der Meulen, J.H.; Lewsey, J.; Gregg, P.J. The Role of Pain and Function in Determining Patient Satisfaction after Total Knee Replacement: Data from the national joint registry for england and wales. J. Bone Jt. Surgery. Br. Vol. 2007, 89-B, 893–900. [Google Scholar] [CrossRef] [PubMed]
- Chotai, S.; Parker, S.L.; Sivaganesan, A.; Sielatycki, J.A.; Asher, A.L.; McGirt, M.J.; Devin, C.J. Effect of Complications within 90 Days on Patient-Reported Outcomes 3 Months and 12 Months Following Elective Surgery for Lumbar Degenerative Disease. Neurosurg. Focus 2015, 39, E8. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.D.; Hamill, C.L.; Bridwell, K.H.; Schwab, F.J.; Dimar, J.R.; Lowe, T.G. The Impact of Perioperative Complications on Clinical Outcome in Adult Deformity Surgery. Spine 2007, 32, 2764–2770. [Google Scholar] [CrossRef] [PubMed]
- McGirt, M.J.; Parker, S.L.; Chotai, S.; Pfortmiller, D.; Sorenson, J.M.; Foley, K.; Asher, A.L. Predictors of Extended Length of Stay, Discharge to Inpatient Rehab, and Hospital Readmission Following Elective Lumbar Spine Surgery: Introduction of the Carolina-Semmes Grading Scale. J. Neurosurg. Spine 2017, 27, 382–390. [Google Scholar] [CrossRef]
- Bortz, C.; Pierce, K.E.; Alas, H.; Brown, A.; Vasquez-Montes, D.; Wang, E.; Varlotta, C.G.; Woo, D.; Abotsi, E.J.; Manning, J.; et al. The Patient-Reported Outcome Measurement Information System (PROMIS) Better Reflects the Impact of Length of Stay and the Occurrence of Complications Within 90 Days Than Legacy Outcome Measures for Lumbar Degenerative Surgery. Int. J. Spine Surg. 2021, 15, 82–86. [Google Scholar] [CrossRef]
- Saravi, B.; Lang, G.; Ülkümen, S.; Südkamp, N.; Hassel, F. Case-Matched Radiological and Clinical Outcome Evaluation of Interlaminar versus Microsurgical Decompression of Lumbar Spinal Stenosis. In Proceedings of the Proce Deutscher Kongress für Orthopädie und Unfallchirurgie (DKOU 2021), Berlin, Germany, 29 October 2021. [Google Scholar] [CrossRef]
- Lozano-Álvarez, C.; Pérez-Prieto, D.; Saló, G.; Molina, A.; Lladó, A.; Ramírez, M. Usefulness of the Core Outcome Measures Index in Daily Clinical Practice for Assessing Patients with Degenerative Lumbar Disease. Adv. Orthop. 2012, 2012, 474685. [Google Scholar] [CrossRef]
- Ohba, T.; Ebata, S.; Haro, H. Comparison of Serum Markers for Muscle Damage, Surgical Blood Loss, Postoperative Recovery, and Surgical Site Pain after Extreme Lateral Interbody Fusion with Percutaneous Pedicle Screws or Traditional Open Posterior Lumbar Interbody Fusion. BMC Musculoskelet. Disord. 2017, 18, 415. [Google Scholar] [CrossRef]
- Iglesias, D.L. Validity of Creatine Kinase as an Indicator of Muscle Injury in Spine Surgery and Its Relation with Postoperative Pain. Clin. Med. Rev. Case Rep. 2014, 1, 545–550. [Google Scholar] [CrossRef]
- Mjaaland, K.E.; Kivle, K.; Svenningsen, S.; Pripp, A.H.; Nordsletten, L. Comparison of Markers for Muscle Damage, Inflammation, and Pain Using Minimally Invasive Direct Anterior versus Direct Lateral Approach in Total Hip Arthroplasty: A Prospective, Randomized, Controlled Trial. J. Orthop. Res. 2015, 33, 1305–1310. [Google Scholar] [CrossRef] [PubMed]
- Grass, R.; Biewener, A.; Dickopf, A.; Rammelt, S.; Heineck, J.; Zwipp, H. Percutaneous dorsal versus open instrumentation for fractures of the thoracolumbar border. A comparative, prospective study. Unfallchirurg 2006, 109, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, W.; Ushmaev, A.; Ruecker, A.; Nuechtern, J.; Grossterlinden, L.; Begemann, P.G.; Baeumer, T.; Rueger, J.M.; Briem, D. Comparison of Open versus Percutaneous Pedicle Screw Insertion in a Sheep Model. Eur. Spine J. 2008, 17, 857–863. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Fu, G.; Li, B.; Li, Y.; Yang, X. Comparison of the Effects of Minimally Invasive Percutaneous Pedicle Screws Osteosynthesis and Open Surgery on Repairing the Pain, Inflammation and Recovery of Thoracolumbar Vertebra Fracture. Exp. Ther. Med. 2017, 14, 4091–4096. [Google Scholar] [CrossRef]
- Colley, C.M.; Fleck, A.; Goode, A.W.; Muller, B.R.; Myers, M.A. Early Time Course of the Acute Phase Protein Response in Man. J. Clin. Pathol. 1983, 36, 203–207. [Google Scholar] [CrossRef]
- White, J.; Kelly, M.; Dunsmuir, R. C-Reactive Protein Level after Total Hip and Total Knee Replacement. J. Bone Jt. Surg. Br. 1998, 80, 909–911. [Google Scholar] [CrossRef]
- Bourguignat, A.; Férard, G.; Jenny, J.Y.; Gaudias, J. Incomplete or Absent Acute Phase Response in Some Postoperative Patients. Clin. Chim. Acta 1997, 264, 27–35. [Google Scholar] [CrossRef]
- Brewster, N.; Guthrie, C.; McBirnie, J. CRP Levels as a Measure of Surgical Trauma: A Comparison of Different General Surgical Procedures. J. R. Coll. Surg. Edinb. 1994, 39, 86–88. [Google Scholar]
- Cole, D.S.; Watts, A.; Scott-Coombes, D.; Avades, T. Clinical Utility of Peri-Operative C-Reactive Protein Testing in General Surgery. Ann. R. Coll. Surg. Engl. 2008, 90, 317–321. [Google Scholar] [CrossRef]
- Chung, W.H.; Ng, W.L.; Chiu, C.K.; Chan, C.; Kwan, M.K. Minimally Invasive versus Conventional Open Surgery for Fixation of Spinal Fracture in Ankylosed Spine. Malays. Orthop. J. 2020, 14, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Pishnamaz, M.; Schemmann, U.; Herren, C.; Horst, K.; Lichte, P.; Hildebrand, F.; Pape, H.-C.; Kobbe, P. Muscular Changes after Minimally Invasive versus Open Spinal Stabilization of Thoracolumbar Fractures: A Literature Review. J. Musculoskelet. Neuronal Interact 2018, 18, 62–70. [Google Scholar] [PubMed]
- Ganse, B.; Pishnamaz, M.; Kobbe, P.; Herren, C.; Gradl-Dietsch, G.; Böhle, F.; Johannes, B.; Kim, B.-S.; Horst, K.; Knobe, M. Microcirculation in Open vs. Minimally Invasive Dorsal Stabilization of Thoracolumbar Fractures. PLoS ONE 2017, 12, e0188115. [Google Scholar] [CrossRef] [PubMed]
- Erichsen, C.J.; Heyde, C.-E.; Josten, C.; Gonschorek, O.; Panzer, S.; von Rüden, C.; Spiegl, U.J. Percutaneous versus Open Posterior Stabilization in AOSpine Type A3 Thoracolumbar Fractures. BMC Musculoskelet. Disord. 2020, 21, 74. [Google Scholar] [CrossRef]
- Palmisani, M.; Gasbarrini, A.; Brodano, G.B.; De Iure, F.; Cappuccio, M.; Boriani, L.; Amendola, L.; Boriani, S. Minimally Invasive Percutaneous Fixation in the Treatment of Thoracic and Lumbar Spine Fractures. Eur. Spine J. 2009, 18 (Suppl. 1), 71–74. [Google Scholar] [CrossRef] [PubMed]
- Wall, B.A.; Moskowitz, A.; Whitaker, M.C.; Jones, T.L.; Stuckey, R.M.; Carr-Maben, C.L.; Chong, A.C. Functional Outcomes of Thoracolumbar Junction Spine Fractures. Kans. J. Med. 2017, 10, 30–34. [Google Scholar] [CrossRef][Green Version]
- Gühring, T.; Raible, C.; Matschke, S. Perkutane dorsale Instrumentierung der thorakolumbalen Wirbelsäule: Technik der geschlossenen Frakturreposition bei gleichzeitiger Dekompression des Spinalkanals. Unfallchirurg 2013, 116, 749–754. [Google Scholar] [CrossRef]
- Blattert, T.R.; Katscher, S.; Josten, C. Percutaneous techniques in the thoracic and lumbar spine. Unfallchirurg 2011, 114, 17–25. [Google Scholar] [CrossRef]
- Wang, H.; Li, C.; Zhou, Y.; Zhang, Z.; Wang, J.; Chu, T. Percutaneous Pedicle Screw Fixation through the Pedicle of Fractured Vertebra in the Treatment of Type A Thoracolumbar Fractures Using Sextant System: An Analysis of 38 Cases. Chin. J. Traumatol. 2010, 13, 137–145. [Google Scholar]

| Pairwise Comparisons | ||||
| Variable | Cohort Characteristics n = 68 | Preoperatively | Postoperatively | p-Value |
| Gender | ||||
| Female | 37 | |||
| Male | 31 | |||
| Age (years) | 76.99 ± 13.89 | |||
| Body mass index (kg/m2) | 24.98 ± 4.74 | |||
| Number of levels | 4.25 ± 1.41 | |||
| Screw-rod system | ||||
| Percusys | 6 | |||
| Z-Medical | 62 | |||
| Screw type | ||||
| Polyaxial | 62 | |||
| Quattroaxial | 6 | |||
| Complications | ||||
| No | 59 | |||
| Yes | 9 | |||
| Operation time (minutes) | 92.21 ± 28.19 | |||
| Length of stay (days) | 14.31 ± 6.81 | |||
| White blood cell count (per nL) | 8.56 ± 3.19 | 8.78 ± 3.37 | ns | |
| C-reactive protein (mg/L) | 24.87 ± 33.29 | 34.84 ± 29.87 | <0.001 | |
| Hemoglobin (g/dL) | 12.74 ± 1.81 | 11.50 ± 1.80 | <0.001 | |
| Hematocrit (L/L) | 0.37 ± 0.05 | 0.34 ± 0.05 | <0.001 | |
| Thrombocytes (per nL) | 280.7 ± 92.01 | 322.9 ± 107.92 | <0.001 | |
| Erythrocytes | 4.15 ± 0.61 | 3.78 ± 0.55 | <0.001 | |
| International normalized ratio | 1.03 ± 0.086 | 1.02 ± 0.032 | ns | |
| Prothrombin time (%) | 94.9 ± 11.98 | 100.2 ± 15.27 | ns | |
| Partial thromboplastin time (seconds) | 28.8 ± 3.69 | 28.6 ± 2.61 | ns | |
| Sodium | 137.8 ± 4.37 | 138.4 ± 4.32 | ns | |
| Blood sugar level (mg/dL) | 115.7 ± 35.30 | 118.2 ± 25.20 | ns | |
| Creatinine (mg/dL) | 0.86 ± 0.45 | 0.82 ± 0.68 | <0.001 | |
| Glomerular filtration rate (ml/min) | 90.30 ± 31.00 | 105.2 ± 39.02 | <0.001 | |
| Urea (mg/dL) | 38.00 ± 23.90 | 33.38 ± 31.63 | <0.001 | |
| ns: not significant | ||||
| ODI | ||||||
| 3 Weeks Postoperatively | 1 Year Postoperatively | |||||
| Variable | Phi Coefficient or Cramer’s V | Chi-squared | p-Value | Phi Coefficient or Cramer’s V | Chi-squared | p-Value |
| Gender | 0.127 | 1.004 | 0.316 | 0.009 | 0.005 | 0.947 |
| Screw-rod system | 0.198 | 2.419 | 0.120 | 0.086 | 0.458 | 0.499 |
| Screw type | 0.115 | 0.814 | 0.367 | 0.069 | 0.295 | 0.587 |
| Complications | 0.025 | 0.038 | 0.845 | 0.095 | 0.557 | 0.456 |
| ASA | 0.2617 | 3.928 | 0.269 | 0.096 | 0.569 | 0.904 |
| Reposition Level | 0.661 | 27.08 | 0.352 | 0.702 | 30.519 | 0.205 |
| COMI | ||||||
| 3 Weeks Postoperatively | 1 Year Postoperatively | |||||
| Variable | Phi Coefficient or Cramer’s V | Chi-squared | p-Value | Phi Coefficient or Cramer’s V | Chi-squared | p-Value |
| Gender | 0.095 | 0.557 | 0.455 | 0.132 | 1.084 | 0.298 |
| Screw-rod system | 0.197 | 2.412 | 0.120 | 0.042 | 0.109 | 0.741 |
| Screw type | 0.158 | 1.553 | 0.213 | 0.034 | 0.070 | 0.791 |
| Complications | 0.232 | 3.335 | 0.068 | 0.049 | 0.151 | 0.698 |
| ASA | 0.279 | 4.813 | 0.186 | 0.200 | 2.485 | 0.478 |
| Reposition Level | 0.535 | 17.769 | 0.852 | 0.701 | 30.492 | 0.206 |
| eQ5D | ||||||
| 3 Weeks Postoperatively | 1 Year Postoperatively | |||||
| Variable | Phi Coefficient or Cramer’s V | Chi-squared | p-Value | Phi Coefficient or Cramer’s V | Chi-squared | p-Value |
| Gender | 0.101 | 0.688 | 0.407 | 0.079 | 0.421 | 0.516 |
| Screw-rod system | 0.208 | 2..940 | 0.086 | 0.172 | 2.011 | 0.156 |
| Screw type | 0.129 | 1.127 | 0.288 | 0.037 | 0.092 | 0.761 |
| Complications | 0.167 | 1.899 | 0.168 | 0.172 | 2.017 | 0.156 |
| ASA | 0.247 | 4.142 | 0.247 | 0.282 | 5.401 | 0.145 |
| Reposition Level | 0.601 | 24.594 | 0.597 | 0.682 | 31.648 | 0.245 |
| NRS-Back | ||||||
| 3 Weeks Postoperatively | 1 Year Postoperatively | |||||
| Variable | Phi Coefficient or Cramer’s V | Chi-squared | p-Value | Phi Coefficient or Cramer’s V | Chi-squared | p-Value |
| Gender | 0.199 | 2.539 | 0.111 | 0.289 | 5.379 | 0.020 (*) |
| Screw-rod system | 0.260 | 4.337 | 0.037 (*) | 0.024 | 0.037 | 0.847 |
| Screw type | 0.066 | 0.276 | 0.599 | 0.049 | 0.158 | 0.691 |
| Complications | 0.039 | 0.096 | 0.756 | 0.017 | 0.019 | 0.892 |
| ASA | 0.321 | 0.606 | 0.086 | 0.244 | 3.809 | 0.283 |
| Reposition Level | 0.729 | 34.015 | 0.135 | 0.855 | 46.761 | 0.007 (**) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saravi, B.; Ülkümen, S.; Couillard-Despres, S.; Lang, G.; Hassel, F. One-Year Clinical Outcomes of Minimal-Invasive Dorsal Percutaneous Fixation of Thoracolumbar Spine Fractures. Medicina 2022, 58, 606. https://doi.org/10.3390/medicina58050606
Saravi B, Ülkümen S, Couillard-Despres S, Lang G, Hassel F. One-Year Clinical Outcomes of Minimal-Invasive Dorsal Percutaneous Fixation of Thoracolumbar Spine Fractures. Medicina. 2022; 58(5):606. https://doi.org/10.3390/medicina58050606
Chicago/Turabian StyleSaravi, Babak, Sara Ülkümen, Sebastien Couillard-Despres, Gernot Lang, and Frank Hassel. 2022. "One-Year Clinical Outcomes of Minimal-Invasive Dorsal Percutaneous Fixation of Thoracolumbar Spine Fractures" Medicina 58, no. 5: 606. https://doi.org/10.3390/medicina58050606
APA StyleSaravi, B., Ülkümen, S., Couillard-Despres, S., Lang, G., & Hassel, F. (2022). One-Year Clinical Outcomes of Minimal-Invasive Dorsal Percutaneous Fixation of Thoracolumbar Spine Fractures. Medicina, 58(5), 606. https://doi.org/10.3390/medicina58050606








