Acetabular Peri-Prosthetic Fractures—A Narrative Review
Abstract
:1. Introduction
2. Classification of Peri-Prosthetic Acetabular Fractures
3. Diagnosis
4. Treatment
4.1. Intra-Operative Fractures
4.2. Post-Operative Fractures
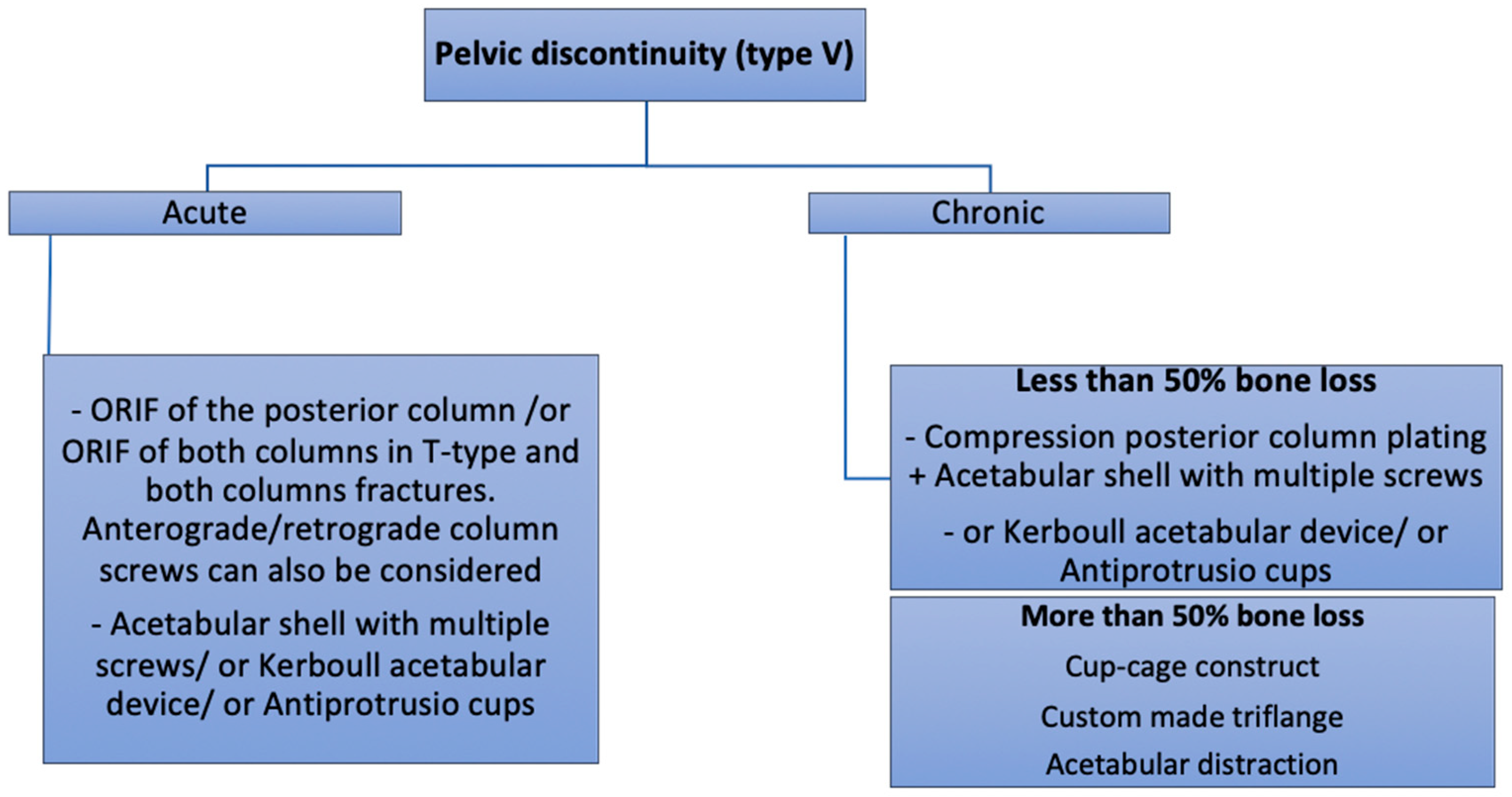
4.3. Pelvic Discontinuity (PD)
- The “Cup-cage construct” technique, currently the most popular treatment of chronic PD [42], was first described by Hanssen and Lewallen in 2005 [44]. It consists of an ilio-ischial cage, placed over an uncemented highly porous metal cup. In a majority of the cases, “jumbo cups”, defined by von Roth et al. [45] as an acetabular component with an outside diameter ≥66 mm in men and ≥62 mm in women, are used and thus help restore the centre of rotation (COR) of the hip in an anatomic position [46,47]. Remaining bone defects can be filled with augments or allograft. The cage offers initial stability and allows the osteointegration of the acetabular component. A polyethylene liner is then cemented in the cage in the correct position. Advantages of this technique are its favourable outcomes and high survival rates, ranging from 75–100% [37,42,48,49,50,51,52]. The main complications of this technique are dislocation (7–8%), infection (4–7%) and aseptic loosening (4–15%) [37,42,48,49].
- Acetabular distraction was first described by Sporer et al. in 2012 [53]. The acetabulum is reamed until the antero-superior and postero-inferior margins are engaged. Remaining bone defects are filed with porous tantalum augments. An acetabular component of the same material, 6–8 mm larger than the last reamer is then impacted. The distraction creates a press fit and a pelvic recoil as a result of ligamentotaxis [54]. The latter in conjunction with multiple screws inserted in the remaining ilium and ischium provides initial stability. The polyethylene liner or a dual mobility cup is then cemented into the shell [53]. Although relatively new, acetabular distraction is a promising treatment for chronic PD. Excellent results [40,42,53,55], with low complication rates, 3–5% aseptic loosening [40,53], have been reported at 2- to 7-year follow-up.
- Custom-made triflange implants are another option to address chronic PD with severe bone loss. Based on a preoperative CT scan, an individually produced titanium, porous and/or hydroxyapatatite-coated triflange cup is made. Through the fixation of the three flanges (ilial, ischial and pubic), initial stability with the hip COR in anatomic position can be achieved. Excellent results and >80% survivorship of the implants are reported [42,56,57,58]. The disadvantages of this implant are high costs, long manufacture time (6 weeks) and the high rates of dislocation, up to 21% [42,56,57].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peterson, C.A.; Lewallen, D.G. Periprosthetic Fracture of the Acetabulum after Total Hip Arthroplasty*. J. Bone Jt. Surg. 1996, 78, 1206–1213. [Google Scholar] [CrossRef] [PubMed]
- Cook, R.E.; Jenkins, P.J.; Walmsley, P.J.; Patton, J.T.; Robinson, C.M. Risk factors for Periprosthetic Fractures of the Hip: A Survivorship Analysis. Clin. Orthop. Relat. Res. 2008, 466, 1652–1656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Graves, S.; Pratt, N.; Roughead, L.; Nemes, S. Increase in Total Joint Arthroplasty Projected from 2014 to 2046 in Australia: A Conservative Local Model With International Implications. Clin. Orthop. Relat. Res. 2017, 475, 2130–2137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, A.D.; Pavlou, G.; Mújica-Mota, R.E.; Toms, A.D. The epidemiology of revision total knee and hip arthroplasty in England and Wales. Bone Jt. J. 2015, 97-B, 1076–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haidukewych, G.J.; Jacofsky, D.J.; Hanssen, A.D.; Lewallen, D.G. Intraoperative Fractures of the Acetabulum during Primary Total Hip Arthroplasty. J. Bone Jt. Surg. 2006, 88, 1952–1956. [Google Scholar]
- Sharkey, P.F.; Hozack, W.J.; Callaghan, J.J.; Kim, Y.S.; Berry, D.J.; Hanssen, A.D.; LeWallen, D.G. Acetabular fracture associated with cementless acetabular component insertion: A report of 13 cases. J. Arthroplast. 1999, 14, 426–431. [Google Scholar] [CrossRef]
- Basilico, M.; Vitiello, R.; Oliva, M.S.; Covino, M.; Greco, T.; Cianni, L.; Dughiero, G.; Ziranu, A.; Perisano, C.; Maccauro, G. Predictable risk factors for infections in proximal femur fractures. J. Biol. Regul. Homeost. Agents 2020, 34, 77–81. [Google Scholar]
- Sánchez-Sotelo, J.; McGrory, B.J.; Berry, D.J. Acute periprosthetic fracture of the acetabulum associated with osteolytic pelvic lesions: A report of 3 cases. J. Arthroplast. 2000, 15, 126–130. [Google Scholar] [CrossRef]
- Acharya, M.; Elnahal, W.A. Strategies of management of traumatic periprosthetic acetabular fractures around a pre-existing total hip arthroplasty. J. Clin. Orthop. Trauma 2020, 11, 1053–1060. [Google Scholar] [CrossRef]
- Vitiello, R.; Bocchi, M.B.; Gessi, M.; Greco, T.; Cianni, L.; de Maio, F.; Pesce, V.; Maccauro, G.; Perisano, C. Induced membrane by silver-coated knee megaprosthesis: Keep or toss? J. Biol. Regul. Homeost. Agents 2021, 34, 101–106. [Google Scholar]
- Berry, D.J.; Lewallen, D.G.; Hanssen, A.D.; Cabanela, M.E. Pelvic Discontinuity in Revision Total Hip Arthroplasty*. J. Bone Jt. Surg. 1999, 81, 1692–1702. [Google Scholar] [CrossRef] [PubMed]
- Springer, B.D.; Berry, D.J.; Cabanela, M.E.; Hanssen, A.D.; Lewallen, D.G. Early Postoperative Transverse Pelvic Fracture. J. Bone Jt. Surg. 2005, 87, 2626–2631. [Google Scholar] [CrossRef]
- Huch, K.; Müller, K.A.C.; Stürmer, T.; Brenner, H.; Puhl, W.; Günther, K.-P. Sports activities 5 years after total knee or hip arthroplasty: The Ulm Osteoarthritis Study. Ann. Rheum. Dis. 2005, 64, 1715–1720. [Google Scholar] [CrossRef] [PubMed]
- Callaghan, J.J.; Kim, Y.S.; Pedersen, D.R.; Brown, T.D. PERIPROSTHETIC FRACTURES OF THE ACETABULUM. Orthop. Clin. N. Am. 1999, 30, 221–234. [Google Scholar] [CrossRef]
- della Valle, C.J.; Momberger, N.G.; Paprosky, W.G. Periprosthetic fractures of the acetabulum associated with a total hip arthroplasty. Instr. Course Lect. 2003, 52, 281–290. [Google Scholar]
- Pascarella, R.; Sangiovanni, P.; Cerbasi, S.; Fantasia, R.; Consonni, O.; Zottola, V.; Panella, A.; Moretti, B. Periprosthetic acetabular fractures: A New classification proposal. Injury 2018, 49, S65–S73. [Google Scholar] [CrossRef]
- Duncan, C.P.; Haddad, F.S. The Unified Classification System (UCS): Improving our understanding of periprosthetic fractures. Bone Jt. J. 2014, 96, 713–716. [Google Scholar] [CrossRef]
- Judet, R.; Judet, J.; Letournel, E. Fractures of the acetabulum: Classification and surgical approaches for open reduction. preliminary report. J. Bone Jt. Surg. 1964, 46, 1615–1646. [Google Scholar] [CrossRef]
- della Valle, C.J.; Haidukewych, G.J.; Callaghan, J.J. Periprosthetic fractures of the hip and knee: A problem on the rise but better solutions. Instr. Course Lect. 2010, 59, 563–575. [Google Scholar]
- Stiehl, J.B. Acetabular Prosthetic Protrusion and Sepsis. J. Arthroplast. 2007, 22, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Ali, F.; Wilkinson, J.M.; Cooper, J.R.; Kerry, R.M.; Hamer, A.J.; Norman, P.; Stockley, I. Accuracy of Joint Aspiration for the Preoperative Diagnosis of Infection in Total Hip Arthroplasty. J. Arthroplast. 2006, 21, 221–226. [Google Scholar] [CrossRef]
- Benazzo, F.; Formagnana, M.; Bargagliotti, M.; Perticarini, L. Periprosthetic acetabular fractures. Int. Orthop. 2015, 39, 1959–1963. [Google Scholar] [CrossRef] [PubMed]
- Yamamuro, Y.; Kabata, T.; Kajino, Y.; Inoue, D.; Hasegawa, K.; Tsuchiya, H. Does intraoperative periprosthetic occult fracture of the acetabulum affect clinical outcomes after primary total hip arthroplasty? Arch. Orthop. Trauma Surg. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pohlemann, T.; Herath, S.C.; Braun, B.J.; Rollmann, M.F.; Histing, T.; Pizanis, A. Anterior approaches to the acetabulum: Which one to choose? EFORT Open Rev. 2020, 5, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Keel, M.J.B.; Ecker, T.M.; Cullmann, J.L.; Bergmann, M.; Bonel, H.M.; Büchler, L.; Siebenrock, K.A.; Bastian, J.D. The Pararectus approach for anterior intrapelvic management of acetabular fractures. J. Bone Jt. Surg. Br. Vol. 2012, 94, 405–411. [Google Scholar] [CrossRef]
- Bastian, J.; Savic, M.; Cullmann, J.; Zech, W.; Djonov, V.; Keel, M. Surgical exposures and options for instrumentation in acetabular fracture fixation: Pararectus approach versus the modified Stoppa. Injury 2016, 47, 695–701. [Google Scholar] [CrossRef]
- Cole, J.D.; Bolhofner, B.R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin. Orthop. Relat. Res. 1994, 1994, 112–123. [Google Scholar] [CrossRef]
- Chitre, A.; Jones, H.W.; Shah, N.; Clayson, A. Complications of total hip arthroplasty: Periprosthetic fractures of the acetabulum. Curr. Rev. Musculoskelet. Med. 2013, 6, 357–363. [Google Scholar] [CrossRef] [Green Version]
- Hickerson, L.E.; Zbeda, R.M.; Gadinsky, N.E.; Wellman, D.S.; Helfet, D.L. Outcomes of Surgical Treatment of Periprosthetic Acetabular Fractures. J. Orthop. Trauma 2019, 33, S49–S54. [Google Scholar] [CrossRef]
- Helfet, D.L.; Ali, A. Periprosthetic fractures of the acetabulum. Instr. Course Lect. 2004, 53, 93–98. [Google Scholar] [PubMed]
- Eisler, T.; Svensson, O.; Muren, C.; Elmstedt, E. Early loosening of the stemmed McMinn cup. J. Arthroplast. 2001, 16, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Issa, S.-P.; Biau, D.; Leclerc, P.; Babinet, A.; Hamadouche, M.; Anract, P. Stemmed acetabular cup as a salvage implant for revision total hip arthroplasty with Paprosky type IIIA and IIIB acetabular bone loss. Orthop. Traumatol. Surg. Res. 2020, 106, 589–596. [Google Scholar] [CrossRef]
- Rogers, B.A.; Whittingham-Jones, P.M.; Mitchell, P.A.; Safir, O.A.; Bircher, M.D.; Gross, A.E. The Reconstruction of Periprosthetic Pelvic Discontinuity. J. Arthroplast. 2012, 27, 1499–1506. [Google Scholar] [CrossRef] [PubMed]
- Moreland, J.R.; Bernstein, M.L. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin. Orthop. Relat. Res. 1995, 319, 141–150. [Google Scholar] [CrossRef]
- Babis, G.C.; Nikolaou, V.S. Pelvic discontinuity: A challenge to overcome. EFORT Open Rev. 2021, 6, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.R.; Barrett, I.; Sierra, R.J.; Lewallen, D.G.; Berry, D.J. Construct Rigidity: Keystone for Treating Pelvic Discontinuity. J. Bone Jt. Surg. 2017, 99, e43. [Google Scholar] [CrossRef]
- Stiehl, J.B.; Saluja, R.; Diener, T. Reconstruction of major column defects and pelvic discontinuity in revision total hip arthroplasty. J. Arthroplast. 2000, 15, 849–857. [Google Scholar] [CrossRef] [Green Version]
- Makita, H.; Kerboull, M.; Inaba, Y.; Tezuka, T.; Saito, T.; Kerboull, L. Revision Total Hip Arthroplasty Using the Kerboull Acetabular Reinforcement Device and Structural Allograft for Severe Defects of the Acetabulum. J. Arthroplast. 2017, 32, 3502–3509. [Google Scholar] [CrossRef]
- Sheth, N.P.; Melnic, C.M.; Paprosky, W.G. Acetabular distraction. Bone Jt. J. 2014, 96, 36–42. [Google Scholar] [CrossRef]
- Paprosky, W.G.; O’Rourke, M.; Sporer, S.M. The Treatment of Acetabular Bone Defects with an Associated Pelvic Discontinuity. Clin. Orthop. Relat. Res. 2005, 441, 216–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malahias, M.-A.; Ma, Q.-L.; Gu, A.; Ward, S.E.; Alexiades, M.M.; Sculco, P.K. Outcomes of Acetabular Reconstructions for the Management of Chronic Pelvic Discontinuity: A Systematic Review. J. Arthroplast. 2020, 35, 1145–1153.e2. [Google Scholar] [CrossRef] [PubMed]
- Hourscht, C.; Abdelnasser, M.K.; Ahmad, S.S.; Kraler, L.; Keel, M.J.; Siebenrock, K.A.; Klenke, F.M. Reconstruction of AAOS type III and IV acetabular defects with the Ganz reinforcement ring: High failure in pelvic discontinuity. Arch. Orthop. Trauma Surg. 2017, 137, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Hanssen, A.D.; Lewallen, D.G. Modular Acetabular Augments: Composite Void Fillers. Orthopedics 2005, 28, 971–972. [Google Scholar] [CrossRef]
- Von Roth, P.; Abdel, M.P.; Harmsen, W.S.; Berry, D.J. Uncemented Jumbo Cups for Revision Total Hip Arthroplasty. J. Bone Jt. Surg. 2015, 97, 284–287. [Google Scholar] [CrossRef]
- Patel, J.; Masonis, J.; Bourne, R.; Rorabeck, C. The fate of cementless jumbo cups in revision hip arthroplasty. J. Arthroplast. 2003, 18, 129–133. [Google Scholar] [CrossRef]
- Whaley, A.L.; Berry, D.J.; Harmsen, W.S. Extra-Large Uncemented Hemispherical Acetabular Components for Revision Total Hip Arthroplasty. J. Bone Jt. Surg. 2001, 83, 1352–1357. [Google Scholar] [CrossRef]
- Konan, S.; Duncan, C.P.; Masri, B.A.; Garbuz, D.S. The Cup-Cage Reconstruction for Pelvic Discontinuity has Encouraging Patient Satisfaction and Functional Outcome at Median 6-Year Follow-Up. HIP Int. 2017, 27, 509–513. [Google Scholar] [CrossRef]
- Wang, C.; Huang, Z.; Wu, B.; Li, W.; Fang, X.; Zhang, W.-M.; Zhang, W. Cup-Cage Solution for Massive Acetabular Defects: A Systematic Review and Meta-Analysis. Orthop. Surg. 2020, 12, 701–707. [Google Scholar] [CrossRef]
- Amenabar, T.; Abdelrahman, W.; Hetaimish, B.M.; Kuzyk, P.R.; Safir, O.A.; Gross, A.E. Promising Mid-term Results With a Cup-cage Construct for Large Acetabular Defects and Pelvic Discontinuity. Clin. Orthop. Relat. Res. 2016, 474, 408–414. [Google Scholar] [CrossRef] [Green Version]
- Alfaro, J.J.B.; Fernández, J.S. Trabecular Metal buttress augment and the Trabecular Metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. HIP Int. 2010, 20, 119–127. [Google Scholar] [CrossRef]
- Goodman, S.; Saastamoinen, H.; Shasha, N.; Gross, A. Complications of ilioischial reconstruction rings in revision total hip arthroplasty. J. Arthroplast. 2004, 19, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Sporer, S.M.; Bottros, J.J.; Hulst, J.B.; Kancherla, V.K.; Moric, M.; Paprosky, W.G. Acetabular Distraction: An Alternative for Severe Defects with Chronic Pelvic Discontinuity? Clin. Orthop. Relat. Res. 2012, 470, 3156–3163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, N.M.; Hellman, M.; Haughom, B.H.; Shah, R.P.; Sporer, S.M.; Paprosky, W.G. Acetabular distraction. Bone Jt. J. 2014, 96, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.-Y.; Ni, M.; Ma, H.-Y.; Du, Y.-Q.; Shen, J.-M.; Chen, J.-Y.; Zhou, Y.-G.; Zhang, G.-Q. Reverse reaming distraction for acetabular reconstruction of chronic pelvic discontinuity. J. Orthop. Surg. Res. 2020, 15, 184. [Google Scholar] [CrossRef] [PubMed]
- Christie, M.J.; Barrington, S.A.; Brinson, M.F.; Ruhling, M.E.; De Boer, D.K. Bridging Massive Acetabular Defects With the Triflange Cup. Clin. Orthop. Relat. Res. 2001, 393, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Matar, H.E.; Selvaratnam, V.; Shah, N.; Wynn Jones, H. Custom triflange revision acetabular components for significant bone defects and pelvic discontinuity: Early UK experience. J. Orthop. 2020, 21, 25–30. [Google Scholar] [CrossRef]
- Taunton, M.J.; Fehring, T.K.; Edwards, P.; Bernasek, T.; Holt, G.E.; Christie, M.J. Pelvic Discontinuity Treated With Custom Triflange Component: A Reliable Option. Clin. Orthop. Relat. Res. 2012, 470, 428–434. [Google Scholar] [CrossRef] [Green Version]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beckers, G.; Djebara, A.-E.; Gauthier, M.; Lubbeke, A.; Gamulin, A.; Zingg, M.; Bastian, J.D.; Hannouche, D. Acetabular Peri-Prosthetic Fractures—A Narrative Review. Medicina 2022, 58, 630. https://doi.org/10.3390/medicina58050630
Beckers G, Djebara A-E, Gauthier M, Lubbeke A, Gamulin A, Zingg M, Bastian JD, Hannouche D. Acetabular Peri-Prosthetic Fractures—A Narrative Review. Medicina. 2022; 58(5):630. https://doi.org/10.3390/medicina58050630
Chicago/Turabian StyleBeckers, Gautier, Az-Eddine Djebara, Morgan Gauthier, Anne Lubbeke, Axel Gamulin, Matthieu Zingg, Johannes Dominik Bastian, and Didier Hannouche. 2022. "Acetabular Peri-Prosthetic Fractures—A Narrative Review" Medicina 58, no. 5: 630. https://doi.org/10.3390/medicina58050630
APA StyleBeckers, G., Djebara, A. -E., Gauthier, M., Lubbeke, A., Gamulin, A., Zingg, M., Bastian, J. D., & Hannouche, D. (2022). Acetabular Peri-Prosthetic Fractures—A Narrative Review. Medicina, 58(5), 630. https://doi.org/10.3390/medicina58050630






