A Survey on the Use of Artificial Intelligence by Clinicians in Dentistry and Oral and Maxillofacial Surgery
Abstract
:1. Introduction
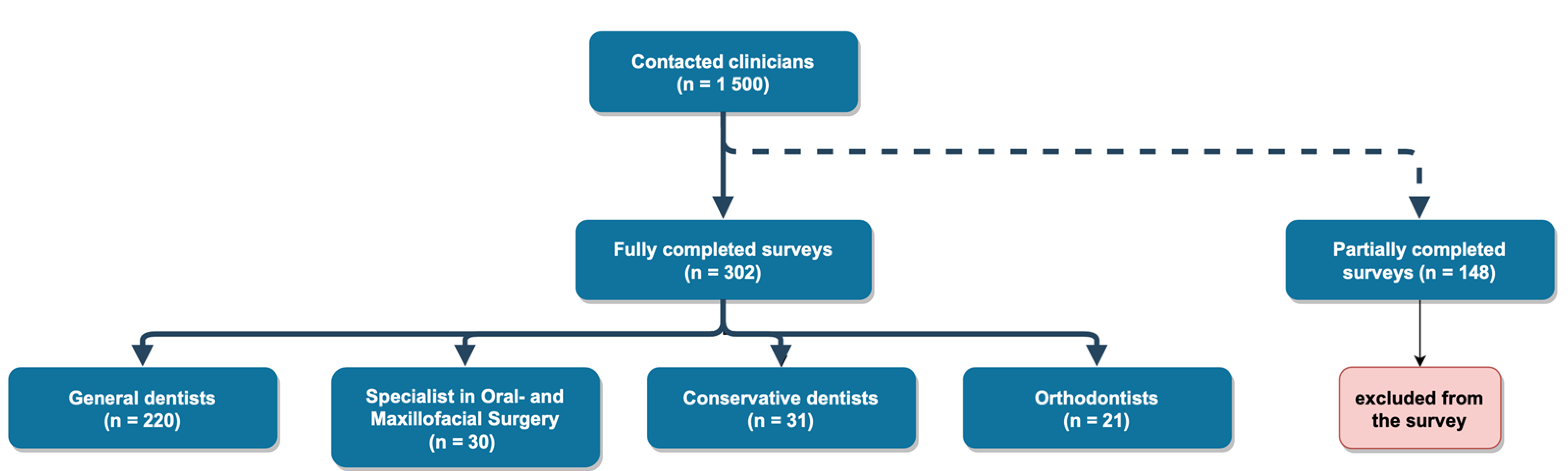
2. Materials and Methods
2.1. Sample Size
2.2. Study Design
2.3. Statistical Analysis
3. Results
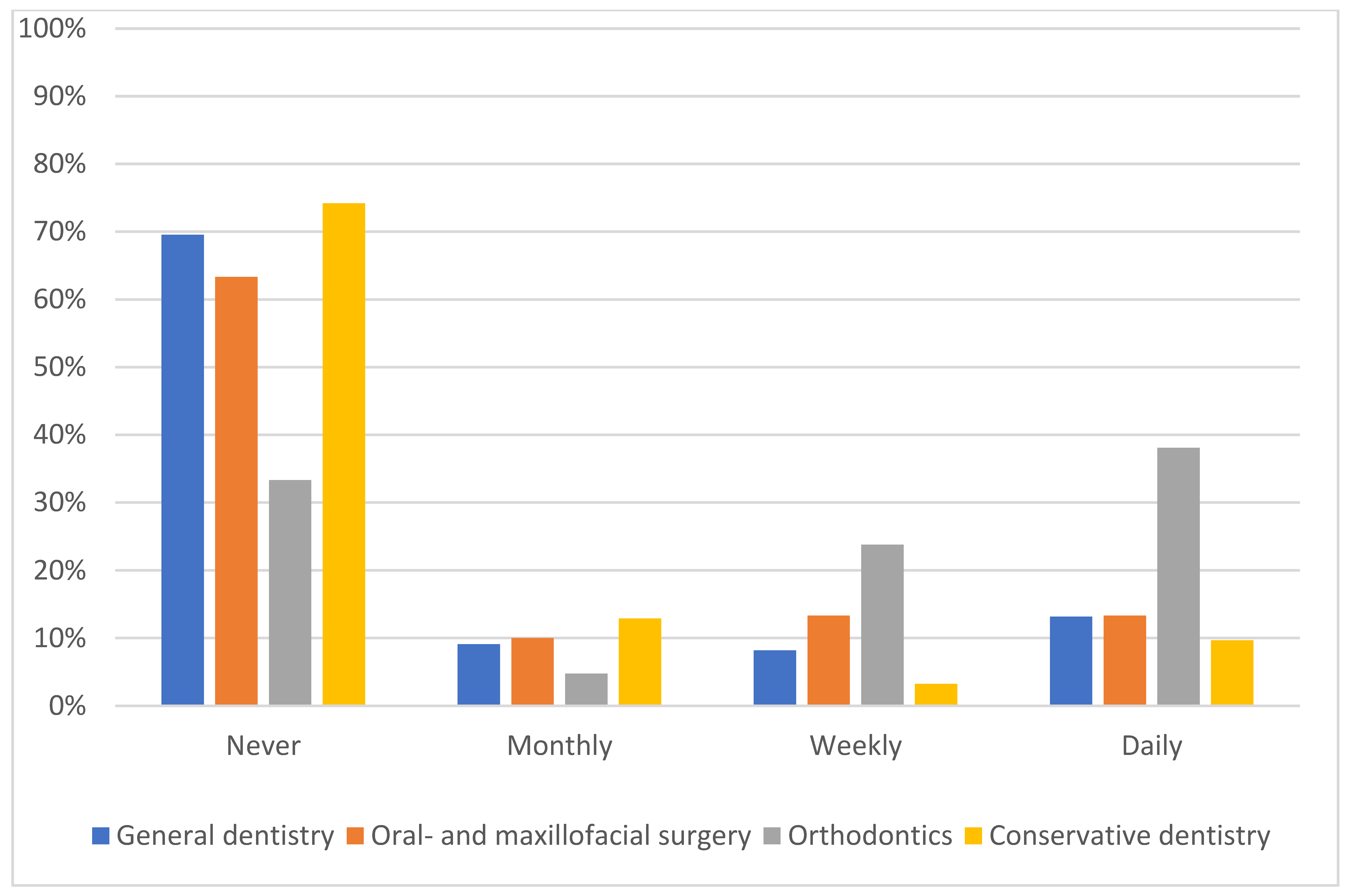
3.1. Status of Knowledge and Use of AI in the Daily Workflow
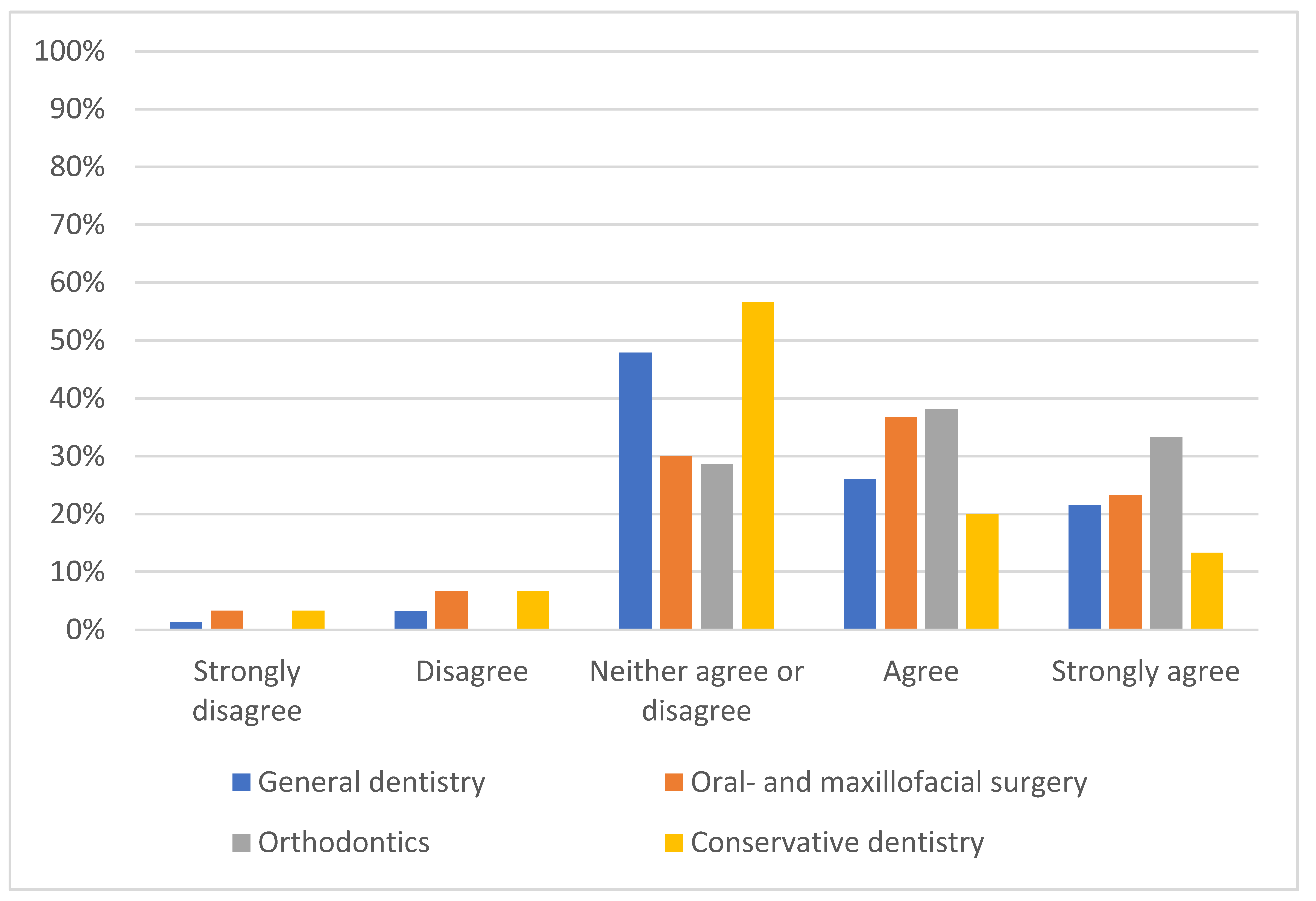
3.2. Predicted Impact of AI
3.3. Tolerance Level of Faulty AI Performance
3.4. Perceived Advantages of AI
3.5. Perceived Concerns over AI
3.6. Perceived Preparation of the Workplace for the Introduction of AI
4. Discussion
Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. | How old are you? | 18–25 | 26–45 | 46–60 | ||||
| 2. | What is your profession? | General dentistry | Periodontology | |||||
| Oral- or maxillofacial surgery | Orthodontics | |||||||
| Endodontics | Pedodontics | |||||||
| Other: | [text] | |||||||
| 3. | Since when do work in your profession? | In training | <5 years | 5–10 years | ||||
| 20–30 years | <30 years | |||||||
| 4. | Work environment | Rural | Urban | Somewhat rural | Somewhat urban | |||
| 5. | How often do you use artificial intelligence in your daily work? | Never | Monthly | Weekly | ||||
| 6. | What are the areas of application you use AI for? | [text] | ||||||
| 7. | In comparison to your colleagues in your profession how would you rate your knowledge in the topic of AI and it’s application possibilities in your profession? | Excellent | Above average | |||||
| Average | Below average | |||||||
| Very poor | ||||||||
| 8. | How long will it take in your opinion until AI has a noticeable impact on your profession? | <1 year | 1–5 years | |||||
| 5–10 years | >10 years | |||||||
| never | ||||||||
| 9. | To what extent do you expect AI to impact the workforce needed in your profession in this decade? | To a great extent | Somewhat | Very little | ||||
| 10. | To what extent do you expect AI to impact the workforce needed in your profession in the next decade? | To a great extent | Somewhat | Very little | ||||
| 11. | How will AI impact the workforce needed? | Increase | Decrease | None | ||||
| 12. | Is your profession adequately equipped for the application of AI? | Yes | No | Unsure | ||||
| 13. | What measures should be taken to prepare your profession for the application of AI? | [text] | ||||||
| 14. | What degree of error tolerance is acceptable for an AI based model that is used for disease screening by non-specialized health care workers? | Equivalent to the worst performing | Equivalent to the average performing | |||||
| Superior to the average performing | Equivalent to the best performing | |||||||
| Superior to the best performing | ||||||||
| 15. | What degree of error tolerance is acceptable for an AI based model that is used for support of a diagnostic decision by specialists? | Equivalent to the worst performing | Equivalent to the average performing | |||||
| Superior to the average performing | Equivalent to the best performing | |||||||
| Superior to the best performing | ||||||||
| 16. | Can you imagine implementing the following workflow in your clinical life: Radiographs of a patient are diagnosed by an AI. A specialist evaluates the radiographs and the AI’s findings. | Yes | No | Unsure | ||||
| 17. | Which of the following advantages regarding the application of AI in clinical life are most important? Evaluate from 1–5 (1 = least significant, 5 = most significant) | Better access to disease-screening | More targeted referrals | |||||
| More cost-efficient healthcare | Better diagnostics | |||||||
| Less time-consuming monotonous tasks | More consistent diagnostics | |||||||
| More individual and evidence-based treatment | Better prediction of the course of disease | |||||||
| 18. | Which of the following aspect are the most concerning regarding the application of AI in clincal life? Evaluate from 1–5 (1 = most concerning, 5 = least concerning) | Concerns regarding the outsouring of the steps of procedure to large data and technology companies | Privacy and data security concerns | |||||
| Concerns over accountability and responsibility in case of machine errors | Lack of trust in diagnostic capability of the AI | |||||||
| Reduced demand for specialist groups | Challenge for the patient–doctor relationship | |||||||
| Concerns regarding the benchmarking between clinicians and AI | Consequences for the workforce | |||||||
| 19. | Which of the following professions will profit most of the introduction of AI? | Endodontics | Orthodontics | |||||
| Pedodontics | Conservative Dentistry | |||||||
| Oral- and maxillofacial surgery | Periodontics | |||||||
| Prosthodontics | Other: [text] | |||||||
| 20. | To what extent do you agree with the following statement:„The introduction of AI will lead to improvement in my profession.” | Strongly agree | Agree | |||||
| Neither agree or disagree | Disagree | |||||||
| Strongly disagree | ||||||||
| 21. | To what extent do you agree with the following statement:„The introduction of AI will reduce iatrogenic errors in my profession.” | Strongly agree | Agree | |||||
| Neither agree or disagree | Disagree | |||||||
| Strongly disagree | ||||||||
References
- Pesapane, F.; Codari, M.; Sardanelli, F. Artificial intelligence in medical imaging: Threat or opportunity? Radiologists again at the forefront of innovation in medicine. Eur. Radiol. Exp. 2018, 2, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Bin Halim, M.S.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. Biomed Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef]
- Chen, Y.-W.; Stanley, K.; Att, W. Artificial intelligence in dentistry: Current applications and future per-spectives. Quintessence Int. 2020, 51, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.-P.; Samala, R.K.; Hadjiiski, L.M.; Zhou, C. Deep Learning in Medical Image Analysis. Adv. Exp. Med. Biol. 2020, 1213, 3–21. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef]
- Chan, H.-P.; Hadjiiski, L.M.; Samala, R.K. Computer-aided diagnosis in the era of deep learning. Med. Phys. 2020, 47, e218–e227. [Google Scholar] [CrossRef]
- Van Leeuwen, K.G.; de Rooij, M.; Schalekamp, S.; van Ginneken, B.; Rutten, M.J.C.M. How does artificial intelligence in radiology improve efficiency and health outcomes? Pediatr. Radiol. 2021, 1–7. [Google Scholar] [CrossRef]
- Thanathornwong, B. Bayesian-Based Decision Support System for Assessing the Needs for Orthodontic Treatment. Healthc. Inform. Res. 2018, 24, 22–28. [Google Scholar] [CrossRef]
- Lu, C.; Lewis, J.S.; Dupont, W.D.; Plummber, W.D.; Janowczyk, A.; Madabhushi, A. An oral cavity squamous cell carcinoma quantitative histomorphometric-based image classifier of nuclear morphology can risk stratify patients for disease-specific survival. Mod. Pathol. 2017, 30, 1655–1665. [Google Scholar] [CrossRef]
- Cantu, A.G.; Gehrung, S.; Krois, J.; Chaurasia, A.; Rossi, J.G.; Gaudin, R.; Elhennawy, K.; Schwendicke, F. Detecting caries lesions of different radiographic extension on bitewings using deep learning. J. Dent. 2020, 100, 103425. [Google Scholar] [CrossRef]
- Saghiri, M.A.; Garcia-Godoy, F.; Gutmann, J.L.; Lotfi, M.; Asgar, K. The Reliability of Artificial Neural Network in Locating Minor Apical Foramen: A Cadaver Study. J. Endod. 2012, 38, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, M.; van Gerven, A.; Willems, H.; Vandemeulebroucke, A.; Leite, A.F.; Politis, C.; Jacobs, R. Artificial Intelligence (AI)-Driven Molar Angulation Measurements to Predict Third Molar Eruption on Panoramic Radiographs. Int. J. Environ. Res. Public Health 2020, 17, 3716. [Google Scholar] [CrossRef]
- Gerke, S.; Babic, B.; Evgeniou, T.; Cohen, I.G. The need for a system view to regulate artificial intelligence/machine learning-based software as medical device. NPJ Digit. Med. 2020, 3, 53. [Google Scholar] [CrossRef] [Green Version]
- Oh, S.; Kim, J.H.; Choi, S.-W.; Lee, H.J.; Hong, J.; Kwon, S.H. Physician Confidence in Artificial Intelligence: An Online Mobile Survey. J. Med. Internet Res. 2019, 21, e12422. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, D.P.; Giese, D.; Brodehl, S.; Chon, S.H.; Staab, W.; Kleinert, R.; Maintz, D.; Baeßler, B. Medical students’ attitude towards artificial intelligence: A multicentre survey. Eur. Radiol. 2019, 29, 1640–1646. [Google Scholar] [CrossRef] [PubMed]
- Litjens, G.; Kooi, T.; Bejnordi, B.E.; Setio, A.A.A.; Ciompi, F.; Ghafoorian, M.; van der Laak, J.A.W.M.; van Ginneken, B.; Sánchez, C.I. A survey on deep learning in medical image analysis. Med. Image Anal. 2017, 42, 60–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castagno, S.; Khalifa, M. Perceptions of Artificial Intelligence Among Healthcare Staff: A Qualitative Survey Study. Front. Artif. Intell. 2020, 3, 578983. [Google Scholar] [CrossRef] [PubMed]
- Sit, C.; Srinivasan, R.; Amlani, A.; Muthuswamy, K.; Azam, A.; Monzon, L.; Poon, D.S. Attitudes and perceptions of UK medical students towards artificial intelligence and radiology: A multicentre survey. Insights Imaging 2020, 11, 14. [Google Scholar] [CrossRef]
- Collado-Mesa, F.; Alvarez, E.; Arheart, K. The Role of Artificial Intelligence in Diagnostic Radiology: A Survey at a Single Radiology Residency Training Program. J. Am. Coll. Radiol. 2018, 15, 1753–1757. [Google Scholar] [CrossRef]
- Bisdas, S.; Topriceanu, C.-C.; Zakrzewska, Z.; Irimia, A.-V.; Shakallis, L.; Subhash, J.; Casapu, M.-M.; Leon-Rojas, J.; dos Santos, D.P.; Andrews, D.M.; et al. Artificial Intelligence in Medicine: A Multinational Multi-Center Survey on the Medical and Dental Students’ Perception. Front. Public Health 2021, 9, 795284. [Google Scholar] [CrossRef]
- Sur, J.; Bose, S.; Khan, F.; Dewangan, D.; Sawriya, E.; Roul, A. Knowledge, attitudes, and perceptions regarding the future of artificial intelligence in oral radiology in India: A survey. Imaging Sci. Dent. 2020, 50, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Scheetz, J.; Rothschild, P.; McGuinness, M.; Hadoux, X.; Soyer, H.P.; Janda, M.; Condon, J.J.J.; Oakden-Rayner, L.; Palmer, L.J.; Keel, S.; et al. A survey of clinicians on the use of artificial intelligence in ophthalmology, dermatology, radiology and radiation oncology. Sci. Rep. 2021, 11, 5193. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, R.; Del Rey, Y.C. Attitude of Brazilian dentists and dental students regarding the future role of artificial intelligence in oral radiology: A multicenter survey. Dentomaxillofac. Radiol. 2021, 50, 20200461. [Google Scholar] [CrossRef] [PubMed]
- Yüzbaşıoğlu, E. Attitudes and perceptions of dental students towards artificial intelligence. J. Dent. Educ. 2021, 85, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef] [Green Version]
- Khanagar, S.B.; Al-Ehaideb, A.; Maganur, P.C.; Vishwanathaiah, S.; Patil, S.; Baeshen, H.A.; Sarode, S.C.; Bhandi, S. Developments, application, and performance of artificial intelligence in dentistry—A systematic review. J. Dent. Sci. 2021, 16, 508–522. [Google Scholar] [CrossRef]
- Woodward, T.M. Dental Radiology. Top. Companion Anim. Med. 2009, 24, 20–36. [Google Scholar] [CrossRef]
- Kulkarni, S.; Seneviratne, N.; Baig, M.S.; Khan, A.H.A. Artificial Intelligence in Medicine: Where Are We Now? Acad. Radiol. 2020, 27, 62–70. [Google Scholar] [CrossRef] [Green Version]
- Morrell, D.C.; Evans, M.E.; Morris, R.W.; Roland, M.O. The “five minute” consultation: Effect of time constraint on clinical content and patient satisfaction. BMJ 1986, 292, 870–873. [Google Scholar] [CrossRef] [Green Version]
- Like, R.; Zyzanski, S.J. Patient satisfaction with the clinical encounter: Social psychological determinants. Soc. Sci. Med. 1987, 24, 351–357. [Google Scholar] [CrossRef]
- Devito, K.L.; de Souza Barbosa, F.; Filho, W.N.F. An artificial multilayer perceptron neural network for diagnosis of proximal dental caries. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Langlotz, C.P. Will Artificial Intelligence Replace Radiologists? Radiol. Artif. Intell. 2019, 1, e190058. [Google Scholar] [CrossRef] [PubMed]
| Application | Appearance (n) | % |
|---|---|---|
| No use of AI in clinical practice | 31 | 28.7% |
| Radiology and diagnosis with radiographs | 21 | 19.4% |
| Intraoral scanning | 20 | 18.6% |
| Aligner treatment | 10 | 9.3% |
| CAD/CAM * | 9 | 8.3% |
| Implantology | 9 | 8.3% |
| Treatment planning | 8 | 7.4% |
| Total | 108 | 100% |
| Statements | Mean (SD) |
|---|---|
| Improved diagnostics | 3.7 (1.3) |
| Uniformity in diagnostics | 3.6 (1.1) |
| More individual and evidence-based health care | 3.4 (1.1) |
| Reduced time on monotonous tasks | 3.2 (1.3) |
| Improvement in disease prediction | 3.2 (1.1) |
| Improved access to disease screening | 3.1 (1.2) |
| More targeted referrals to specialists | 3.0 (1.2) |
| More cost-efficient health care | 2.9 (1.2) |
| Statements | Mean (SD) |
|---|---|
| Concerns over liability and responsibility for machine errors | 3.7 (1.3) |
| Concerns over data security and privacy issues | 3.5 (1.2) |
| Concerns over the divestment of healthcare to technology companies | 3.5 (1.3) |
| Lack of trust in the diagnostic capability of AI | 3.1 (1.0) |
| Concerns over a reduced need for specialists | 3.0 (1.2) |
| Challenge for the patient–doctor relationship | 2.8 (1.2) |
| Concerns regarding the comparison between clinicians and AI | 2.8 (1.2) |
| Negative impact on the workforce | 2.7 (1.2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eschert, T.; Schwendicke, F.; Krois, J.; Bohner, L.; Vinayahalingam, S.; Hanisch, M. A Survey on the Use of Artificial Intelligence by Clinicians in Dentistry and Oral and Maxillofacial Surgery. Medicina 2022, 58, 1059. https://doi.org/10.3390/medicina58081059
Eschert T, Schwendicke F, Krois J, Bohner L, Vinayahalingam S, Hanisch M. A Survey on the Use of Artificial Intelligence by Clinicians in Dentistry and Oral and Maxillofacial Surgery. Medicina. 2022; 58(8):1059. https://doi.org/10.3390/medicina58081059
Chicago/Turabian StyleEschert, Tim, Falk Schwendicke, Joachim Krois, Lauren Bohner, Shankeeth Vinayahalingam, and Marcel Hanisch. 2022. "A Survey on the Use of Artificial Intelligence by Clinicians in Dentistry and Oral and Maxillofacial Surgery" Medicina 58, no. 8: 1059. https://doi.org/10.3390/medicina58081059
APA StyleEschert, T., Schwendicke, F., Krois, J., Bohner, L., Vinayahalingam, S., & Hanisch, M. (2022). A Survey on the Use of Artificial Intelligence by Clinicians in Dentistry and Oral and Maxillofacial Surgery. Medicina, 58(8), 1059. https://doi.org/10.3390/medicina58081059









