Superior Mesenteric Artery Occlusion Caused by Infective Endocarditis and Worsened by Mycotic Aneurysm and Intracranial Hemorrhage: A Case Report
Abstract
:1. Introduction
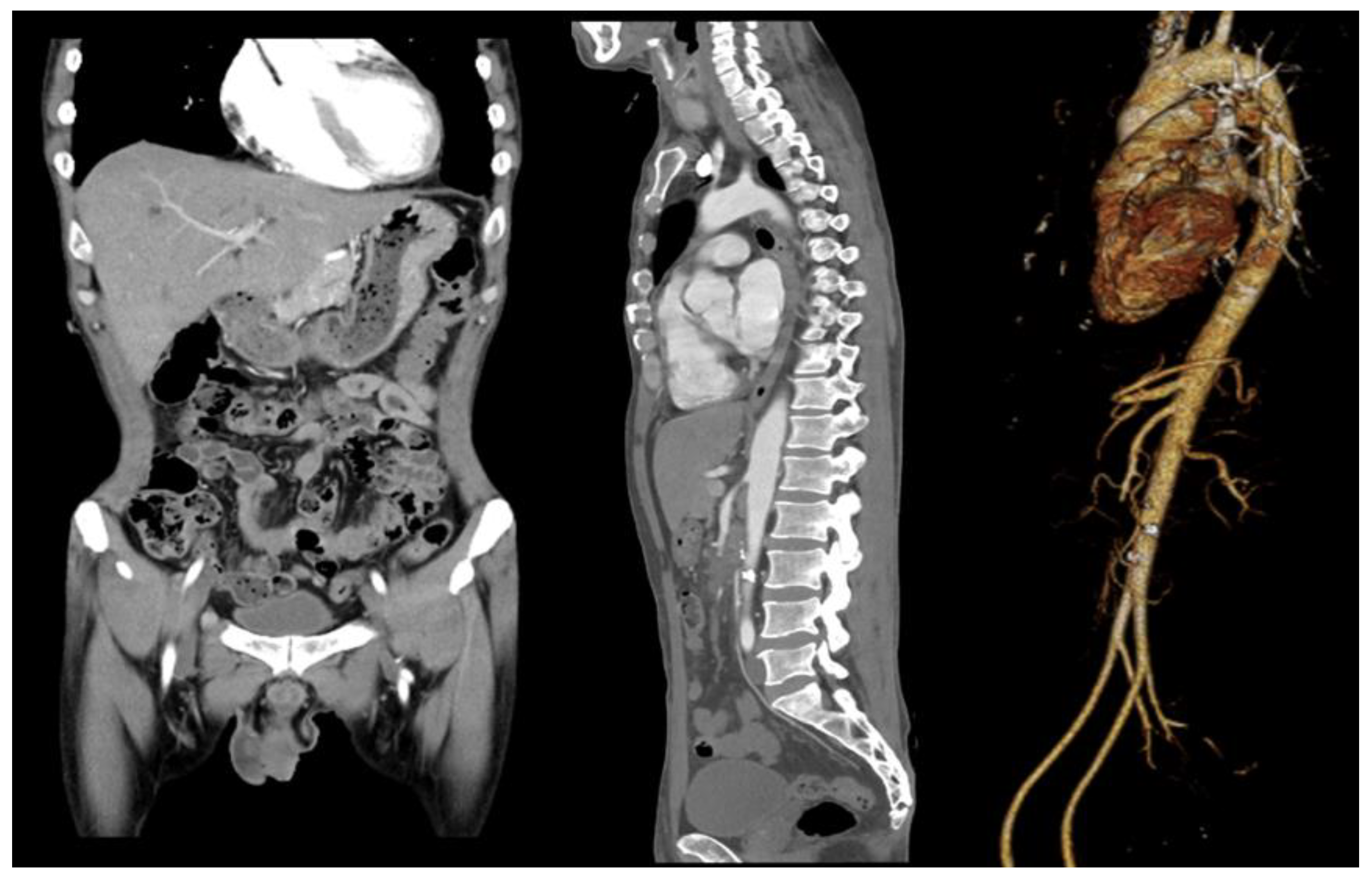
2. Case Report
3. Investigations
4. Treatment
5. Outcome and Follow Up
6. Discussion
6.1. The Patient Visited the Hospital with Abdominal Pain and Fever, and SMA Occlusion Was Diagnosed—The Patient Was Initially Observed without Surgery
6.2. Infective Endocarditis Was Found on Examination and Thoracic Surgery Was Performed
6.3. The Patient Was Treated with Anticoagulants—During Hospitalization, He Complained of Severe Headache without Neurological Symptoms, and a Brain CT Scan Showed Intracranial Hemorrhage
6.4. The Patient Was Diagnosed with SMA Aneurysm Using Abdominal CT, Which Was Followed by Persistent Abdominal Pain and Fever—Surgery Was Performed on the Transplanted Vessel
6.5. A Multidisciplinary Approach, Involving Emergency Medicine, Radiology, Thoracic Surgery, Transplant and Vascular Surgery, and Neurosurgery Specialists Was Required
7. Conclusions
- SMA occlusion is a rare disease. However, it should be considered as a cause in patients with severe abdominal pain if other causes are ruled out.
- Examining the cause of SMA occlusion is necessary, and infective endocarditis should be suspected when accompanied by fever.
- For infective endocarditis with vegetation over 10 mm, rapid valve surgery should be considered.
- Anticoagulation treatment in this disease is controversial, and side effects such as intracranial hemorrhage should always be considered.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bala, M.; Kashuk, J.; Moore, E.E.; Kluger, Y.; Biffl, W.; Gomes, C.A.; Ben-Ishay, O.; Rubinstein, C.; Balogh, Z.J.; Civil, I.; et al. Acute mesenteric ischemia: Guidelines of the World Society of Emergency Surgery. World J. Emerg. Surg. 2017, 12, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lock, G. Acute intestinal ischaemia. Best Pract. Res. Clin. Gastroenterol. 2001, 15, 83–98. [Google Scholar] [CrossRef]
- Waqas, M.; Waheed, S.; Haider, Z.; Shariff, A.H. Acute mesenteric ischaemia with infective endocarditis: Is there a role for anticoagulation? BMJ Case Rep. 2013, 2013, bcr2013009741. [Google Scholar] [CrossRef] [Green Version]
- Okonta, K.E.; Adamu, Y.B. What size of vegetation is an indication for surgery in endocarditis? Interact. Cardiovasc. Thorac. Surg. 2012, 15, 1052–1056. [Google Scholar] [CrossRef] [Green Version]
- Harrison, J.L.; Prendergast, B.D.; Habib, G. The European Society of Cardiology 2009 guidelines on the prevention, diagnosis, and treatment of infective endocarditis: Key messages for clinical practice. Pol. Arch. Med. Wewn. 2009, 119, 773–776. [Google Scholar] [CrossRef]
- Lorelli, D.R.; Cambria, R.A.; Seabrook, G.R.; Towne, J.B. Diagnosis and management of aneurysms involving the superior mesenteric artery and its branches—A report of four cases. Vasc. Endovasc. Surg. 2003, 37, 59–66. [Google Scholar] [CrossRef]
- Lai, K.M.; Rosenthal, D.; Wellons, E.D.; Bikk, A.; Franklin, J.S. Mycotic superior mesenteric aneurysm. J. Vasc. Surg. 2007, 45, 191. [Google Scholar] [CrossRef] [Green Version]
- Palmucci, S.; Mauro, L.A.; Milone, P.; Di Stefano, F.; Scolaro, A.; Di Cataldo, A.; Ettorre, G.C. Diagnosis of ruptured superior mesenteric artery aneurysm mimicking a pancreatic mass. World J. Gastroenterol. 2010, 16, 2298–2301. [Google Scholar] [CrossRef]
- de Troia, A.; Mottini, F.; Biasi, L.; Azzarone, M.; Tecchio, T.; Salcuni, P. Superior mesenteric artery aneurysm caused by aortic valve endocarditis: The case report and review of the literature. Vasc. Endovasc. Surg. 2016, 50, 88–93. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.; Oh, T.-H. Superior Mesenteric Artery Occlusion Caused by Infective Endocarditis and Worsened by Mycotic Aneurysm and Intracranial Hemorrhage: A Case Report. Medicina 2022, 58, 1585. https://doi.org/10.3390/medicina58111585
Kim C, Oh T-H. Superior Mesenteric Artery Occlusion Caused by Infective Endocarditis and Worsened by Mycotic Aneurysm and Intracranial Hemorrhage: A Case Report. Medicina. 2022; 58(11):1585. https://doi.org/10.3390/medicina58111585
Chicago/Turabian StyleKim, Changho, and Tak-Hyuk Oh. 2022. "Superior Mesenteric Artery Occlusion Caused by Infective Endocarditis and Worsened by Mycotic Aneurysm and Intracranial Hemorrhage: A Case Report" Medicina 58, no. 11: 1585. https://doi.org/10.3390/medicina58111585
APA StyleKim, C., & Oh, T. -H. (2022). Superior Mesenteric Artery Occlusion Caused by Infective Endocarditis and Worsened by Mycotic Aneurysm and Intracranial Hemorrhage: A Case Report. Medicina, 58(11), 1585. https://doi.org/10.3390/medicina58111585




