Qualitative Phytochemical Fingerprint and Network Pharmacology Investigation of Achyranthes aspera Linn. Extracts
Abstract
:1. Introduction
2. Results and Discussion
2.1. Total Phenolic and Flavonoid Contents
2.2. Characterisation of Metabolites in A. aspera Extracts
2.3. Fatty Acids
2.4. Saturated Free Fatty Acids
2.5. Monounsaturated Free Fatty Acids
2.6. Polyunsaturated Free Fatty Acids
2.7. Carboxylic, Phenolic and Acylquinic Acids, Phenylethanoid Glycosides and Flavonoids
2.8. Other Compounds
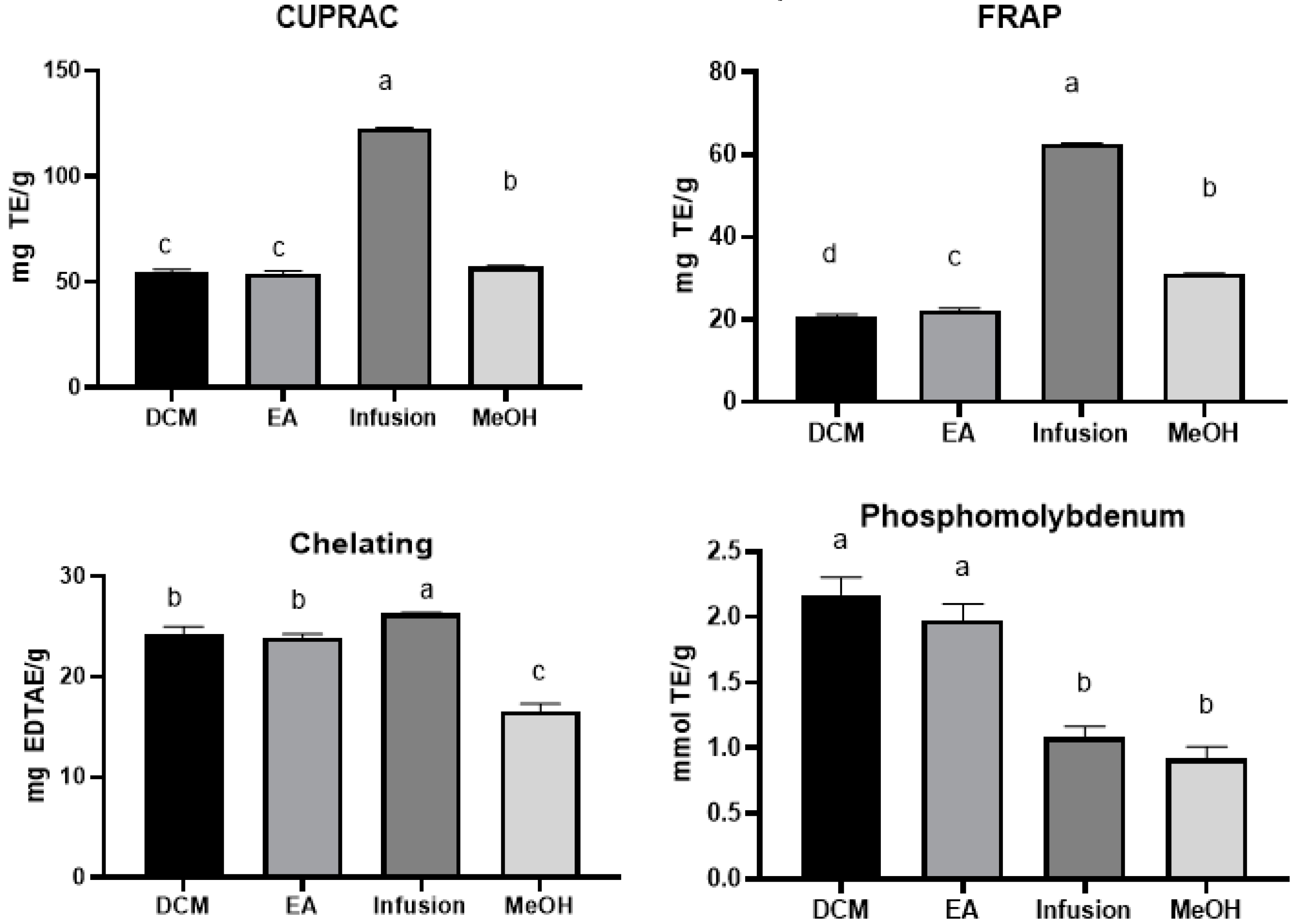
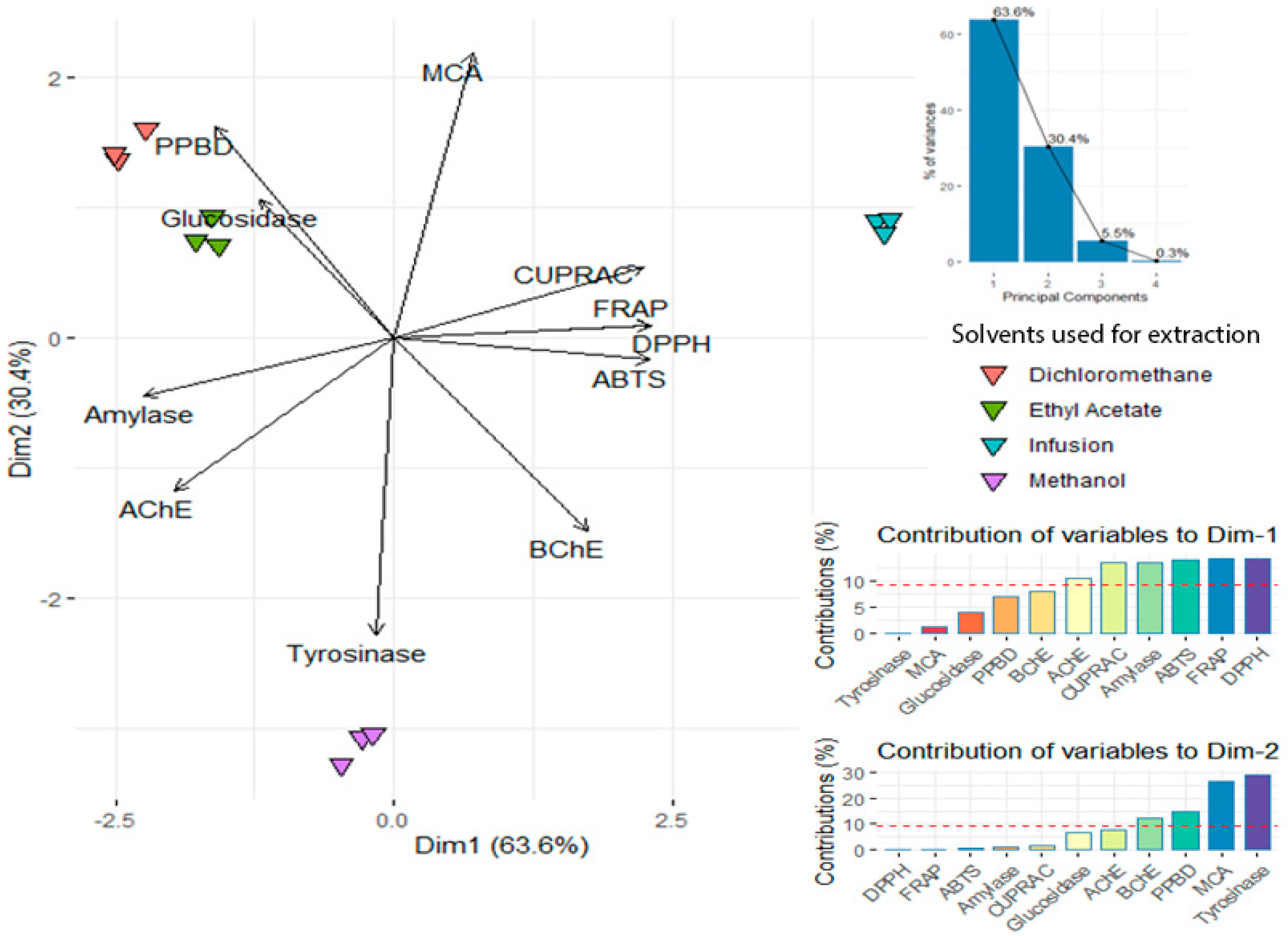
2.9. Antioxidant and Enzyme Inhibitory Effects
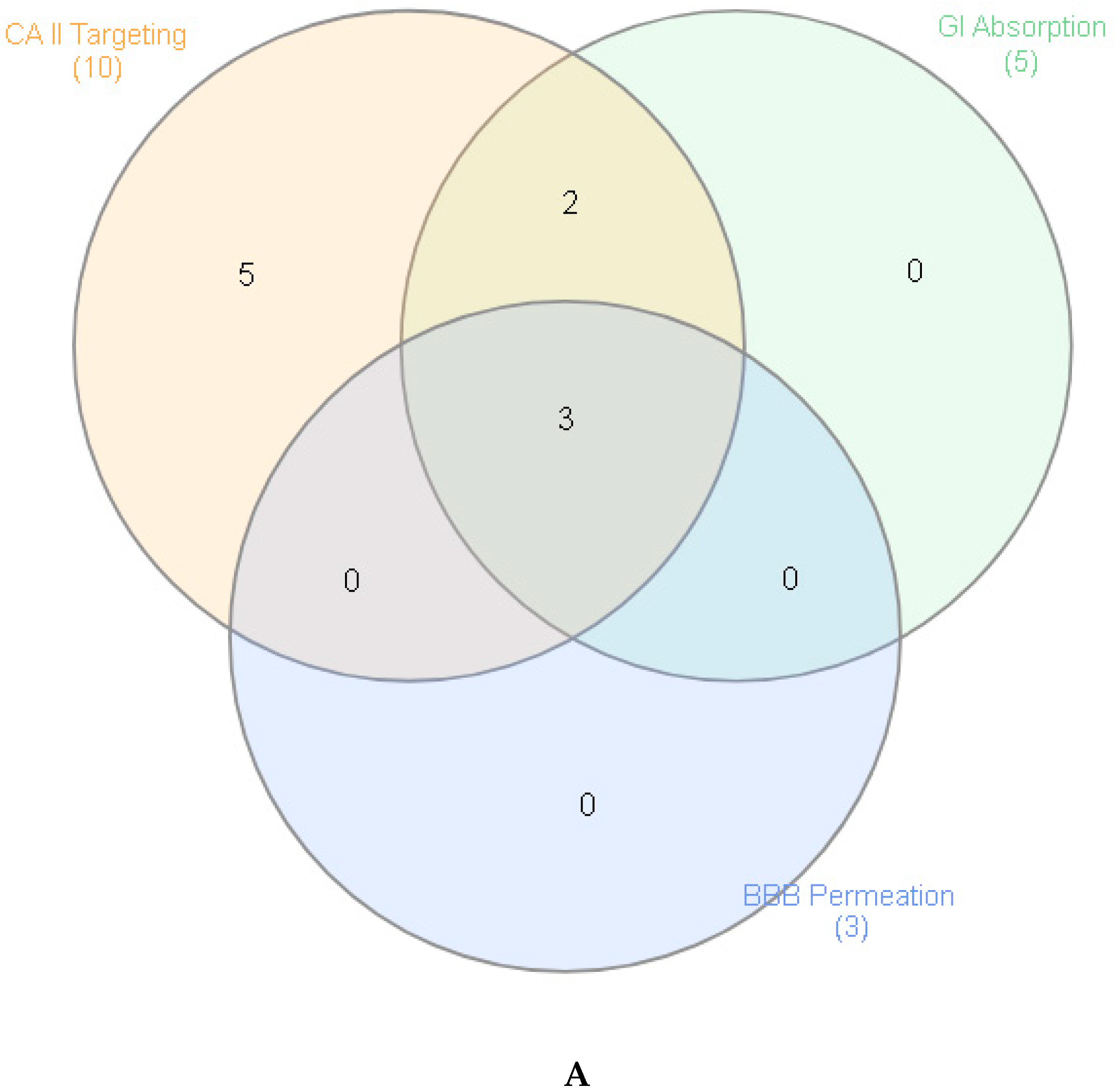
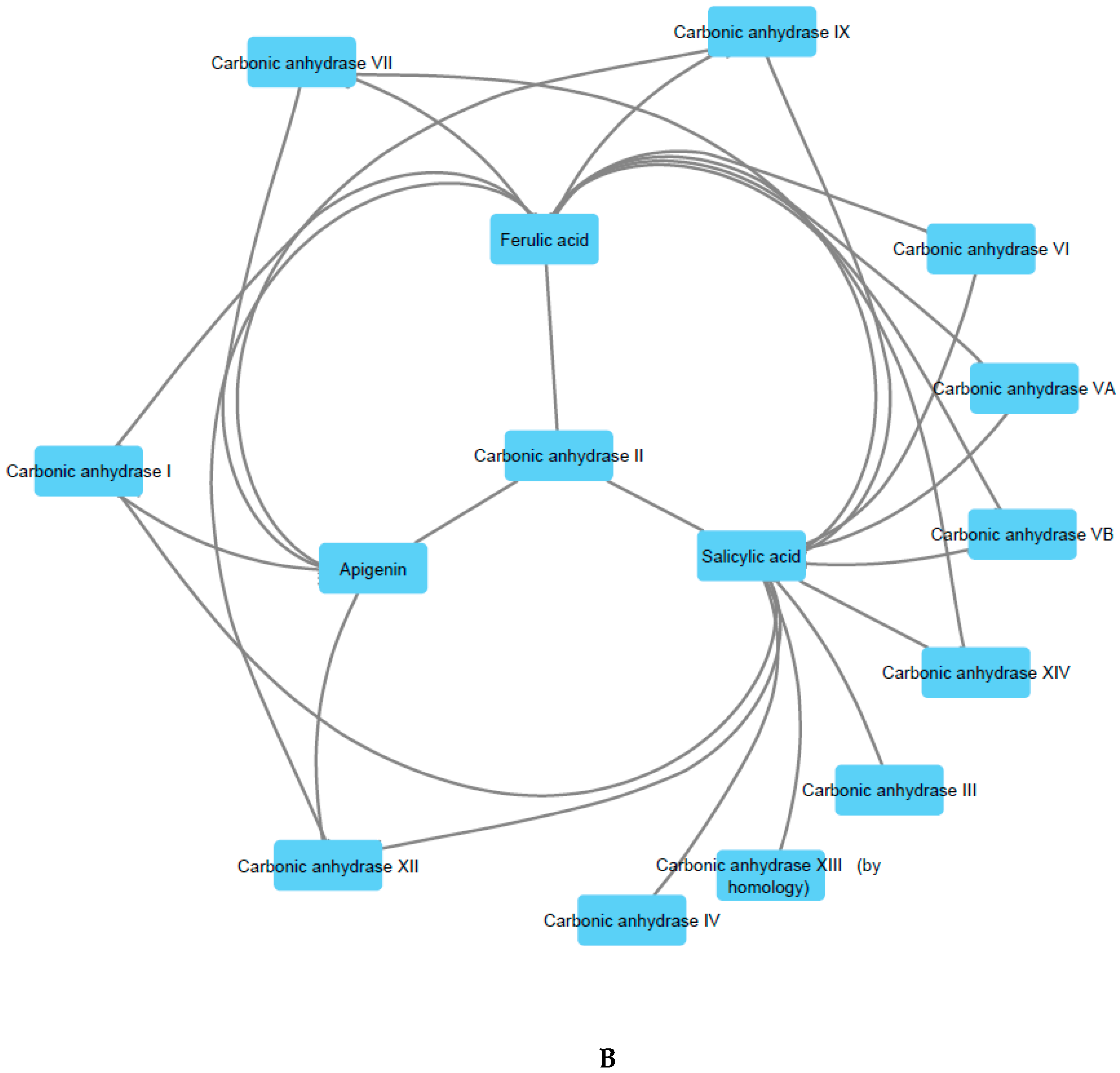
2.10. Prediction of Pharmacologic Targets and Pharmacokinetic Profile
3. Materials and Methods
3.1. Plant Material and Preparation of Extracts
3.2. Extraction
3.3. Chemical Profiling
3.4. Determination of Antioxidant and Enzyme Inhibitory Effects
3.5. Prediction of Putative Targets and Pharmacokinetics
3.6. Statistical Evaluation
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Yuyun:, M.F.; Sliwa, K.; Kengne, A.P.; Mocumbi, A.O.; Bukhman, G. Cardiovascular Diseases in Sub-Saharan Africa Compared to High-Income Countries: An Epidemiological Perspective. Global Heart 2020, 15. [Google Scholar] [CrossRef] [Green Version]
- Gowshall, M.; Taylor-Robinson, S.D. The increasing prevalence of non-communicable diseases in low-middle income countries: The view from Malawi. Int. J. Gen. Med. 2018, 11, 255. [Google Scholar] [CrossRef] [Green Version]
- Witter, S.; Zou, G.; Diaconu, K.; Senesi, R.G.; Idriss, A.; Walley, J.; Wurie, H.R. Opportunities and challenges for delivering non-communicable disease management and services in fragile and post-conflict settings: Perceptions of policy-makers and health providers in Sierra Leone. Conflict Health 2020, 14, 3. [Google Scholar] [CrossRef]
- Konkon, N.; Ouatara, D.; Kpan, W.; Kouakou, T. Medicinal plants used for treatment of diabetes by traditional practitioners in the markets of Abidjan district in Côte d’Ivoire. J. Med. Plants Stud. 2017, 5, 39–48. [Google Scholar]
- Fikru, A.; Makonnen, E.; Eguale, T.; Debella, A.; Mekonnen, G.A. Evaluation of in vivo wound healing activity of methanol extract of Achyranthes aspera L. J. Ethnopharmacol. 2012, 143, 469–474. [Google Scholar] [CrossRef] [PubMed]
- Ndhlala, A.R.; Ghebrehiwot, H.M.; Ncube, B.; Aremu, A.O.; Gruz, J.; Šubrtová, M.; Doležal, K.; du Plooy, C.P.; Abdelgadir, H.A.; Van Staden, J. Antimicrobial, anthelmintic activities and characterisation of functional phenolic acids of Achyranthes aspera linn.: A medicinal plant used for the treatment of wounds and ringworm in east africa. Front. Pharmacol. 2015, 6, 274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tahiliani, P.; Kar, A. Achyranthes aspera elevates thyroid hormone levels and decreases hepatic lipid peroxidation in male rats. J. Ethnopharmacol. 2000, 71, 527–532. [Google Scholar] [CrossRef]
- Chakraborty, A.; Brantner, A.; Mukainaka, T.; Nobukuni, Y.; Kuchide, M.; Konoshima, T.; Tokuda, H.; Nishino, H. Cancer chemopreventive activity of Achyranthes aspera leaves on Epstein–Barr virus activation and two-stage mouse skin carcinogenesis. Cancer Lett. 2002, 177, 1–5. [Google Scholar] [CrossRef]
- Vetrichelvan, T.; Jegadeesan, M. Effect of alcohol extract of Achyranthes aspera Linn. on acute and subacute inflammation. Phytother. Res. 2003, 17, 77–79. [Google Scholar] [CrossRef]
- Verma, D.; Singh, S.; Tripathi, V. Rare antibacterial activity of Achyranthes aspera Linn. Indian Drug 1997, 34, 32–35. [Google Scholar]
- Gokhale, A.; Damre, A.; Kulkarni, K.; Saraf, M. Preliminary evaluation of anti-inflammatory and anti-arthritic activity of S. lappa, A. speciosa and A. aspera. Phytomedicine 2002, 9, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Rao, Y.V.; Das, B.; Jyotyrmayee, P.; Chakrabarti, R. Effect of Achyranthes aspera on the immunity and survival of Labeo rohita infected with Aeromonas hydrophila. Fish Shellfish Immunol. 2006, 20, 263–273. [Google Scholar]
- Vasudeva, R.Y.; Duddukuri, G.R.; Sunil, B.G.; Athota, R.R. Immunomodulatory activity of Achyranthes aspera on the elicitation of antigen-specific murine antibody response. Pharm. Biol. 2002, 40, 175–178. [Google Scholar] [CrossRef]
- Edwin, S.; Jarald, E.E.; Deb, L.; Jain, A.; Kinger, H.; Dutt, K.; Raj, A.A. Wound healing and antioxidant activity of Achyranthes aspera. Pharm. Biol. 2008, 46, 824–828. [Google Scholar] [CrossRef]
- Rani, N.; Sharma, S.K.; Vasudeva, N. Assessment of antiobesity potential of Achyranthes aspera Linn. seed. Evid. Based Complement. Altern. Med. 2012, 2012. [Google Scholar]
- Gawande, D.Y.; Druzhilovsky, D.; Gupta, R.C.; Poroikov, V.; Goel, R.K. Anticonvulsant activity and acute neurotoxic profile of Achyranthes aspera Linn. J. Ethnopharmacol. 2017, 202, 97–102. [Google Scholar] [CrossRef]
- Bafna, A.; Mishra, S. Effect of methanol extract of Achyranthes aspera linn. on rifampicin-induced hepatotoxicity in rats. Ars Pharm. 2004, 45, 343–351. [Google Scholar]
- Mandefro, B.; Mereta, S.T.; Tariku, Y.; Ambelu, A. Molluscicidal effect of Achyranthes aspera L. (Amaranthaceae) aqueous extract on adult snails of Biomphalaria pfeifferi and Lymnaea natalensis. Infect. Dis. Poverty 2017, 6, 133. [Google Scholar] [CrossRef]
- Abbas, M.; Saeed, F.; Anjum, F.M.; Afzaal, M.; Tufail, T.; Bashir, M.S.; Ishtiaq, A.; Hussain, S.; Suleria, H.A.R. Natural polyphenols: An overview. Int. J. Food Properties 2017, 20, 1689–1699. [Google Scholar] [CrossRef] [Green Version]
- Bhullar, K.S.; Rupasinghe, H. Polyphenols: Multipotent therapeutic agents in neurodegenerative diseases. Oxidative Med. Cell. Longevity 2013, 2013. [Google Scholar] [CrossRef] [Green Version]
- Huo, C.; Wan, S.; Lam, W.; Li, L.; Wang, Z.; Landis-Piwowar, K.; Chen, D.; Dou, Q.; Chan, T. The challenge of developing green tea polyphenols as therapeutic agents. Inflammopharmacology 2008, 16, 248–252. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Liang, C.; Li, C.; Bu, M.; Bu, L.; Xiao, Y.; Sun, H.; Zhang, L. Simultaneous Qualitative and Quantitative Study of Main Compounds in Commelina communis Linn. by UHPLC–Q-TOF-MS-MS and HPLC–ESI-MS-MS. J. Chromatogr. Sci. 2018, 56, 582–594. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Yan, G.Y.; Wu, J.L.; Zong, X.; Liu, Z.; Zhou, H.; Liu, L.; Li, N. Qualitative and quantitative analysis of lipo-alkaloids and fatty acids in Aconitum carmichaelii using LC–MS and GC–MS. Phytochem. Anal. 2018, 29, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Clifford, M.N.; Knight, S.; Kuhnert, N. Discriminating between the six isomers of dicaffeoylquinic acid by LC-MS n. J. Agric. Food Chem. 2005, 53, 3821–3832. [Google Scholar] [CrossRef] [PubMed]
- Clifford, M.N.; Wu, W.; Kirkpatrick, J.; Kuhnert, N. Profiling the chlorogenic acids and other caffeic acid derivatives of herbal Chrysanthemum by LC− MS n. J. Agric. Food Chem. 2007, 55, 929–936. [Google Scholar] [CrossRef]
- de Rijke, E.; Out, P.; Niessen, W.M.; Ariese, F.; Gooijer, C.; Udo, A.T. Analytical separation and detection methods for flavonoids. J. Chromatogr. A 2006, 1112, 31–63. [Google Scholar] [CrossRef]
- Stevens, J.F.; Reed, R.L.; Morré, J.T. Characterization of phytoecdysteroid glycosides in meadowfoam (Limnanthes alba) seed meal by positive and negative ion LC-MS/MS. J. Agric. Food Chem. 2008, 56, 3945–3952. [Google Scholar] [CrossRef] [Green Version]
- Takemoto, T.; Hikino, Y.; Hikino, H.; Ogawa, S.; Nishimoto, N. Rubrosterone, a metabolite of insect metamorphosing substance from Achyranthes rubrofusca: Structure and absolute configuration. Tetrahedron 1969, 25, 1241–1248. [Google Scholar] [CrossRef]
- Chakrabarti, R.; Srivastava, P.K.; Kundu, K.; Khare, R.S.; Banerjee, S. Evaluation of immunostimulatory and growth promoting effect of seed fractions of Achyranthes aspera in common carp Cyprinus carpio and identification of active constituents. Fish Shellfish Immunol. 2012, 32, 839–843. [Google Scholar] [CrossRef]
- He, X.; Wang, X.; Fang, J.; Chang, Y.; Ning, N.; Guo, H.; Huang, L.; Huang, X. The genus Achyranthes: A review on traditional uses, phytochemistry, and pharmacological activities. J. Ethnopharmacol. 2017, 203, 260–278. [Google Scholar] [CrossRef]
- Yang, N.-Y.; Yang, Y.-F.; Li, K. Analysis of Hydroxy Fatty Acids from the Pollen of Brassica campestris L. var. oleifera DC. by UPLC-MS/MS. J. Pharm. 2013, 2013. [Google Scholar]
- Mao, X.; Gu, C.; Chen, D.; Yu, B.; He, J. Oxidative stress-induced diseases and tea polyphenols. Oncotarget 2017, 8, 81649. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ozsurekci, Y.; Aykac, K. Oxidative stress related diseases in newborns. Oxidative Med. Cell. Longevity 2016, 2016. [Google Scholar] [CrossRef] [Green Version]
- Adefegha, S.A.; Oboh, G.; Ejakpovi, I.I.; Oyeleye, S.I. Antioxidant and antidiabetic effects of gallic and protocatechuic acids: A structure–function perspective. Comp. Clin. Pathol. 2015, 24, 1579–1585. [Google Scholar] [CrossRef]
- Joshi, R.; Gangabhagirathi, R.; Venu, S.; Adhikari, S.; Mukherjee, T. Antioxidant activity and free radical scavenging reactions of gentisic acid: In-vitro and pulse radiolysis studies. Free Radical Res. 2012, 46, 11–20. [Google Scholar] [CrossRef]
- Ludwig, I.A.; Clifford, M.N.; Lean, M.E.; Ashihara, H.; Crozier, A. Coffee: Biochemistry and potential impact on health. Food Funct. 2014, 5, 1695–1717. [Google Scholar] [CrossRef] [PubMed]
- Moosavi, F.; Hosseini, R.; Rajaian, H.; Silva, T.; Silva, D.M.; Saso, L.; Edraki, N.; Miri, R.; Borges, F.; Firuzi, O. Derivatives of caffeic acid, a natural antioxidant, as the basis for the discovery of novel nonpeptidic neurotrophic agents. Bioorg. Med. Chem. 2017, 25, 3235–3246. [Google Scholar] [CrossRef]
- Yeh, C.-T.; Yen, G.-C. Induction of hepatic antioxidant enzymes by phenolic acids in rats is accompanied by increased levels of multidrug resistance–associated protein 3 mRNA expression. J. Nutr. 2006, 136, 11–15. [Google Scholar] [CrossRef] [Green Version]
- Hung, T.M.; Na, M.; Thuong, P.T.; Su, N.D.; Sok, D.; Song, K.S.; Seong, Y.H.; Bae, K. Antioxidant activity of caffeoyl quinic acid derivatives from the roots of Dipsacus asper Wall. J. Ethnopharmacol. 2006, 108, 188–192. [Google Scholar] [CrossRef]
- Balasundram, N.; Sundram, K.; Samman, S. Phenolic compounds in plants and agri-industrial by-products: Antioxidant activity, occurrence, and potential uses. Food Chem. 2006, 99, 191–203. [Google Scholar] [CrossRef]
- Yin, B.; Fang, D.M.; Zhou, X.L.; Gao, F. Natural products as important tyrosine kinase inhibitors. Eur. J. Med. Chem. 2019, 182, 111664. [Google Scholar] [CrossRef] [PubMed]
- Dorababu, A. Critical Evaluation of Current Alzheimer′ s Drug Discovery (2018-19) & Futuristic Alzheimer drug model approach. Bioorg. Chem. 2019, 103299. [Google Scholar]
- Sun, L.; Warren, F.J.; Gidley, M.J. Natural products for glycaemic control: Polyphenols as inhibitors of alpha-amylase. Trends Food Sci. Technol. 2019, 91, 262–273. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Biswas, R.; Sharma, A.; Banerjee, S.; Biswas, S.; Katiyar, C.K. Validation of medicinal herbs for anti-tyrosinase potential. J. Herbal Med. 2018, 14, 1–16. [Google Scholar] [CrossRef]
- Adefegha, S.A.; Oboh, G.; Omojokun, O.S.; Adefegha, O.M. Alterations of Na+/K+-ATPase, cholinergic and antioxidant enzymes activity by protocatechuic acid in cadmium-induced neurotoxicity and oxidative stress in Wistar rats. Biomed. Pharmacother. 2016, 83, 559–568. [Google Scholar] [CrossRef]
- Srinivasulu, N.; Mallaiah, P.; Sudhakara, G.; Sasi, B.; Rao, S.; Kumari, D.; Kumari, S. Alpha amylase inhibitory activity and in vitro glucose uptake in psoas muscle and adipose tissue of male wistar rats of leaf methanolic extract of Achyranthes aspera. J. Pharmacognosy Phytochem. 2016, 176, 176–180. [Google Scholar]
- Ohnishi, M.; Matuo, T.; Tsuno, T.; Hosoda, A.; Nomura, E.; Taniguchi, H.; Sasaki, H.; Morishita, H. Antioxidant activity and hypoglycemic effect of ferulic acid in STZ-induced diabetic mice and KK-A mice. Biol. Factors 2004, 21, 315–319. [Google Scholar] [CrossRef]
- Santana-Galvez, J.; Cisneros-Zevallos, L.; Jacobo-Velazquez, D.A. Chlorogenic Acid: Recent Advances on Its Dual Role as a Food Additive and a Nutraceutical against Metabolic Syndrome. Molecules 2017, 22, 358. [Google Scholar] [CrossRef] [Green Version]
- Jones, W.P.; Chin, Y.-W.; Kinghorn, A.D. The role of pharmacognosy in modern medicine and pharmacy. Curr. Drug Targets 2006, 7, 247–264. [Google Scholar] [CrossRef]
- Chichiriccò, G.; Ferrante, C.; Menghini, L.; Recinella, L.; Leone, S.; Chiavaroli, A.; Brunetti, L.; Di Simone, S.; Ronci, M.; Piccone, P. Crocus sativus by-products as sources of bioactive extracts: Pharmacological and toxicological focus on anthers. Food Chem. Toxicol. 2019, 126, 7–14. [Google Scholar] [CrossRef]
- Ferrante, C.; Recinella, L.; Ronci, M.; Menghini, L.; Brunetti, L.; Chiavaroli, A.; Leone, S.; Di Iorio, L.; Carradori, S.; Tirillini, B. Multiple pharmacognostic characterization on hemp commercial cultivars: Focus on inflorescence water extract activity. Food Chem. Toxicol. 2019, 125, 452–461. [Google Scholar] [CrossRef] [PubMed]
- KANG, Y.; TERASAKI, T.; TSUJI, A. Acidic drug transport in vivo through the blood-brain barrier. A role of the transport carrier for monocarboxylic acids. J. Pharmacobio Dyn. 1990, 13, 158–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mi, Y.; Guo, S.; Cheng, H.; Liu, M.; Wei, P.; Wang, M.; Mao, Y.; Ke, G. Pharmacokinetic comparative study of tetramethylpyrazine and ferulic acid and their compatibility with different concentration of gastrodin and gastrodigenin on blood–stasis migraine model by blood–brain microdialysis method. J. Pharm. Biomed. Anal. 2020, 177, 112885. [Google Scholar] [CrossRef] [PubMed]
- Leyva-López, N.; Gutierrez-Grijalva, E.P.; Ambriz-Perez, D.L.; Heredia, J.B. Flavonoids as cytokine modulators: A possible therapy for inflammation-related diseases. Int. J. Mol. Sci. 2016, 17, 921. [Google Scholar] [CrossRef] [PubMed]
- Bayram, E.; Senturk, M.; Kufrevioglu, O.I.; Supuran, C.T. In vitro inhibition of salicylic acid derivatives on human cytosolic carbonic anhydrase isozymes I and II. Bioorg. Med. Chem. 2008, 16, 9101–9105. [Google Scholar] [CrossRef] [PubMed]
- Innocenti, A.; Vullo, D.; Scozzafava, A.; Supuran, C.T. Carbonic anhydrase inhibitors: Inhibition of mammalian isoforms I–XIV with a series of substituted phenols including paracetamol and salicylic acid. Bioorg. Med. Chem. 2008, 16, 7424–7428. [Google Scholar] [CrossRef] [PubMed]
- Jakubowski, M.; Szahidewicz-Krupska, E.; Doroszko, A. The Human Carbonic Anhydrase II in Platelets: An Underestimated Field of Its Activity. Biol. Med. Res. Int. 2018, 2018. [Google Scholar] [CrossRef]
- Beyza Öztürk Sarıkaya, S.; Gülçin, İ.; Supuran, C.T. Carbonic anhydrase inhibitors: Inhibition of human erythrocyte isozymes I and II with a series of phenolic acids. Chem. Biol. Drug Des. 2010, 75, 515–520. [Google Scholar] [CrossRef]
- Karioti, A.; Carta, F.; Supuran, C.T. Phenols and polyphenols as carbonic anhydrase inhibitors. Molecules 2016, 21, 1649. [Google Scholar] [CrossRef] [Green Version]
- Chiavaroli, A.; Recinella, L.; Ferrante, C.; Locatelli, M.; Macchione, N.; Zengin, G.; Leporini, L.; Leone, S.; Martinotti, S.; Brunetti, L.; et al. Crocus sativus, Serenoa repens and Pinus massoniana extracts modulate inflammatory response in isolated rat prostate challenged with LPS. J. Biol. Regul. Homeost. Agents 2017, 31, 531–541. [Google Scholar]
- Zengin, G.; Locatelli, M.; Stefanucci, A.; Macedonio, G.; Novellino, E.; Mirzaie, S.; Dvorácskó, S.; Carradori, S.; Brunetti, L.; Orlando, G.; et al. Chemical characterization, antioxidant properties, anti-inflammatory activity, and enzyme inhibition of Ipomoea batatas L. leaf extracts. Int. J. Food Properties 2017, 20, 1907–1919. [Google Scholar] [CrossRef] [Green Version]
- Grochowski, D.M.; Uysal, S.; Aktumsek, A.; Granica, S.; Zengin, G.; Ceylan, R.; Locatelli, M.; Tomczyk, M. In vitro enzyme inhibitory properties, antioxidant activities, and phytochemical profile of Potentilla thuringiaca. Phytochem. Lett. 2017, 20, 365–372. [Google Scholar] [CrossRef]
- Gu, L.; Lu, J.; Li, Q.; Wu, N.; Zhang, L.; Li, H.; Xing, W.; Zhang, X. A network-based analysis of key pharmacological pathways of Andrographis paniculata acting on Alzheimer’s disease and experimental validation. J. Ethnopharmacol. 2020, 251, 112488. [Google Scholar] [CrossRef]
Sample Availability: Samples of the compounds are not available from the authors. |

| No | Tentative Structure | Molecular Formula | Exact Mass [M − H]− | Presence | Reference | |
|---|---|---|---|---|---|---|
| Fatty acids | ||||||
| 1 | azelaic acid | C9H16O4 | 187.0968 | 1,2,4 | [22] | |
| 2 | undecanedioic acid | C11H20O4 | 215.1285 | 1,2,3 | ||
| 3 | dodecenedioic acid (traumatic acid) | C12H20O4 | 227.1289 | 1,2,3,4 | ||
| 4 | dodecanoic acid (lauric acid) | C12H22O4 | 229.1442 | 1,2,3,4 | ||
| 5 | linolenic acid | C18H30O2 | 277.2177 | 1 | [23] | |
| 6 | 8-hydroxy-9,11,13-heptadecatrienoc acid | C17H28O3 | 279.1968 | 1,3 | ||
| 7 | 12-hydroxy-6-heptadecenoic acid | C17H30O3 | 281.2123 | 1,3 | ||
| 8 | 9-hydroxy-10,11,13,15-octadecatetranoic acid | C18H28O3 | 291.1970 | 1,3 | ||
| 9 | 13-hydroxy-9,11,15-octadecatrienoic acid | C18H30O3 | 293.2119 | 1,2,3,4 | ||
| 10 | 15-hydroxy-9,11,13-octadecatrienoic acid | C18H30O3 | 293.2126 | 1,2,3,4 | ||
| 11 | 13-hydroxy-9,11-octadecadienoic acid | C18H32O3 | 295.2280 | 1,2,3,4 | [23] | |
| 12 | 9-hydroxy-?-octadecenoic acid | C18H34O3 | 297.2438 | 1,3 | [24] | |
| 13 | 15-hydroxy-9-oxo-10,12,14-octadecatrienoic acid | C18H26O4 | 305.1762 | 1,2,3,4 | ||
| 14 | 14-hydroxy-9-oxo-11,13,15-octadecatrienoic acid | C18H28O4 | 307.1919 | 1,2,3,4 | ||
| 15 | 9,10-dihydroxy-12,14,16-octadecatrienoic acid | C18H30O4 | 309.2076 | 1,2,3,4 | ||
| 16 | 9,10-dihydroxy-11,13,16-octadecatrienoic acid | C18H30O4 | 309.2074 | 1,2,3 | ||
| 17 | 9,10-dihydroxy-12,15,16-octadecatrienoic acid | C18H30O4 | 309.2074 | 1,2,3,4 | ||
| 18 | 11,12-dihydroxy-9,14,15-octadecatrienoic acid | C18H30O4 | 309.2076 | 1,2,3,4 | ||
| 19 | 15,16-dihydroxy-9,12-octadecadienoic acid | C18H32O4 | 311.2234 | 1,3,4 | ||
| 20 | 9,10-dihydroxy-12,14-octadecadienoic acid | C18H32O4 | 311.2233 | 1,2,3,4 | ||
| 21 | 9,10-dihydroxy-10,13-octadecadienoic acid | C18H32O4 | 311.2232 | 1,2,3,4 | ||
| 22 | 12,13-dihydroxy-9-octadecenoic acid | C18H34O4 | 313.2389 | 1,2,3,4 | [23] | |
| 23 | 9,10-dihydroxy-12-octadecenoic acid | C18H34O4 | 313.2388 | 1,2,3,4 | [23] | |
| 24 | 9,10-dihydroxy-octadecanoic acid | C18H36O4 | 315.2544 | 1,2,3 | [23] | |
| 25 | 9,10,13-trihydroxy-11,15-octadecadienoic acid | C18H32O5 | 327.2179 | 1,2,3,4 | ||
| 26 | 9,12,13-trihydroxy-10,15-octadecadienoic acid | C18H32O5 | 327.2179 | 1,2,3,4 | ||
| 27 | 11,12,15-trihydroxy-9,12-octadecadienoic acid | C18H32O5 | 327.2179 | 1,2,3,4 | ||
| 28 | 11,12,13-trihydroxy-9,12-octadecadienoic acid | C18H32O5 | 327.2179 | 1,2,3,4 | ||
| 29 | 9,10,15-trihydroxy-12,15-octadecadienoic acid | C18H32O5 | 327.2179 | 1,2,3,4 | ||
| 30 | 11,12,15-trihydroxy-9,12-octadecadienoic acid | C18H32O5 | 327.2180 | 1,2,3,4 | ||
| 31 | 9,10,13-trihydroxy,12-octadecenoic acid | C18H34O5 | 329.2338 | 1,2,3,4 | [23] | |
| 32 | 9,12,13-trihydroxy,10-octadecenoic acid | C18H34O5 | 329.2338 | 1,2,3,4 | [23] | |
| Carboxylic, phenolic and acylquinic acids, and phenylethanoid glycosides | ||||||
| 33 | salicylic acid | C7H6O3 | 137.0230 | 1,2,3,4 | ||
| 34 | protocatechuic acid | C7H6O4 | 153.0184 | 1,2,3 | * | |
| 35 | gentisic acid | C7H6O4 | 153.0183 | 2,3,4 | * | |
| 36 | caffeic acid | C9H8O4 | 179.0338 | 1,2,3,4 | * | |
| 37 | quinic acid | C7H12O6 | 191.0552 | 1,2,3,4 | ||
| 38 | ferulic acid | C10H10O4 | 193.0498 | 1,2,3,4 | * | |
| 39 | salicylic acid-O-hexoside | C13H16O8 | 299.0776 | 1,2,3,4 | ||
| 40 | gentisic acid-O-hexoside | C13H16O9 | 315.0725 | 2,4 | ||
| 41 | chlorogenic (5-caffeoylquinic) acid | C16H18O9 | 353.0867 | 1,2,3,4 | * | |
| 42 | 4-caffeoylquinic acid | C16H18O9 | 353.0872 | 3,4 | ||
| 43 | 3,5-dicaffeoylquinic acid | C25H24O12 | 515.1218 | 1,2,3,4 | * | |
| 44 | 4,5-dicaffeoylquinic acid | C25H24O12 | 515.1198 | 1,2,3,4 | * | |
| 45 | 3,4,5-tricaffeoylquinic acid | C34H30O15 | 677.1532 | 1,2,3 | * | |
| Flavonoids | ||||||
| 46 | kaempferol-3-O-glucoside | C21H20O11 | 447.0941 | 1,2,3,4 | * | |
| 47 | isoquercitrin | C21H20O12 | 463.0891 | 1,2,3,4 | * | |
| 48 | apigenin-7-O-hexuronide-4’-O-rhamnoside | C27H28O15 | 591.1356 | 1,2,3,4 | ||
| 49 | kaempferol-3-O-neohesperidoside | C27H30O15 | 593.1522 | 1,2,3,4 | ||
| 50 | kaempferol-3-O-rutinoside | C27H30O15 | 593.1528 | 1,2,3,4 | * | |
| 51 | tiliroside | C30H26O13 | 593.1307 | 1,2,4 | * | |
| Other compounds | ||||||
| 52 | Roseoside corchoionoside C | C19H30O8 | 385.1884 | 1,2,3,4 | ||
| 53 | rubrosterone | C19H26O5 | 333.1680 | 1,2,3,4 | ||
| 54 | 20-hydroxyecdysterone | C27H44O7 | 479.3018 | 1,2,3,4 | [25] | |
| AChE Inhibition | BChE Inhibition | Tyrosinase Inhibition | α-Amylase Inhibition | α-Glucosidase Inhibition | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| mg GALAE/g | IC50 (mg /mL) | mg GALAE/g | IC50 (mg /mL) | Mg KAE/g | IC50 (mg /mL) | mmol ACAE/g | IC50 (mg /mL) | mmol ACAE/g | IC50 (mg /mL) | ||
| Extracts | DCM | 3.97 ± 0.36 b | 0.68 ± 0.02 b | na | na | na | na | 0.66 ± 0.03 a | 1.69 ± 0.08 b | 2.28 ± 0.17 | 0.80 ± 0.06 a |
| EA | 3.28 ± 0.21 c | 0.82 ± 0.05 c | na | na | na | na | 0.68 ± 0.01 a | 1.65 ± 0.01 b | na | na | |
| Infusion | na | na | 15.36 ± 0.22 a | 0.55 ± 0.01 b | na | na | 0.20 ± 0.01 b | >5 | na | na | |
| MeOH | 4.87 ± 0.10 a | 0.55 ± 0.01 b | 16.00 ± 0.48 a | 0.53 ± 0.01 b | 56.24 ± 5.05 | 1.90 ± 0.17 b | 0.63 ± 0.04 a | 1.78 ± 0.12 b | na | na | |
| Standards | Galatamine | 0.003 ± 0.0001 a | 0.008 ± 0.0001 a | − | − | − | |||||
| Kojic acid | − | − | 0.11 ± 0.01 a | − | − | ||||||
| Acarbose | − | − | − | 0.72 ± 0.02 a | 1.04 ± 0.08 b | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sinan, K.I.; Zengin, G.; Zheleva-Dimitrova, D.; Etienne, O.K.; Fawzi Mahomoodally, M.; Bouyahya, A.; Lobine, D.; Chiavaroli, A.; Ferrante, C.; Menghini, L.; et al. Qualitative Phytochemical Fingerprint and Network Pharmacology Investigation of Achyranthes aspera Linn. Extracts. Molecules 2020, 25, 1973. https://doi.org/10.3390/molecules25081973
Sinan KI, Zengin G, Zheleva-Dimitrova D, Etienne OK, Fawzi Mahomoodally M, Bouyahya A, Lobine D, Chiavaroli A, Ferrante C, Menghini L, et al. Qualitative Phytochemical Fingerprint and Network Pharmacology Investigation of Achyranthes aspera Linn. Extracts. Molecules. 2020; 25(8):1973. https://doi.org/10.3390/molecules25081973
Chicago/Turabian StyleSinan, Kouadio Ibrahime, Gokhan Zengin, Dimitrina Zheleva-Dimitrova, Ouattara Katinan Etienne, Mohamad Fawzi Mahomoodally, Abdelhakim Bouyahya, Devina Lobine, Annalisa Chiavaroli, Claudio Ferrante, Luigi Menghini, and et al. 2020. "Qualitative Phytochemical Fingerprint and Network Pharmacology Investigation of Achyranthes aspera Linn. Extracts" Molecules 25, no. 8: 1973. https://doi.org/10.3390/molecules25081973










