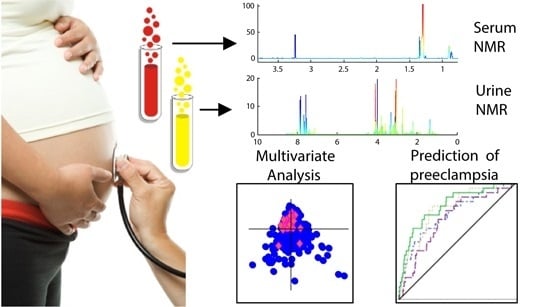
First Trimester Urine and Serum Metabolomics for Prediction of Preeclampsia and Gestational Hypertension: A Prospective Screening Study
Abstract
:1. Introduction
2. Results
2.1. Characteristics of the Study Participants
| Characteristics (Stratified Per Pregnancy Outcome) | Preeclampsia | Gestational Hypertension | Normotensive Pregnancies | p-value a |
|---|---|---|---|---|
| Number of women included | 26 | 21 | 552 | - |
| Age in years, median (IQR) | 26 (7) | 28 (6) | 28 (5) | NS |
| BMI at enrolment in kg/m2, median (IQR) | 24.8 (5.6) | 27.1 (7.6) | 23.5 (4.9) | <0.01 |
| Smoking, n (%) b | 4 (15.3) | 2 (9.5) | 63 (11.4) | NS |
| MAP at enrolment, median (IQR) | 87.0 (11.1) | 92.1 (8.1) | 82.7 (8.8) | <0.001 |
| UtAPI at enrolment, median (IQR) | 1.75 (0.70) | 1.49 (0.39) | 1.46 (0.52) | <0.05 |
| GA at enrolment, weeks, median (IQR) | 13.1 (0.6) | 13.1 (0.7) | 12.9 (0.9) | NS |
| GA at delivery, weeks, median (IQR) | 38.0 (3.1) | 40.1 (1.3) | 40.2 (1.9) | <0.001 |
| Birth weight, g, median (IQR) | 3243 (705) | 3460 (1096) | 3475 (600) | <0.01 |

2.2. Metabolic Biomarkers in Urine
| Hypertensive Pregnancy Outcome | Accuracy (%) | Specificity (%) | Sensitivity (%) | Sensitivity at 10% FPR (%) | p-Value b | Indicated Metabolites c |
|---|---|---|---|---|---|---|
| Preeclampsia (n = 26) vs. no preeclampsia (n = 561) | ||||||
| Full urine spectra | 61.4 | 65.3 | 57.5 | 11.3 | <0.01 | ↑ Crn, Gly, α-HIB, Hist, DMA ↓ Hipp, Lac/Thr, ProlB |
| VIP ≥ 1 variables | 68.2 | 60.1 | 76.3 | 23.8 | <0.01 | ↑ Crn, Gly, α-HIB, Hist, DMA ↓ Hipp, Lac/Thr |
| CARS variables | 70.8 | 74.2 | 67.5 | 51.3 | <0.01 | ↑ Gly, 4-DEA, DMA ↓ Hipp, Lac, Cre, ProlB |
| Gestational hypertension (n = 20) d vs. no gestational hypertension (n = 567) | ||||||
| Full urine spectra | 59.1 | 68.2 | 50.0 | 11.7 | <0.01 | ↑ Crn, α-HIB, DMA ↓ Hipp, Lac/Thr, ProlB, Citrate |
| VIP ≥ 1 variables | 63.7 | 65.7 | 61.7 | 16.7 | 0.01 | ↑ Crn, α-HIB, DMA ↓ Hipp, Lac/Thr, ProlB, Citrate |
| CARS variables | 63.8 | 89.3 | 38.3 | 40.0 | 0.04 | ↑ DMA ↓ PAG, Ala |
| Preeclampsia or gestational hypertension (n = 46) vs. normotensive (n = 541) | ||||||
| Full urine spectra | 61.5 | 56.1 | 66.8 | 14.4 | <0.01 | ↑ Crn, α-HIB, DMA, ↓ Hipp, Lac/Thr, ProlB ↑ Crn, α-HIB, DMA ↓ Hipp, Lac/Thr, ProlB |
| VIP ≥ 1 variables | 64.0 | 56.2 | 71.9 | 20.0 | <0.01 | |
| CARS variables | 66.4 | 75.9 | 56.9 | 36.9 | <0.01 | ↑ α-HIB, DMA ↓ Hipp, PAG, Lys, Ala |

2.3. Metabolic Biomarkers in Serum
| Hypertensive Pregnancy Outcome | Accuracy (%) | Specificity (%) | Sensitivity (%) | Sensitivity at 10% FPR (%) | p-Value b | Indicated Metabolites c |
|---|---|---|---|---|---|---|
| Preeclampsia (n = 26), vs. no preeclampsia (n = 565) | ||||||
| Full serum spectra | 59.4 | 73.8 | 45.0 | 20.0 | >0.05 | NS |
| VIP ≥ 1 variables | 58.3 | 70.3 | 46.3 | 26.3 | >0.05 | NS |
| CARS variables | 64.6 | 65.4 | 63.8 | 15.0 | 0.05 | ↑ Signals from triglycerides, 3-HB, ↓ Pyruvate, PtdCho, Lac |
| Gestational Hypertension (n = 21) vs. no gestational hypertension (n = 570) | ||||||
| Full serum spectra | 59.1 | 74.8 | 43.3 | 25.0 | >0.05 | NS |
| VIP ≥ 1 variables | 58.1 | 75.0 | 41.3 | 22.5 | >0.05 | NS |
| CARS variables | 66.1 | 55.0 | 76.9 | 33.3 | 0.02 | ↑ Signals from triglycerides, ↓ Variables corresponding to HDL, Lac, N-Ac, PtdCho, Glc |
| Preeclampsia or gestational hypertension (n = 47) vs. normotensive (n = 544) | ||||||
| Full serum spectra | 62.6 | 70.8 | 54.4 | 24.4 | 0.01 | ↑ Lipid signals, signals from triglycerides, ↓ Signals from HDL, Glc, Val, Leu, Lac, Ala, PtdCho |
| VIP ≥ 1 variables | 63.0 | 70.4 | 55.6 | 27.5 | <0.00 | ↑ Lipid signals, signals from triglycerides, ↓ Signals from HDL, Glc, Leu, Val, Ala, Lac, PtdCho |
| CARS variables | 64.5 | 69.1 | 60.0 | 30.0 | 0.02 | ↑ Variables corresponding to triglycerides, ↓ Lac, PtdCho |

2.4. Combined Metabolic and Clinical Biomarkers Predict Preeclampsia
| Variable | AUC (95% CI) | Sensitivity (%) a | PPV | NPV | p-Value b |
|---|---|---|---|---|---|
| Hippurate/creatinine ratio c | 0.694 (0.595–0.793) | 0.192 | 0.082 | 0.960 | 0.004 |
| MAP, age d, UtAPI | 0.738 (0.637–0.839) | 0.346 | 0.138 | 0.967 | <0.001 |
| Metabolites, MAP, age d | 0.778 (0.695–0.862) | 0.423 | 0.164 | 0.971 | <0.001 |
| Metabolites, MAP, age d, UtAPI | 0.807 (0.721–0.893) | 0.538 | 0.200 | 0.977 | <0.001 |

3. Discussion
4. Experimental Section
4.1. Study Population
4.2. 1H NMR Metabolomic Analyses
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Myatt, L.; Redman, C.W.; Staff, A.C.; Hansson, S.; Wilson, M.L.; Laivuori, H.; Poston, L.; Roberts, J.M. Strategy for standardization of preeclampsia research study design. Hypertension 2014, 63, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Sibai, B.M. Diagnosis and management of gestational hypertension and preeclampsia. Obstet. Gynecol. 2003, 102, 181–192. [Google Scholar] [CrossRef]
- Roberts, J.M.; August, P.A.; Bakris, G.; Barton, J.R.; Bernstein, I.M.; Druzin, M.; Gaiser, R.R.; Granger, J.R.; Jeyabalan, A.; Johnson, D.D.; et al. Hypertension in Pregnancy. Obstet. Gynecol. 2013, 122, 1122–1131. [Google Scholar]
- Roberge, S.; Villa, P.; Nicolaides, K.; Giguere, Y.; Vainio, M.; Bakthi, A.; Ebrashy, A.; Bujold, E. Early administration of low-dose aspirin for the prevention of preterm and term preeclampsia: A systematic review and meta-analysis. Fetal Diagn. Ther. 2012, 31, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Akolekar, R.; Syngelaki, A.; Poon, L.; Wright, D.; Nicolaides, K.H. Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagn. Ther. 2013, 33, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Poon, L.C.; Kametas, N.; Maiz, N.; Akolekar, R.; Nicolaides, K.H. First-trimester prediction of hypertensive disorders in pregnancy. Hypertension 2009, 53, 812–818. [Google Scholar] [CrossRef] [PubMed]
- Scazzocchio, E.; Figueras, F.; Crispi, F.; Meler, E.; Masoller, N.; Mula, R.; Gratacos, E. Performance of a first-trimester screening of preeclampsia in a routine care low-risk setting. Am. J. Obstet. Gynecol. 2013, 208, 203.e201–203.e210. [Google Scholar] [CrossRef] [PubMed]
- Akolekar, R.; Syngelaki, A.; Sarquis, R.; Zvanca, M.; Nicolaides, K.H. Prediction of early, intermediate and late pre-eclampsia from maternal factors, biophysical and biochemical markers at 11–13 weeks. Prenat. Diagn. 2011, 31, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Skråstad, R.B.; Hov, G.G.; Blaas, H.G.; Romundstad, P.R.; Salvesen, K.Å. A prospective study of screening for hypertensive disorders of pregnancy at 11–13 weeks in a Scandinavian population. Acta Obstet. Gynecol. Scand. 2014, 93, 1238–1247. [Google Scholar] [CrossRef] [PubMed]
- Fanos, V.; Atzori, L.; Makarenko, K.; Melis, G.B.; Ferrazzi, E. Metabolomics application in maternal-fetal medicine. Biomed. Res. Int. 2013, 2013, 720514. [Google Scholar] [CrossRef] [PubMed]
- Lindon, J.C.; Nicholson, J.K.; Holmes, E.; Everett, J.R. Metabonomics: Metabolic processes studied by NMR spectroscopy of biofluids. Concepts Magn. Res. 2000, 12, 289–320. [Google Scholar] [CrossRef]
- Bahado-Singh, R.O.; Akolekar, R.; Mandal, R.; Dong, E.; Xia, J.; Kruger, M.; Wishart, D.S.; Nicolaides, K. First-trimester metabolomic detection of late-onset preeclampsia. Am. J. Obstet. Gynecol. 2013, 208, e10–e11. [Google Scholar] [CrossRef] [PubMed]
- Bahado-Singh, R.O.; Akolekar, R.; Mandal, R.; Dong, E.; Xia, J.; Kruger, M.; Wishart, D.S.; Nicolaides, K.H. Metabolomics and first-trimester prediction of early-onset preeclampsia. J. Matern. Fetal Neonatal Med. 2012, 25, 1840–1847. [Google Scholar] [CrossRef] [PubMed]
- Diaz, S.O.; Barros, A.S.; Goodfellow, B.J.; Duarte, I.F.; Galhano, E.; Pita, C.; Almeida Mdo, C.; Carreira, I.M.; Gil, A.M. Second trimester maternal urine for the diagnosis of trisomy 21 and prediction of poor pregnancy outcomes. J. Proteome Res. 2013, 12, 2946–2957. [Google Scholar] [CrossRef] [PubMed]
- Pinto, J.; Maciel, E.; Melo, T.S.; Domingues, M.R.M.; Galhano, E.; Pita, C.; Almeida, M.D.C.; Carreira, I.M.; Gil, A.M. Maternal plasma phospholipids are altered in trisomy 21 cases and prior to preeclampsia and preterm outcomes. Rapid Commun. Mass Spectrom. 2014, 28, 1635–1638. [Google Scholar] [CrossRef] [PubMed]
- Kenny, L.C.; Broadhurst, D.I.; Dunn, W.B.; Brown, M.; North, R.A.; McCowan, L.; Roberts, C.; Cooper, G.J.S.; Kell, D.B.; Baker, N.B. Robust early pregnancy prediction of later preeclampsia using metabolomic biomarkers. Hypertension 2010, 56, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Kenny, L.C.; Black, M.A.; Poston, L.; Taylor, R.; Myers, J.E.; Baker, P.N.; McCowan, L.M.; Simpson, N.A.; Dekker, G.A.; Roberts, C.T.; et al. Early Pregnancy Prediction of Preeclampsia in Nulliparous Women, Combining Clinical Risk and Biomarkers: The Screening for Pregnancy Endpoints (SCOPE) International Cohort Study. Hypertension 2014, 64, 644–652. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.; Loo, R.L.; Stamler, J.; Bictash, M.; Yap, I.K.; Chan, Q.; Ebbels, T.; de Iorio, M.; Brown, I.J.; Veselkov, K.A.; et al. Human metabolic phenotype diversity and its association with diet and blood pressure. Nature 2008, 453, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.K.; Holmes, E.; Kinross, J.; Burcelin, R.; Gibson, G.; Jia, W.; Pettersson, S. Host-gut microbiota metabolic interactions. Science 2012, 336, 1262–1267. [Google Scholar] [CrossRef] [PubMed]
- Heinzmann, S.S.; Merrifield, C.A.; Rezzi, S.; Kochhar, S.; Lindon, J.C.; Holmes, E.; Nicholson, J.K. Stability and robustness of human metabolic phenotypes in response to sequential food challenges. J. Proteome Res. 2012, 11, 643–655. [Google Scholar] [CrossRef] [PubMed]
- Appiah-Amponsah, E.; Shanaiah, N.; Nagana Gowda, G.A.; Owusu-Sarfo, K.; Ye, T.; Raftery, D. Identification of 4-deoxythreonic acid present in human urine using HPLC and NMR techniques. J. Pharm. Biomed. Anal. 2009, 50, 878–885. [Google Scholar] [CrossRef] [PubMed]
- Tsikas, D.; Thum, T.; Becker, T.; Pham, V.V.; Chobanyan, K.; Mitschke, A.; Beckmann, B.; Gutzki, F.M.; Bauersachs, J.; Stichtenoth, D.O. Accurate quantification of dimethylamine (DMA) in human urine by gas chromatography-mass spectrometry as pentafluorobenzamide derivative: Evaluation of the relationship between DMA and its precursor asymmetric dimethylarginine (ADMA) in health and disease. J. Chromatogr. B 2007, 851, 229–239. [Google Scholar] [CrossRef]
- Boger, R.H. Association of asymmetric dimethylarginine and endothelial dysfunction. Clin. Chem. Lab. Med. 2003, 41, 1467–1472. [Google Scholar] [CrossRef] [PubMed]
- Diaz, S.O.; Barros, A.S.; Goodfellow, B.J.; Duarte, I.F.; Carreira, I.M.; Galhano, E.; Pita, C.; Almeida Mdo, C.; Gil, A.M. Following healthy pregnancy by nuclear magnetic resonance (NMR) metabolic profiling of human urine. J. Proteome Res. 2013, 12, 969–979. [Google Scholar] [CrossRef] [PubMed]
- Baweja, S.; Kent, A.; Masterson, R.; Roberts, S.; McMahon, L.P. Prediction of pre-eclampsia in early pregnancy by estimating the spot urinary albumin: Creatinine ratio using high-performance liquid chromatography. BJOG 2011, 118, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Kuromoto, K.; Watanabe, M.; Adachi, K.; Ohashi, K.; Iwatani, Y. Increases in urinary creatinine and blood pressure during early pregnancy in pre-eclampsia. Ann. Clin. Biochem. 2010, 47, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Palatini, P. Glomerular hyperfiltration: A marker of early renal damage in pre-diabetes and pre-hypertension. Nephrol. Dial. Transplant. 2012, 27, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.; Posma, J.M.; Chan, Q.; Garcia-Perez, I.; Wijeyesekera, A.; Bictash, M.; Ebbels, T.M.; Ueshima, H.; Zhao, L.; van Horn, L.; et al. Urinary metabolic signatures of human adiposity. Sci. Transl. Med. 2015, 7, 285ra62–285ra62. [Google Scholar] [CrossRef]
- Odibo, A.O.; Goetzinger, K.R.; Odibo, L.; Cahill, A.G.; Macones, G.A.; Nelson, D.M.; Dietzen, D.J. First-trimester prediction of preeclampsia using metabolomic biomarkers: A discovery phase study. Prenat. Diagn. 2011, 31, 990–994. [Google Scholar] [CrossRef] [PubMed]
- Enquobahrie, D.A.; Williams, M.A.; Butler, C.L.; Frederick, I.O.; Miller, R.S.; Luthy, D.A. Maternal plasma lipid concentrations in early pregnancy and risk of preeclampsia. Am. J. Hypertens. 2004, 17, 574–581. [Google Scholar] [CrossRef] [PubMed]
- Demirci, O.; Tugrul, A.S.; Dolgun, N.; Sozen, H.; Eren, S. Serum lipids level assessed in early pregnancy and risk of pre-eclampsia. J. Obstet. Gynaecol. Res. 2011, 37, 1427–1432. [Google Scholar] [CrossRef] [PubMed]
- Demir, B.; Demir, S.; Atamer, Y.; Guven, S.; Atamer, A.; Kocyigit, Y.; Hekimoglu, A.; Toprak, G. Serum levels of lipids, lipoproteins and paraoxonase activity in pre-eclampsia. J. Int. Med. Res. 2011, 39, 1427–1431. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Bar, H.Y.; Yan, J.; Jones, S.; Brannon, P.M.; West, A.A.; Perry, C.A.; Ganti, A.; Pressman, E.; Devapatla, S.; et al. A higher maternal choline intake among third-trimester pregnant women lowers placental and circulating concentrations of the antiangiogenic factor fms-like tyrosine kinase-1 (sFLT1). FASEB J. 2013, 27, 1245–1253. [Google Scholar] [CrossRef] [PubMed]
- Mehta, A.K.; Singh, B.P.; Arora, N.; Gaur, S.N. Choline attenuates immune inflammation and suppresses oxidative stress in patients with asthma. Immunobiology 2010, 215, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Mehedint, M.G.; Craciunescu, C.N.; Zeisel, S.H. Maternal dietary choline deficiency alters angiogenesis in fetal mouse hippocampus. Proc. Natl. Acad. Sci. USA 2010, 107, 12834–12839. [Google Scholar] [CrossRef]
- Bye, A.; Vettukattil, R.; Aspenes, S.T.; Giskeødegård, G.F.; Gribbestad, I.S.; Wisløff, U.; Bathen, T.F. Serum Levels of Choline-Containing Compounds Are Associated with Aerobic Fitness Level: The HUNT-Study. PLoS ONE 2012, 7, e42330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laffel, L. Ketone bodies: A review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab. Res. Rev. 1999, 15, 412–426. [Google Scholar] [CrossRef]
- Poon, L.C.; Nicolaides, K.H. Early prediction of preeclampsia. Obstet. Gynecol. Int. 2014, 297397. [Google Scholar] [CrossRef] [PubMed]
- Roberge, S.; Giguere, Y.; Villa, P.; Nicolaides, K.; Vainio, M.; Forest, J.C.; von Dadelszen, P.; Vaiman, D.; Tapp, S.; Bujold, E. Early administration of low-dose aspirin for the prevention of severe and mild preeclampsia: A systematic review and meta-analysis. Am. J. Perinatol. 2012, 29, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Villa, P.M.; Kajantie, E.; Raikkonen, K.; Pesonen, A.K.; Hamalainen, E.; Vainio, M.; Taipale, P.; Laivuori, H.; Predo, S.G. Aspirin in the prevention of pre-eclampsia in high-risk women: A randomised placebo-controlled PREDO Trial and a meta-analysis of randomised trials. BJOG 2013, 120, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Skrastad, R.; Hov, G.; Blaas, H.G.; Romundstad, P.; Salvesen, K. Risk assessment for preeclampsia in nulliparous women at 11–13 weeks gestational age: Prospective evaluation of two algorithms. BJOG 2014. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Broadhurst, D.I.; Wilson, M.; Wishart, D.S. Translational biomarker discovery in clinical metabolomics: An introductory tutorial. Metabolomics 2013, 9, 280–299. [Google Scholar] [CrossRef] [PubMed]
- Kuc, S.; Koster, M.P.; Pennings, J.L.; Hankemeier, T.; Berger, R.; Harms, A.C.; Dane, A.D.; Schielen, P.C.; Visser, G.H.; Vreeken, R.J. Metabolomics profiling for identification of novel potential markers in early prediction of preeclampsia. PLoS ONE 2014, 9, e98540. [Google Scholar] [CrossRef] [PubMed]
- North, R.A.; McCowan, L.M.E.; Dekker, G.A.; Poston, L.; Chan, E.H.Y.; Stewart, A.W.; Black, M.A.; Taylor, R.S.; Walker, J.J.; Baker, P.N.; et al. Clinical risk prediction for preeclampsia in nulliparous women: Development of model in international prospective cohort. Brit. Med. J. 2011, 342. [Google Scholar] [CrossRef]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; de Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension. Blood Press. 2013, 22, 193–278. [Google Scholar] [CrossRef] [PubMed]
- Khalil, A.; Nicolaides, K.H. How to record uterine artery Doppler in the first trimester. Ultrasound Obstet. Gynecol. 2013, 42, 478–479. [Google Scholar] [CrossRef] [PubMed]
- Diagnosis and management of preeclampsia and eclampsia. Int. J. Gynaecol. Obstet. 2002, 77, 67–75.
- Maršál, K.; Persson, P.H.; Larsen, T.; Lilja, H.; Selbing, A.; Sultan, B. Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Padiatr. 1996, 85, 843–848. [Google Scholar] [CrossRef]
- Savorani, F.; Tomasi, G.; Engelsen, S. icoshift: A versatile tool for the rapid alignment of 1D NMR spectra. J. Magn. Res. 2010, 443, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Giskeodegard, G.F.; Bloemberg, T.G.; Postma, G.; Sitter, B.; Tessem, M.B.; Gribbestad, I.S.; Bathen, T.F.; Buydens, L.M. Alignment of high resolution magic angle spinning magnetic resonance spectra using warping methods. Anal. Chim. Acta 2010, 683, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dieterle, F.; Ross, A.; Schlotterbeck, G.; Senn, H. Probabilistic quotient normalization as robust method to account for dilution of complex biological mixtures. Application in 1H NMR metabonomics. Anal. Chem. 2006, 78, 4281–4290. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, R.; Hoefsloot, H.; Westerhuis, J.; Smilde, A.; van der Werf, M. Centering, scaling, and transformations: Improving the biological information content of metabolomics data. BMC Genomics 2006, 7, 142. [Google Scholar] [CrossRef] [PubMed]
- Massey, F.J. The Kolmogorov-Smirnov test for goodness of fit. J. Am. Stat. Assoc. 1951, 46, 68–78. [Google Scholar] [CrossRef]
- Wold, S.; Sjöström, M.; Eriksson, L. PLS-regression: A basic tool of chemometrics. Chemom. Intell. Lab. 2001, 58, 109–130. [Google Scholar] [CrossRef]
- Chong, I.-G.; Jun, C.-H. Performance of some variable selection methods when multicollinearity is present. Chemom. Intell. Lab. 2005, 78, 103–112. [Google Scholar] [CrossRef]
- Li, H.; Liang, Y.; Xu, Q.; Cao, D. Key wavelengths screening using competitive adaptive reweighted sampling method for multivariate calibration. Anal. Chim. Acta 2009, 648, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Westerhuis, J.; Hoefsloot, H.J.; Smit, S.; Vis, D.; Smilde, A.; Velzen, E.J.; Duijnhoven, J.M.; Dorsten, F. Assessment of PLSDA cross validation. Metabolomics 2008, 4, 81–89. [Google Scholar] [CrossRef]
- Saftlas, A.F.; Olson, D.R.; Franks, A.L.; Atrash, H.K.; Pokras, R. Epidemiology of preeclampsia and eclampsia in the United States, 1979–1986. Am. J. Obstet. Gynecol. 1990, 163, 460–465. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Austdal, M.; Tangerås, L.H.; Skråstad, R.B.; Salvesen, K.; Austgulen, R.; Iversen, A.-C.; Bathen, T.F. First Trimester Urine and Serum Metabolomics for Prediction of Preeclampsia and Gestational Hypertension: A Prospective Screening Study. Int. J. Mol. Sci. 2015, 16, 21520-21538. https://doi.org/10.3390/ijms160921520
Austdal M, Tangerås LH, Skråstad RB, Salvesen K, Austgulen R, Iversen A-C, Bathen TF. First Trimester Urine and Serum Metabolomics for Prediction of Preeclampsia and Gestational Hypertension: A Prospective Screening Study. International Journal of Molecular Sciences. 2015; 16(9):21520-21538. https://doi.org/10.3390/ijms160921520
Chicago/Turabian StyleAustdal, Marie, Line H. Tangerås, Ragnhild B. Skråstad, Kjell Salvesen, Rigmor Austgulen, Ann-Charlotte Iversen, and Tone F. Bathen. 2015. "First Trimester Urine and Serum Metabolomics for Prediction of Preeclampsia and Gestational Hypertension: A Prospective Screening Study" International Journal of Molecular Sciences 16, no. 9: 21520-21538. https://doi.org/10.3390/ijms160921520