Clostridium butyricum Can Promote Bone Development by Regulating Lymphocyte Function in Layer Pullets
Abstract
:1. Introduction
2. Results
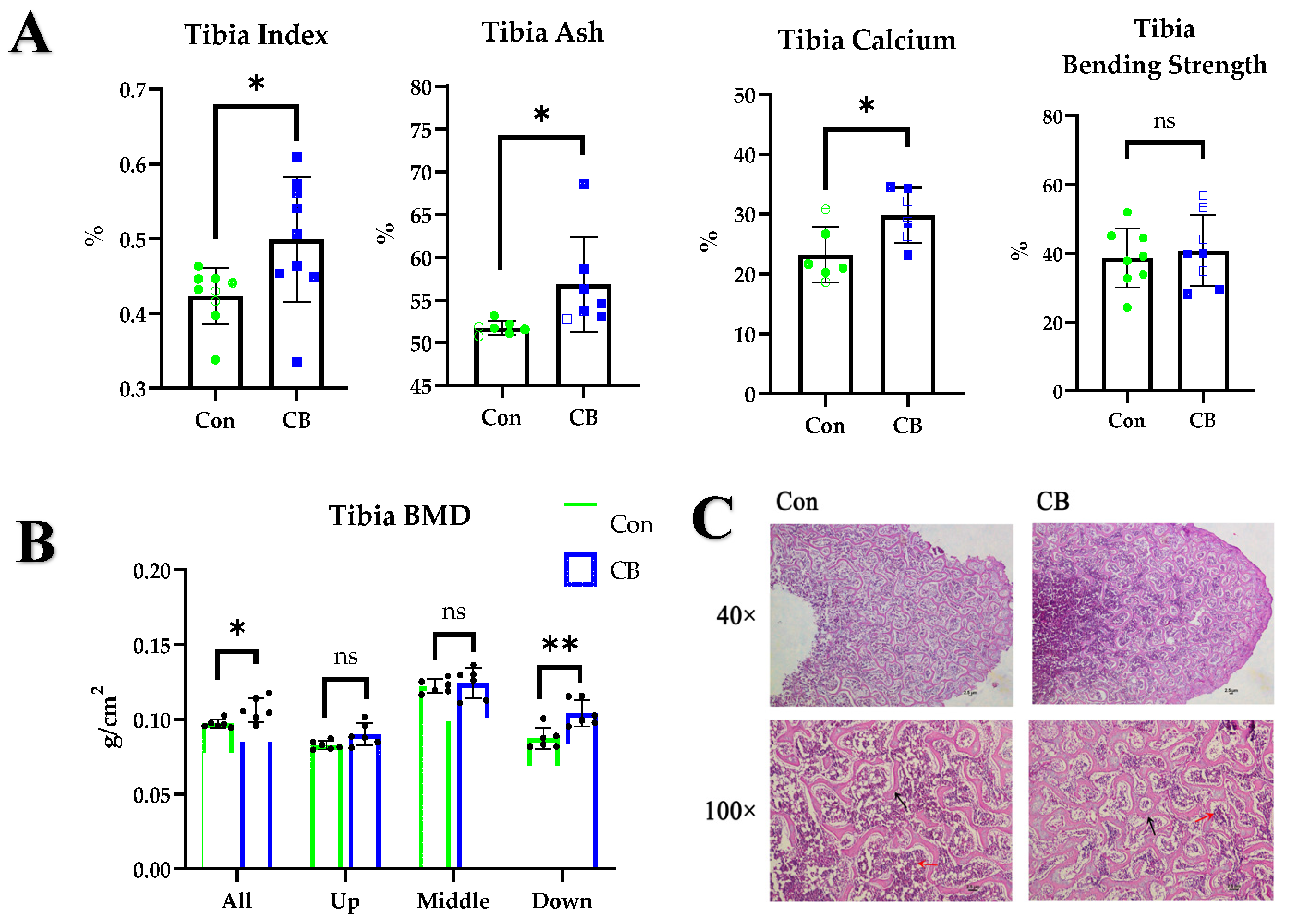
2.1. CB Promotes Bone Development in Layer Pullets
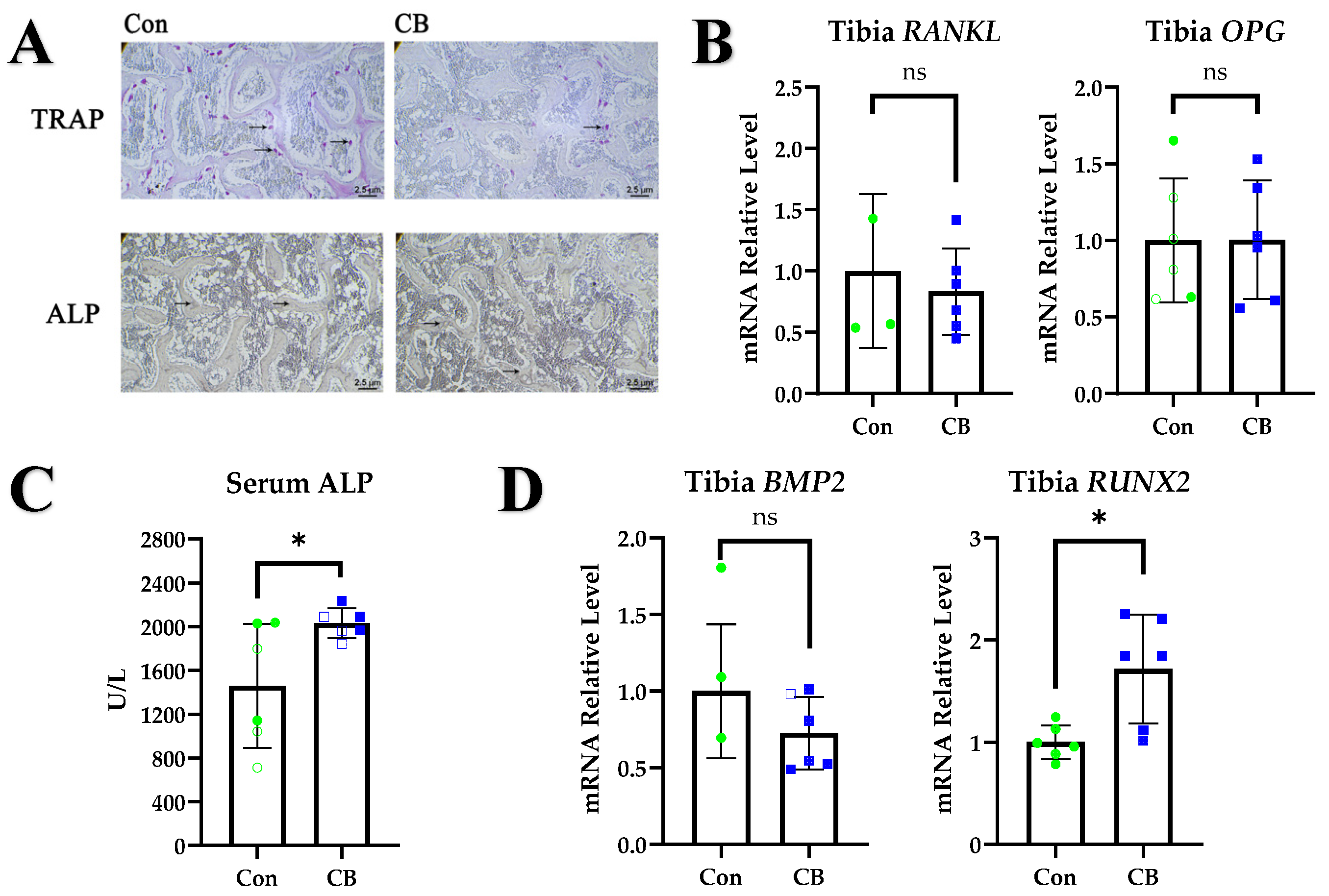
2.2. CB Promotes Osteoblast Metabolism
2.3. CB Upregulates the Proportion of Treg Cells
2.4. CB Promotes Osteoblast Activity In Vitro but Requires Lymphocyte Involvement
3. Discussion
4. Materials and Methods
4.1. Bacterial Strains
4.2. Experimental Design
4.3. Bone Function Evaluation Index
4.4. Real-Time PCR Analyses
4.5. Bone RNA Extraction
4.6. Gut Microbiome Analysis and Determination of SCFA Concentrations
4.7. In Vitro Culture and Processing of Lymphocytes
4.8. In Vitro Culture and Processing of Osteoblasts
4.9. Flow Cytometry
4.10. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bar, A. Calcium transport in strongly calcifying laying birds: Mechanisms and regulation. Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 2009, 152, 447–469. [Google Scholar] [CrossRef] [PubMed]
- Webster, A.B. Welfare implications of avian osteoporosis. Poult. Sci. 2004, 83, 184–192. [Google Scholar] [CrossRef]
- Cooney, O.D.; Nagareddy, P.R.; Murphy, A.J.; Lee, M.K.S. Healthy Gut, Healthy Bones: Targeting the Gut Microbiome to Promote Bone Health. Front. Endocrinol. 2020, 11, 620466. [Google Scholar] [CrossRef]
- Zheng, D.; Liwinski, T.; Elinav, E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020, 30, 492–506. [Google Scholar] [CrossRef]
- Hooper, L.V.; Littman, D.R.; Macpherson, A.J. Interactions between the microbiota and the immune system. Science 2012, 336, 1268–1273. [Google Scholar] [CrossRef] [Green Version]
- Lee, H.W.; Suh, J.H.; Kim, A.Y.; Lee, Y.S.; Park, S.Y.; Kim, J.B. Histone deacetylase 1-mediated histone modification regulates osteoblast differentiation. Mol. Endocrinol. 2006, 20, 2432–2443. [Google Scholar] [CrossRef] [Green Version]
- Katono, T.; Kawato, T.; Tanabe, N.; Suzuki, N.; Iida, T.; Morozumi, A.; Ochiai, K.; Maeno, M. Sodium butyrate stimulates mineralized nodule formation and osteoprotegerin expression by human osteoblasts. Arch. Oral Biol. 2008, 53, 903–909. [Google Scholar] [CrossRef]
- Rahman, M.M.; Kukita, A.; Kukita, T.; Shobuike, T.; Nakamura, T.; Kohashi, O. Two histone deacetylase inhibitors, trichostatin A and sodium butyrate, suppress differentiation into osteoclasts but not into macrophages. Blood 2003, 101, 3451–3459. [Google Scholar] [CrossRef]
- D’Amelio, P.; Sassi, F. Gut Microbiota, Immune System, and Bone. Calcif. Tissue Int. 2018, 102, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Arpaia, N.; Campbell, C.; Fan, X.; Dikiy, S.; van der Veeken, J.; Deroos, P.; Liu, H.; Cross, J.R.; Pfeffer, K.; Coffer, P.J.; et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 2013, 504, 451–455. [Google Scholar] [CrossRef]
- Kelchtermans, H.; Geboes, L.; Mitera, T.; Huskens, D.; Leclercq, G.; Matthys, P. Activated CD4+CD25+ regulatory T cells inhibit osteoclastogenesis and collagen-induced arthritis. Ann. Rheum Dis. 2009, 68, 744–750. [Google Scholar] [CrossRef]
- Kim, Y.G.; Lee, C.K.; Nah, S.S.; Mun, S.H.; Yoo, B.; Moon, H.B. Human CD4+CD25+ regulatory T cells inhibit the differentiation of osteoclasts from peripheral blood mononuclear cells. Biochem. Biophys. Res. Commun. 2007, 357, 1046–1052. [Google Scholar] [CrossRef] [PubMed]
- Lei, H.; Schmidt-Bleek, K.; Dienelt, A.; Reinke, P.; Volk, H.D. Regulatory T cell-mediated anti-inflammatory effects promote successful tissue repair in both indirect and direct manners. Front. Pharmacol. 2015, 6, 184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quach, D.; Britton, R.A. Gut Microbiota and Bone Health. Adv. Exp. Med. Biol. 2017, 1033, 47–58. [Google Scholar]
- Guo, P.; Zhang, K.; Ma, X.; He, P. Clostridium species as probiotics: Potentials and challenges. J. Anim. Sci. Biotechnol. 2020, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, Y.; Lin, X.; Gou, Z.; Fan, Q.; Jiang, S. Effects of Clostridium butyricum, Sodium Butyrate, and Butyric Acid Glycerides on the Reproductive Performance, Egg Quality, Intestinal Health, and Offspring Performance of Yellow-Feathered Breeder Hens. Front. Microbiol. 2021, 12, 657542. [Google Scholar] [CrossRef]
- Li, W.; Xu, B.; Wang, L.; Sun, Q.; Deng, W.; Wei, F.; Ma, H.; Fu, C.; Wang, G.; Li, S. Effects of Clostridium butyricum on Growth Performance, Gut Microbiota and Intestinal Barrier Function of Broilers. Front. Microbiol. 2021, 12, 777456. [Google Scholar] [CrossRef]
- Molnar, A.; Such, N.; Farkas, V.; Pal, L.; Menyhart, L.; Wagner, L.; Husveth, F.; Dublecz, K. Effects of Wheat Bran and Clostridium butyricum Supplementation on Cecal Microbiota, Short-Chain Fatty Acid Concentration, pH and Histomorphometry in Broiler Chickens. Animals 2020, 10, 2230. [Google Scholar] [CrossRef]
- Liao, X.D.; Ma, G.; Cai, J.; Fu, Y.; Yan, X.Y.; Wei, X.B.; Zhang, R.J. Effects of Clostridium butyricum on growth performance, antioxidation, and immune function of broilers. Poult. Sci. 2015, 94, 662–667. [Google Scholar] [CrossRef]
- Yu, Y.; Li, Q.; Zhang, H.; Wu, Y.; Zhang, R.; Yue, M.; Yang, C.; Cao, G. Clostridium butyricum alone or combined with 1, 25-dihydroxyvitamin D3 improved early-stage broiler health by modulating intestinal flora. J. Appl. Microbiol. 2022, 132, 155–166. [Google Scholar] [CrossRef]
- Yang, C.M.; Cao, G.T.; Ferket, P.R.; Liu, T.T.; Zhou, L.; Zhang, L.; Xiao, Y.P.; Chen, A.G. Effects of probiotic, Clostridium butyricum, on growth performance, immune function, and cecal microflora in broiler chickens. Poult. Sci. 2012, 91, 2121–2129. [Google Scholar] [CrossRef] [PubMed]
- Zhan, H.Q.; Dong, X.Y.; Li, L.L.; Zheng, Y.X.; Gong, Y.J.; Zou, X.T. Effects of dietary supplementation with Clostridium butyricum on laying performance, egg quality, serum parameters, and cecal microflora of laying hens in the late phase of production. Poult. Sci. 2019, 98, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Yang, J.; Wang, L.; Lin, H.; Sun, S. Protection Mechanism of Clostridium butyricum against Salmonella Enteritidis Infection in Broilers. Front. Microbiol. 2017, 8, 1523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, X.; Yang, J.; Ju, Z.; Wu, J.; Wang, L.; Lin, H.; Sun, S. Clostridium butyricum Ameliorates Salmonella Enteritis Induced Inflammation by Enhancing and Improving Immunity of the Intestinal Epithelial Barrier at the Intestinal Mucosal Level. Front. Microbiol. 2020, 11, 299. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Song, M.; Lv, P.; Hao, G.; Sun, S. Effects of Clostridium butyricum on intestinal environment and gut microbiome under Salmonella infection. Poult. Sci. 2022, 101, 102077. [Google Scholar] [CrossRef]
- Kim, J.M.; Lin, C.; Stavre, Z.; Greenblatt, M.B.; Shim, J.H. Osteoblast-Osteoclast Communication and Bone Homeostasis. Cells 2020, 9, 2073. [Google Scholar] [CrossRef]
- Lacey, D.L.; Boyle, W.J.; Simonet, W.S.; Kostenuik, P.J.; Dougall, W.C.; Sullivan, J.K.; San Martin, J.; Dansey, R. Bench to bedside: Elucidation of the OPG-RANK-RANKL pathway and the development of denosumab. Nat. Rev. Drug Discov. 2012, 11, 401–419. [Google Scholar] [CrossRef]
- Siller, A.F.; Whyte, M.P. Alkaline phosphatase: Discovery and naming of our favorite enzyme. J. Bone Miner. Res. 2018, 33, 362–364. [Google Scholar] [CrossRef] [Green Version]
- Komori, T. Regulation of Proliferation, Differentiation and Functions of Osteoblasts by Runx2. Int. J. Mol. Sci. 2019, 20, 1694. [Google Scholar] [CrossRef] [Green Version]
- Nguyen, V.; Meyers, C.A.; Yan, N.; Agarwal, S.; Levi, B.; James, A.W. BMP-2-induced bone formation and neural inflammation. J. Orthop. 2017, 14, 252–256. [Google Scholar] [CrossRef]
- Okamoto, K.; Nakashima, T.; Shinohara, M.; Negishi-Koga, T.; Komatsu, N.; Terashima, A.; Sawa, S.; Nitta, T.; Takayanagi, H. Osteoimmunology: The Conceptual Framework Unifying the Immune and Skeletal Systems. Physiol. Rev. 2017, 97, 1295–1349. [Google Scholar] [CrossRef] [PubMed]
- Ni, S.; Shan, F.; Geng, J. Interleukin-10 family members: Biology and role in the bone and joint diseases. Int. Immunopharmacol. 2022, 108, 108881. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, N.B.; Elleder, D.; Schusser, B.; Krchlikova, V.; Gobel, T.W.; Hartle, S.; Kaspers, B. The Discovery of Chicken Foxp3 Demands Redefinition of Avian Regulatory T Cells. J. Immunol. 2022, 208, 1128–1138. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.; Gao, H.; Wang, Y.; Gao, L.; Cao, H.; Li, X.; Zheng, S. [Analysis of the structure of chicken Foxp3 and its expression profile in tissues]. Sheng Wu Gong Cheng Xue Bao 2022, 38, 2928–2938. [Google Scholar]
- Selvaraj, R.K. Avian CD4(+)CD25(+) regulatory T cells: Properties and therapeutic applications. Dev. Comp. Immunol. 2013, 41, 397–402. [Google Scholar] [CrossRef]
- Tang, N.; Song, W.X.; Luo, J.; Luo, X.; Chen, J.; Sharff, K.A.; Bi, Y.; He, B.C.; Huang, J.Y.; Zhu, G.H.; et al. BMP-9-induced osteogenic differentiation of mesenchymal progenitors requires functional canonical Wnt/beta-catenin signalling. J. Cell. Mol. Med. 2009, 13, 2448–2464. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, Y.; Thirukonda, G.J.; Nakamura, Y.; Koide, M.; Yamashita, T.; Uehara, S.; Kato, H.; Udagawa, N.; Takahashi, N. Wnt16 regulates osteoclast differentiation in conjunction with Wnt5a. Biochem. Biophys. Res. Commun. 2015, 463, 1278–1283. [Google Scholar] [CrossRef]
- Maeda, K.; Kobayashi, Y.; Udagawa, N.; Uehara, S.; Ishihara, A.; Mizoguchi, T.; Kikuchi, Y.; Takada, I.; Kato, S.; Kani, S. Wnt5a-Ror2 signaling between osteoblast-lineage cells and osteoclast precursors enhances osteoclastogenesis. Nat. Med. 2012, 18, 405–412. [Google Scholar] [CrossRef]
- Zaiss, M.M.; Jones, R.M.; Schett, G.; Pacifici, R. The gut-bone axis: How bacterial metabolites bridge the distance. J. Clin. Investig. 2019, 129, 3018–3028. [Google Scholar] [CrossRef] [Green Version]
- Boyce, B.F.; Xing, L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch. Biochem. Biophys. 2008, 473, 139–146. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.J.; Kim, W.J.; Ryoo, H.M. Post-Translational Regulations of Transcriptional Activity of RUNX2. Mol. Cells 2020, 43, 160–167. [Google Scholar]
- Abd El-Hack, M.E.; El-Saadony, M.T.; Shafi, M.E.; Qattan, S.Y.A.; Batiha, G.E.; Khafaga, A.F.; Abdel-Moneim, A.E.; Alagawany, M. Probiotics in poultry feed: A comprehensive review. J. Anim. Physiol. Anim. Nutr. 2020, 104, 1835–1850. [Google Scholar] [CrossRef] [PubMed]
- Takayanagi, H.; Ogasawara, K.; Hida, S.; Chiba, T.; Murata, S.; Sato, K.; Takaoka, A.; Yokochi, T.; Oda, H.; Tanaka, K.; et al. T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-gamma. Nature 2000, 408, 600–605. [Google Scholar] [CrossRef]
- Takayanagi, H. Osteoimmunology: Shared mechanisms and crosstalk between the immune and bone systems. Nat. Rev. Immunol. 2007, 7, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zeng, D.; Yang, M.; Wen, B.; Lai, J.; Zhou, Y.; Sun, H.; Xiong, L.; Wang, J.; Lin, Y.; et al. Probiotic Clostridium butyricum Improves the Growth Performance, Immune Function, and Gut Microbiota of Weaning Rex Rabbits. Probiotics Antimicrob. Proteins 2019, 11, 1278–1292. [Google Scholar] [CrossRef] [PubMed]
- Zhong, D.Y.; Li, L.; Ma, R.M.; Deng, Y.H. The Effect of Probiotics in Stroke Treatment. Evid. Based Complement. Alternat. Med. 2021, 2021, 4877311. [Google Scholar] [CrossRef]
- Tyagi, A.M.; Yu, M.; Darby, T.M.; Vaccaro, C.; Li, J.Y.; Owens, J.A.; Hsu, E.; Adams, J.; Weitzmann, M.N.; Jones, R.M.; et al. The Microbial Metabolite Butyrate Stimulates Bone Formation via T Regulatory Cell-Mediated Regulation of WNT10B Expression. Immunity 2018, 49, 1116–1131 e7. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, A.; Sato, T.; Kamada, N.; Mikami, Y.; Matsuoka, K.; Hisamatsu, T.; Hibi, T.; Roers, A.; Yagita, H.; Ohteki, T.; et al. A single strain of Clostridium butyricum induces intestinal IL-10-producing macrophages to suppress acute experimental colitis in mice. Cell Host Microbe 2013, 13, 711–722. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Gong, Y.; Xie, Y.; Sun, Q.; Li, Y. Clostridium butyricum protects the epithelial barrier by maintaining tight junction protein expression and regulating microflora in a murine model of dextran sodium sulfate-induced colitis. Scand. J. Gastroenterol. 2018, 53, 1031–1042. [Google Scholar] [CrossRef]
- Carmody, E.E.; Schwarz, E.M.; Puzas, J.E.; Rosier, R.N.; O’Keefe, R.J. Viral interleukin-10 gene inhibition of inflammation, osteoclastogenesis, and bone resorption in response to titanium particles. Arthritis Rheumatol. 2002, 46, 1298–1308. [Google Scholar] [CrossRef]
- Evans, K.E.; Fox, S.W. Interleukin-10 inhibits osteoclastogenesis by reducing NFATc1 expression and preventing its translocation to the nucleus. BMC Cell Biol. 2007, 8, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dresner-Pollak, R.; Gelb, N.; Rachmilewitz, D.; Karmeli, F.; Weinreb, M. Interleukin 10-deficient mice develop osteopenia, decreased bone formation, and mechanical fragility of long bones. Gastroenterology 2004, 127, 792–801. [Google Scholar] [CrossRef]
- Huang, T.; Peng, X.Y.; Gao, B.; Wei, Q.L.; Xiang, R.; Yuan, M.G.; Xu, Z.H. The Effect of Clostridium butyricum on Gut Microbiota, Immune Response and Intestinal Barrier Function During the Development of Necrotic Enteritis in Chickens. Front. Microbiol. 2019, 10, 2309. [Google Scholar] [CrossRef] [PubMed]
- Maynard, C.L.; Harrington, L.E.; Janowski, K.M.; Oliver, J.R.; Zindl, C.L.; Rudensky, A.Y.; Weaver, C.T. Regulatory T cells expressing interleukin 10 develop from Foxp3+ and Foxp3- precursor cells in the absence of interleukin 10. Nat. Immunol. 2007, 8, 931–941. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, Y. Clinical immunity in bone and joints. J. Bone Miner. Metab. 2019, 37, 2–8. [Google Scholar] [CrossRef]
- Furusawa, Y.; Obata, Y.; Fukuda, S.; Endo, T.A.; Nakato, G.; Takahashi, D.; Nakanishi, Y.; Uetake, C.; Kato, K.; Kato, T.; et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013, 504, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Ma, X.; Liu, Y.; Ma, L.; Chen, Z.; Lin, X.; Si, L.; Ma, X.; Chen, X. Gut Microbiota Interventions With Clostridium butyricum and Norfloxacin Modulate Immune Response in Experimental Autoimmune Encephalomyelitis Mice. Front. Immunol. 2019, 10, 1662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H.; Jia, Y.; Weng, D.; Ju, Z.; Zhao, Y.; Liu, S.; Liu, Y.; Song, M.; Cui, L.; Sun, S.; et al. Clostridium butyricum Inhibits Fat Deposition via Increasing the Frequency of Adipose Tissue-Resident Regulatory T Cells. Mol. Nutr. Food Res. 2022, 66, e2100884. [Google Scholar] [CrossRef]
- Chen, C.; Dong, B.; Wang, Y.; Zhang, Q.; Wang, B.; Feng, S.; Zhu, Y. The role of Bacillus acidophilus in osteoporosis and its roles in proliferation and differentiation. J. Clin. Lab. Anal. 2020, 34, e23471. [Google Scholar] [CrossRef]
- Schroeder, T.M.; Westendorf, J.J. Histone deacetylase inhibitors promote osteoblast maturation. J. Bone Miner. Res. 2005, 20, 2254–2263. [Google Scholar] [CrossRef]
- Song, M.; Jiao, H.; Zhao, J.; Wang, X.; Li, H.; Wang, P.; Ma, B.; Sun, S.; Lin, H. Dietary Supplementation of Calcium Propionate and Calcium Butyrate Improves Eggshell Quality of Laying Hens in the Late Phase of Production. J. Poult. Sci. 2022, 59, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Lin, X.; Zhao, J.; Wang, X.; Jiao, H.; Li, H.; Sun, S.; Lin, H. High frequency vaccination-induced immune stress reduces bone strength with the involvement of activated osteoclastogenesis in layer pullets. Poult. Sci. 2020, 99, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Yang, X.; Wang, N.; Zhang, Y.; Cai, G. Tigogenin inhibits adipocytic differentiation and induces osteoblastic differentiation in mouse bone marrow stromal cells. Mol. Cell. Endocrinol. 2007, 270, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Cui, Q.; Kao, C.; Wang, G.J.; Balian, G. Lovastatin inhibits adipogenic and stimulates osteogenic differentiation by suppressing PPARgamma2 and increasing Cbfa1/Runx2 expression in bone marrow mesenchymal cell cultures. Bone 2003, 33, 652–659. [Google Scholar] [CrossRef]


| Test Items | Test Result | Unit | Test Basis |
|---|---|---|---|
| Acetic acid | 247.27 | μg/g | GCMS |
| Propionic acid | Not detected | μg/g | GCMS |
| Isobutyric acid | Not detected | μg/g | GCMS |
| n-Butyric acid | 866.50 | μg/g | GCMS |
| Isovaleric acid | Not detected | μg/g | GCMS |
| n-Valeric acid | Not detected | μg/g | GCMS |
| Items | Composition, % |
|---|---|
| Ingredients | |
| Corn | 63 |
| Soybean meal | 24 |
| Limestone | 8 |
| NaCl | 0.3 |
| Choline chloride (50%) | 0.1 |
| Premix 1 | 4.6% |
| Total | 100 |
| Nutrient levels 2 | |
| Metabolizable energy (Kcal/kg) | 2700 |
| Crude protein (%) | 16.1 |
| Lysine (%) | 0.79 |
| Methionine (%) | 0.34 |
| Calcium (%) | 3.50 |
| Available phosphorus (%) | 0.45 |
| Gene Name | Genbank Number | Primer Position | Primer Sequences (5′→3′) |
|---|---|---|---|
| IL-1 | Y15006 | Forward | ATCACAGCCACACAGAAGACG |
| Reverse | TGACTTTCCCCACAGCCTTA | ||
| IL-6 | NM204628.2 | Forward | CTCCTCGCCAATCTGAAGTC |
| Reverse | AGGCACTGAAACTCCTGGTC | ||
| IL-10 | NM204100.1 | Forward | CGCTGTCACCGCTTCTTCA |
| Reverse | TCCCGTTCTCATCCATCTTCTC | ||
| TNF-α | AY765397 | Forward | CATTTGGAAGCAGCGTTTGG |
| Reverse | GGTTGTGGGACAGGGTAGGG | ||
| NF-κB | NM205129 | Forward | CTCTCCCAGCCCATCTATGA |
| Reverse | CCTCAGCCCAGAAACGAAC | ||
| RANKL | NM001083361.2 | Forward | TGTTGGCTCTGATGCTTGTC |
| Reverse | TCCTGCTTCTGGCTCTCAAT | ||
| OPG | DQ098013.1 | Forward | CGCTTGTGCTCTTGGACATT |
| Reverse | GCTGCTTTACGTAGCTCCCA | ||
| BMP2 | NM001398170.1 | Forward | CCTTCGGAAGACGTCCTCAG |
| Reverse | CTGAGTGCCTGCGGTACAGA | ||
| RUNX2 | NM204128.1 | Forward | TTTTTCCTGCCCGTATTCTG |
| Reverse | GCTTGGTGCTGGAGAGTCTT | ||
| Wnt3a | EF068232.1 | Forward | GTGGCTTTTGCAGTGACCAG |
| Reverse | GTTGTGCCTTCATGGCTG | ||
| Wnt5a | NM001037269.1 | Forward | TGGCTTCTCAGTACCTCGTAGTGG |
| Reverse | GCCGAAGACGGACGTGTTGTC | ||
| β-actin | L08165 | Forward | GAGAAATTGTGCGTGACATCAAGG |
| Reverse | CACCTGAACCTCTCATTGCCA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, M.; Zhang, X.; Hao, G.; Lin, H.; Sun, S. Clostridium butyricum Can Promote Bone Development by Regulating Lymphocyte Function in Layer Pullets. Int. J. Mol. Sci. 2023, 24, 1457. https://doi.org/10.3390/ijms24021457
Song M, Zhang X, Hao G, Lin H, Sun S. Clostridium butyricum Can Promote Bone Development by Regulating Lymphocyte Function in Layer Pullets. International Journal of Molecular Sciences. 2023; 24(2):1457. https://doi.org/10.3390/ijms24021457
Chicago/Turabian StyleSong, Mengze, Xuesong Zhang, Guijuan Hao, Hai Lin, and Shuhong Sun. 2023. "Clostridium butyricum Can Promote Bone Development by Regulating Lymphocyte Function in Layer Pullets" International Journal of Molecular Sciences 24, no. 2: 1457. https://doi.org/10.3390/ijms24021457





