The Effect of Er,Cr:YSGG and Diode Laser Applications on Dental Implant Surfaces Contaminated with Acinetobacter Baumannii and Pseudomonas Aeruginosa
Abstract
:1. Literature Survey
2. Material and Methodology
2.1. Manipulation
2.2. Decontamination
2.3. Analysis of Decontamination
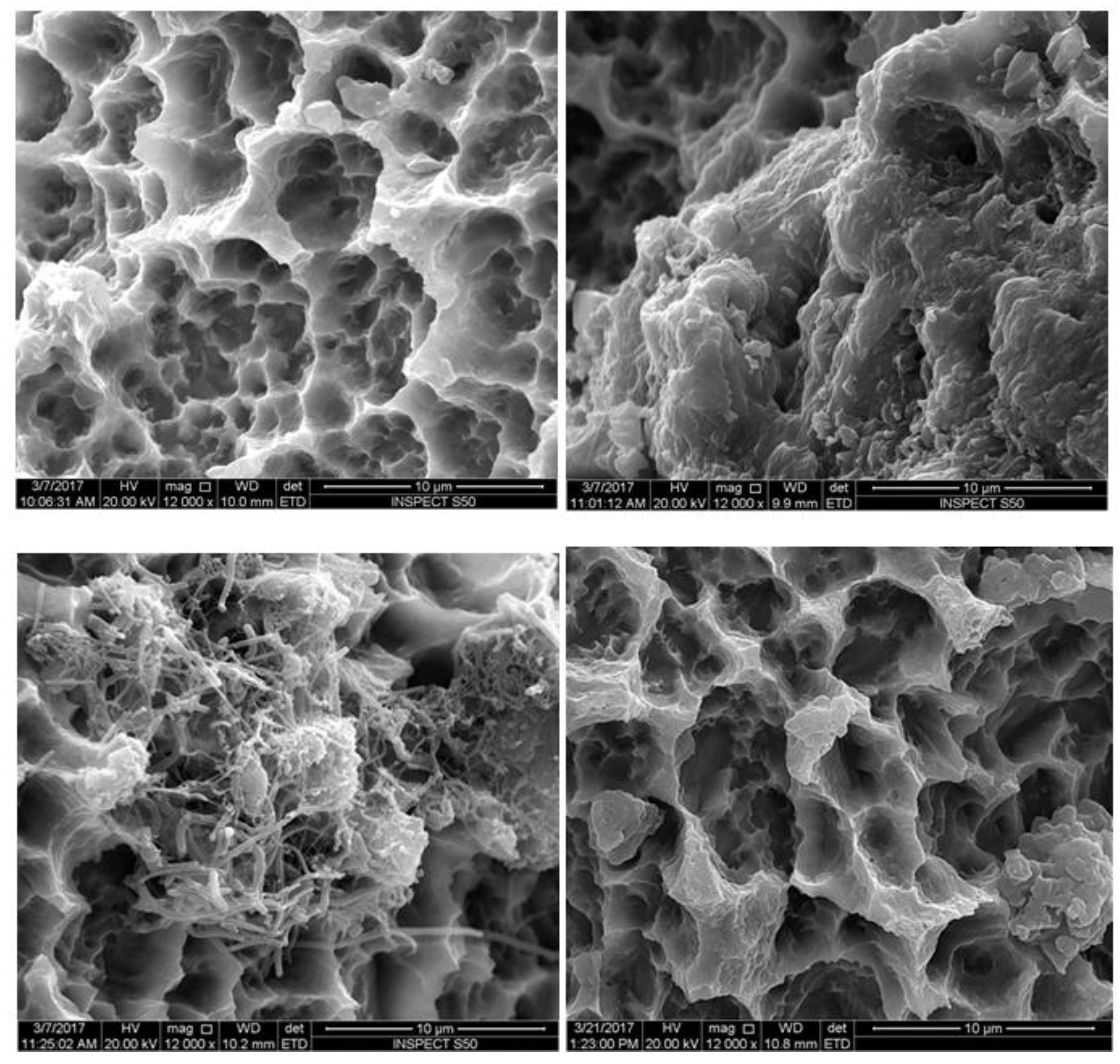
2.4. SEM Evaluation
2.5. Statistical Analysis
3. Results
SEM Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lindhe, J.; Meyle, J. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [Green Version]
- Esposito, M.; Grusovin, M.G.; Coulthard, P.; Worthington, H.V. The efficacy of interventions to treat peri-implantitis: A Cochrane systematic review of randomised controlled clinical trials. Eur. J. Oral Implantol. 2008, 1, 2. [Google Scholar]
- Koo, K.-T.; Khoury, F.; Keeve, P.L.; Schwarz, F.; Ramanauskaite, A.; Sculean, A.; Romanos, G. Implant Surface Decontamination by Surgical Treatment of Periimplantitis. Implant Dent. 2019, 28, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Toma, S.; Behets, C.; Brecx, M.C.; Lasserre, J.F. In Vitro Comparison of the Efficacy of Peri-Implantitis Treatments on the Removal and Recolonization of Streptococcus gordonii Biofilm on Titanium Disks. Masteries 2018, 11, 2484. [Google Scholar] [CrossRef] [PubMed]
- Louropoulou, A.; Slot, D.E.; Van der Weijden, F. The effects of mechanical instruments on contaminated titanium dental implant surfaces: A systematic review. Clin. Oral Implants Res. 2014, 25, 1149–1160. [Google Scholar] [CrossRef]
- Al-Hashedi, A.A.; Laurenti, M.; Abdallah, M.-N.; Albuquerque, R.F., Jr.; Tamimi, F. Electrochemical Treatment of Contaminated Titanium Surfaces in Vitro: An Approach for Implant Surface Decontamination. ACS Biomater. Sci. Eng. 2016, 2, 1504–1518. [Google Scholar] [CrossRef]
- Al-Hashedi, A.A.; Laurenti, M.; Benhamou, V.; Tamimi, F. Decontamination of titanium implants using physical methods. Clin. Oral Implants Res. 2017, 28, 1013–1021. [Google Scholar] [CrossRef]
- Alotaibi, M.; Moran, G.; Grufferty, B.; Renvert, S.; Polyzois, I. The effect of a decontamination protocol on contaminated titanium dental implant surfaces with different surface topography in edentulous patients. Acta Odontol. Scand. 2019, 77, 66–75. [Google Scholar] [CrossRef]
- Htet, M.; Madi, M.; Zakaria, O.; Miyahara, T.; Xin, W.; Lin, Z.; Aoki, K.; Kasugai, S.; Zakaria, O. Decontamination of Anodized Implant Surface with Different Modalities for Peri-Implantitis Treatment: Lasers and Mechanical Debridement with Citric Acid. J. Periodontol. 2016, 87, 953–961. [Google Scholar] [CrossRef]
- Madi, M.; Htet, M.; Zakaria, O.; Alagl, A.; Kasugai, S. Re-osseointegration of dental implants after periimplantitis treatments: A systematic review. Implant Dent. 2018, 27, 101–110. [Google Scholar] [CrossRef]
- Louropoulou, A.; Slot, D.E.; Van der Weijden, F.A. Titanium surface alterations following the use of different mechanical instruments: A systematic review. Clin. Oral Implants Res. 2012, 23, 643–658. [Google Scholar] [CrossRef]
- Parlar, A.; Bosshardt, D.D.; Çetiner, D.; Schafroth, D.; Ünsal, B.; Haytaç, C.; Lang, N.P. Effects of decontamination and implant surface characteristics on re-osseointegration following treatment of peri-implantitis. Clin. Oral Implants Res. 2009, 20, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Stübinger, S.; Henke, J.; Donath, K.; Deppe, H. Bone regeneration after peri-implant care with the CO2 laser: A fluorescence microscopy study. Int. J. Oral Maxillofac. Implant. 2005, 20, 203–210. [Google Scholar]
- Marotti, J.; Geraldo-Martins, V.R.; Bello-Silva, M.S.; de Paula Eduardo, C.; Apel, C.; Gutknecht, N. Influence of etching with erbium, chromium:yttrium-scandium-gallium-garnet laser on microleakage of class V restoration. Lasers Med. Sci. 2010, 25, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Kreisler, M.; Al Haj, H.; D’Hoedt, B. Temperature changes induced by 809-nm GaAlAs laser at the implant-bone interface during simulated surface decontamination. Clin. Oral Implants Res. 2003, 14, 91–96. [Google Scholar] [CrossRef]
- Ting, C.-C.; Fukuda, M.; Watanabe, T.; Aoki, T.; Sanaoka, A.; Noguchi, T. Effects of Er,Cr:YSGG Laser Irradiation on the Root Surface: Morphologic Analysis and Efficiency of Calculus Removal. J. Periodontol. 2007, 78, 2156–2164. [Google Scholar] [CrossRef]
- Schwarz, F.; Nuesry, E.; Bieling, K.; Herten, M.; Becker, J. Influence of an Erbium, Chromium-Doped Yttrium, Scandium, Gallium, and Garnet (Er,Cr:YSGG) Laser on the Reestablishment of the Biocompatibility of Contaminated Titanium Implant Surfaces. J. Periodontol. 2006, 77, 1820–1827. [Google Scholar] [CrossRef]
- Strever, J.M.; Lee, J.; Ealick, W.; Peacock, M.; Shelby, D.; Susin, C.; Mettenberg, D.; El-Awady, A.; Rueggeberg, F.; Cutler, C.W. Erbium, Chromium:Yttrium-Scandium-Gallium-Garnet Laser Effectively Ablates Single-Species Biofilms on Titanium Disks Without Detectable Surface Damage. J. Periodontol. 2017, 88, 484–492. [Google Scholar] [CrossRef]
- Romanos, G.; Crespi, R.; Barone, A.; Covani, U. Osteoblast attachment on titanium disks after laser irradiation. Int. J. Oral Maxillofac. Implant. 2006, 21, 232–236. [Google Scholar]
- Takasaki, A.A.; Aoki, A.; Mizutani, K.; Schwarz, F.; Sculean, A.; Wang, C.Y.; Koshy, G.; Romanos, G.; Ishikawa, I.; Izumi, Y. Application of antimicrobial photodynamic therapy in periodontal and peri-implant diseases. Periodontology 2000, 51, 109–140. [Google Scholar] [CrossRef]
- Romanos, G.E.; Gutknecht, N.; Dieter, S.; Schwarz, F.; Crespi, R.; Sculean, A. Laser wavelengths and oral implantology. Lasers Med Sci. 2009, 24, 961–970. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Cataldo, M.; Dancer, S.; De Angelis, G.; Falcone, M.; Frank, U.; Kahlmeter, G.; Pan, A.; Petrosillo, N.; Rodríguez-Baño, J.; et al. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant Gram-negative bacteria in hospitalized patients. Clin. Microbiol. Infect. 2014, 20, 1–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marotti, J.; Tortamano, P.; Cai, S.; Ribeiro, M.S.; Franco, J.E.; de Campos, T.T. Decontamination of dental implant surfaces by means of photodynamic therapy. Lasers Med Sci. 2013, 28, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Giannelli, M.; Landini, G.; Materassi, F.; Chellini, F.; Antonelli, A.; Tani, A.; Zecchi-Orlandini, S.; Rossolini, G.M.; Bani, D. The effects of diode laser on Staphylococcus aureus biofilm and Escherichia coli lipopolysaccharide adherent to titanium oxide surface of dental implants. An in vitro study. Lasers Med. Sci. 2016, 31, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Ušjak, D.; Ivković, B.; Božić, D.D.; Bošković, L.; Milenković, M. Antimicrobial activity of novel chalcones and modulation of virulence factors in hospital strains of Acinetobacter baumannii and Pseudomonas aeruginosa. Microb. Pathog. 2019, 131, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Moley, J.P.; McGrath, M.S.; Granger, J.F.; Stoodley, P.; Dusane, D.H. Reduction in Pseudomonas aeruginosa and Staphylococcus aureus biofilms from implant materials in a diffusion dominated environment. J. Orthop. Res. 2018, 36, 3081–3085. [Google Scholar] [CrossRef]
- Miles, A.A.; Misra, S.S.; Irwin, J.O. The estimation of the bactericidal power of the blood. J. Hyg. 1938, 38, 732. [Google Scholar] [CrossRef] [PubMed]
- Souto, R.; Silva-Boghossian, C.M.; Colombo, A.P.V. Prevalence of Pseudomonas aeruginosa and Acinetobacter spp. in subgingival biofilm and saliva of subjects with chronic periodontal infection. Braz. J. Microbiol. 2014, 45, 495–501. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, L.S.; Souto, R.; Colombo, A.P.V. Detection of Helicobacter pylori, Enterococcus faecalis, and Pseudomonas aeruginosa in the subgingival biofilm of HIV-infected subjects undergoing HAART with chronic periodontitis. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 1335–1342. [Google Scholar] [CrossRef]
- Zuanazzi, D.; Souto, R.; Mattos, M.B.A.; Zuanazzi, M.R.; Tura, B.R.; Sansone, C.; Colombo, A.P.V. Prevalence of potential bacterial respiratory pathogens in the oral cavity of hospitalised individuals. Arch. Oral Boil. 2010, 55, 21–28. [Google Scholar] [CrossRef]
- Da Silva-Boghossian, C.M.; Souto, R.M.D.; Luiz, R.R.; Colombo, A.P.V. Association of red complex, A. actinomycetemcomitans and non-oral bacteria with periodontal diseases. Arch. Oral Boil. 2011, 56, 899–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sousa, V.; Nibali, L.; Spratt, D.; Dopico, J.; Mardas, N.; Petrie, A.; Donos, N. Peri-implant and periodontal microbiome diversity in aggressive periodontitis patients: A pilot study. Clin. Oral Implants Res. 2017, 28, 558–570. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, L.F.; Watt, R.M.; Mattheos, N.; Si, M.S.; Lai, H.C.; Lang, N.P. Periodontal and peri-implant microbiota in patients with healthy and inflamed periodontal and peri-implant tissues. Clin. Oral Implants Res. 2016, 27, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Albertini, M.; Lopez-Cerero, L.; O’Sullivan, M.G.; Chereguini, C.F.; Ballesta, S.; Rios, V.; Herrero-Climent, M.; Bullon, P. Assessment of periodontal and opportunistic flora in patients with peri-implantitis. Clin. Oral Implants Res. 2015, 26, 937–941. [Google Scholar] [CrossRef] [PubMed]
- Colombo, A.V.; Barbosa, G.M.; Higashi, D.; Di Micheli, G.; Rodrigues, P.H.; Simionato, M.R.L. Quantitative detection of Staphylococcus aureus, Enterococcus faecalis and Pseudomonas aeruginosa in human oral epithelial cells from subjects with periodontitis and periodontal health. J. Med Microbiol. 2013, 62, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Yoon, S.S. Pseudomonas aeruginosa biofilm, a programmed bacterial life for fitness. J. Microbiol. Biotechnol. 2017, 27, 1053–1064. [Google Scholar] [PubMed]
- Marti, S.; Soto, S.M.; Cisneros, J.; Pachón, J.; Pascual, A.; McQueary, C.; Actis, L.; Vilá, J.; Rodríguez-Baño, J.; Martínez-Martínez, L.; et al. Biofilm formation in Acinetobacter baumannii: Associated features and clinical implications. Clin. Microbiol. Infect. 2008, 14, 276–278. [Google Scholar]
- Bogdan, M.; Drenjancevic, D.; Harsanji Drenjancevic, I.; Bedenic, B.; Zujic Atalic, V.; Talapko, J.; Vukovic, D. In vitro effect of subminimal inhibitory concentrations of antibiotics on the biofilm formation ability of Acinetobacter baumannii clinical isolates. J. Chemother. (Florence, Italy) 2018, 30, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Saffarpour, A.; Nozari, A.; Fekrazad, R.; Saffarpour, A.; Heibati, M.N.; Iranparvar, K. Microstructural Evaluation of Contaminated Implant Surface Treated by Laser, Photodynamic Therapy, and Chlorhexidine 2 percent. Int. J. Oral Maxillofac. Implants 2018, 33, 1019–1026. [Google Scholar] [CrossRef] [PubMed]



| Groups | Group A Implants Contaminated with A. Baumannii | Group B Implants Contaminated with P. Aeruginosa | Decontamination Method | Watt | Time |
|---|---|---|---|---|---|
| Group I | 5 implants | 5 implants | Er,Cr:YSGG (2780 nm H mode) | 1 W, 30 Hz, Air and water 50% contact mode 2 mm (120 J) then 3 mL PBS (twice) | 60 s |
| Group II | 5 implants | 5 implants | 650 Diode + TBO 1mg/mL (5 min in dark) | 50 mW contact mode 2 mm (60 J) then 3 mL PBS (twice) | 60 s |
| Group III | 5 implants | 5 implants | 808 Diode | 1 W contact mode 2 mm (120 J) then 3 mL PBS (twice) | 60 s |
| Group IV | 5 implants | 5 implants | CHX 0.12% | then washed with 3 mL PBS (twice) | 120 s |
| Group V | 5 implants | 5 implants | Bacterial contamination only |
| Study Groups | Acinetobacter Baumannii | Pseudomonas Aeruginosa |
|---|---|---|
| Group I Er,Cr:YSGG (2790 nm) | 1.2 ± 1.3 a | 1.4 ± 1.3 a |
| Gp II PDT | 9176 ± 401 b | 7673 ± 307 b |
| Gp III 808 | 4360 ± 421 c | 8156 ± 552 b |
| Gp IV CHX | 1536 ± 382 d | 1464 ± 207 c |
| GpV cont | 10,880 ± 563 e | 12,362 ± 481 d |
| p value | <0.0001 * | <0.0001 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alagl, A.S.; Madi, M.; Bedi, S.; Al Onaizan, F.; Al-Aql, Z.S. The Effect of Er,Cr:YSGG and Diode Laser Applications on Dental Implant Surfaces Contaminated with Acinetobacter Baumannii and Pseudomonas Aeruginosa. Materials 2019, 12, 2073. https://doi.org/10.3390/ma12132073
Alagl AS, Madi M, Bedi S, Al Onaizan F, Al-Aql ZS. The Effect of Er,Cr:YSGG and Diode Laser Applications on Dental Implant Surfaces Contaminated with Acinetobacter Baumannii and Pseudomonas Aeruginosa. Materials. 2019; 12(13):2073. https://doi.org/10.3390/ma12132073
Chicago/Turabian StyleAlagl, Adel S., Marwa Madi, Sumit Bedi, Faisal Al Onaizan, and Zainab S. Al-Aql. 2019. "The Effect of Er,Cr:YSGG and Diode Laser Applications on Dental Implant Surfaces Contaminated with Acinetobacter Baumannii and Pseudomonas Aeruginosa" Materials 12, no. 13: 2073. https://doi.org/10.3390/ma12132073
APA StyleAlagl, A. S., Madi, M., Bedi, S., Al Onaizan, F., & Al-Aql, Z. S. (2019). The Effect of Er,Cr:YSGG and Diode Laser Applications on Dental Implant Surfaces Contaminated with Acinetobacter Baumannii and Pseudomonas Aeruginosa. Materials, 12(13), 2073. https://doi.org/10.3390/ma12132073




