Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible
Abstract
:1. Introduction
1.1. Epidemiological Information
1.2. Surgical Procedures
1.3. Biomechanics of the Mandible
1.4. Osseosynthesis Plates
1.5. Aim
2. Materials and Methods
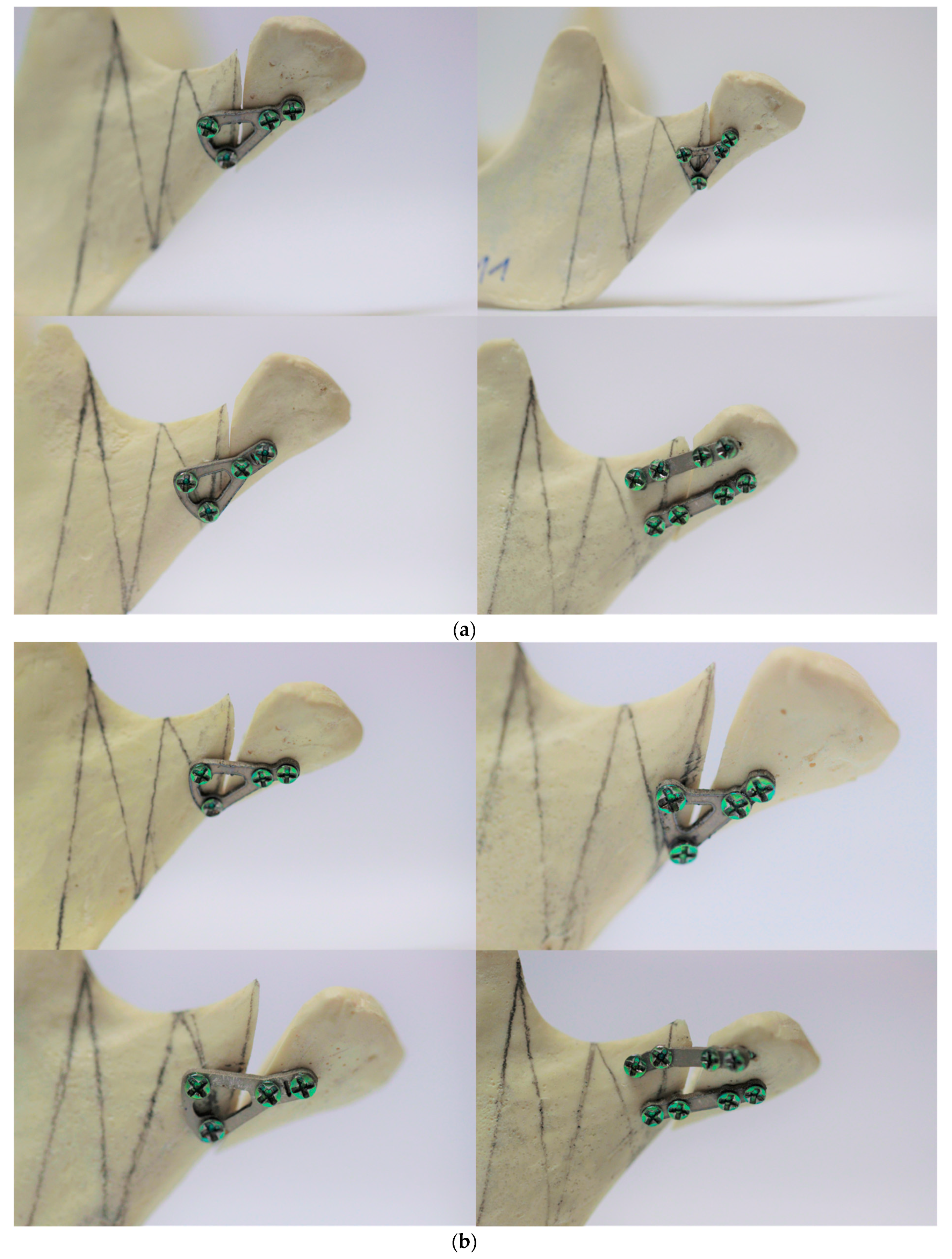
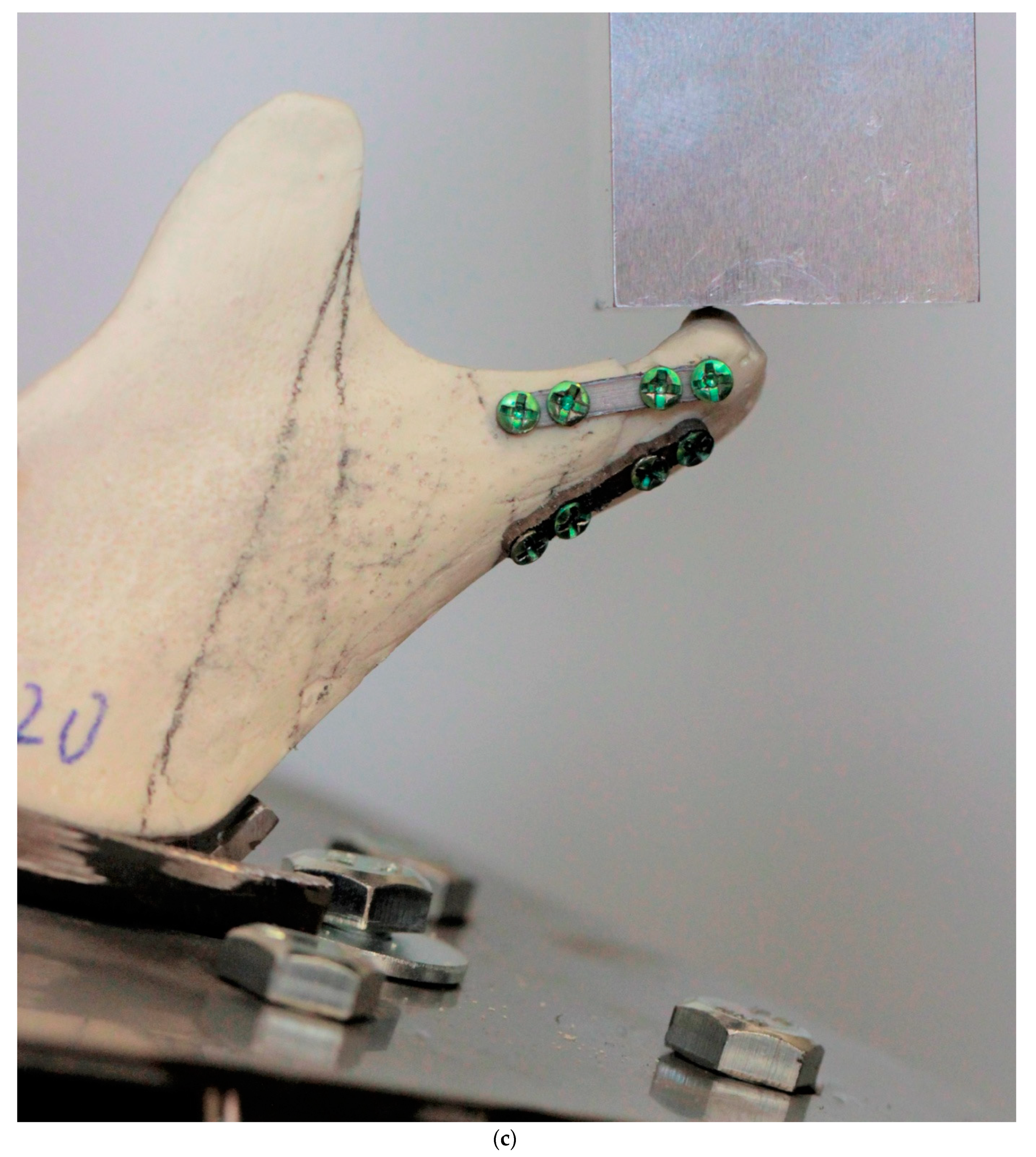
2.1. Mandibles
2.2. Plates
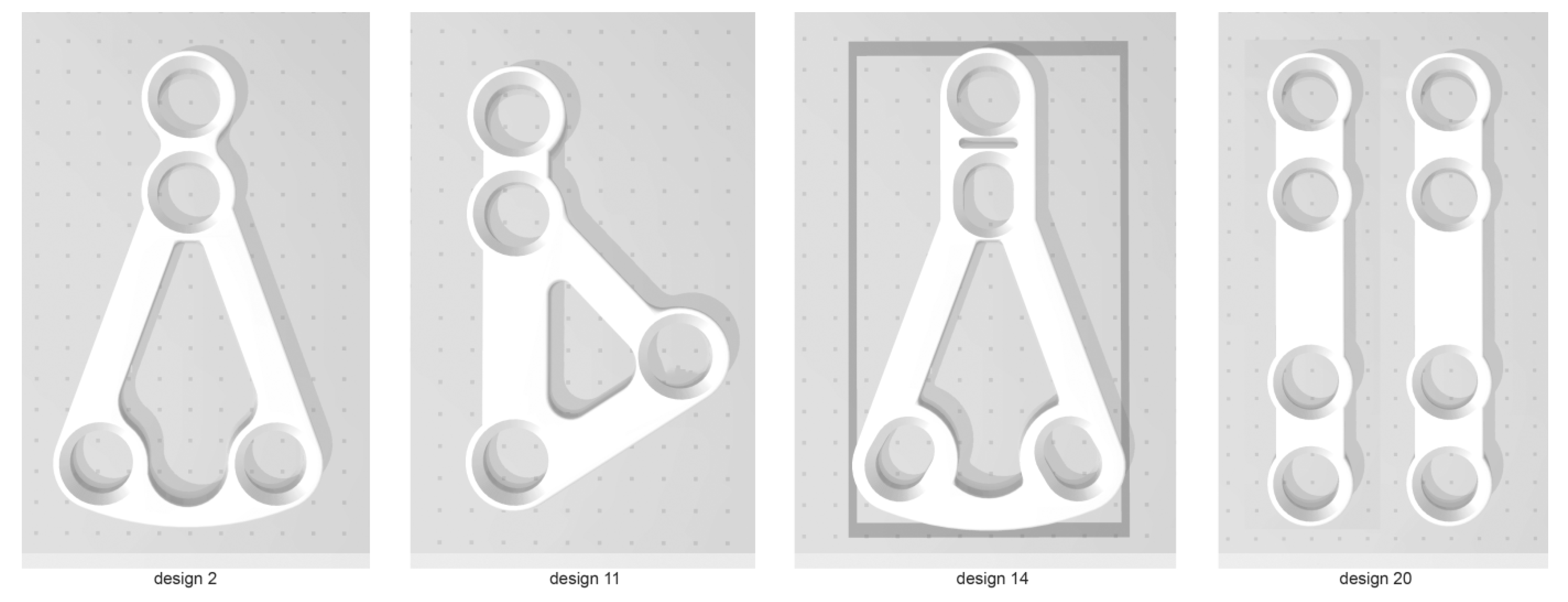
2.3. Simulation Set
2.4. Statistical Analysis
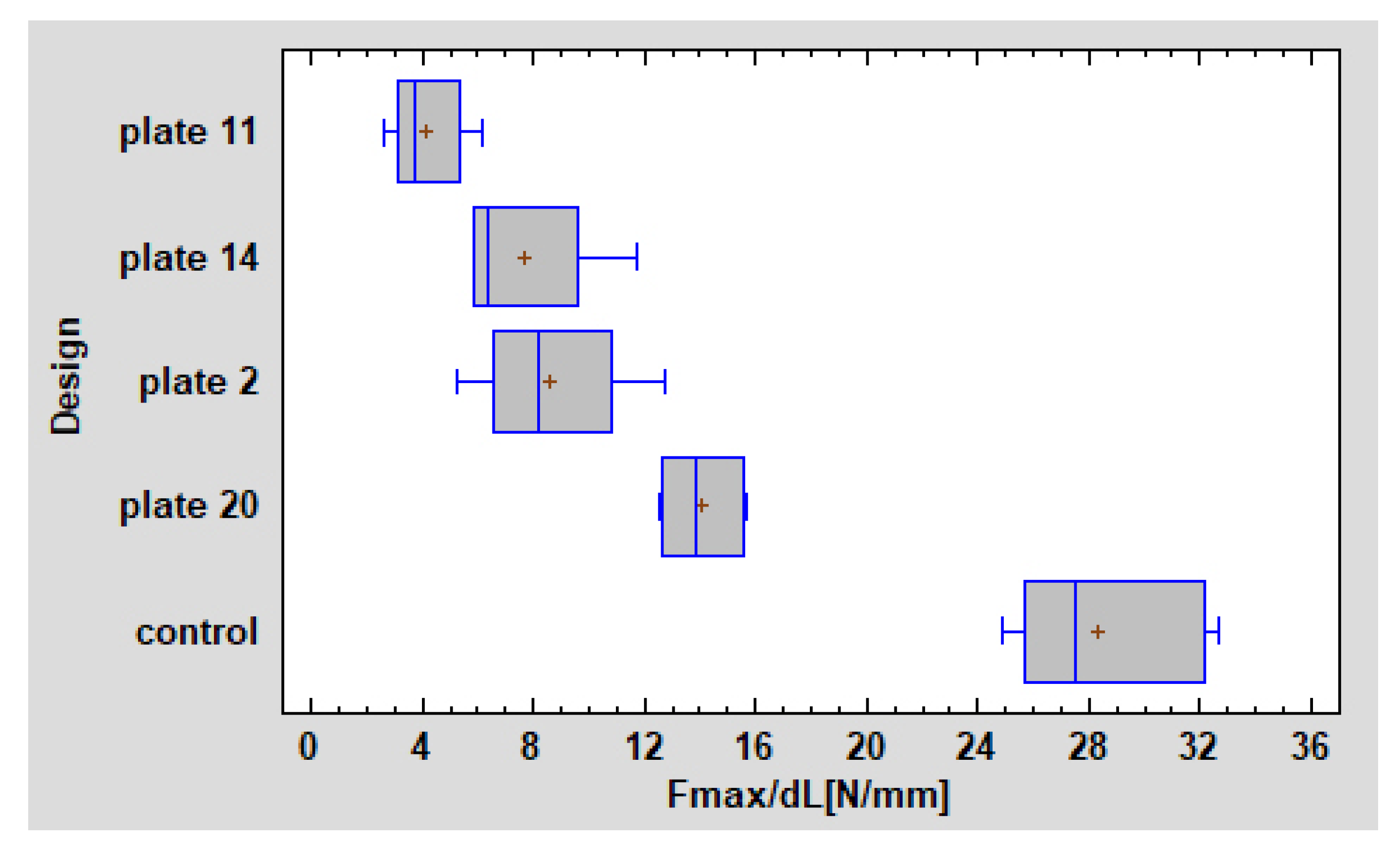
3. Results
4. Discussion
4.1. Plates Combination
4.2. Finite Element Method (FEM)
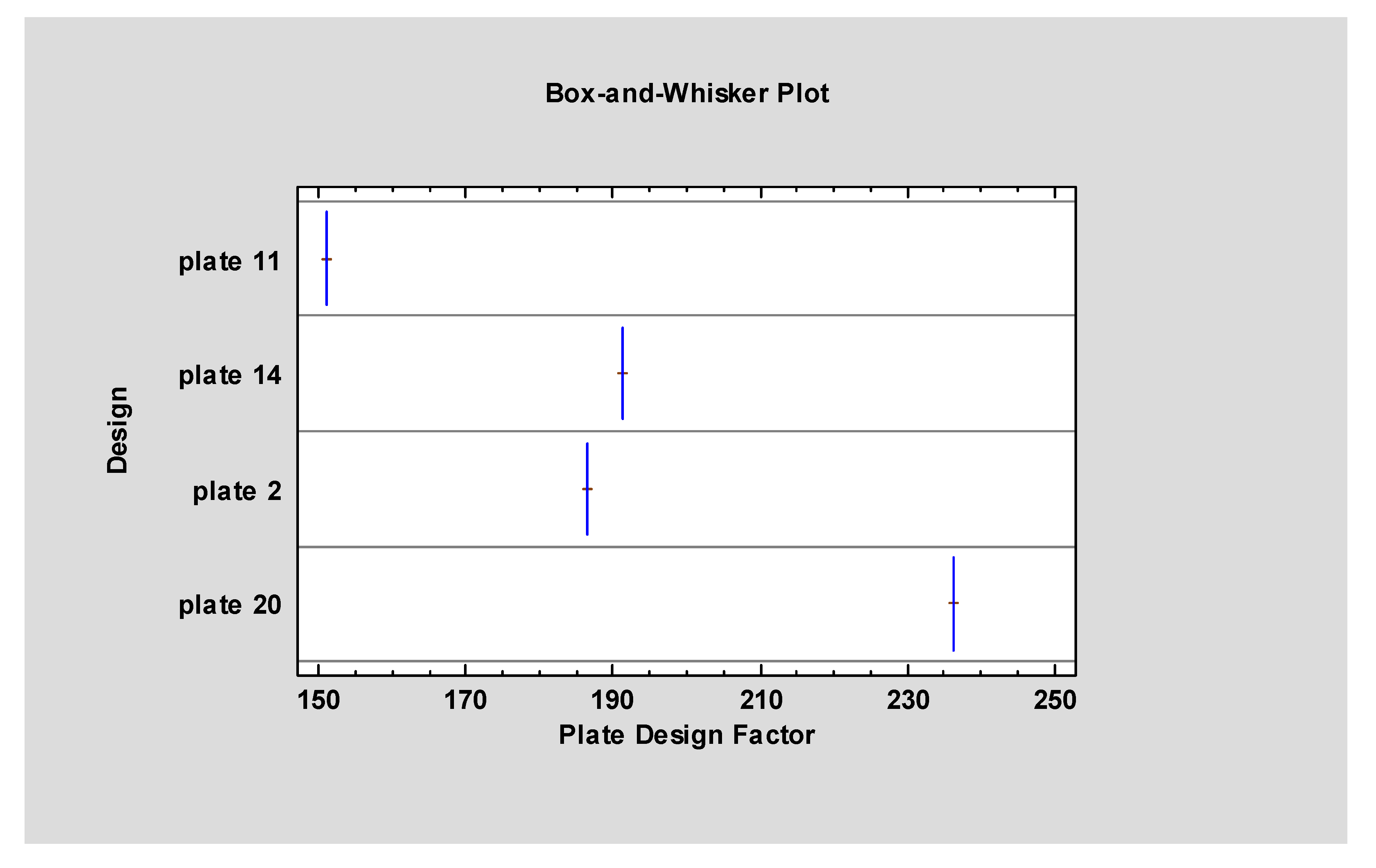
4.3. Plate Design Factor (PDF)
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Asprino, L.; Consani, S.; De Moraes, M. A comparative biomechanical evaluation of mandibular fracture plating techniques. J. Oral Maxillofac. Surg. 2006, 64, 452–456. [Google Scholar] [CrossRef]
- Chrcanovic, B. Surgical versus non-surgical treatment of mandibular condylar fractures: A meta-analysis. Int. J. Oral Maxillofac. Surg. 2015, 44, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-T.; Feng, C.-H.; Tsay, P.-K.; Lai, J.-P.; Chen, Y.-R. Functional outcomes following surgical treatment of bilateral mandibular condylar fractures. Int. J. Oral Maxillofac. Surg. 2011, 40, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Ehrenfeld, M.; Manson, P.N.; Prein, J. Thieme, Principles of Internal Fixation of the Craniomaxillofacial Skeleton Trauma and Orthognathic Surgery; AO Publishing: Stockholm, Sweden, 2012. [Google Scholar] [CrossRef]
- Abdel-Galil, K.; Loukota, R. Review: Fractures of the mandibular condyle: Evidence base and current concepts management. Br J Oral MaxillofacSurg 2010, 48, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Al-Moraissi, E.A.; Ellis, E. Surgical Treatment of Adult Mandibular Condylar Fractures Provides Better Outcomes Than Closed Treatment: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2015, 73, 482–493. [Google Scholar] [CrossRef]
- Neff, A.; Chossegros, C.; Blanc, J.; Chanpsaur, P.; Cheynet, F.; Devauchelle, B.; Eckelt, U.; Ferri, J.; Gabrielli, M.F.R.; Guyot, L.; et al. Position paper from the IBRA symposium on surgery of the head-the 2nd international Simposium for condylar fracture Osteosynthesis, Marseille, France 2012. J CraniomaxillofacSurg 2014, 42, 1234–1249. [Google Scholar] [CrossRef] [Green Version]
- Bredbenner, T.L.; Haug, R.H. Substitutes for human cadaveric bone in maxillofacial rigid fixation research. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 2000, 90, 574–580. [Google Scholar] [CrossRef]
- Montazem, A.H.; Anastassov, G. Management of Condylar Fractures. Atlas Oral Maxillofac. Surg. Clin. 2009, 17, 55–69. [Google Scholar] [CrossRef]
- Zachariades, N.; Mezitis, M.; Mourouzis, C. Fractures of themandibular condyle: A reviewof 466 cases. Literature review, reflections on treatment and proposals. J CraniomaxillofacSurg 2006, 34, 421–432. [Google Scholar] [CrossRef]
- Silvennoinen, U.; Iizuka, T.; Oikarinen, K. Analysis of possibile factors leading to problems after surgical treatment of condylar fractures. J Oral MaxillofacSurg 1994, 52, 793–799. [Google Scholar] [CrossRef]
- Newman, L. A clinical evaluation of the long-term outcome of patients treated for bilateral fracture of the mandibular condyles. Br. J. Oral Maxillofac. Surg. 1998, 36, 176–179. [Google Scholar] [CrossRef]
- De Riu, G.; Gamba, U.; Anghinoni, M. A comparison of open and closed treatment of condylar fractures: A change in philosophy. Int J Oral MaxillofacSurg 2001, 30, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Villarreal, P.M.; Monje, F.; Junquera, L.M.; Mateo, J.; Morillo, A.J.; González, C. Mandibular condyle fractures: Determinants of treatment and outcome. J. Oral Maxillofac. Surg. 2004, 62, 155–163. [Google Scholar] [CrossRef]
- Achour, A.B.; Meißner, H.; Teicher, U.; Haim, D.; Range, U.; Brosius, A.; Lauer, G. Biomechanical Evaluation of Mandibular Condyle Fracture Osteosynthesis Using the Rhombic Three-Dimensional Condylar Fracture Plate. J. Oral Maxillofac. Surg. 2019, 77, 1868.e1–1868.e15. [Google Scholar]
- Emam, H.A.; Jatana, C.A.; Ness, G.M. Matching Surgical Approach to Condylar Fracture Type. Atlas Oral Maxillofac. Surg. Clin. 2017, 25, 55–61. [Google Scholar] [CrossRef]
- Wagner, A.; Krach, W.; Schicho, K.; Undt, G.; Ploder, O.; Ewers, R. A 3-dimensional finite-element analysis investigating the biomechanical behavior of the mandible and plate osteosynthesis in cases of fractures of the condylar process. Oral Surgery, Oral Med. Oral Pathol. Oral Radiol. Endodontology 2002, 94, 678–686. [Google Scholar] [CrossRef]
- Meyer, C.; Kahn, J.L.; Boutemi, P. Photoelastic analysis of bone deformation in the region of the mandibular condyle Turing mastication. J CraniomaxillofacSurg 2002, 30, 160e9. [Google Scholar]
- Sikes, J.W., Jr.; Smith, B.R.; Mukherjee, D.P. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible Model.Including commentary by Tucker MR. J Oral MaxillofacSurg 2000, 58, 56e61. [Google Scholar]
- Trainor, P.; McLachlan, K.; McCall, W. Modelling of forces in the human masticatory system with optimization of the angulations of the joint loads. J. Biomech. 1995, 28, 829–843. [Google Scholar] [CrossRef]
- Tuchtan, L.; Piercecchi-Marti, M.-D.; Bartoli, C.; Boisclair, D.; Adalian, P.; Leonetti, G.; Behr, M.; Thollon, L. Forces transmission to the skull in case of mandibular impact. Forensic Sci. Int. 2015, 252, 22–28. [Google Scholar] [CrossRef]
- Kozakiewicz, M.; Zieliński, R.; Krasowski, M.; Okulski, J. Forces causing one-millimeter displacement of bonefragments of condylar base fractures of the mandible after fixation by All available plate designs. Materials (Basel) 2019, 12, 3122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, S. The mechanical properties of trabecular bone: Dependence on anatomic location and function. J. Biomech. 1987, 20, 1055–1061. [Google Scholar] [CrossRef] [Green Version]
- Chapman, J.R.; Harrington, R.M.; Lee, K.M.; Anderson, P.A.; Tencer, A.F.; Kowalski, D. Factors Affecting the Pullout Strength of Cancellous Bone Screws. J. Biomech. Eng. 1996, 118, 391–398. [Google Scholar] [CrossRef] [PubMed]
- ASTMF 1839-08. Standard Specification for Rigid Polyurethane Foam for Use as a Standard Material for Testing Orthopaedic Devices and Instruments; ASTM International: West Conshohocken, PA, USA, 2016. [Google Scholar]
- Kozakiewicz, M. Comparison of compression screws used for mandible head fracture treatment—Experimentalstudy. Clin. oral Investig. 2019, 23, 4059–4066. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assari, S.; Darvish, K.; Ilyas, A.M. Biomechanical analysis of second-generation headless compression screws. Inj. 2012, 43, 1159–1165. [Google Scholar] [CrossRef]
- Baran, O.; Sagol, E.; Oflaz, H.; Sarikanat, M.; Havitcioglu, H. Abiomechanical study on preloaded compression effect on headless screws. Arch. Orthop. Trauma. Surg. 2009, 129, 1601–1605. [Google Scholar] [CrossRef]
- Ramaswamy, R.; Evans, S.; Kosashvili, Y. Holding power of variable pitch screws in osteoporotic, osteopenic and normal bone: Are all screws created equal? Inj. 2010, 41, 179–183. [Google Scholar] [CrossRef]
- Bailey, C.A.; Kuiper, J.H.; Kelly, C.P. Biomechanical Evaluation of a New Composite Bioresorbable Screw. J. Hand Surg. 2006, 31, 208–212. [Google Scholar] [CrossRef]
- Kozakiewicz, M. Classification proposal for fractures of the processuscondylaris mandibulae. Clin. Oral Investig. 2018, 23, 485–491. [Google Scholar] [CrossRef] [Green Version]
- Choi, B.-H.; Kim, K.-N.; Kim, H.-J.; Kim, M.-K. Evaluation of condylar neck fracture plating techniques. J. Cranio-Maxillofacial Surg. 1999, 27, 109–112. [Google Scholar] [CrossRef]
- Cienfuegos, R.; Cornelius, C.; Ellis, E.I.; Kushner, G.M. Condylar Process and Head; Ellis, E., Figari, M., Aniceto, G., Shimozato, K., Eds.; AO CMF Surgery Reference; AO Foundation: New York, NY, USA; Thieme Publisher: New York, NY, USA, 2014. [Google Scholar]
- Kozakiewicz, M.; Świniarski, J. Treatment of high fracture of the neck of the mandibular condylar process by rigid fixation performed by lag screws: Finite element analysis. Dent Med. Probl. 2017, 54, 223–228. [Google Scholar] [CrossRef] [Green Version]
- Adamus, J.; Lacki, P.; Motyka, M. Analysis of titanium sheet bending process. Inz. Mater. 2010, 31, 716–719. [Google Scholar]
- Aquilina, P.; Parr, W.C.; Chamoli, U.; Wroe, S. Finite element analysis of patient-specific condyle fracture plates: a preliminary study. Craniomaxillofac Trauma Reconstr. 2015, 8, 111–116. [Google Scholar] [CrossRef] [PubMed] [Green Version]
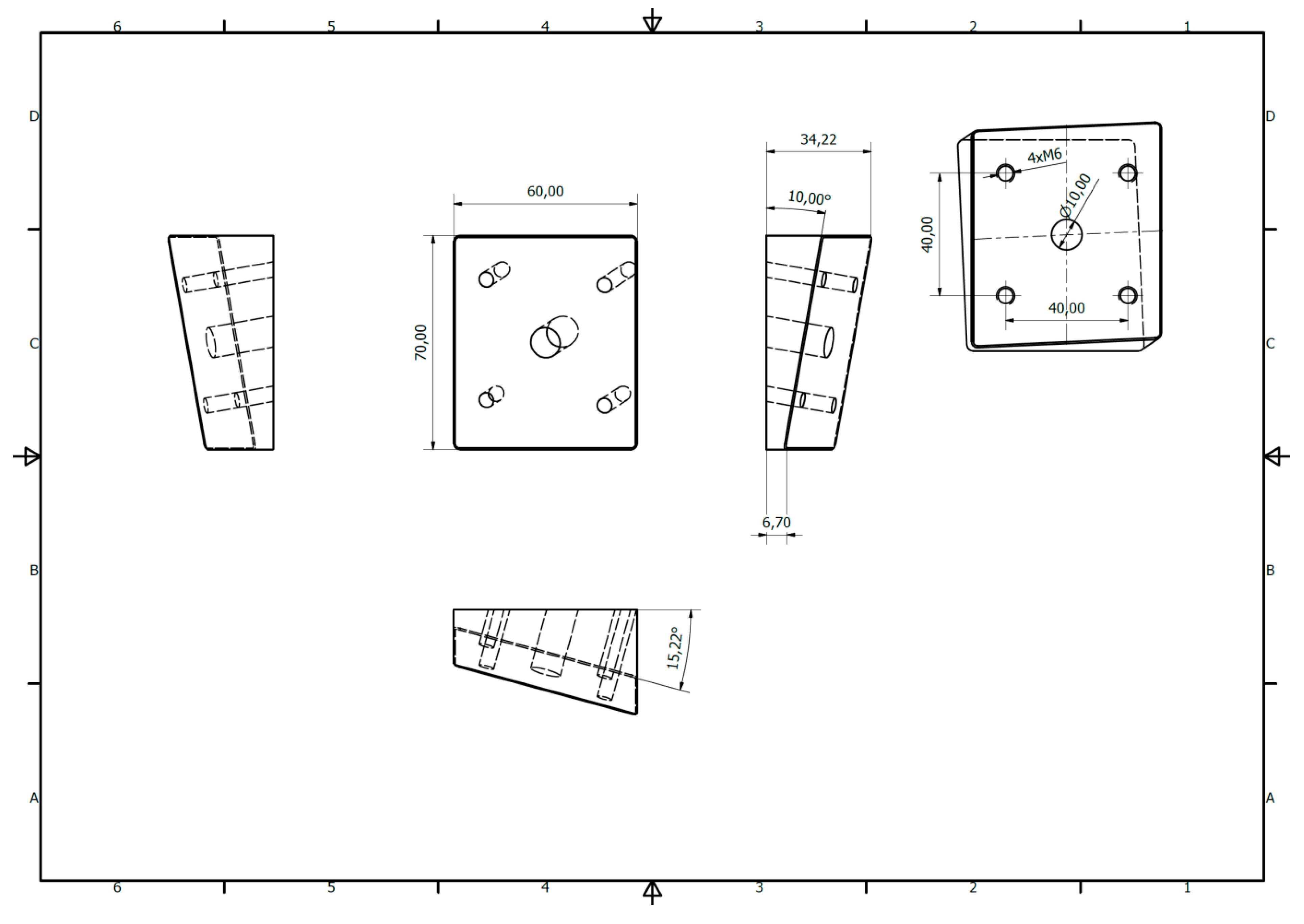
| Design Code | Manufacturer | Design | Height (mm) | Width (mm) |
|---|---|---|---|---|
| Plate11 | Synthes |  | 13,5 | 8 |
| Plate14 | Medartis |  | 15,3 | 8,8 |
| Plate02 | Medartis |  | 15,4 | 8,8 |
| Plate20 | any |  | 16,5 | 3,4 |
| Plates No | Broken | Endured | Row Total |
|---|---|---|---|
| Plate 11 | 0 | 7 | 7 |
| 0.00% | 25.00% | 25.00% | |
| Plate 14 | 0 | 7 | 7 |
| 0.00% | 25.00% | 25.00% | |
| Plate 2 | 0 | 7 | 7 |
| 0.00% | 25.00% | 25.00% | |
| Plate 20 | 7 | 0 | 7 |
| 25.00% | 0.00% | 25.00% | |
| Column Total | 7 | 21 | 28 |
| 25.00% | 75.00% | 100.00% |
| One-millimeter Displacement in Fracture Line | Height (mm) | Width (mm) | Plate Surface Area (mm2) | Plate Design Factor | F max/dL (N/mm) |
|---|---|---|---|---|---|
| Average±stand. dev. | 15.18±1.10 | 7.25±2.29 | 179.28±32.15 | 191.23±30.79 | 8.60±4.03 |
| Minimum | 13.5 | 3.4 | 138.13 | 151.05 | 2.57 |
| Maximum | 16.5 | 8.8 | 226.82 | 236.17 | 15.65 |
| Range | 3.0 | 5.4 | 88.69 | 85.13 | 13.08 |
| Stnd. skewness | −1.08 | −2.48 | 0.68 | 0.53 | 0.68 |
| Stnd. kurtosis | −0.97 | −0.68 | −1.02 | −1.03 | −1.30 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zieliński, R.; Kozakiewicz, M.; Konieczny, B.; Krasowski, M.; Okulski, J. Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible. Materials 2020, 13, 592. https://doi.org/10.3390/ma13030592
Zieliński R, Kozakiewicz M, Konieczny B, Krasowski M, Okulski J. Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible. Materials. 2020; 13(3):592. https://doi.org/10.3390/ma13030592
Chicago/Turabian StyleZieliński, Rafał, Marcin Kozakiewicz, Bartłomiej Konieczny, Michał Krasowski, and Jakub Okulski. 2020. "Mechanical Evaluation of Titanium Plates for Osteoesynthesis High Neck Condylar Fracture of Mandible" Materials 13, no. 3: 592. https://doi.org/10.3390/ma13030592






