Design and Fabrication of a Precision Template for Spine Surgery Using Selective Laser Melting (SLM)
Abstract
:1. Introduction
2. Customized Design of the Template in Spinal Surgery
2.1. Steps for Designing the Template
- The Biograph 64 PET/CT apparatus (SIEMENS, Munich, Germany) was used to obtain scan data, with a scan condition of 120 kv,150 mAs; scan slice thickness of 0.5 mm; and a scanning time of 10–15 s. The factor that affects the geometrical accuracy is the scan slice thickness, which would impact the surface fitting accuracy. The data from a thin-layer CT scan of the cervical vertebrae of the patient was imported into Mimics 16.0 (Materialise, Leuven, Belgium) to extract the target spine. Store this as STL (binary) to be imported into Geomagic software (3D syestems, Rock Hill, SC, USA). Elimination of the noise points inside the bone to obtain the 3D entity was accomplished by executing the following process: extract surface—construct patches—construct grids—surface fitting, and store it in the STEP AP203 format; import the data from Geomagic software into SolidWorks software; and integrate the separate 3D entity models into an assembled model to obtain the target spine model (as shown in Figure 1a).
- Step 2: Design of the contact surface of the template in the spinal surgeryIn the atlantoaxial fixation surgery, the curved surface is chosen to be at the arcus posterior of the cervical vertebra. A rectangle of appropriate size is clipped and then the curved surface is thickened outwardly (as shown in Figure 1b).
- Step 3: Choice of the locations of the guider hole and locating holeThe criterion for choosing the guider hole is to enable the nail to reach the lateral mass and to minimize the surface of the arcus posterior atlantis. The screws should be buried in the lateral mass to bypass important nerves and blood vessels. The locating hole should be placed at a distance of around 10 mm from the center of the template, with its direction normal to its curved surface (as shown in Figure 1c).
- Step 4: Design of the handleIn order to stabilize the surgical template while inserting the screws, a handle is placed in the middle of the template for the doctor to hold. The long column is clamped with the forefinger and the disk is pressed with the thumb. Edges and corners of the handle are chamfered to make the clamping comfortable. The final proposed design of the template is shown in Figure 1d.
2.2. Geometrical Parameters of the Surgical Template
- (a)
- The template’s thickness was designed to be 0.8–1.0 mm: (1) this value is assigned to guarantee the template’s strength and hardness, so as to resist deformation or fracture during the clinical operation; (2) the thinner the template is, the better the contact between the template and the bone surface should be. Based on above two reasons, the template’s thickness is designed to be 0.8–1 mm.
- (b)
- The guider hole diameter was designed to be 2.7 mm: this dimension is designed according to the screw’s size.
- (c)
- The guide’s wall thickness was designed to be 0.15 mm: as long as the strength is ok, the guider hole’s wall thickness should be as thin as possible
- (d)
- The guide’s length was designed to be 10 mm: as long as the screw placement is stable, the guide’s length should be as short as possible.
- (e)
- The locating hole size was designed to be 1.0 mm: this dimension is designed according to the screw’s size.
- (f)
- The locating holes’ distance to the center was designed to be 10 mm, (1) in order to secure the template to the bone surface through tiny screws during clinical operation; and (2) the locating holes should be placed as close to the guider holes as possible, so as to guarantee stability during the screw placement.
3. Experimental Techniques and Procedures
3.1. Equipment, Materials, and Optimization for the SLM Process
3.2. Design-Manufacturing Procedures of Template
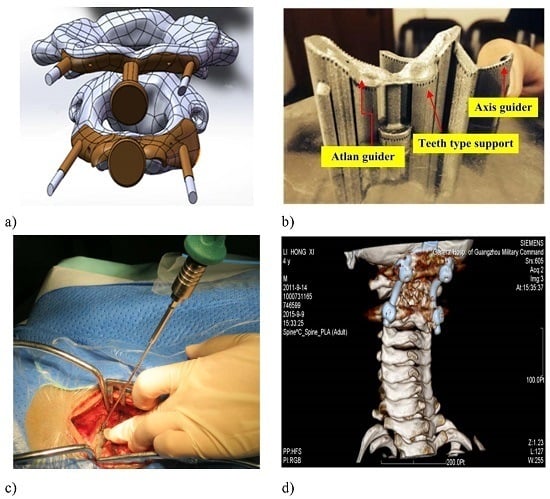
- A customized spinal surgery template was designed under the guidance of a surgeon (Hospital of Orthopedics, Guangzhou General Hospital of Guangzhou Military Command).
- The designed surgical template model was exported as a STL data file and was imported into Magics 16.0 to adjust the location of the model (Figure 5). The data on triangular slices was restored, the metal supports were added and the other necessary operations were carried out. The contact face between the template and the vertebra was placed upwards to ensure high surface quality.
- The slicing operations were carried out by setting the parameters for laser spot compensation and layer thickness in Magics 16.0 (Materialise, Leuven, Belgium), and then the data for laser scanning track control was generated.
- The processing data was input into the self-developed 3D metal printer, DiMetal-100, to build the template, and then the precision and mechanical properties of the fabricated surgical template were evaluated.
- Finally, the spinal surgery template was put into clinical use to evaluate its efficacy, and the key technologies for fabrication of the precision spinal surgery template were evaluated.
3.3. Testing Procedures
4. Results and Discussion
4.1. Results of SLM Manufacturing for the Spinal Surgery Template
4.2. Manufacturing Accuracy and Mechanical Property
4.2.1. Manufacturing Accuracy
4.2.2. Hardness and Mechanical Property Measurement
4.3. Clinical Test of the Customized Spinal Surgery Template
4.4. Discussion
- (1)
- A locating hole with a diameter of 2.3 mm was recommended for the template. It was set to 1 mm in the current study. A small size of the locating hole made it difficult for a naked eye to spot the hole. Adjusting the diameter of the locating hole according to industrial standards on the screws justified the use of standard screws.
- (2)
- The two key screw holes were required to enlarge their diameters to 3.0 mm. The diameters of these screw holes were set to 2.7 mm. The reason why the sizes of the parts were smaller than the design was that some powder particles remained adhered to the wall of the holes, due to laser radiation. Detailed analysis on the principles is given below.
- (3)
- The thickness of the walls of the screw holes was increased to 0.3 mm to prevent walls of the hole from breaking during the removal of the support by sand blasting. As discussed in Section 3.1, the strength of the hole could be guaranteed by setting the width of the melting track to 100–120 μm, scanning interval to 80 μm, wall thickness of the hole to 0.3 mm or the stacking thickness of about four melting tracks.
- (4)
- The curved surface in current experiment was so wide that the incision made in the surgery was very large, which caused more harm to the patient. Hence, for the design of the customized spinal surgery template, redundant parts should be removed. Taking the atlas template in Figure 12 as an example, the parts circled red in the designed model should be eliminated.
- The criterion for adding the support is to ensure that the support can be easily removed after the forming process and it remains stable and free from warpage. At the same time, heat conduction should be guaranteed during the forming process in order to reduce accumulation of thermal stress in the template. The added supports in the current investigation were very dense with high strength, which made it difficult to remove the supports, leaving the guider holes prone to fracture. The further optimization of the customized metal template should focus on the parameters pertaining to the teeth between the endpoints of the support and the template, including the gap between the teeth, penetration of teeth into the parts, and teeth width.
- The techniques for fabricating the screw holes should be improved. When the spatial locations of parts are adjusted in Magics 16.0, the locations of holes in the template should also change. Based on the way in which the holes incline, the 3D metal printed holes are categorized into three classes: round holes parallel to the fabricating direction, round holes vertical to the fabricating direction, and round holes making an angle with the X-Y plane. In what follows, limitations of principles for fabricating the first two classes of round holes will be discussed as depicted in Figure 13.
5. Conclusions
- A customized surgical template with tiny locating holes was successfully fabricated through computer-aided design and selective laser melting to assist the doctors in inserting high-precision screws into the spine. The design innovation in this study is that tiny locating screw holes were added on the template, the two locating holes are used for making the template contact the bone surface firmly by using two tiny screws, without needing to press the metal template by hand during clinical operation. The proposed metal template provided high navigation precision, was robust against damage, and could be easily autoclaved.
- To ensure accurate fabrication of the spinal surgery template, the contact face was placed upwards, which resulted in better surface quality of the contact face between the template and the spine. The roughness of the contact face was Ra = 13 ± 2 micrometers for the printed template and Ra = 7 ± 0.5 micrometers after abrasive blasting. The metal template was bound with the ABS model. The micro-hardness measured at the cross-sections of SLM-processed samples varied from HV0.3 250 to HV0.3 280, and the measured tensile strengths were in the range of 450–560 MPa.
- Improvements in the design of the template and 3D metal printing are required. For example, the wall thickness of the two guider holes in the axis guide should be increased to avoid fracturing. The size of the locating holes and guider holes should also be enlarged. Redundant parts of the model should be removed to prevent the excessively wide, curved surface from causing more pain to the patients.
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kabins, M.B.; Weinstein, J.N. The history of vertebral screw and pedicle screw fixation. Iowa Orthop. J. 1991, 11, 127–136. [Google Scholar]
- Manbachi, A.; Cobbold, R.S.; Ginsberg, H.J. Guiderd pedicle screw insertion: Techniques and training. Spine J. 2014, 14, 165–179. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Xu, Y.Q.; Cheng, Y.B.; Jiang, M.Y.; Xu, X.M.; Xie, L.; Lu, S. A novel computer-Assisted drill guider template for thoracic pedicle screw placement: A cadaveric study. Arch. Orthop. Trauma Surg. 2012, 132, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Eftekhar, B.; Ghodsi, M.; Ketabchi, E.; Rasaee, S. Surgical simulation software for insertion of pedicle screws. Neurosurgery 2002, 50, 222–224. [Google Scholar] [PubMed]
- Ryken, T.C.; Kim, J.; Owen, B.D.; Christensen, G.E.; Reinhardt, J.M. Engineering patient-specific drill templates and bioabsorbable posterior cervical plates: A feasibility study. J. Neurosurg. Spine 2009, 10, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Lund, T.; Laine, T.; Österman, H.; Yrjönen, T.; Schlenzka, D. Accuracy of computer assisted pedicle screw insertion: The evidence. J. Bone Jt. Surg. Br. 2012, 94-B, 32. [Google Scholar]
- Ryken, T.C.; Owen, B.D.; Christensen, G.E.; Reinhardt, J.M. Image-based drill templates for cervical pedicle screw placement. J. Neurosurg. Spine 2009, 10, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Melkent, T.; Foley, K.T.; Estes, B.T.; Chaudoin, J. Image Guided Spinal Surgery Guide, System, and Method for Use Thereof. U.S. Patent 6,348,058, 19 February 2002. [Google Scholar]
- Owen, B.D.; Christensen, G.E.; Reinhardt, J.M.; Ryken, T.C. Rapid prototype patient-specific drill template for cervical pedicle screw placement. Comput. Aided Surg. 2007, 12, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Xu, N.; Wei, F.; Liu, X.; Jiang, L.; Cai, H.; Li, Z.; Yu, M.; Wu, F.; Liu, Z. Reconstruction of the upper cervical spine using a personalized 3D-printed vertebral body in an adolescent with ewingsarcoma. Spine 2016, 41, E50–E54. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.; Lin, L.; Kong, X.; Zhao, W.; Tang, L.; Li, J.; Ouyang, J. Construction and accuracy assessment of patient-specific biocompatible drill template for cervical anterior transpedicular screw (ATPS) insertion: An in vitro study. PLoS ONE 2013, 8, e53580. [Google Scholar] [CrossRef] [PubMed]
- Goffin, J.; Van Brussel, K.; Martens, K.; Vander Sloten, J.; Van Audekercke, R.; Smet, M.H. Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1–C2. Spine 2001, 26, 1343–1347. [Google Scholar] [CrossRef] [PubMed]
- Kaneyama, S.; Sugawara, T.; Sumi, M.; Higashiyama, N.; Takabatake, M.; Mizoi, K. A novel screw guiding method with a screw guide template system for posterior C-2 fixation: Clinical article. J. Neurosurg. Spine 2014, 21, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Sarment D, P.; Sukovic, P.; Clinthorne, N. Accuracy of implant placement with a stereolithographic surgical guide. Int. J. Oral Maxillofac. Implant. 2003, 18, 571–577. [Google Scholar]
- Di Giacomo, G.A.; Cury, P.R.; de Araujo, N.S.; Sendyk, W.R.; Sendyk, C.L. Clinical application of stereolithographic surgical guides for implant placement: Preliminary results. J. Periodontol. 2005, 76, 503–507. [Google Scholar] [CrossRef] [PubMed]
- Bremen, S.; Meiners, W.; Diatlov, A. Selective laser melting. Laser Tech. J. 2012, 9, 33–38. [Google Scholar] [CrossRef]
- Leuders, S.; Thöne, M.; Riemer, A.; Niendorf, T.; Tröster, T.; Richard, H.A.; Maier, H.J. On the mechanical behaviour of titanium alloy TiAl6V4 manufactured by selective laser melting: Fatigue resistance and crack growth performance. Int. J. Fatigue 2013, 48, 300–307. [Google Scholar] [CrossRef]
- Hasan, R.; Mines, R.A.W. Variations in diameter of struts for micro-lattice structure manufactured using selective laser melting. In Proceedings of the Mechanical Engineering Research Day 2016, Centre for Advanced Research on Energy, Melaka, Malaysia, 31 March 2016; pp. 119–120.
- Wu, W.; Tor, S.B.; Chua, C.K.; Leonga, K.F.; Merchant, A. Investigation on processing of ASTM A131 Eh36 high tensile strength steel using selective laser melting. Virtual Phys. Prototyp. 2015, 10, 187–193. [Google Scholar] [CrossRef]
- Lam, L.P.; Zhang, D.Q.; Liu, Z.H.; Chua, C.K. Phase analysis and microstructure characterisation of AlSi10Mg parts produced by Selective Laser Melting. Virtual Phys. Prototyp. 2015, 10, 207–215. [Google Scholar] [CrossRef]
- Yadroitsev, I.; Yadroitsava, I. Evaluation of residual stress in stainless steel 316L and Ti6Al4V samples produced by selective laser melting. Virtual Phys. Prototyp. 2015, 10, 67–76. [Google Scholar] [CrossRef]
- Takemoto, M.; Fujibayashi, S.; Ota, E.; Otsuki, B.; Kimura, H.; Sakamoto, T.; Kawai, T.; Futami, T.; Sasaki, K.; Matsushita, T.; et al. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: Novel design with reduced contact area. Eur. Spine J. 2016, 25, 1698–1705. [Google Scholar] [CrossRef] [PubMed]
- Verweij, J.P.; Moin, D.A.; Mensink, G.; Nijkamp, P.; Wismeijer, D.; van Merkesteyn, J.P. Autotransplantation of Premolars With a 3-Dimensional Printed Titanium Replica of the Donor Tooth Functioning as a Surgical Guide: Proof of Concept. J. Oral Maxillofac. Surg. 2016, 74, 1114–1119. [Google Scholar] [CrossRef] [PubMed]
- Cornelius, C.P.; Smolka, W.; Giessler, G.A.; Wilde, F.; Probst, F.A. Patient-specific reconstruction plates are the missing link in computer-assisted mandibular reconstruction: A showcase for technical description. J. Maxillofac. Surg. 2015, 43, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Foroozmehr, A.; Badrossamay, M.; Foroozmehr, E. Finite element simulation of selective laser melting process considering optical penetration depth of laser in powder bed. Mater. Des. 2016, 89, 255–263. [Google Scholar] [CrossRef]
- Attar, H.; Prashanth, K.G.; Chaubey, A.K.; Calin, M.; Zhang, L.C.; Scudino, S.; Eckert, J. Comparison of wear properties of commercially pure titanium prepared by selective laser melting and casting processes. Mater. Lett. 2015, 142, 38–41. [Google Scholar] [CrossRef]
- Kasperovich, G.; Hausmann, J. Improvement of fatigue resistance and ductility of TiAl6V4 processed by selective laser melting. J. Mater. Process. Technol. 2015, 220, 202–214. [Google Scholar] [CrossRef]
- Salonitis, K. Design for additive manufacturing based on the axiomatic design method. Int. J. Adv. Manufac. Technol. 2016, 1–8. [Google Scholar] [CrossRef]
- Wang, D.; Yang, Y.Q.; Liu, R.C.; Xiao, D.M.; Sun, J.F. Study on the designing rules and processability of porous structure based on selective laser melting (SLM). J. Mater. Process. Technol. 2013, 213, 1734–1742. [Google Scholar] [CrossRef]
- Amirouche, F.; Solitro, G.F. Innovative Approach in the Development of Computer Assisted Algorithm for Spine Pedicle. Med. Eng. Phys. 2016, 38, 354–365. [Google Scholar]














| Guider Position | Thickness (mm) | Left Guider Hole | Right Guider Hole | Left Locating Hole | Right Locating Hole | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Inner Diameter(mm) | Wall Thickness(mm) | Length | Inner Diameter(mm) | Wall Thickness (mm) | Length(mm) | Inner Diameter(mm) | Distance to the Center (mm) | Inner Diameter (mm) | Distance to the Center (mm) | ||
| Atlas guider | 0.8 | 2.7 | 0.15 | 10.0 | 2.7 | 0.15 | 10.0 | 1.0 | 12.45 | 1.0 | 10.84 |
| Axis guider | 1.0 | 2.7 | 0.11 | 10.0 | 2.7 | 0.11 | 10.0 | 1.0 | 11.08 | 1.0 | 10.72 |
| Laser Power (W) | 120 |
|---|---|
| Scanning Speed (mm/s) | 600 |
| Scanning Space (µm) | 80 |
| Layer Thickness (µm) | 25 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, D.; Wang, Y.; Wang, J.; Song, C.; Yang, Y.; Zhang, Z.; Lin, H.; Zhen, Y.; Liao, S. Design and Fabrication of a Precision Template for Spine Surgery Using Selective Laser Melting (SLM). Materials 2016, 9, 608. https://doi.org/10.3390/ma9070608
Wang D, Wang Y, Wang J, Song C, Yang Y, Zhang Z, Lin H, Zhen Y, Liao S. Design and Fabrication of a Precision Template for Spine Surgery Using Selective Laser Melting (SLM). Materials. 2016; 9(7):608. https://doi.org/10.3390/ma9070608
Chicago/Turabian StyleWang, Di, Yimeng Wang, Jianhua Wang, Changhui Song, Yongqiang Yang, Zimian Zhang, Hui Lin, Yongqiang Zhen, and Suixiang Liao. 2016. "Design and Fabrication of a Precision Template for Spine Surgery Using Selective Laser Melting (SLM)" Materials 9, no. 7: 608. https://doi.org/10.3390/ma9070608