Social and Spatial Inequalities during COVID-19: Evidence from France and the Need for a New Sustainable Urban and Regional Development Paradigm
Abstract
:1. Introduction
- -
- What are the theoretical and operational implications of social and spatial inequality in cities and regions?
- -
- Is there a correlation between population density and the numbers of infections and deaths caused by COVID-19?
- -
- Is there a correlation between poverty and the numbers of infections and deaths caused by COVID-19?
- -
- How effective were the lockdown measures during the COVID-19 pandemic, and did they play a role in reducing the rates of infection and death?
- -
- What lessons can be learned from the French experience?
- -
- How can we reshape the future of cities, regions, and communities for the post-COVID-19 era?
1.1. The Theoretical Framework: Social and Spatial Inequality Discourse
1.2. The Operational Framework: Population Density, Poverty, and the Spread of COVID-19
1.3. The Empirical Framework: Spread of COVID-19 in French Regions
1.4. Population Density in French Regions
| Department | Density h/km2 | N° of Infections | N° of Deaths | Department | Density h/km2 | N° of Infections | N° of Deaths | Department | Density h/km2 | N° of Infections | N° of Deaths |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Val-d’Oise (95) | 1133 | 861 | 1996 | Bas-Rhin (67) | 207 | 262 | 1691 | Deux Sèvres (79) | 65 | 308 | 253 |
| Seine Saint- Denis (93) | 7822 | 825 | 2416 | Haute-Rhin (68) | 204 | 203 | 1503 | Hautes-Pyrénées (65) | 65 | 180 | 202 |
| Val-de-Marne (94) | 7103 | 749 | 2947 | Hérqult (34) | 197 | 381 | 968 | Tarne (81) | 64 | 360 | 372 |
| Seine et Marne (77) | 319 | 736 | 2003 | Gironde (33) | 195 | 275 | 1031 | Lot-et-Garanne (47) | 63 | 195 | 180 |
| Paris (75) | 21,000 | 631 | 4438 | Morbihan (56) | 172 | 221 | 417 | Loir-et-Cher (41) | 62 | 333 | 327 |
| Essonne (91) | 956 | 634 | 1840 | Moselle (57) | 167 | 292 | 2387 | Côte-d’Or (21) | 62 | 264 | 924 |
| Oise (60) | 129 | 615 | 1345 | Ile-et-Vilaine (35) | 164 | 300 | 697 | Haute-Vienne (87) | 60 | 297 | 323 |
| Yvelines (78) | 774 | 590 | 1805 | Savoie (73) | 159 | 363 | 693 | Landes (40) | 57 | 104 | 237 |
| Nord (59) | 475 | 489 | 3756 | Meurthe-et-Moselle (54) | 158 | 365 | 1200 | Orne (61) | 56 | 273 | 351 |
| Bouches-du-Rhône (13) | 376 | 581 | 3560 | Haute-Garonne (31) | 155 | 288 | 797 | Mayenne (53) | 55 | 228 | 272 |
| Aube (10) | 71 | 567 | 429 | Finistère (29) | 154 | 91 | 259 | Tarne et- Caronne (82) | 54 | 275 | 219 |
| Hauts de Seine (92) | 10,866 | 544 | 2688 | Calvados (14) | 147 | 273 | 588 | Jura (39) | 53 | 370 | 480 |
| Rhône (69) | 573 | 550 | 3119 | Pyrénées-Orientales (66) | 138 | 323 | 321 | Ardennes (08) | 52 | 360 | 369 |
| Pas-de-Calais (62) | 217 | 519 | 1918 | Maine-et-Loire (49) | 134 | 332 | 703 | Vosges (88) | 52 | 331 | 847 |
| Doubs (25) | 97 | 488 | 512 | Loiret (45) | 128 | 326 | 636 | Aude (11) | 52 | 263 | 361 |
| Aisne (02) | 66 | 480 | 1095 | Côtes-d’armor (22) | 119 | 207 | 244 | Yonne (89) | 49 | 324 | 566 |
| Vaucluse (84) | 149 | 479 | 883 | Indre-et-Loire (37) | 117 | 367 | 489 | Dordogne (24) | 48 | 332 | 218 |
| Somme (80) | 72 | 478 | 919 | Pay-du-Drôme (63) | 109 | 296 | 739 | Haute-Corse (2B) | 47 | 140 | 88 |
| Var (83) | 220 | 465 | 1460 | Pyrénées-Atlantiques (64) | 105 | 111 | 475 | Haute-Saône (70) | 45 | 229 | 265 |
| Loire (42) | 27 | 460 | 1332 | Eure-et-Loire (28) | 96 | 381 | 503 | Ariège (09) | 42 | 227 | 1332 |
| Alpes-de-Hautes de Provence (04) | 27 | 458 | 247 | Charente-Maritime (17) | 94 | 179 | 319 | Cher (18) | 40 | 318 | 504 |
| The Alpes Maritimes (06) | 402 | 440 | 1517 | Vendée (85) | 91 | 308 | 286 | Aveyron (12) | 40 | 309 | 228 |
| Nièvre (58) | 38 | 439 | 322 | Sarthe (72) | 88 | 378 | 588 | Corrèze (19) | 40 | 273 | 216 |
| Gard (30) | 114 | 436 | 634 | Manche (50) | 84 | 250 | 364 | Indre (36) | 36 | 207 | 261 |
| Hautes-Alpes (05) | 29 | 434 | 253 | Drôme (26) | 81 | 320 | 767 | Lot (46) | 35 | 170 | 98 |
| Eure (27) | 98 | 426 | 479 | Ardèche (07) | 78 | 210 | 494 | Corse-du-Sud (2A) | 29 | 181 | 117 |
| Seine Maritime (76) | 191 | 422 | 1507 | Charente (16) | 70 | 233 | 159 | Creuse (23) | 28 | 71 | 97 |
| Isère (38) | 224 | 411 | 1746 | Saône-et-Loire (71) | 69 | 280 | 1097 | Meuse (55) | 27 | 365 | 380 |
| Ain (01) | 145 | 402 | 616 | Vienne (86) | 69 | 271 | 267 | Cantal (15) | 25 | 186 | 133 |
| Loire-Atlantique (44) | 202 | 277 | 827 | Marne (51) | 68 | 380 | 895 | Haut-Marne (52) | 25 | 365 | 366 |
| Haute-Savoie (74) | 258 | 258 | 1007 | Allier (03) | 68 | 267 | 580 | Gers (32) | 25 | 185 | 98 |
| Territoire de belfort (90) | 213 | 333 | 590 | Haute-Loire (43) | 66 | 345 | 251 | Gozère (48) | 19 | 273 | 118 |

1.5. Poverty, Social Inequalities, and Spatial Disparities in France
2. Methods and Materials
2.1. Methodologies
2.2. Data for COVID-19 Infections and Deaths
2.3. Population Density and Poverty Rates
2.4. Data Analysis and Variables
3. Results
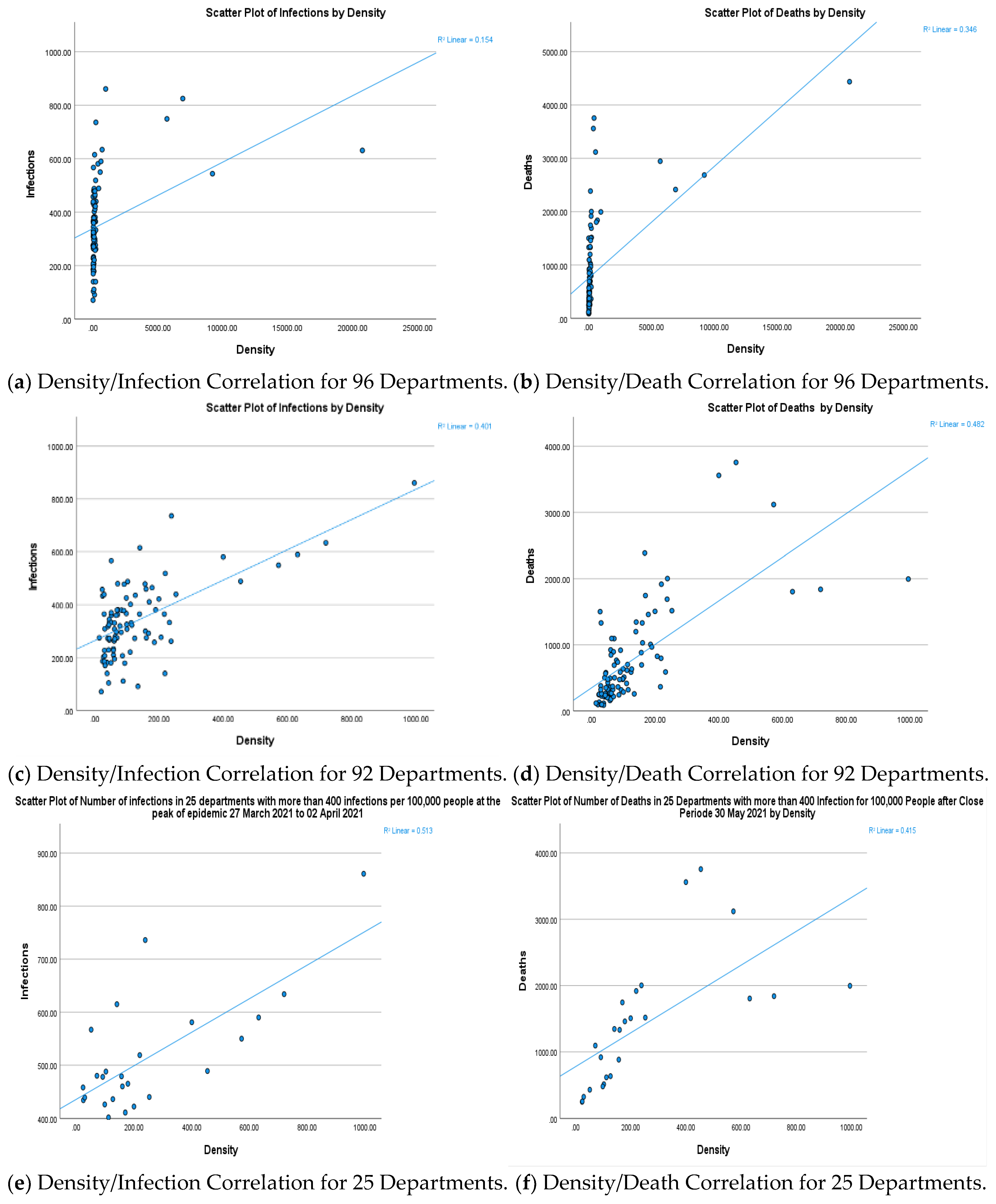
3.1. Population Density and Infection/Death Correlation in 96 French Departments
- The Paris department (75) recorded the highest density in France at 21,000 inhabitants per square kilometer, where infections in the third wave reached 631 per 100,000 inhabitants, with deaths totaling 4438 by the end of the wave.
- Seine-Saint-Denis (93) noted France’s highest infection rate at 825 per 100,000 inhabitants and 2416 deaths per 100,000, with a density of 7822 inhabitants per square kilometer.
- Val-de-Marne (94), ranking third, reported 749 infections per 100,000 inhabitants, and 2947 deaths, despite having the lowest density in the Île-de-France region at 7103 inhabitants per square kilometer.
- Hauts de Seine (92), with the second highest density in France after Paris at 10,866 inhabitants per square kilometer, recorded the lowest infection number per 100,000 inhabitants in the Île-de-France region at 544, alongside 2688 deaths.
- Bordering departments such as Nord (59), second only to Paris (75) in death numbers at 3756, followed by Bouches-du-Rhône (13) with 3560 deaths, show contrasting data given their densities of 475 for the first, and 376 inhabitants per square kilometer for the second. Even the number of infections per 100,000 inhabitants was lower than Paris, 489 for Nord (59), and 581 for Boches-du-Rhône (13).
3.2. Population Density and Infection/Death Correlation in 92 French Departments
3.3. Population Density and Infection/Death Correlation in 25 French Departments
3.4. Poverty and Infection/Death Correlation in French Departments
3.5. Evidence of Spatial and Social Inequality in French Departments
- (a)
- The first group with low density demonstrates that some areas, despite having low density, reported high infection rates (over 400 infections per 100,000 inhabitants with more than 1000 deaths) but also recorded high poverty levels. For example, in the Aisne (02) department, 18.5% of the population lives below the national poverty line set at 14.6%. Similar results were observed in Pas-de-Calais (62), where the poverty rate reaches 19.30%, despite relatively low density (72 inhabitants per square kilometer for the first and 217 for the second). A comparable situation exists in the Var (83) department, where 18.3% are below the poverty line, and the death count is relatively high at 1332, despite a low density of about 220 inhabitants per square kilometer.
- (b)
- The second group with low poverty rates highlights some dense departments, like Hauts de Seine (92) in Île-de-France. Here, poverty stands at 11.80%, below the national average, while the density is high at 10,866 inhabitants per square kilometer. The department recorded 2688 deaths, despite a high infection rate of 544 cases per 100,000 inhabitants. However, the number of deaths were relatively high in relation to the infections rate.
- (c)
- The third group, combining high population density and high poverty percentage, illustrates extreme cases, as seen in Seine-Saint-Denis (93). Here, the density is 7822 inhabitants per square kilometer, and 27.90% of the population is under the poverty line, nearly double the national average. In this department, north of Paris, some of the highest infection rates were recorded at 825 cases per 100,000 inhabitants, along with 2416 deaths.
3.6. Impact of Lockdown Policies on Infection/Death Correlation in 29 Departments
4. Discussion
4.1. Prioritizing Social and Spatial Inequality
4.2. Population Density and Sustainability Challenges
4.3. Department Size and Accessibility to Health Services: A Policy Dilemma and the Need for a New Social Contract
4.4. Correlation between Poverty, Infections, and Deaths: Limitation of Statistical Results
4.5. Successful Lockdowns Mitigate COVID-19 Transmission
4.6. Towards a New Urban and Regional Paradigm
- (a)
- Inclusive Cities
- (b)
- Green Cities
- (c)
- Smart Cities
- (d)
- Good Governance
- (e)
- Financial Resources
- -
- (S1) Effective scale and policy action based on: (1) Empower cities of all sizes to contribute to prosperity and well-being. (2) Customize policies to local living and working environments. (3) Promote urban–rural collaboration and support.
- -
- (S2) Integrated strategy for inclusive, smart, and green cities: (4) Set forward-looking national urban policies for upcoming challenges. (5) Utilize the urban potential of cities of all sizes to enhance environmental sustainability and transition to a low carbon and greener economy. (6) Create inclusive cities of all sizes with opportunities for everyone. (7) Implement an integrated urban policy framework to coordinate sectoral policies for holistic development. (8) Ensure ample funding for urban policy execution at all government levels.
- -
- (S3) Stakeholder Engagement: (9) Involve stakeholders in urban policy design and implementation. (10) Boost the innovation and efficiency of urban actors. (11) Maintain continuous urban policy evaluation and governance accountability.
5. Conclusions
6. Study Limitations
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Novel Coronavirus (2019-nCoV): Situation Report, 11; WHO: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/bitstream/handle/10665/330776/nCoVsitrep31Jan2020-eng.pdf (accessed on 8 March 2022).
- WHO. Coronavirus Disease COVID-19 Dashboard. 19 November 2020. Available online: https://covid19.who.int/?gclid=EAIaIQobChMIjfDYqqfE7gIV82DmCh2R4QWrEAAYASAAEgLCNPD_BwE (accessed on 20 November 2021).
- World Health Organization. Coronavirus Disease COVID-19 Dashboard. 28 September 2021. Available online: https://covid19.who.int/ (accessed on 28 September 2001).
- World Health Organization. Coronavirus Disease COVID-19 Dashboard. 2022. Available online: https://covid19.who.int/region/wpro/country/cn (accessed on 2 September 2022).
- World Health Organization. Data.who.int, WHO Coronavirus (COVID-19) Dashboard > Cases [Dashboard]. 2024. Available online: https://data.who.int/dashboards/covid19/cases (accessed on 14 January 2024).
- UN-HABITAT. COVID-19, Key Facts, and Data. 5 March 2021. Available online: https://unhabitat.org/covid-19/key-facts-and-data (accessed on 20 March 2021).
- Cascella, M.; Rajnik, M.; Aleem, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation, and Treatment of Coronavirus (COVID-19); StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554776 (accessed on 14 October 2023).
- Hamidi, S.; Sabouri, S.; Ewing, R. Does Density Aggravate the COVID-19 Pandemic? J. Am. Plan. Assoc. 2020, 86, 495–509. [Google Scholar] [CrossRef]
- Sassen, S.; Kourtit, K. A Post-Corona Perspective for Smart Cities: ‘Should I Stay, or Should I Go?’. Sustainability 2021, 13, 9988. [Google Scholar] [CrossRef]
- UN. Transforming Our World: The 2030 Agenda for Sustainable Development; Resolution Adopted by the General Assembly on 25 September 2015; United Nations: New York, NY, USA, 2015; Volume 42809, pp. 1–13. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed on 20 March 2024).
- OECD. OECD Regional Outlook 2021: Addressing COVID-19 and Moving to Net Zero Greenhouse Gas Emissions; OCDE: Paris, France, 2021. [Google Scholar] [CrossRef]
- UNDP. Human Development Report 2021/2022. Uncertain Times, Unsettled Lives: Shaping our Future in a Transforming World; United Nations Development Programme: New York, NY, USA, 2022; Available online: https://hdr.undp.org/system/files/documents/global-report-document/hdr2021-22pdf_1.pdf (accessed on 22 April 2022).
- UN-HABITAT. Spatial Planning Guidelines during COVID-19. September 2020. Available online: https://unhabitat.org/sites/default/files/2020/11/covid19_spatialplanning_eng1.pdf (accessed on 20 March 2021).
- UN-HABITAT. Report Calls for Cities Post-Pandemic to Lead the Way to a Fairer, Greener, Healthier Future. UN News. United Nations. 30 March 2021. Available online: https://news.un.org/en/story/2021/03/1088622 (accessed on 18 February 2023).
- Jillian, D.; Robert, K.; Radha, C. Tackling Inequality in Cities is Essential for Fighting COVID-19, 14 April 2020. Available online: https://www.wri.org/blog/2020/04/coronavirus-inequality-cities (accessed on 21 July 2021).
- Sharifi, A.; Khavarian-Garmsir, A.R. The COVID-19 pandemic: Impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020, 749, 142391. [Google Scholar] [CrossRef]
- Bilal, U.; Tabb, L.P.; Barber, S.; Diez Roux, A.V. Spatial Inequities in COVID-19 Testing, Positivity, Confirmed Cases, and Mortality in 3 U.S. Cities: An Ecological Study. Ann. Intern. Med. 2021, 174, 936–944. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef]
- Bajos, N.; Counil, E.; Franck, J.E.; Jusot, F.; Pailhé, A.; Spire., A.; Martin, C.; Lydie, N.; Slama, R.; Meyer, L.; et al. Social inequalities and dynamics of the early COVID-19 epidemic: A prospective cohort study in France. BMJ Open 2021, 11, e052888. [Google Scholar] [CrossRef] [PubMed]
- Gaudart, J.; Landier, J.; Huiart, L.; Legendre, E.; Lehot, L.; Bendiane, M.K.; Chiche, L.; Petitjean, A.; Mosnier, E.; Kirakoya-Samadoulougou, F.; et al. Factors associated with the spatial heterogeneity of the first wave of COVID-19 in France: A nationwide geo-epidemiological study. Lancet Public Health 2021, 6, e222–e231. [Google Scholar] [CrossRef]
- Wolf, M. Rethinking Urban Epidemiology: Natures, Networks and Materialities. Int. J. Urban Reg. Res. 2016, 40, 958–982. [Google Scholar] [CrossRef] [PubMed]
- Shirazi, M.R.; Keivani, R. Social sustainability discourse. In Urban Social Sustainability; Routledge: London, UK, 2019; pp. 1–26. [Google Scholar] [CrossRef]
- Harvey, D. Front Matter. In Social Justice and the City (REV-Revised); University of Georgia Press: Athens, GA, USA, 1973; pp. 1–4. Available online: http://www.jstor.org/stable/j.ctt46nm9v.1 (accessed on 10 March 2024).
- Leven, C. Towards a Theory of the City. In Urban Development Models; Special Report 97; Hemmens, G., Ed.; National Academy of Sciences, Highway Research Board: Washington, DC, USA, 1978. [Google Scholar]
- Magis, K.; Shinn, C. Emergent Principles of Social Sustainability; Dillard, J.F., Dujon, V., Magisy, M.C.K., Eds.; Routledge: London, UK, 2009; Volume 40, pp. 629–648. [Google Scholar]
- Yiftachel, O.; Hedgcock, D. Urban social sustainability: The planning of an Australian city. Cities 1993, 10, 139–157. [Google Scholar] [CrossRef]
- Kay, A. Territorial justice and devolution. Br. J. Politics Int. Relat. 2005, 7, 544–560. [Google Scholar] [CrossRef]
- Piketty, T. Capital in the Twenty-First Century; Harvard University Press: Cambridge, MA, USA; London, UK, 2014. [Google Scholar] [CrossRef]
- Vallance, S.; Perkins, H.C.; Dixon, J.E. What is social sustainability? A clarification of concepts. Geoforum 2011, 42, 342–348. [Google Scholar] [CrossRef]
- Bramley, G.; Dempsey, N.; Power, S.; Brown, C.; Watkins, D. Social Sustainability and Urban Form: Evidence from Five British Cities. Environ. Plan. A Econ. Space 2009, 41, 2125–2142. [Google Scholar] [CrossRef]
- Bramley, G.; Brown, C.; Dempsey, N.; Power, S.; Watkins, D. Social Acceptability. In Dimensions of the Sustainable City; Future City; Jenks, M., Jones, C., Eds.; Springer: Dordrecht, The Netherlands, 2010; Volume 2. [Google Scholar] [CrossRef]
- Dave, S. High Urban Densities in Developing Countries: A Sustainable Solution? Built Environ. 2010, 36, 9–27. Available online: http://www.jstor.org/stable/23289981 (accessed on 10 March 2024). [CrossRef]
- Dave, S. Neighbourhood density and social sustainability in cities of developing countries. Sustain. Dev. 2011, 19, 189–205. [Google Scholar] [CrossRef]
- Kyttä, M.; Broberg, A.; Haybatollahi, M.; Schmidt-Thomé, K. Urban happiness: Context-sensitive study of the social sustainability of urban settings. Environ. Plan. B Plan. Des. 2016, 43, 34–57. [Google Scholar] [CrossRef]
- Shirazi, M.R.; Keivani, R. The triad of social sustainability: Defining and measuring social sustainability of urban neighbourhoods. Urban Res. Pract. 2019, 12, 448–471. [Google Scholar] [CrossRef]
- Shields, R. Spatial stress and resistance: Social meanings of spatialization. In Space and Social Theory: Interpreting Modernity and Postmodernity; Benko, G., Strohmayer, U., Eds.; Blackwell: Oxford, UK, 1997; pp. 33–186. [Google Scholar]
- Shirazi, M.R.; Keivani, R. (Eds.) Urban Social Sustainability: Theory, Policy and Practice, 1st ed.; Routledge: London, UK, 2019. [Google Scholar] [CrossRef]
- McFarlane, C. The geographies of urban density: Topology, politics and the city. Prog. Hum. Geogr. 2016, 40, 629–648. [Google Scholar] [CrossRef]
- Ali, S.H.; Keil, R. Contagious Cities. Geogr. Compass 2007, 1, 1207–1226. [Google Scholar] [CrossRef]
- Kendall, C.; Hudelson, P.; Leontsini, E.; Winch, P.; Lloyd, L.; Cruz, F. Urbanization, Dengue, and the Health Transition: Anthropological Contributions to International Health. Med. Anthropol. Q. 2009, 5, 257–268. [Google Scholar] [CrossRef]
- Andrew, M. Human Culture, Ecological Change, and Infectious Disease: Are We Experiencing History’s Fourth Great Transition? Ecosyst. Health 2001, 7, 107–115. [Google Scholar] [CrossRef]
- United Nations. Policy Brief: COVID-19 in an Urban World; United Nations: New York, NY, USA, 2020; Available online: https://unsdg.un.org/resources/policy-brief-covid-19-urban-world (accessed on 15 July 2021).
- Kadi, N.; Khelfaoui, M. Population Density, a Factor in the Spread of COVID-19 in Algeria: Statistic Study—Bulletin of the National Research Centre; Springer Open: London, UK, 2020; Available online: https://BNRC.springeropen.com/articles/10.1186/s42269-020-00393-x (accessed on 23 August 2022).
- Wong, D.W.; Li, Y. Spreading of COVID-19: Density matters. PLoS ONE 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, A.; Mukherjee, A.; Sarkar, K. Impact of population density on Covid-19 infected and mortality rate in India. Model Earth Syst. Environ. 2021, 7, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Fang, W.; Wahba, S. Urban Density Is Not an Enemy in the Coronavirus Fight: Evidence from China. World Bank Sustainable Cities Blog, 20 April 2020. Available online: https://blogs.worldbank.org/sustainablecities/urban-density-not-enemy-coronavirus-fight-evidence-china (accessed on 20 November 2021).
- Hamidi, S.; Ewing, R.; Sabouri, S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: Early evidence from 1,165 metropolitan counties in the United States. Health Place 2020, 64, 102378. [Google Scholar] [CrossRef] [PubMed]
- Carozzi, F.; Provenzano, S.; Sefi, R. Urban Density and COVID-19; CEP Discussion Papers (1711); Centre for Economic Performance; LSE: London, UK, 2020. [Google Scholar]
- Henao-Cespedes, V.; Garcés-Gómez, Y.A.; Ruggeri, S.; Henao-Cespedes, T.M. Relationship analysis between the spread of COVID-19 and the multidimensional poverty index in the city of Manizales, Colombia. Egypt. J. Remote Sens. Space Sci. 2022, 25, 197–204. [Google Scholar] [CrossRef]
- WHO. Coronavirus Disease COVID-19 Dashboard. 2023. Available online: https://data.who.int/dashboards/covid19/cases?m49=250&n=c (accessed on 6 September 2023).
- Reuters. 4 October 2022. France’s 8th Wave of COVID is Gaining in Intensity, Health Official Says. 21 June 2023. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/frances-8th-wave-covid-is-gaining-intensity-health-official-2022-10-04/ (accessed on 21 June 2023).
- Santé Publique France. Coronavirus-covid-19. 5 March 2021. Available online: https://www.santepubliquefrance.fr/dossiers/coronavirus-covid-19/coronavirus-chiffres-cles-et-evolution-de-la-covid-19-en-france-et-dans-le-monde#block-266151 (accessed on 5 March 2020).
- Pasteur Institut. Une Modélisation Indique Qu’entre 5 et 7% des Français ont été infectés. 21 April 2020. Available online: https://www.pasteur.fr/fr/espace-presse/documents-presse/modelisation-indique-qu-entre-3-7-francais-ont-ete-infectes (accessed on 22 February 2021).
- Santé Publique France. GEODES. 22 March 2021. Available online: https://geodes.santepubliquefrance.fr/#c=home (accessed on 22 March 2021).
- World Bank. Data Bank, Metadata Glossary. 2023. Available online: https://databank.worldbank.org/metadataglossary/jobs/series/EN.POP.DNST (accessed on 31 January 2024).
- INSEE. Demographic Report 2023. 23 November 2024. Available online: https://www.insee.fr/en/statistiques/7757334 (accessed on 21 January 2024).
- INSEE. France, Portrait Social. 16 January 2023. Available online: https://www.insee.fr/fr/statistiques/7666835?sommaire=7666953&q=densite+departement (accessed on 21 January 2024).
- Romanova, E. Increase in population density and aggravation of social and psychological problems in areas with high-rise construction. E3S Web Conf. 2018, 33, 03061. [Google Scholar] [CrossRef]
- Santé Publique France. GEODES. 30 May 2021. Available online: https://geodes.santepubliquefrance.fr/#bbox=-1878154,6775601,4220720,1847697&c=indicator&f=0&i=covid_hospit.dc&s=2021-05-30&t=a01&view=map2 (accessed on 3 June 2021).
- INSEE. Définitions, Méthodes et Qualité, Départment. 27 March 2018. Available online: https://www.insee.fr/fr/metadonnees/definition/c1762 (accessed on 10 July 2021).
- INSEE. France, Portrait Social-Pauvreté. 3 December 2020. Available online: https://www.insee.fr/fr/statistiques/4797606?sommaire=4928952 (accessed on 30 April 2021).
- INSEE. Tableaux de L’Économie Française. 27 July 2020. Available online: https://www.insee.fr/fr/statistiques/4277596?sommaire=4318291 (accessed on 10 July 2021).
- INSEE. Tableaux de L’Économie Française-Régions—Départements Population. 27 February 2018. Available online: https://www.insee.fr/fr/statistiques/3303305?sommaire=3353488 (accessed on 30 May 2021).
- Siddique, A.B.; Haynes, K.E.; Kulkarni, R.; Li, M. Regional poverty, and infection disease: Early exploratory evidence from the COVID-19 pandemic. Ann. Reg. Sci. 2023, 70, 209–236. [Google Scholar] [CrossRef] [PubMed]
- Brunner, A. Rapport sur Les Inégalités, 2023 ed. Observatoire Des Inégalités. 12 June 2023. Available online: https://www.inegalites.fr/Rapport-sur-les-inegalites-edition-2023 (accessed on 10 September 2023).
- France Stratégie. 2017/2027 Voir plus Loin, Voir plus Clair. Présentation de la démarche. France Stratégie. 2016. Available online: http://francestrategie1727.fr/wp-content/uploads/2016/02/17-27-dexxmarche-29.02-1.pdf (accessed on 7 January 2024).
- Altakarli, N. China’s Response to the COVID-19 Outbreak: A Model for Epidemic Preparedness and Management. Dubai Med. J. 2020, 3, 44–49. [Google Scholar] [CrossRef]
- Lehman, A. JMP for Basic Univariate and Multivariate Statistics: A Step-by-Step Guide; Sas Press: Stockholm, Sweden, 2005. [Google Scholar]
- SENAT. Un Nouveau Pacte de Solidarité Pour les Quartiers, Annexe 8-La Seine-Saint-Denis: Un département Contrasté. 2021. Available online: https://www.senat.fr/rap/r06-049-1/r06-049-166.html (accessed on 11 June 2021).
- Boterman, W. Population density and SARS-CoV-2 pandemic: Comparing the geography of different waves in the Netherlands. Urban Stud. 2023, 60, 1377–1402. [Google Scholar] [CrossRef] [PubMed]
- Aw, S.B.; Teh, B.T.; Ling, G.H.T.; Leng, P.C.; Chan, W.H.; Ahmad, M.H. The COVID-19 Pandemic Situation in Malaysia: Lessons Learned from the Perspective of Population Density. Int. J. Environ. Res. Public Health 2021, 18, 6566. [Google Scholar] [CrossRef]
- Wang, J.; Yang, Y.; Peng, J.; Yang, L.; Gou, Z.; Lu, Y. Moderation effect of urban density on changes in physical activity during the coronavirus disease 2019 pandemic. Sustain. Cities Soc. 2021, 72, 103058. [Google Scholar] [CrossRef]
- Marí-Dell’Olmo, M.; Gotsens, M.; Pasarín, M.I.; Rodríguez-Sanz, M.; Artazcoz, L.; Garcia de Olalla, P.; Rius, C.; Borrell, C. Socioeconomic inequalities in COVID-19 in a European urban area: Two waves, two patterns. Int. J. Environ. Res. Public Health 2021, 18, 1256. [Google Scholar] [CrossRef]
- Sauze, L.; Chanut, F.E.E.C. Assurance Maladie: Un Futur à (Re)construire; Après-Demain: Lausanne, Switzerland, 2009; Volume 12, pp. 20–23. ISSN 0003-7176. [Google Scholar] [CrossRef]
- Aubry, A. Déserts Médicaux. Pourquoi Manque-t-on Tant de Médecins en France ? La Vie. 19 octobre 2022. Available online: https://www.lavie.fr/actualite/societe/pourquoi-manque-t-on-tant-de-medecins-en-france-84789.php (accessed on 20 March 2024).
- Figaro, L. Coronavirus: Le Déficit de la Sécu Plonge à 41 Milliards d’euros [Archive]. 22 April 2020. Available online: https://www.lefigaro.fr/economie/coronavirus-le-deficit-de-la-secu-plonge-a-41-milliards-d-euros-20200422 (accessed on 11 June 2021).
- Sik, D. Towards a post-pandemic social contract. Thesis Elev. 2023, 174, 62–80. [Google Scholar] [CrossRef]
- Alexander, A.; Morita, J.; Ridell, N.G.; Hoek, T.V.L. Social Contracts, and the Problem of Asymmetries. In Remaking the Urban Social Contract: Health, Energy, and the Environment; Pagano, M.A., Ed.; University of Illinois Press: Champaign, IL, USA, 2016; pp. 114–120. Available online: http://www.jstor.org/stable/10.5406/j.ctt1hfr0bc.10 (accessed on 11 June 2021).
- Brandily, P.; Brebion, C.; Briole, S.; Khoury, L. A Poorly Understood Disease? The Unequal Distribution of Excess Mortality Due to COVID-19 Across French Municipalities; SSRN Scholarly Paper ID 3682513; Social Sciences Research Network: Rochester, NY, USA, 2020. [Google Scholar] [CrossRef]
- Khafaie, M.A.; Rahim, F. Cross-Country Comparison of Case Fatality Rates of COVID-19/SARS-COV-2. Osong Public Health Res. Perspect. 2020, 11, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Feldman, J.M.; Bassett, M. The Relationship between Neighborhood Poverty and COVID-19 Mortality within Racial/Ethnic Groups (Cook County, Illinois). MedRxiv 2020, 15. [Google Scholar] [CrossRef]
- Alirol, E.; Getaz, L.; Stoll, B.; Chappuis, F.; Loutan, L. Urbanisation and infectious diseases in a globalised world. Lancet Infect. Dis. 2011, 11, 131–141. [Google Scholar] [CrossRef]
- Butler, J.C.; Crengle, S.; Cheek, J.E.; Leach, A.J.; Lennon, D.; O’Brien, K.L.; Santosham, M. Emerging infectious diseases among indigenous peoples. Emerg. Infect. Dis. 2001, 7 (Suppl. S3), 554–555. [Google Scholar] [CrossRef] [PubMed]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, eabg5298. [Google Scholar] [CrossRef]
- Cattell, V. Poor people, poor places, and poor health: The mediating role of social networks and social capital. Soc. Sci. Med. 2001, 52, 1501–1516. [Google Scholar] [CrossRef]
- Kapitsinis, N. The underlying factors of the COVID-19 spatially uneven spread. Initial evidence from regions in nine EU countries. Reg. Sci. Policy Pract. 2020, 12, 1027–1045. [Google Scholar] [CrossRef]
- Salje, H.; Tran Kiem, C.; Lefrancq, N.; Courtejoie, N.; Bosetti, P.; Paireau, J.; Andronico, A.; Hozé, N.; Richet, J.; Dubost, C.L.; et al. Estimating the burden of SARS-CoV-2 in France. Science 2020, 369, 208–211. [Google Scholar] [CrossRef]
- Di Domenico, L.; Pullano, G.; Sabbatini, C.E.; Boëlle, P.Y.; Colizza, V. Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Med. 2020, 18, 240. [Google Scholar] [CrossRef] [PubMed]
- Islam, N.; Sharp, S.J.; Chowell, G.; Shabnam, S.; Kawachi, I.; Lacey, B.; Massaro, J.M.; D’Agostino Sr, R.B.; White, M. Physical distancing interventions and incidence of coronavirus disease 2019: Natural experiment in 149 countries. BMJ 2020, 370, m2743. [Google Scholar] [CrossRef] [PubMed]
- Bouchet, C.; Duvoux, N. Post-COVID-19 poverty in France: Magnitude, manifestations, and actors from nine case studies. Int. J. Sociol. Soc. Policy 2023, 43, 823–837. [Google Scholar] [CrossRef]
- OECD. Cities policy responses (updated May 2020). 2020. Available online: https://www.oecd.org/coronavirus/policy-responses/cities-policy-responses-fd1053ff/ (accessed on 5 April 2024).
- OECD. Implementation toolkit of the OECD Principles on urban policy. In OECD Regional Development Papers, 31st ed.; OCDE: Paris, France, 2022. [Google Scholar] [CrossRef]
- Stratigea, A. The Concept of ‘Smart Cities. Towards Community Development? Netcom. 2012, 26, pp. 375–388. [CrossRef]
- Duan, Z.; Kim, S. Progress in Research on Net-Zero-Carbon Cities: A Literature Review and Knowledge Framework. Energies 2023, 16, 6279. [Google Scholar] [CrossRef]
- Seto, K.C.; Churkina, G.; Hsu, A.; Keller, M.; Newman PW, G.; Qin, B.; Ramaswami, A. From Low- to Net-Zero Carbon Cities: The Next Global Agenda. Annu. Rev. Environ. Resour. 2021, 46, 377–415. [Google Scholar] [CrossRef]
- World Economic Forum. The Global Risks Report 2024. Switzerland. 2024. Available online: https://www3.weforum.org/docs/WEF_The_Global_Risks_Report_2024.pdf (accessed on 6 April 2024).
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W.; et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020, 257–261. [Google Scholar] [CrossRef]
- World Economic Forum. Why We Need a New Social Contract for the 21st Century. Davos Agenda. 2022. Available online: https://www.weforum.org/agenda/2022/01/a-new-social-contract-for-21st-century/ (accessed on 5 April 2024).



| The Results for 96 Departments | |||||
|---|---|---|---|---|---|
| Density | Poverty | Infections * | Death * | ||
| Density | Pearson correlation | 1 | 0.137 | 0.393 ** | 0.589 ** |
| Sig. (2-tailed) | 0.183 | <0.001 | <0.001 | ||
| Poverty | Pearson correlation | 0.137 | 1 | 0.267 ** | 0.197 |
| Sig. (2-tailed) | 0.183 | 0.108 | 0.055 | ||
| Infections * | Pearson correlation | 0.393 ** | 0.267 ** | 1 | 0.654 ** |
| Sig. (2-tailed) | <0.001 | 0.009 | <0.001 | ||
| Deaths * | Pearson correlation | 0.589 ** | 0.197 | 0.654 ** | 1 |
| Sig. (2-tailed) | <0.001 | 0.055 | <0.001 | ||
| The Results for 92 Departments | |||||
| Density | Pearson correlation | 1 | 0.030 | 0.633 ** | 0.695 ** |
| Sig. (2-tailed) | 0.779 | <0.001 | <0.001 | ||
| Poverty | Pearson correlation | 0.030 | 1 | 0.135 | 0.136 |
| Sig. (2-tailed) | 0.779 | 0.198 | 00.197 | ||
| Infections * | Pearson correlation | 0.633 ** | 0.135 | 1 | 0.579 ** |
| Sig. (2-tailed) | <0.001 | 0.198 | <.001 | ||
| Deaths * | Pearson correlation | 0.695 ** | 0.136 | 0.579 ** | 1 |
| Sig. (2-tailed) | <0.001 | 0.197 | <0.001 | ||
| The Results for 25 Departments | |||||
| Density | Pearson correlation | 1 | 0.037 | 0.716 ** | 0.644 ** |
| Sig. (2-tailed) | 0.860 | <0.001 | <0.001 | ||
| Poverty | Pearson correlation | −0.037 | 1 | −0.140 | 0.158 |
| Sig. (2-tailed) | 0.860 | 0.860 | 0.452 | ||
| Infections * | Pearson correlation | 0.716 ** | -0.040 | 1 | 0.391 |
| Sig. (2-tailed) | <0.001 | 0.850 | 0.053 | ||
| Deaths * | Pearson correlation | 0.644 ** | 0.158 | 0.391 | 1 |
| Sig. (2-tailed) | <0.001 | 0.452 | 0.053 | ||
| Departements | Density hab/km2 | Number of Infections for 100,000 Habitants | ||||
|---|---|---|---|---|---|---|
| Before the 2.Peak of Epidemic 22–28 March 2021 | During the Peak of Epidemic 27 March–2 April 2021 | The Close Period 05–11 April 2021 | After the Close Period 27 April–3 May 2021 | |||
| 1 | Seine Saint- Denis (93) | 7822 | 779 | 825 | 686 | 379 |
| 2 | Val-de-Marne (94) | 7103 | 716 | 749 | 609 | 380 |
| 3 | Paris (75) | 21,000 | 608 | 631 | 525 | 310 |
| 4 | Seine et Marne (77) | 319 | 695 | 736 | 544 | 331 |
| 5 | Val-d’Oise (95) | 1133 | 813 | 861 | 672 | 355 |
| 6 | Essonne (91) | 956 | 560 | 634 | 522 | 332 |
| 7 | Bouches-du-Rhône (13) | 376 | 531 | 581 | 490 | 288 |
| 8 | Oise (60) | 129 | 557 | 615 | 478 | 299 |
| 9 | Hauts de Seine (92) | 10,866 | 501 | 544 | 472 | 283 |
| 10 | Yvelines (78) | 774 | 554 | 590 | 464 | 248 |
| 11 | Rhône (69) | 573 | 500 | 550 | 441 | 267 |
| 12 | Loire (42) | 27 | 437 | 460 | 434 | 278 |
| 13 | Doubs (25) | 97 | 483 | 488 | 415 | 229 |
| 14 | Vaucluse (84) | 149 | 461 | 479 | 404 | 256 |
| 15 | Nord (59) | 475 | 544 | 489 | 405 | 273 |
| 16 | Pas-de-Calais (62) | 217 | 496 | 519 | 399 | 255 |
| 17 | Nièvre (58) | 38 | 395 | 439 | 394 | 225 |
| 18 | Aisne (02) | 66 | 473 | 480 | 390 | 277 |
| 19 | Gard (30) | 114 | 392 | 436 | 371 | 227 |
| 20 | Seine Maritime (76) | 191 | 312 | 422 | 369 | 263 |
| 21 | Var (83) | 220 | 452 | 465 | 361 | 177 |
| 22 | Somme (80) | 72 | 454 | 478 | 352 | 233 |
| 23 | Eure (27) | 98 | 331 | 426 | 345 | 208 |
| 24 | Aube (10) | 71 | 531 | 567 | 339 | 196 |
| 25 | Alpes-de-Hautes de Provence (04) | 27 | 410 | 458 | 332 | 196 |
| 26 | Ain (01) | 145 | 289 | 402 | 314 | 184 |
| 27 | Isère (38) | 224 | 308 | 411 | 308 | 173 |
| 28 | Hautes-Alpes (05) | 29 | 370 | 434 | 291 | 190 |
| 29 | The Alpes Maritimes (06) | 402 | 402 | 440 | 274 | 110 |
| Measure: MEASURE_1 | ||||||
|---|---|---|---|---|---|---|
| (I) Lockdown Impact | (J) Lockdown Impact | Mean Difference (I–J) | Std. Error | Sig. b | 95% Confidence Interval for Difference b | |
| Lower Bound | Upper Bound | |||||
| (1) Before the peak | 2 | −43.279 * | 6.388 | <0.001 | −61.411 | −25.141 |
| 3 | 67.379 * | 10.648 | <0.001 | 37.150 | 97.609 | |
| 4 | 239.034 * | 16.640 | <0.001 | 191.795 | 286.274 | |
| (2) During the peak | 1 | 43.276* | 6.388 | <0.001 | 25.141 | 61.411 |
| 3 | 110.655 * | 8.444 | <0.001 | 86.682 | 134.628 | |
| 4 | 282.310 * | 14.914 | <0.001 | 239.969 | 324.651 | |
| (3) Lockdown period | 1 | −67.379 * | 10.648 | <0.001 | −97.609 | −37.150 |
| 2 | −110.655 * | 8.444 | <0.001 | −134.628 | −86.682 | |
| 4 | 171.655 * | 9.682 | <0.001 | 144.168 | 199.143 | |
| (4) End of Lockdown | 1 | −239.034 * | 16.640 | <0.001 | −286.274 | −191.795 |
| 2 | −282.310 * | 14.914 | <0.001 | −324.651 | −239.969 | |
| 3 | −171.655 * | 9.682 | <0.001 | −199.143 | −144.168 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maya, R. Social and Spatial Inequalities during COVID-19: Evidence from France and the Need for a New Sustainable Urban and Regional Development Paradigm. Sustainability 2024, 16, 3501. https://doi.org/10.3390/su16083501
Maya R. Social and Spatial Inequalities during COVID-19: Evidence from France and the Need for a New Sustainable Urban and Regional Development Paradigm. Sustainability. 2024; 16(8):3501. https://doi.org/10.3390/su16083501
Chicago/Turabian StyleMaya, Roula. 2024. "Social and Spatial Inequalities during COVID-19: Evidence from France and the Need for a New Sustainable Urban and Regional Development Paradigm" Sustainability 16, no. 8: 3501. https://doi.org/10.3390/su16083501





