Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function
Abstract
1. Introduction
2. Dietary Potassium Intake
2.1. Renal Regulation of Potassium Balance
2.2. The Role of the Gastrointestinal Tract in Regulating Potassium Balance
2.3. Sources, Composition of Diet and Hyperkalaemia
3. Dietary Intervention to Limit Potassium Intake
- (a)
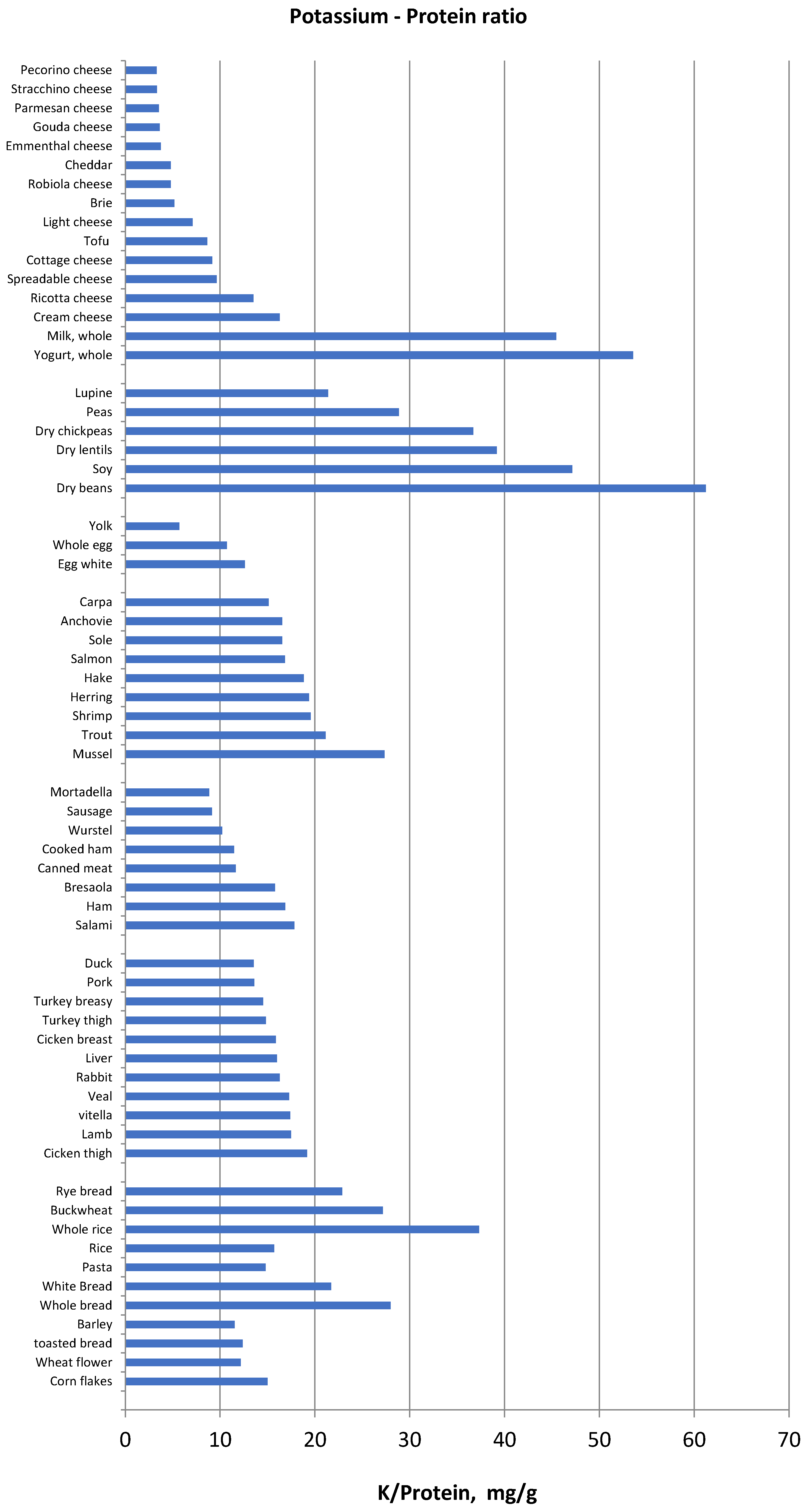
- Knowledge and education about the type of foods which contain excess potassium (per serving or per unit of weight), about the foods needed for proper nutrition in CKD and ESRD, and that supply a low potassium load.
- (b)
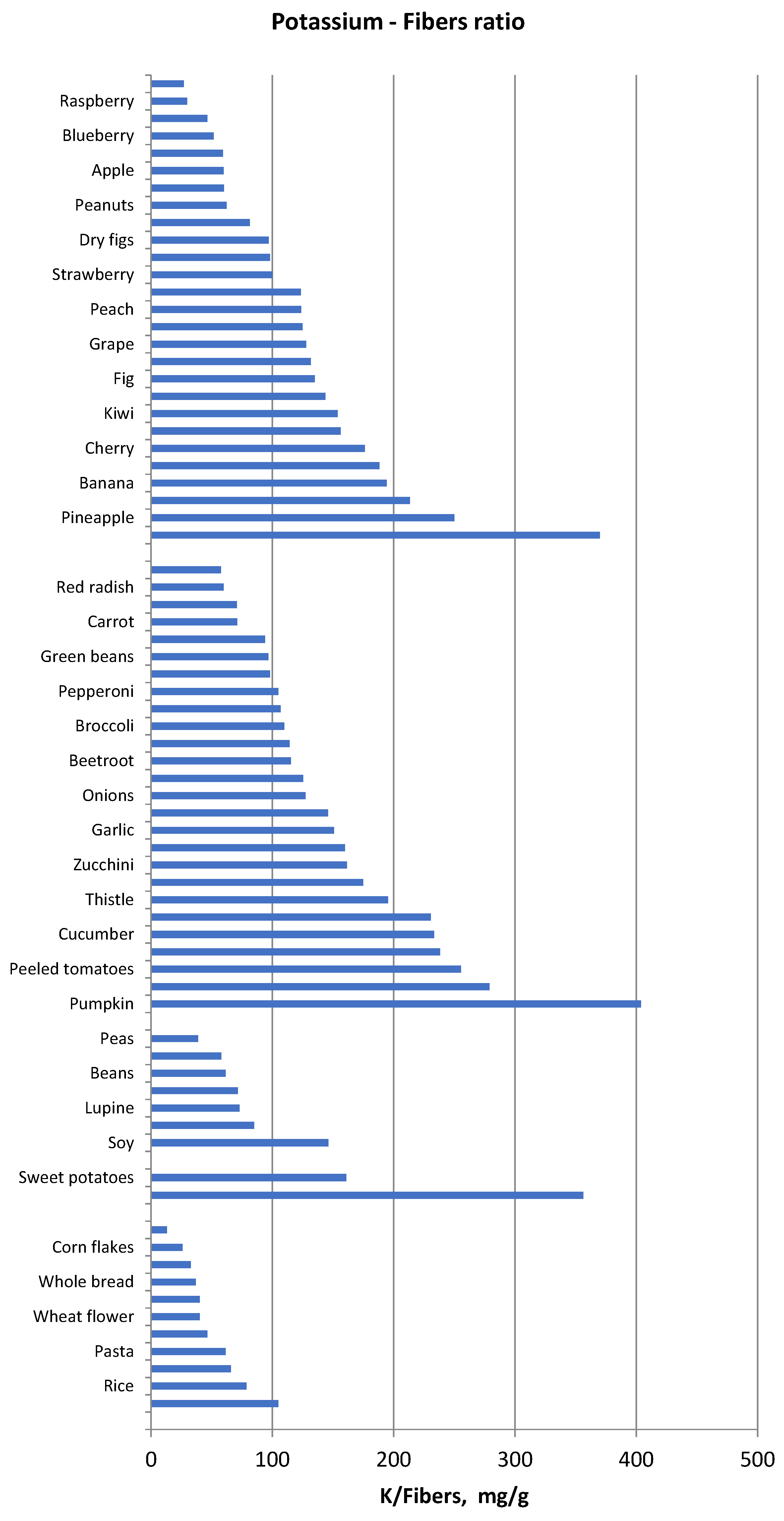
- Classification of foods based on their potassium content normalized per unit of fibre.
- (c)
- Education about the use of cooking procedures (especially boiling) in order to achieve demineralization and in particular for removing potassium before eating.
- (d)
- Attention to hidden sources of potassium (e.g., food additives and low-sodium salt substitutes).
4. Low Potassium Regimens for Pragmatic Management of CKD Patients with Hyperkalaemia
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
Abbreviations
| CKD | Chronic Kidney Disease |
| RAAS | Renin-Angiotensin-Aldosterone System |
| ESRD | End Stage Renal Disease |
| RDA | Recommended Daily Allowance |
| NDD | Non-Dialysis Dependent |
| NKF | National Kidney Foundation |
| MBD | Mineral Bone Disease |
| HF | Heart Failure |
| LPD | Low Protein Diet |
| ADI | Acceptable Daily Intake |
| BSA | Body Surface Area |
| DPI | Dietary Protein Intake |
| EAA | Essential Amino-Acids |
| eGFR | estimated Glomerular Filtration Rate |
| HBV | High Biologic Value (referred to protein) |
| HTN | Hypertension |
| IBW | Ideal Body Weight |
| KA | Ketoacids (keto-analogues of amino-acids) |
| P | Phosphorus |
| PD | Peritoneal Dialysis |
| RKF | Residual Kidney Function |
| sHPT | secondary Hyperparathyroidism |
References
- Kovesdy, C.P.; Regidor, D.L.; Mehrotra, R.; Jing, J.; McAllister, C.J.; Greenland, S.; Kopple, J.D.; Kalantar-Zadeh, K. Serum and dialysate potassium concentrations and survival in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2007, 2, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Pun, P.H.; Lehrich, R.W.; Honeycutt, E.F.; Herzog, C.A.; Middleton, J.P. Modifiable risk factors associated with sudden cardiac arrest within hemodialysis clinics. Kidney Int. 2011, 79, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Gumz, M.L.; Rabinowitz, L.; Wingo, C.S. An Integrated View of Potassium Homeostasis. N. Engl. J. Med. 2015, 373, 60–72. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.F.; Clegg, D.J. Physiology and pathophysiology of potassium homeostasis. Adv. Physiol. Educ. 2016, 40, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Palmer, B.F.; Clegg, D.J. Achieving the Benefits of a High-Potassium, Paleolithic Diet, without the Toxicity. Mayo Clin. Proc. 2016, 91, 496–508. [Google Scholar] [CrossRef] [PubMed]
- Burnier, M. Should we eat more potassium to better control blood pressure in hypertension? Nephrol. Dial. Transplant. 2018. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Management of hyperkalaemia in chronic kidney disease. Nat. Rev. Nephrol. 2014, 10, 653–662. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P.; Appel, L.J.; Grams, M.E.; Gutekunst, L.; McCullough, P.A.; Palmer, B.F.; Pitt, B.; Sica, D.A.; Townsend, R.R. Potassium homeostasis in health and disease: A scientific workshop cosponsored by the National Kidney Foundation and the American Society of Hypertension. J. Am. Soc. Hypertens. 2017, 11, 783–800. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Guideline: Potassium Intake for Adults and Children; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- K/DOQI, National Kidney Foundation. Clinical Practice guidelines for nutrition in chronic renal failure. Am. J. Kidney Dis. 2000, 35, S1–S140. [Google Scholar]
- Kalantar-Zadeh, K.; Fouque, D. Nutritional Management of Chronic Kidney Disease. N. Engl. J. Med. 2017, 377, 1765–1776. [Google Scholar] [CrossRef] [PubMed]
- Rabelink, T.J.; Koomans, H.A.; Hené, R.J.; Dorhout Mees, E.J. Early and late adjustment to potassium loading in humans. Kidney Int. 1990, 38, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Hayes, C.P., Jr.; Robinson, R.R. Fecal potassium excretion in patients on chronic intermittent hemodialysis. Trans. Am. Soc. Artif. Intern. Organs 1965, 11, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Hayes, C.P., Jr.; McLeod, M.E.; Robinson, R.R. An extrarenal mechanism for the maintenance of potassium balance in severe chronic renal failure. Trans. Assoc. Am. Physicians 1967, 80, 207–216. [Google Scholar] [PubMed]
- Agarwal, R.; Afzalpurkar, R.; Fordtran, J.S. Pathophysiology of potassium absorption and secretion by the human intestine. Gastroenterology 1994, 107, 548–571. [Google Scholar] [CrossRef]
- St-Jules, D.E.; Goldfarb, D.S.; Sevick, M.A. Nutrient Non-equivalence: Does Restricting High-Potassium Plant Foods Help to Prevent Hyperkalemia in Hemodialysis Patients? J. Ren. Nutr. 2016, 26, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Noori, N.; Kalantar-Zadeh, K.; Kovesdy, C.P.; Murali, S.B.; Bross, R.; Nissenson, A.R.; Kopple, J.D. Dietary potassium intake and mortality in long-term hemodialysis patients. Am. J. Kidney Dis. 2010, 56, 338–347. [Google Scholar] [CrossRef] [PubMed]
- USDA National Nutrient Database for Standard Reference, Release 28. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/nutrient-data-laboratory/docs/usda-national-nutrient-database-for-standard-reference/ (accessed on 15 December 2016).
- Prajapati, K.; Modi, H.A. The importance of potassium in plant growth—A review. Indian J. Plant Sci. 2012, 1, 177–186. [Google Scholar]
- Gupta, S.; Yadav, B.S.; Raj, U.; Freilich, S.; Varadwaj, P.K. Transcriptomic analysis of soil grown T. aestivum cv. root to reveal the changes in expression of genes in response to multiple nutrients deficiency. Front. Plant Sci. 2017, 8, 1025. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wu, W.H. Regulation of potassium transport and signaling in plants. Curr. Opin. Plant Biol. 2017, 12, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Aparicio, M.; Bellizzi, V.; Chauveau, P.; Cupisti, A.; Ecder, T.; Fouque, D.; Garneata, L.; Lin, S.; Mitch, W.E.; Teplan, V.; et al. Keto acid therapy in predialysis chronic kidney disease patients: Final consensus. J. Ren. Nutr. 2012, 22, S22–S24. [Google Scholar] [CrossRef] [PubMed]
- Cupisti, A.; D’Alessandro, C.; Gesualdo, L.; Cosola, C.; Gallieni, M.; Egidi, M.F.; Fusaro, M. Non-Traditional Aspects of Renal Diets: Focus on Fiber, Alkali and Vitamin K1 Intake. Nutrients 2017, 9, 444. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Metabolic acidosis and kidney disease: Does bicarbonate therapy slow the progression of CKD? Nephrol. Dial. Transplant. 2012, 27, 3056–3062. [Google Scholar] [CrossRef] [PubMed]
- Barsotti, G.; Morelli, E.; Cupisti, A.; Meola, M.; Dani, L.; Giovannetti, S. A low-nitrogen low-phosphorus vegan diet for patients with chronic renal failure. Nephron 1996, 74, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Cupisti, A.; Morelli, E.; Meola, M.; Barsotti, M.; Barsotti, G. Vegetarian diet alternated with conventional low-protein diet for patients with chronic renal failure. J. Ren. Nutr. 2002, 12, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Di Iorio, B.R.; Di Micco, L.; Marzocco, S.; De Simone, E.; De Blasio, A.; Sirico, M.L.; Nardone, L.; On Behalf Of Ubi Study Group. Very Low- protein Diet (VLPD) Reduces Metabolic Acidosis in subjects with Chronic Kidney Disease: The “Nutritional Light Signal” of the RenalAcid Load. Nutrients 2017, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Moorthi, R.N.; Armstrong, C.L.; Janda, K.; Ponsler-Sipes, K.; Asplin, J.R.; Moe, S.M. The effect of a diet containing 70% protein from plants on mineral metabolism and musculoskeletal health in chronic kidney disease. Am. J. Nephrol. 2014, 40, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Meijers, B.K.; De Pretern, V.; Verbeke, K.; Vanrenterghem, Y.; Evenepoel, P. p-Cresyl sulfate serum concentrations in haemodialysis patients are reduced by the prebiotic oligofructose-enriched inulin. Nephrol. Dial. Transplant. 2010, 25, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Salmean, Y.A.; Segal, M.S.; Langkamp-Henken, B.; Canales, M.T.; Zello, G.A.; Dahl, W.J. Foods with added fiber lower serum creatinine levels in patients with chronic kidney disease. J. Ren. Nutr. 2013, 23, e29–e32. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, M.; Montemurno, E.; Vannini, L.; Cosola, C.; Cavallo, N.; Gozzi, G.; Maranzano, V.; Di Cagno, R.; Gobbetti, M.; Gesualdo, L. Effect of whole-grain barley on the human fecal microbiota and metabolome. Appl. Environ. Microbiol. 2015, 81, 7945–7956. [Google Scholar] [CrossRef] [PubMed]
- Cosola, C.; De, M.; Rocchetti, M.T.; Montemurno, E.; Maranzano, V.; Dalfino, G.; Manno, C.; Zito, A.; Gesualdo, M.; Ciccone, M.M.; et al. Beta-glucans supplementation associates with reduction in p-cresyl sulfate levels and improved endothelial vascular reactivity in healthy individuals. PLoS ONE 2017, 12, e0169635. [Google Scholar] [CrossRef] [PubMed]
- Goraya, N.; Simoni, J.; Jo, C.H.; Wesson, D.E. A comparison of treating metabolic acidosis in CKD stage 4 hypertensive kidney disease with fruits and vegetables or sodium bicarbonate. Clin. J. Am. Soc. Nephrol. 2013, 8, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Weir, M.R.; Bakris, G.L.; Bushinsky, D.A.; Mayo, M.R.; Garza, D.; Stasiv, Y.; Wittes, J.; Christ-Schmidt, H.; Berman, L.; Pitt, B. Patiromer in patients with kidney disease and hyperkalemia receiving RAAS inhibitors. N. Engl. J. Med. 2015, 372, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Packham, D.K.; Rasmussen, H.S.; Lavin, P.T.; El-Shahawy, M.A.; Roger, S.D.; Block, G.; Qunibi, W.; Pergola, P.; Singh, B. Sodium zirconium cyclosilicate in hyperkalemia. N. Engl. J. Med. 2015, 372, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Bellizzi, V.; Cupisti, A.; Locatelli, F.; Bolasco, P.; Brunori, G.; Cancarini, G.; Caria, S.; De Nicola, L.; Di Iorio, B.R.; Di Micco, L.; et al. “Conservative Treatment of CKD” study group of the Italian Society of Nephrology. Low-protein diets for chronic kidney disease patients: The Italian experience. BMC Nephrol. 2016, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Jones, W.L. Demineralization of a wide variety of foods for the renal patient. J. Renal Nutr. 2001, 11, 90–96. [Google Scholar] [CrossRef]
- Burrowes, J.D.; Ramer, N.J. Removal of potassium from tuberous root vegetables by leaching. J. Ren. Nutr. 2006, 16, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Asiimwe, J.; Sembajwe, L.F.; Senoga, A.; Bakiika, E.; Muwonge, H.; Kalyesubula, R. Overnight soaking or boiling of “Matooke” to reduce potassium content for patients with chronic kidney disease: Does it really work? Afr. Health Sci. 2013, 13, 546–550. [Google Scholar] [CrossRef] [PubMed]
- Picq, C.; Asplanato, M.; Bernillon, N.; Fabre, C.; Roubeix, M.; Ricort, J.M. Effects of water soaking and/or sodium polystyrene sulfonate addition on potassium content of foods. Int. J. Food Sci. Nutr. 2014, 65, 673–677. [Google Scholar] [CrossRef] [PubMed]
- Bethke, P.C.; Jansky, S.H. The effects of boiling and leaching on the content of potassium and other minerals in potatoes. J. Food Sci. 2008, 73, H80–H85. [Google Scholar] [CrossRef] [PubMed]
- Kovesdy, C.P. Updates in hyperkalemia: Outcomes and therapeutic strategies. Rev. Endocr. Metab. Disord. 2017, 18, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Sherman, R.A.; Mehta, O. Phosphorus and potassium content of enhanced meat and poultry products: Implications for patients who receive dialysis. Clin. J. Am. Soc. Nephrol. 2009, 4, 1370–1373. [Google Scholar] [CrossRef] [PubMed]
- Parpia, A.S.; L’Abbé, M.; Goldstein, M.; Arcand, J.; Magnuson, B.; Darling, P. The Impact of Additives on the Phosphorus, Potassium, and Sodium Content of Commonly Consumed Meat, Poultry, and Fish Products Among Patients With Chronic Kidney Disease. J. Ren. Nutr. 2017, 28, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Parpia, A.S.; Goldstein, M.B.; Arcand, J.; Cho, F.; L’Abbé, M.R.; Darling, P.B. Sodium-reduced Meat and Poultry Products Contain a Significant Amount of Potassium from Food Additives. J. Acad. Nutr. Diet. 2018. [Google Scholar] [CrossRef] [PubMed]
- Dietary Guidelines Advisory Committee. The Report of the Dietary Guidelines Advisory Committee on Dietary Guidelines for Americans; Department of Health and Human Services and Department of Agriculture: Washington, DC, USA, 2005.
| Normal kidney function (eGFR ≥ 60 *) and no proteinuria but at higher CKD risk, e.g., diabetes, hypertension, or solitary kidney | Mild to moderate CKD (eGFR 30 < 60 *) without substantial proteinuria (<0.3 g/day) | Advanced CKD (eGFR < 30 *) or any CKD with substantial proteinuria (>0.3 g/day) | Prevalent dialysis therapy, or any CKD stage with existing or imminent PEW | |
|---|---|---|---|---|
| Dietary Potassium (g/day) | Same as recommended for the general population (4.7 g/day). | Same as the general population unless frequent or severe hyperkalaemia excursions. | <3 g/day if hyperkalaemia occurs frequently while maintaining high fibre intake. | <3 g/day target high fibre intake |
| Potassium (mg) | Potassium (mg) | ||||||
|---|---|---|---|---|---|---|---|
| 100 g | Serving | 100 kcal | 100 g | Serving | 100 kcal | ||
| Meat | Milk and dairy | ||||||
| Chicken breast | 370 | 370 | 370 | Milk | 150 | 188 | 234 |
| Chicken thigh | 355 | 355 | 332 | Yogurt | 150 | 188 | 170 |
| Duck | 290 | 290 | 182 | Brie | 100 | 50 | 31 |
| Lamb | 350 | 350 | 220 | Cheddar | 120 | 60 | 31 |
| Liver | 320 | 320 | 225 | Cottage cheese | 89 | 89 | 77 |
| Pork | 290 | 290 | 185 | Cream cheese | 150 | 150 | 84 |
| Rabbit | 360 | 360 | 261 | Emmenthal cheese | 107 | 54 | 27 |
| Turkey breast | 320 | 320 | 221 | Gouda cheese | 89 | 45 | 26 |
| Turkey thigh | 310 | 310 | 167 | Parmesan cheese | 120 | 60 | 30 |
| Beef | 330 | 330 | 206 | Pecorino cheese | 94 | 47 | 24 |
| Veal | 360 | 360 | 391 | Ricotta cheese | 119 | 119 | 82 |
| Preserved meat | Spreadable cheese | 108 | 54 | 35 | |||
| Bresaola | 505 | 253 | 334 | Stracchino cheese | 62 | 62 | 21 |
| Canned meat | 140 | 140 | 226 | Fats | |||
| Cooked ham | 227 | 114 | 106 | Butter | 15 | 2 | 2 |
| Ham | 454 | 227 | 203 | Cream | 91 | 9 | 44 |
| Mortadella | 130 | 65 | 41 | Margarine | 5 | 1 | 1 |
| Salami | 473 | 237 | 123 | Olive oil | 0 | 0 | 0 |
| Sausage | 130 | 65 | 33 | Sugar and Sweets sand | |||
| Wurstel | 140 | 70 | 52 | Dark chocolate | 300 | 30 | 55 |
| Fish | Fruit ice cream | 180 | 72 | 101 | |||
| Anchovies | 278 | 417 | 290 | Honey | 51 | 3 | 17 |
| Carpa | 286 | 429 | 204 | Marmalade | 100 | 5 | 45 |
| Hake | 320 | 480 | 451 | Milk chocolate | 420 | 42 | 74 |
| Herring | 320 | 480 | 148 | Milk ice cream | 110 | 44 | 46 |
| Mussel | 320 | 480 | 381 | Sugar | 2 | 0 | 1 |
| Salmon | 310 | 465 | 168 | Beverages | |||
| Shrimp | 266 | 399 | 375 | Beer | 35 | 116 | 78 |
| Sole | 280 | 420 | 326 | Cola | 1 | 3 | 3 |
| Trout | 429 | 644 | 364 | Orange juice | 150 | 300 | 417 |
| Egg | Red wine | 110 | 138 | 145 | |||
| Egg white | 135 | 95 | 314 | Tea | 0 | 0 | 0 |
| Whole egg | 133 | 67 | 104 | Wine | 61 | 76 | 86 |
| Yolk | 90 | 31 | 28 | ||||
| Potassium (mg) | Potassium (mg) | |||||||
|---|---|---|---|---|---|---|---|---|
| 100 g | Serving | 100 kcal | 100 g | Serving | 100 kcal | |||
| Cereals and tubers | Pulses | |||||||
| Barley | 120 | 60 | 38 | Beans | 650 | 650 | 625 | |
| Buckwheat | 220 | 176 | 60 | Dry beans | 1445 | 723 | 465 | |
| Corn flakes | 99 | 45 | 27 | Dry chickpeas | 800 | 400 | 239 | |
| Pasta | 160 | 128 | 45 | Dry lentils | 980 | 490 | 302 | |
| Rice | 110 | 88 | 30 | Dry soy beans | 1740 | 870 | 437 | |
| Rye bread | 190 | 95 | 86 | Lupine | 351 | 351 | 308 | |
| Toasted bread | 140 | 35 | 34 | Peas | 202 | 202 | 266 | |
| White Bread | 176 | 88 | 64 | Fruits | ||||
| Whole bread | 210 | 105 | 86 | Apple | 120 | 180 | 267 | |
| Whole rice | 250 | 200 | 70 | Apricot | 320 | 480 | 1143 | |
| Potatoes | 570 | 1140 | 671 | Banana | 350 | 525 | 530 | |
| Sweet potatoes | 370 | 740 | 425 | Blackberry | 260 | 390 | 722 | |
| Vegetables | Blueberry | 160 | 240 | 640 | ||||
| Asparagus | 240 | 480 | 828 | Cherry | 229 | 344 | 603 | |
| Basil | 300 | 600 | 769 | Fig | 270 | 405 | 574 | |
| Beetroot | 300 | 600 | 1579 | Grape | 192 | 288 | 315 | |
| Broccoli | 340 | 680 | 1259 | Grapefruit | 230 | 345 | 885 | |
| Carrot | 220 | 440 | 667 | Kiwi | 400 | 600 | 909 | |
| Cauliflower | 350 | 700 | 1400 | Lemon | 140 | 210 | 298 | |
| Celery | 280 | 560 | 1400 | Mango | 250 | 375 | 472 | |
| Chard | 286 | 572 | 1682 | Melon | 333 | 500 | 1009 | |
| Cucumber | 140 | 280 | 1000 | Orange | 200 | 300 | 588 | |
| Eggplant | 184 | 368 | 1227 | Peach | 260 | 390 | 963 | |
| Fennel | 276 | 552 | 3067 | Pear | 130 | 195 | 325 | |
| Green beans | 280 | 560 | 1556 | Pineapple | 250 | 375 | 625 | |
| Leeks | 310 | 620 | 1069 | Pomegranate | 290 | 435 | 460 | |
| Lettuce | 240 | 192 | 1263 | Raspberry | 220 | 330 | 647 | |
| Mushrooms | 235 | 470 | 870 | Strawberry | 160 | 240 | 593 | |
| Olives | 432 | 130 | 304 | Tangerine | 210 | 315 | 292 | |
| Onions | 140 | 280 | 538 | Watermelon | 280 | 420 | 1867 | |
| Peeled tomatoes | 230 | 460 | 1095 | Dried fruits and nuts | ||||
| Pepperoni | 210 | 420 | 955 | Dried figs | 1010 | 303 | 395 | |
| Pumpkin | 202 | 404 | 1122 | Dried plum | 824 | 247 | 375 | |
| Red radish | 180 | 360 | 1385 | Almond | 860 | 258 | 159 | |
| Rocket salad | 369 | 295 | 1476 | Cashew nuts | 565 | 170 | 104 | |
| Spinach | 530 | 1060 | 1710 | Nuts | 368 | 110 | 56 | |
| Zucchini | 210 | 420 | 1909 | Peanuts | 680 | 204 | 114 | |
| Food Group/Item | Type of Treatment or Food Processing | % Potassium Content Reduction |
|---|---|---|
| Vegetables (15 different varieties) | Each food was placed in 2 liters of hot tap water (100–110 °F), stirred vigorously for 15–20 s and allowed to stand for a predetermined time period. Ham and hot dogs (meat group) were placed in boiling water bath, stirred and allowed to boil for 3 min. Avocado and banana from the fruit group were placed in cold tap water, stirred gently and allowed to stand for the predetermined time period [37]. | 59 ± 40 |
| Fruits (8 different varieties) | 43 ± 16 | |
| Legumes (5 different varieties) | 78.5 ± 20.5 | |
| Meats (7 different varieties) | 57 ± 41 | |
| Tuberous root vegetables * | Soaking [38] | 8% |
| Tuberous root vegetables * | Double cooking (boil, rinse and boil again) [38] | 46% |
| White Potato (Solanum tuberosum) | Leaching overnight after cubing [41] | 0–4% |
| White Potato (Solanum tuberosum) | Leaching overnight after shredding [41] | 2–17% |
| White Potato (Solanum tuberosum) | Boiling after cubing [41] | 50% |
| White Potato (Solanum tuberosum) | Boiling after shredding [41] | 69–75% |
| Banana (Matooke) | Soaking | No significant reduction |
| Banana (Matooke) | Boiling 60 min at 200 °C [39] | 37% |
| Chocolate | Soaking [40] | 16% |
| Potato | 16% | |
| Apple | 26% | |
| Tomato | 37% | |
| Banana | Soaking [40] | 41% |
| Categories | Chemical Name | E Number (Europe) | ADI | Where to Find Them |
|---|---|---|---|---|
| Preservatives | Potassium sorbate | E202 | 3 mg/kg | Pre-cooked or long-lasting foods, powder dressings, nuts, sauces, preserved meats, stuffed pasta (tortellini, ravioli), jellies, concentrated fruit juices, processed cheeses, wine, margarine |
| Potassium metabisulphite | E224 | 0.35 mg/kg | ||
| Potassium nitrate | E252 | 5 mg/kg | ||
| Antioxidants and acidity regulators | Potassium citrate | E332 | No limit | |
| Potassium tartrate | E336 | 30 mg/kg | ||
| Stabilizers, emulsifier, thickeners | Potassium alginate | E402 | 50 mg/kg | |
| Potassium diphosphate | E450 | 70 mg/kg | ||
| Potassium triphosphate | E451 | 70 mg/kg | ||
| Flavour enhancer | Potassium glutamate | E622 | Not defined | |
| Potassium guanylate | E628 | |||
| Potassium inosinate | E632 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cupisti, A.; Kovesdy, C.P.; D’Alessandro, C.; Kalantar-Zadeh, K. Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function. Nutrients 2018, 10, 261. https://doi.org/10.3390/nu10030261
Cupisti A, Kovesdy CP, D’Alessandro C, Kalantar-Zadeh K. Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function. Nutrients. 2018; 10(3):261. https://doi.org/10.3390/nu10030261
Chicago/Turabian StyleCupisti, Adamasco, Csaba P. Kovesdy, Claudia D’Alessandro, and Kamyar Kalantar-Zadeh. 2018. "Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function" Nutrients 10, no. 3: 261. https://doi.org/10.3390/nu10030261
APA StyleCupisti, A., Kovesdy, C. P., D’Alessandro, C., & Kalantar-Zadeh, K. (2018). Dietary Approach to Recurrent or Chronic Hyperkalaemia in Patients with Decreased Kidney Function. Nutrients, 10(3), 261. https://doi.org/10.3390/nu10030261






