Is a Nutrition Education Intervention Associated with a Higher Intake of Fruit and Vegetables and Improved Nutritional Knowledge among Housewives in Mauritius?
Abstract
:1. Introduction
- To assess the nutrition knowledge, nutrition attitudes, and fruit and vegetable intake of the housewives before and after the nutrition intervention.
- To assess the differences in nutrition knowledge, attitudes, fruit and vegetable intake, and BMI between the determinants categories.
- To determine the impact of the nutrition education intervention on the participants’ nutrition knowledge, attitudes, fruit and vegetable intake, and body mass index.
2. Materials and Methods
2.1. Participants
2.2. Data Gathering Procedure
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics
3.2. Nutrition Behaviors and Body Mass Index
3.3. Impact of Nutrition Education on Nutrition Behaviors and Body Mass Index
4. Discussion
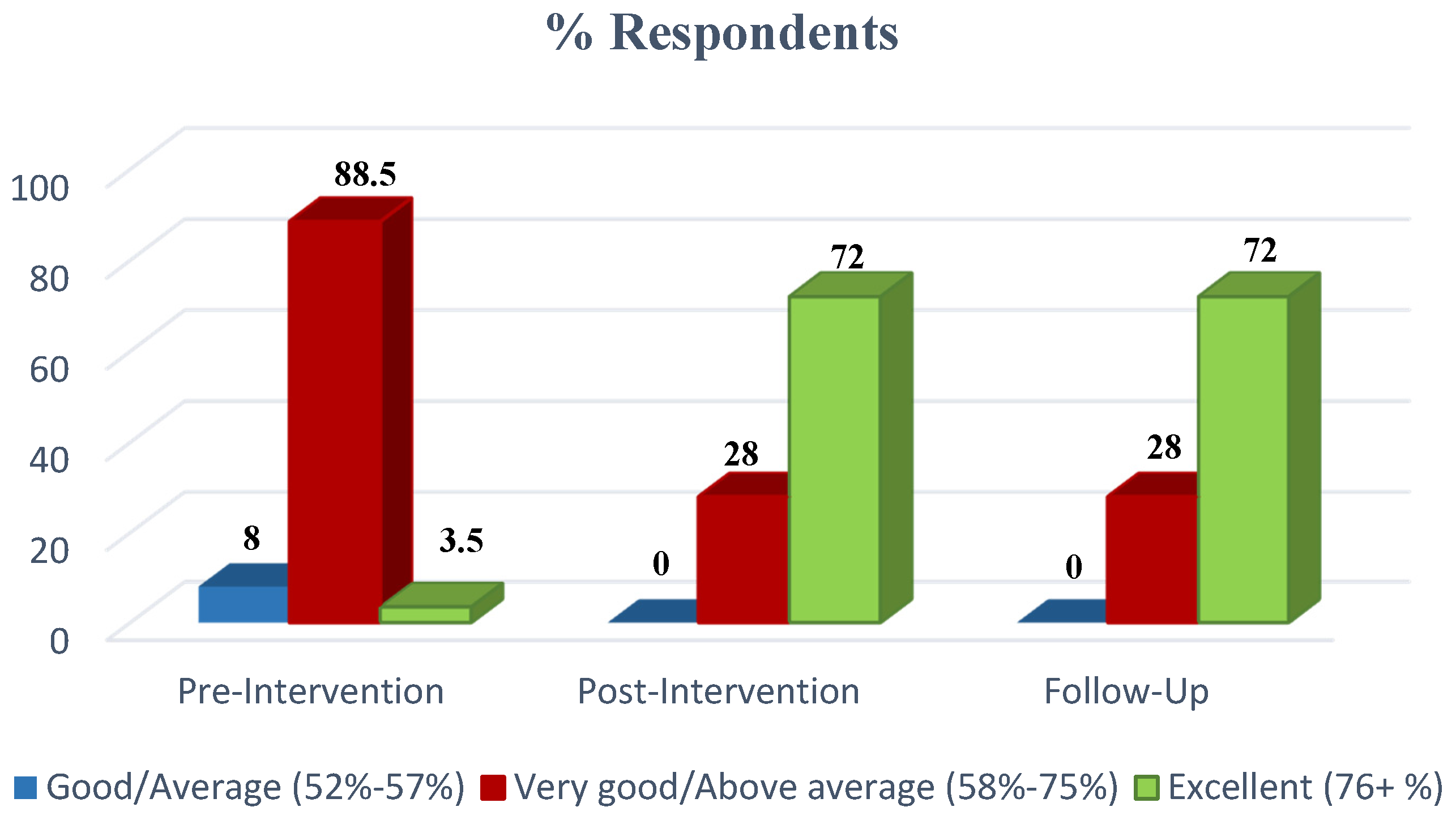
4.1. Nutrition Knowledge
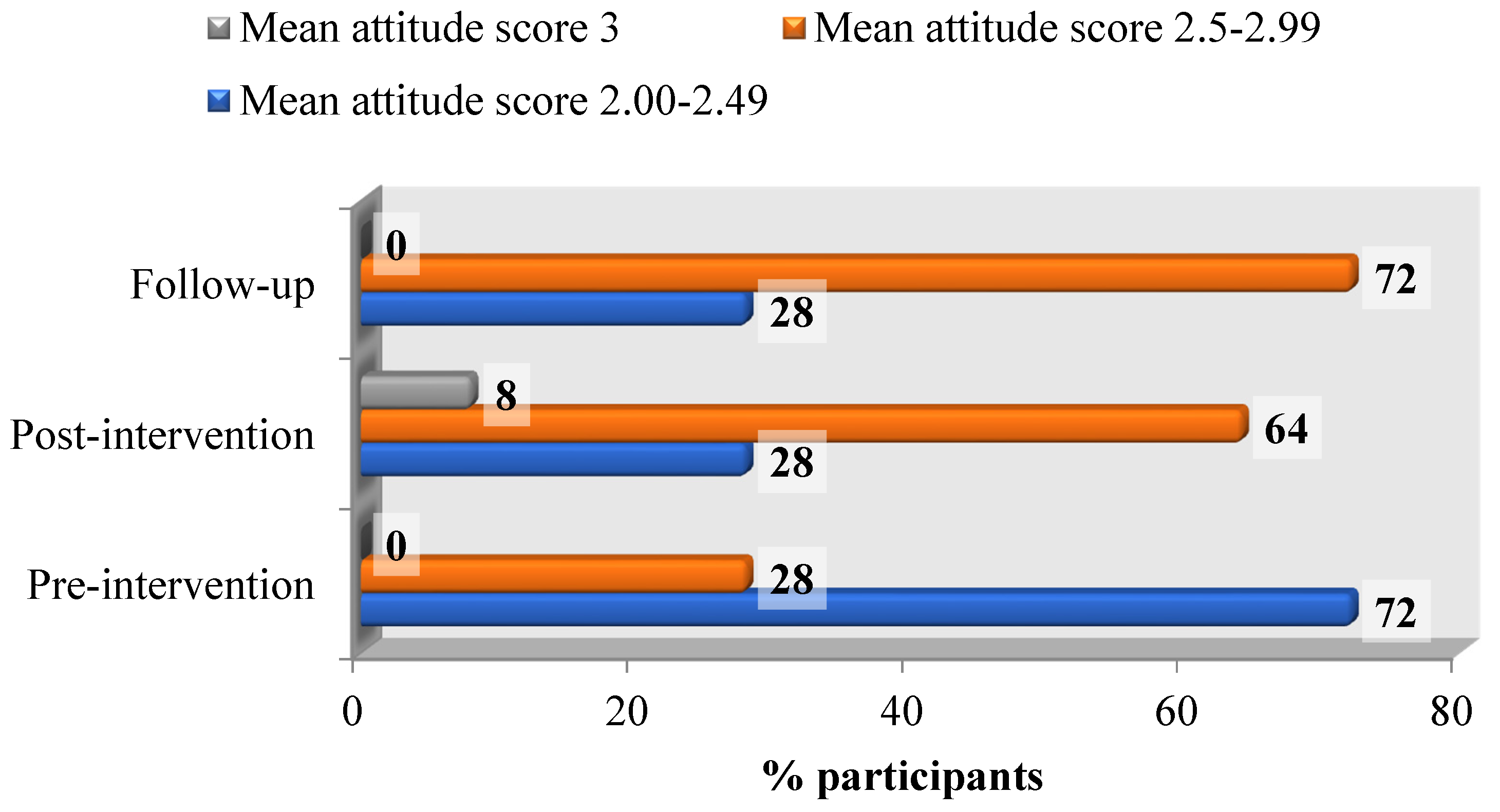
4.2. Nutrition Attitude
4.3. Fruit and Vegetable Intake
4.4. Body Mass Index
4.5. Impact of Nutrition Education on Nutrition Behaviors and Body Mass Index
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- The World Bank. The Growing Danger of Non-Communicable Diseases: Acting Now to Reverse Course; The World Bank: Washington, DC, USA, 2011; Available online: http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/Peer-Reviewed-Publications/WBDeepeningCrisis.pdf (accessed on 17 January 2016).
- Contento, I. Nutrition Education: Linking Theory, Research and Practice, 2nd ed.; Jones and Bartlett Publishers: Burlington, MA, USA, 2010. [Google Scholar]
- Woolf, S.H. A closer look at the economic argument for disease prevention. JAMA 2009, 301, 536–538. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.L.; Sherriff, J.L.; Dhaliwal, S.S.; Mamo, J.C.L. Tailored, iterative, printed dietary feedback is as effective as group education in improving dietary behaviours: Results from a randomised control trial in middle-aged adults with cardiovascular risk factors. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 2–12. [Google Scholar] [CrossRef] [PubMed]
- De Vriendt, T.; Matthys, C.; Verbeke, W.; Pynaert, I.; de Henauw, S. Determinants of nutrition knowledge in young and middle-aged Belgian women and the association with their dietary behaviour. Appetite 2009, 52, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Mirsanjari, M.; Muda, W.A.M.W.; Ahmad, A.; Othman, M.S.; Mosavat, M. Does nutritional knowledge have relationship with healthy dietary attitude and practices during pregnancy? ICNFS 2012, 39, 159–163. [Google Scholar]
- Sabbag, C. Nutrition Habits of Women in Karapinar (Central Anatolia): Corrects and Incorrect. Int. J. Hum. Soc. 2012, 2, 81–88. [Google Scholar]
- Powers, A.R.; Struempler, B.J.; Guarino, A.; Parmer, S.M. Effects of a nutrition education program on the dietary behaviour and nutrition knowledge of second-grade and third-grade students. J. Sch. Health 2005, 75, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Dissen, A.R.; Policastro, P.; Quick, V.; Byrd-Bredbenner, C. Interrelationships among nutrition knowledge, attitudes, behaviours and body satisfaction. J. Health Educ. 2011, 111, 283–295. [Google Scholar] [CrossRef]
- Ministry of Health and Quality of Life (Republic of Mauritius). National Plan of Action for Nutrition 2009–2010; MOHQL: Port Louis, Mauritius, 2009. Available online: http://health.govmu.org/English/Documents/nut1-8.pdf (accessed on 17 January 2016).
- Smith, S.C.; Taylor, J.G.; Stephen, A.M. Use of food labels and beliefs about diet-disease relationships among university students. Public Health Nutr. 2000, 3, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Parmenter, K.; Wardle, J. Development of a general nutrition knowledge questionnaire for adults. Eur. J. Clin. Nutr. 1999, 53, 298–308. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Bredbenner, C.; O’connell, L.H.; Shannon, B.; Eddy, J.M. A nutrition curriculum for health education: Its effects on students’ knowledge, attitudes and behaviour. J. Sch. Health 1984, 54, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Godin, G.; Bélanger-Gravel, A.; Paradis, A.; Vohl, M.; Perusse, L. A simple method to assess fruit and vegetable intake among obese and non-obese individuals. Can. J. Public Health 2008, 99, 494–498. [Google Scholar] [PubMed]
- Ghanem, A.M.; Sen, A.; Philip, B.; Dziewulski, P.; Shelley, O.P. Body Mass Index (BMI) and mortality in patients with severe burns: Is there a “tilt point” at which obesity influences outcome? Burns 2011, 37, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Escamilla, R.; Hromi-Fiedler, A.; Vega-López, S.; Bermúdez-Millán, A.; Segura-Pérez, S. Impact of peer nutrition education on dietary behaviours and health outcomes among Latinos: A systematic literature review. J. Nutr. Educ. Behav. 2008, 40, 208–225. [Google Scholar] [CrossRef] [PubMed]
- Grunert, K.G.; Wills, J.M.; Celemín, L.F.; Lähteenmäki, L.; Scholderer, J.; Bonsmann, S.S.G. Socio-demographic and attitudinal determinants of nutrition knowledge of food shoppers in six European countries. Food Qual. Pref. 2012, 26, 166–177. [Google Scholar] [CrossRef]
- Lyons, B.P. Nutrition education intervention with community-dwelling older adults: Research challenges and opportunities. J. Community Health 2014, 39, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Whati, L.; Senekal, M.; Steyn, N.P.; Lombard, C.; Nel, J. Development of a performance-rating scale for a nutrition knowledge test developed for adolescents. Public Health Nutr. 2009, 12, 1839–1845. [Google Scholar] [CrossRef] [PubMed]
- Bhurosy, T.; Jeewon, R. Effectiveness of a Theory-Driven Nutritional Education Program in Improving Calcium Intake among Older Mauritian Adults. Sci. World J. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Hayward, R.D.; Kang, Y. Psychological, physical, social and spiritual well-being similarities between Korean older adults and family caregivers. Geriatr. Nurs. 2013, 34, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Kisa, S. Health status of elderly women in Turkey. Ageing Int. 2014, 39, 46–54. [Google Scholar] [CrossRef]
- Drichoutis, A.C.; Lazaridis, P.; Nayga, R.M. Nutrition knowledge and consumer use of nutritional food labels. Eur. Rev. Agric. Econ. 2005, 32, 93–118. [Google Scholar] [CrossRef]
- Williams, L.; Campbell, K.; Abbott, G.; Crawford, D.; Ball, K. Is maternal nutrition knowledge more strongly associated with the diets of mothers or their school-aged children? Public Health Nutr. 2012, 15, 1396–1401. [Google Scholar] [CrossRef] [PubMed]
- Tan, C.; Luo, J.; Zong, R.; Fu, C.; Zhang, L.; Mou, J.; Duan, D. Nutrition knowledge, attitudes, behaviours and the influencing factors among non-parent caregivers of rural left-behind children under 7 years old in China. Public Health Nutr. 2010, 13, 1663–1668. [Google Scholar] [CrossRef] [PubMed]
- Kakinami, L.; Houle-Johnson, S.; McGrath, J.J. Parental Nutrition Knowledge Rather Than Nutrition Label Use Is Associated with Adiposity in Children. J. Nutr. Educ. Behav. 2016, 48, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Mistretta, A.; Turconi, G.; Cena, H.; Roggi, C.; Galvano, F. Nutrition knowledge and other determinants of food intake and lifestyle habits in children and young adolescents living in a rural area of Sicily, South Italy. Public Health Nutr. 2013, 16, 1827–1836. [Google Scholar] [CrossRef] [PubMed]
- O’brien, G.; Davies, M. Nutrition knowledge and body mass index. Health Educ. Res. 2007, 22, 571–575. [Google Scholar] [CrossRef] [PubMed]
- Dallongeville, J.; Marécaux, N.; Cottel, D.; Bingham, A. Amouyel Association between nutrition knowledge and nutritional intake in middle-aged men from Northern France. Public Health Nutr. 2000, 4, 27–33. [Google Scholar]
- Choi, E.; Shin, N.; Jung, E.; Park, H.; Lee, H.; Song, K. A study on nutrition knowledge and dietary behaviour of elementary school children in Seoul. Nutr. Res. Pract. 2008, 2, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.M. A Study on the Nutrition Knowledge, the Eating Attitude, and the Eating Behavior of Elementary School Students in Busan. Master’s Thesis, Dong-A University of Korea, Busan, Korea, 2002. [Google Scholar]
- Cox, D.N.; Anderson, A.S.; Lean, M.E.; Mela, D.J. UK consumer attitudes, beliefs and barriers to increasing fruit and vegetable consumption. Public Health Nutr. 1998, 1, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Kostanjevec, S.; Jerman, J.; Koch, V. The influence of nutrition education on the food consumption and nutrition attitude of school children in Slovenia. US-China Educ. Rev. 2012, 11, 953–964. [Google Scholar]
- Erinosho, T.O.; Moser, R.P.; Oh, A.Y.; Nebeling, L.C.; Yaroch, A.L. Awareness of the Fruits and Veggies-More Matters campaign, knowledge of the fruit and vegetable recommendation, and fruit and vegetable intake of adults in the 2007 Food Attitudes and Behaviors (FAB) survey. Appetite 2012, 59, 155–160. [Google Scholar] [CrossRef] [PubMed]
- William, L.; Ball, K.; Crawford, D. Why do some socioeconomically disadvantaged women eat better than others? An investigation of the personal, social and environmental correlates of fruit and vegetable consumption. Appetite 2010, 55, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Ferris, M. Dakota County Childhood Obesity Prevention Initiative: Results from Caregiver Focus Group; Wilder Research: St Paul, MN, USA, 2007; Available online: https://www.wilder.org/Wilder-Research/Publications/Studies/Dakota%20County%20Childhood%20Obesity%20Prevention%20Initiative/Dakota%20County%20Childhood%20Obesity%20Prevention%20Initiative%20-%20Results%20from%20Caregiver%20Focus%20Groups,%20Full%20Report.pdf (accessed on 15 February 2016).
- Boukouvalas, G.; Shankar, B.; Traill, B. Determinants of fruit and vegetable intake in England: A re-examination based on quantile regression. Public Health Nutr. 2009, 12, 2183–2191. [Google Scholar] [CrossRef] [PubMed]
- Zenk, S.N.; Schulz, A.J.; Hollis-Neely, T.; Campbell, R.T.; Holmes, N.; Watkins, G.; Nwankwo, R.; Odoms-Young, A. Fruit and Vegetable Intake in African Americans: Income and Store Characteristics. Am. J. Prev. Med. 2005, 29, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Heimendinger, J.; Patterson, B.H.; Krebs-Smith, S.M.; Pivonka, E.; Kessler, R. Fruit and vegetable intake in the United States: The baseline survey of the Five a Day for Better Health Program. Am. J. Health Promot. 1995, 9, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Alaimo, K.; Packnett, E.; Miles, R.A.; Kruger, D.J. Fruit and vegetable intake among Urban community gardeners. J. Nutr. Educ. Behav. 2008, 40, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Serdula, M.K.; Coates, R.J.; Byers, T.; Simoes, E.; Mokdad, A.H.; Subar, A.F. Fruit and vegetable intake among adults in 16 states: Results of a brief telephone survey. Am. J. Public Health 1998, 85, 236–239. [Google Scholar] [CrossRef]
- Nicklett, E.J.; Kadell, A.R. Fruit and vegetable intake among older adults: A scoping review. Maturitas 2013, 75, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Yannakoulia, M.; Panagiotakos, D.; Pitsavos, C.; Skoumas, Y.; Stafanadis, C. Eating patterns may mediate the association between marital status, body mass index, and blood cholesterol levels in apparently healthy men and women from the ATTICA study. Soc. Sci. Med. 2008, 66, 2230–2239. [Google Scholar] [CrossRef] [PubMed]
- Havas, S.; Treiman, K.; Langenberg, P.; Ballesteros, M.; Anliker, J.; Damron, D.; Feldman, R. Factors associated with fruit and vegetable consumption among women participating in WIC. J. Am. Diet. Assoc. 1998, 98, 1141–1148. [Google Scholar] [CrossRef]
- Wolf, R.L.; Lepore, S.J.; Vandergrift, J.L.; Wetmore-Arkader, L.; Mcginty, E.; Pietrzak, G.; Yaroch, A.L. Knowledge, barriers and stage of change as correlates of fruits and vegetable consumption among urban and mostly immigrant black men. J. Am. Diet. Assoc. 2008, 108, 1315–1322. [Google Scholar] [CrossRef] [PubMed]
- Salehi, L.; Eftekhar, H.; Mohammad, K.; Tavafian, S.S.; Jazayery, A.; Montazeri, A. Consumption of fruit and vegetables among elderly people: A cross sectional study from Iran. Nutr. J. 2010, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Dittus, K.L.; Hillers, V.N.; Beerman, K.A. Benefits and barriers to fruit and vegetable intake: Relationship between attitudes and consumption. J. Nutr. Educ. 1995, 27, 120–126. [Google Scholar] [CrossRef]
- Nooyens, A.C.J.; Visscher, T.L.S.; Verschuren, W.M.M.; Schuit, A.J.; Boshuizen, H.C.; Van Mechelen, W.; Seidell, J.C. Age, period and cohort effects on body weight and body mass index in adults: The Doetinchem cohort study. Public Health Nutr. 2008, 12, 862–870. [Google Scholar] [CrossRef] [PubMed]
- Johnson, W.; Kyvik, K.O.; Skytthe, A.; Deary, A.I.J.; Sørensen, T.I.A. Education modifies genetic and environmental influences on BMI. PLoS ONE 2001, 6, e16290. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, C.A.; Conde, W.L.; Popkin, B.M. Independent effects of income and education on the risk of obesity in the Brazilian adult population. J. Nutr. 2001, 131, 881S–886S. [Google Scholar] [PubMed]
- Fokeena, W.B.; Jeewon, R. Is there an association between socioeconomic status and body mass index among adolescents in Mauritius? Sci. World J. 2012, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bhurosy, T.; Jeewon, R. Food habits, socioeconomic status and body mass index among premenopausal and post-menopausal women in Mauritius. J. Hum. Nutr. Diet. 2013, 26, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Acheampong, I.; Haldeman, L. Are Nutrition Knowledge, Attitudes, and Beliefs Associated with Obesity among Low-Income Hispanic and African American Women Caretakers? J. Obes. 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Azagba, S.; Sharaf, M.F. Fruit and vegetable consumption and body mass index: A quantile regression approach. J. Prim. Care Community Health 2012, 3, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Inayati, D.A.; Scherbaum, V.; Purwestri, R.C.; Wirawan, N.N.; Suryantan, J.; Hartono, S.; Bloem, M.A.; Pangaribuan, R.V.; Biesalski, H.K.; Hoffmann, V.; et al. Improved nutrition knowledge and practice through intensive nutrition education: A study among caregivers of mildly wasted children on Nias Island, Indonesia. Food Nutr. Bull. 2012, 33, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Kostanjevec, S.; Jerman, J.; Koch, V. The effects of nutrition education on 6th graders knowledge of nutrition in nine-year primary schools in Slovenia. Eurasia J. Mathem. Sci. Tech. Educ. 2011, 7, 243–252. [Google Scholar]
- Garcia-Lascurain, M.C.; Kicklighter, J.R.; Jonnalagadda, S.S.; Boudolf, E.A.; Duchon, D. Effect of a nutrition education program on nutrition related knowledge of English-as-second-language elementary school students: A pilot study. J. Immigr. Minor. Health 2006, 8, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Shariff, Z.M.; Bukhari, S.S.; Othman, N.; Hashim, N.; Ismail, M.; Jamil, Z.; Kasim, S.M.; Paim, L.; Samah, B.A.S.; Hussein, Z.A.M. Nutrition education intervention improves nutrition knowledge, attitude and practice of primary school children: A pilot study. Int. Electron. J. Health Educ. 2008, 11, 119–132. [Google Scholar]
- Brug, J.; Steenhuis, I.; van Assema, P.; de Vries, H. The impact of a computer-tailored nutrition intervention. Prev. Med. 1996, 25, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Pomerleau, J.; Lock, K.; Knai, C.; Mckee, M. Interventions designed to increase adult fruit and vegetable intake can be effective: A systematic review of the literature. J. Nutr. 2005, 135, 2486–2495. [Google Scholar] [PubMed]
- Allicock, M.; Johnson, L.S.; Leone, L.; Carr, C.; Walsh, J.; Ni, A.; Resnicow, K.; Pignone, M.; Campbell, M. Promoting Fruit and Vegetable Consumption Among Members of Black Churches, Michigan and North Carolina, 2008–2010. Prev. Chron. Dis. 2013, 10, E33. [Google Scholar] [CrossRef] [PubMed]
- Kothe, E.J.; Mullan, B.A.; Butow, P. Promoting fruits and vegetable Consumption-Testing an intervention based on the theory of planned behaviour. Appetite 2012, 58, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.J.; Warren, J.M.; Lubans, D.R.; Saunders, K.L.; Quick, G.L.; Collins, C.E. The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students. Public Health Nutr. 2010, 13, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Pollard, J.; Kirk, S.F.L.; Cade, J.E. Factors affecting food choice in relation to fruit and vegetable intake: A review. Nutr. Res. Rev. 2002, 15, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Pem, D.; Bhagwant, S.; Jeewon, R. A Pre-and Post-Survey to Determine Effectiveness of a Dietitian-Based Nutrition Education Strategy on Fruit and Vegetable Intake and Energy Intake among Adults. Nutrients 2016, 8, 127. [Google Scholar] [CrossRef] [PubMed]
- Gough, S.; McCann, V.; Seal, J. Do elderly patients with non-insulin dependent diabetes mellitus benefit from diabetes group education? Aust. J. Nutr. Diet. 1992, 49, 55–58. [Google Scholar]
- Friedrich, R.R.; Schuch, I.; Wagner, M.B. Effect of interventions on the body mass index of school-age students. Rev. Saude Publica 2012, 46, 551–560. [Google Scholar] [CrossRef] [PubMed]
| Classification | BMI (kg/m2) |
|---|---|
| Underweight | <18.5 |
| Normal range | 18.5–24.9 |
| Overweight | 25.0–29.9 |
| Obese | ≥30.0 |
| Characteristics | n | % |
|---|---|---|
| Age (years) | ||
| 30–39 | 48 | 24 |
| 40–49 | 80 | 40 |
| 50–59 | 32 | 16 |
| >60 | 40 | 20 |
| Education level | ||
| Never been to school | 32 | 16 |
| Primary level | 32 | 16 |
| Secondary level | 136 | 68 |
| Household income | ||
| <Rs 10,000 (<322 USD) | 32 | 16 |
| Rs 10,000 to Rs 20,000 (322–644 USD) | 64 | 32 |
| >Rs 20,000 to Rs 30,000 (644–966 USD) | 88 | 44 |
| >Rs 30,000 (>966 USD) | 16 | 8 |
| Marital status | ||
| Single | 48 | 24 |
| Married | 152 | 76 |
| Household size | ||
| 1 | 32 | 16 |
| 2 | 8 | 4 |
| 3 | 48 | 24 |
| 4 | 96 | 48 |
| ≥5 | 16 | 8 |
| Number of persons | ||
| Adults | ||
| 1 | 48 | 24 |
| 2 | 152 | 76 |
| Children | ||
| 0 | 40 | 20 |
| 1 | 32 | 16 |
| 2 | 120 | 60 |
| 3 | 8 | 4 |
| Elders | ||
| 0 | 184 | 92 |
| 1 | 16 | 8 |
| Medically certified disease | ||
| No | 64 | 32 |
| Yes | 136 | 64 |
| Mean Scores ± SD | |||
|---|---|---|---|
| Pre-Intervention | Post-Intervention | Follow-Up | |
| Nutrition knowledge | 65.8 ± 6.92 | 82.9 ± 9.32 | 81.9 ± 9.14 |
| Nutrition attitude | 2.37 ± 0.22 | 2.57 ± 0.29 | 2.54 ± 0.26 |
| Fruit and vegetable intake/servings per day | 4.77 ± 1.11 | 4.98 ± 1.13 | 5.03 ± 1.20 |
| Body mass index/kg·m−2 | 22.5 ± 3.87 | 22.5 ± 3.87 | 22.4 ± 3.85 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannoosamy, K.; Pem, D.; Bhagwant, S.; Jeewon, R. Is a Nutrition Education Intervention Associated with a Higher Intake of Fruit and Vegetables and Improved Nutritional Knowledge among Housewives in Mauritius? Nutrients 2016, 8, 723. https://doi.org/10.3390/nu8120723
Cannoosamy K, Pem D, Bhagwant S, Jeewon R. Is a Nutrition Education Intervention Associated with a Higher Intake of Fruit and Vegetables and Improved Nutritional Knowledge among Housewives in Mauritius? Nutrients. 2016; 8(12):723. https://doi.org/10.3390/nu8120723
Chicago/Turabian StyleCannoosamy, Komeela, Dhandevi Pem, Suress Bhagwant, and Rajesh Jeewon. 2016. "Is a Nutrition Education Intervention Associated with a Higher Intake of Fruit and Vegetables and Improved Nutritional Knowledge among Housewives in Mauritius?" Nutrients 8, no. 12: 723. https://doi.org/10.3390/nu8120723




