Optimizing the Nutritional Support of Adult Patients in the Setting of Cirrhosis
Abstract
:1. Introduction
2. Malnutrition in End-Stage Liver Disease
3. Improved Assessment of Malnutrition
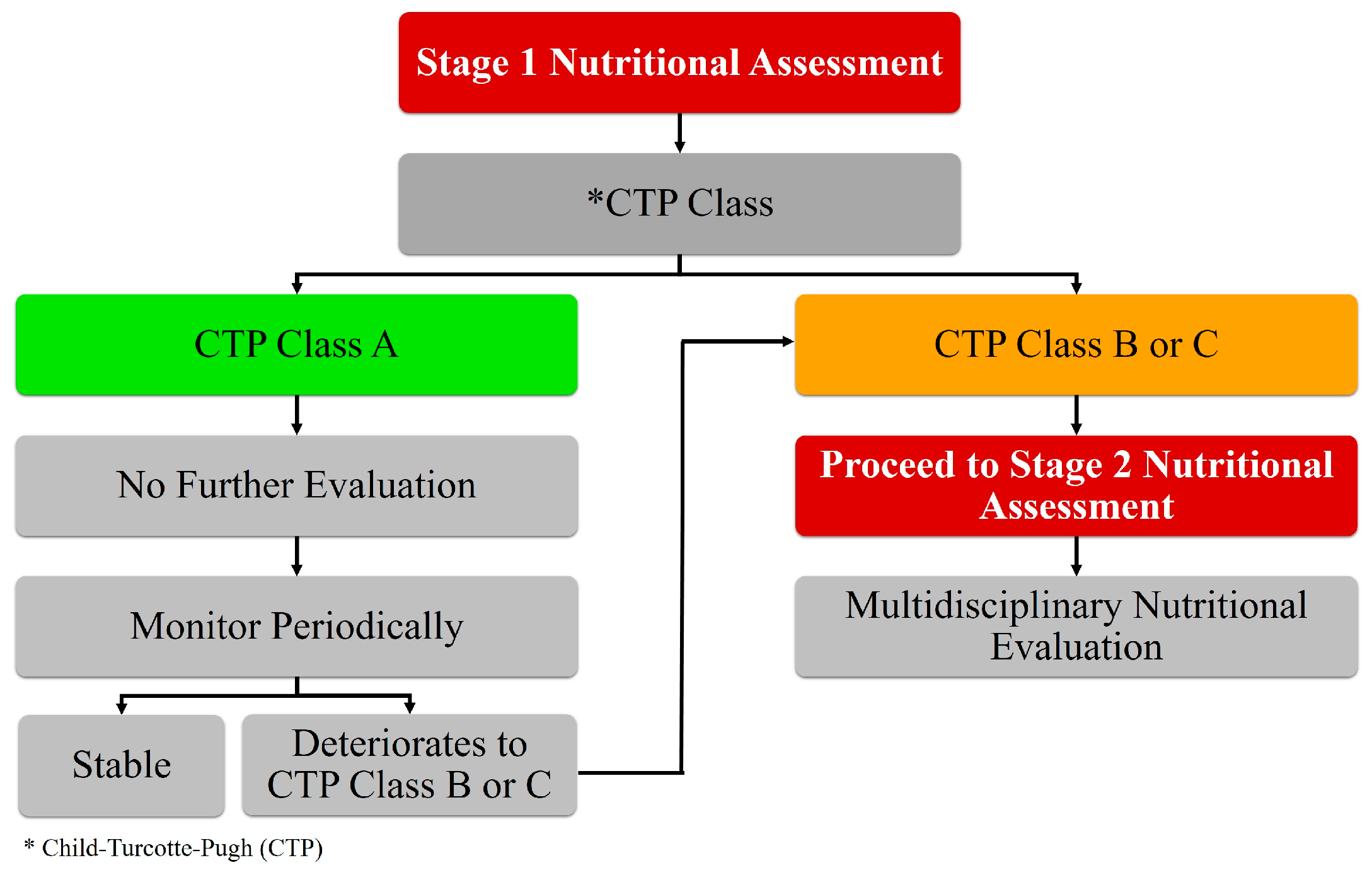
3.1. Stage 1 Assessment for Malnutrition: Define Immediate-Need Populations
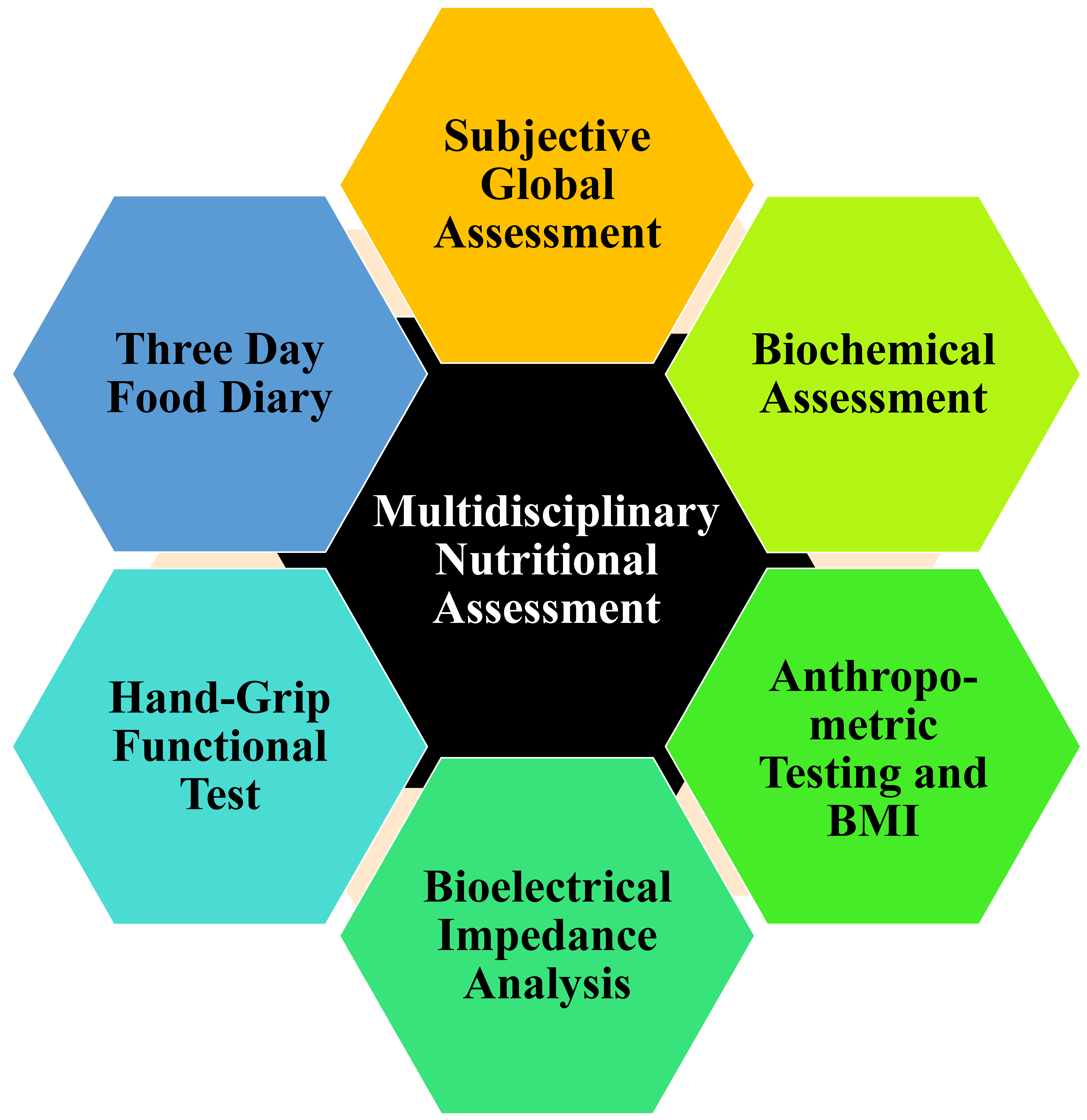
3.2. Stage 2 Assessment for Malnutrition: Multidisciplinary Nutritional Assessment
4. Treatment Options for Malnourished Patients
4.1. Proper Dietary Recommendations and Education
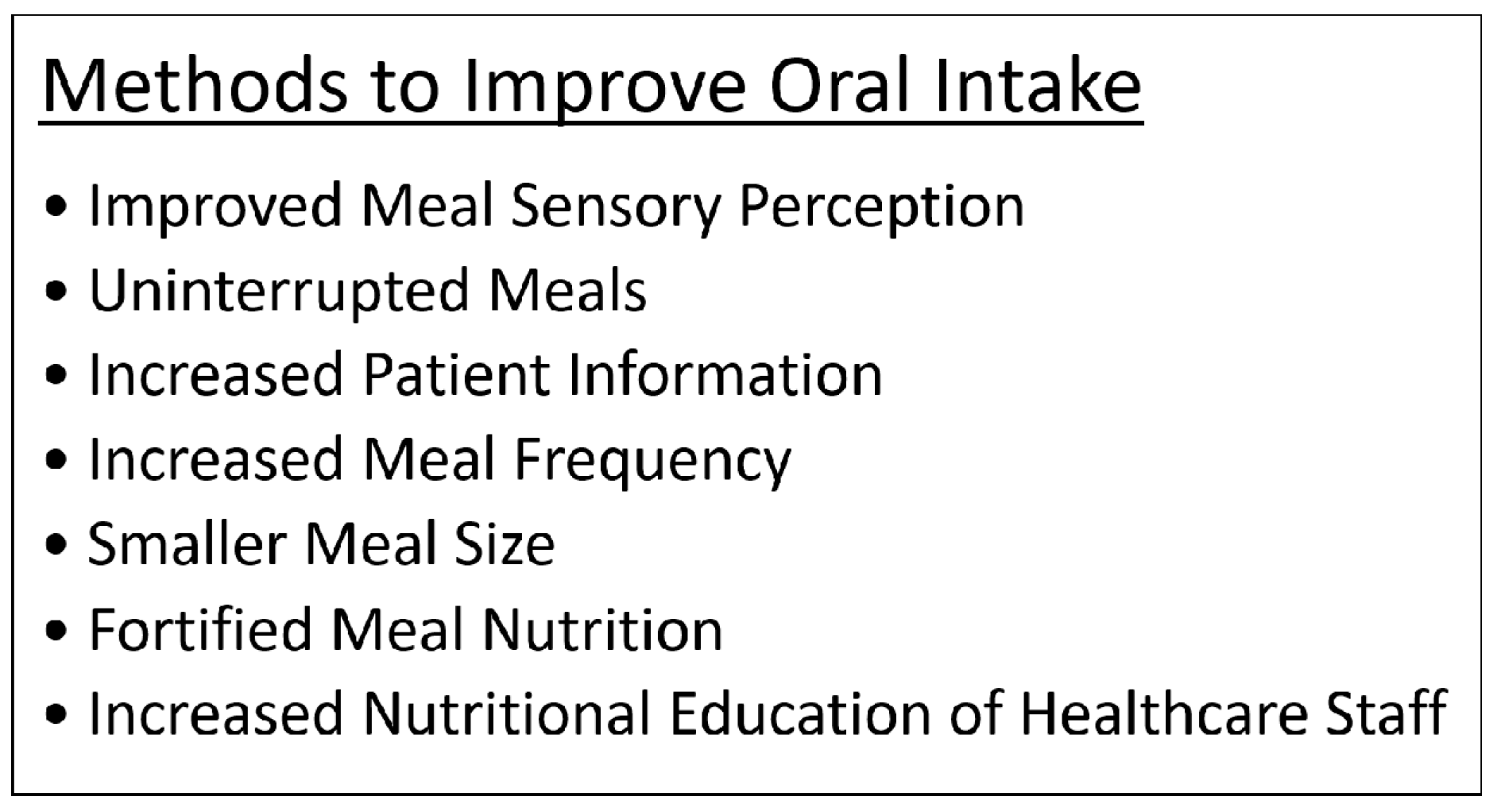
4.2. Techniques to Promote Oral Intake
4.3. Alternative Feeding Methods
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Lim, H.S.; Kim, H.C.; Park, Y.H.; Kim, S.K. Evaluation of Malnutrition Risk after Liver Transplantation Using the Nutritional Screening Tools. Clin. Nutr. Res. 2015, 4, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Marr, K.J.; Shaheen, A.A.; Lam, L.; Stapleton, M.; Burak, K.; Raman, M. Nutritional status and the performance of multiple bedside tools for nutrition assessment among patients waiting for liver transplantation: A Canadian experience. Clin. Nutr. ESPEN 2017, 17, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Maharshi, S.; Sharma, B.C.; Srivastava, S. Malnutrition in cirrhosis increases morbidity and mortality. J. Gastroenterol. Hepatol. 2015, 30, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.; Lee, S.S.; Raman, M. Prevalence and mechanisms of malnutrition in patients with advanced liver disease, and nutrition management strategies. Clin. Gastroenterol. Hepatol. 2012, 10, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, G.R.; Moretti, E.W.; El-Moalem, H.; Clavien, P.A.; Tuttle-Newhall, J.E. Malnutrition in liver transplant patients: Preoperative subjective global assessment is predictive of outcome after liver transplantation. Transplantation 2001, 72, 666–670. [Google Scholar] [CrossRef] [PubMed]
- McClain, C.J. Nutrition in patients with cirrhosis. Gastroenterol. Hepatol. 2016, 12, 507–510. [Google Scholar]
- Alberda, C.; Gramlich, L.; Jones, N.; Jeejeebhoy, K.; Day, A.G.; Dhaliwal, R.; Heyland, D.K. The relationship between nutritional intake and clinical outcomes in critically ill patients: Results of an international multicenter observational study. Intensive Care Med. 2009, 35, 1728–1737. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Yin, W.; Zhang, L.; Xiao, H.; Qi, Y.; Liu, S.; Qian, B.; Wang, F.; Han, T. The value of grip test, lysophosphatidlycholines, glycerophosphocholine, ornithine, glucuronic acid decrement in assessment of nutritional and metabolic characteristics in hepatitis B cirrhosis. PLoS ONE 2017, 12, e0175165. [Google Scholar] [CrossRef] [PubMed]
- Patton, H.M. Nutritional assessment of patients with chronic liver disease. Gastroenterol. Hepatol. 2012, 8, 687–690. [Google Scholar]
- Patel, J.J.; McClain, C.J.; Sarav, M.; Hamilton-Reeves, J.; Hurt, R.T. Protein requirements for critically Ill patients with renal and liver failure. Nutr. Clin. Pract. 2017, 32 (Suppl. 1), 101S–111S. [Google Scholar] [CrossRef] [PubMed]
- Teiusanu, A.; Andrei, M.; Arbanas, T.; Nicolaie, T.; Diculescu, M. Nutritional status in cirrhotic patients. Maedica 2012, 7, 284–289. [Google Scholar] [PubMed]
- Eghtesad, S. Malnutrition in liver cirrhosis: The influence of protein and sodium. Middle East J. Dig. Dis. 2013, 5, 65–75. [Google Scholar] [PubMed]
- Shi, S.; Han, J.; Yan, M.; Wang, K.; Yu, H.; Meng, Q. Nutritional risk assessment in patients with chronic liver disease. Zhonghua Gan Zang Bing Za Zhi 2014, 22, 536–539. [Google Scholar] [PubMed]
- Child, C.G.; Turcotte, J.G. Surgery and portal hypertension. Major Probl. Clin. Surg. 1964, 1, 1–85. [Google Scholar] [PubMed]
- Pugh, R.N.; Murray-Lyon, I.M.; Dawson, J.L.; Pietroni, M.C.; Williams, R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 1973, 60, 646–649. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Hou, C.; Cheng, D.; Tang, W.; Lv, W. Predictive accuracy comparison of MELD and Child-Turcotte-Pugh scores for survival in patients underwent TIPS placement: A systematic meta-analytic review. Int. J. Clin. Exp. Med. 2015, 8, 13464–13472. [Google Scholar] [PubMed]
- Raszeja-Wyszomirska, J.; Wasilewicz, M.P.; Wunsch, E.; Szymanik, B.; Jarosz, K.; Wójcicki, M.; Milkiewicz, P. Assessment of a modified Child-Pugh-Turcotte score to predict early mortality after liver transplantation. Transplant. Proc. 2009, 41, 3114–3116. [Google Scholar] [CrossRef] [PubMed]
- Prijatmoko, D.; Strauss, B.J.; Lambert, J.R.; Sievert, W.; Stroud, D.B.; Wahlqvist, M.L.; Katz, B.; Colman, J.; Jones, P.; Korman, M.G. Early detection of protein depletion in alcoholic cirrhosis: Role of body composition analysis. Gastroenterology 1993, 105, 1839–1845. [Google Scholar] [CrossRef]
- Bharadwaj, S.; Ginoya, S.; Tandon, P.; Gohel, T.D.; Guirguis, J.; Vallabh, H.; Jevenn, A.; Hanouneh, I. Malnutrition: Laboratory markers vs nutritional assessment. Gastroenterol. Rep. 2016, 4, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Tai, M.L.; Goh, K.L.; Mohd-Taib, S.H.; Rampal, S.; Mahadeva, S. Anthropometric, biochemical and clinical assessment of malnutrition in Malaysian patients with advanced cirrhosis. Nutr. J. 2010, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Nunes, F.F.; Bassani, L.; Fernandes, S.A.; Deutrich, M.E.; Pivatto, B.C.; Marroni, C.A. Food consumption of cirrhotic patients, comparison with the nutritional status and disease staging. Arq. Gastroenterol. 2016, 53, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Filipovic, B.F.; Gajic, M.; Milinic, N.; Milovanović, B.; Filipović, B.R.; Cvetković, M.; Sibalić, N. Comparison of two nutritional assessment methods in gastroenterology patients. World J. Gastroenterol. 2010, 16, 1999–2004. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Fink, J.; Daniel de Mello, P.; Daniel de Mello, E. Subjective global assessment of nutritional status—A systematic review of the literature. Clin. Nutr. 2015, 34, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Mourao, F.; Amado, D.; Ravasco, P.; Vidal, P.M.; Camilo, M.E. Nutritional risk and status assessment in surgical patients: A challenge amidst plenty. Nutr. Hosp. 2004, 19, 83–88. [Google Scholar] [PubMed]
- Detsky, A.S.; McLaughlin, J.R.; Baker, J.P.; Johnston, N.; Whittaker, S.; Mendelson, R.A.; Jeejeebhoy, K.N. What is subjective global assessment of nutritional status? JPEN J. Parenter. Enteral Nutr. 1987, 11, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Fuhrman, M.P.; Charney, P.; Mueller, C.M. Hepatic proteins and nutrition assessment. J. Am. Diet. Assoc. 2004, 104, 1258–1264. [Google Scholar] [CrossRef] [PubMed]
- Chaves, G.V.; Peres, W.A.; Goncalves, J.C.; Ramalho, A. Vitamin A and retinol-binding protein deficiency among chronic liver disease patients. Nutrition 2015, 31, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Rand, W.M.; Pellett, P.L.; Young, V.R. Meta-analysis of nitrogen balance studies for estimating protein requirements in healthy adults. Am. J. Clin. Nutr. 2003, 77, 109–127. [Google Scholar] [PubMed]
- Johnson, T.M.; Overgard, E.B.; Cohen, A.E.; DiBaise, J.K. Nutrition assessment and management in advanced liver disease. Nutr. Clin. Pract. 2013, 28, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.; Ney, M.; Irwin, I.; Ma, M.M.; Gramlich, L.; Bain, V.G.; Esfandiari, N.; Baracos, V.; Montano-Loza, A.J.; Myers, R.P. Severe muscle depletion in patients on the liver transplant wait list: Its prevalence and independent prognostic value. Liver Transpl. 2012, 18, 1209–1216. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.; Low, G.; Mourtzakis, M.; Zenith, L.; Myers, R.P.; Abraldes, J.G.; Shaheen, A.A.; Qamar, H.; Mansoor, N.; Carbonneau, M.; et al. A model to identify sarcopenia in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 2016, 14, 1473–1480. [Google Scholar] [CrossRef] [PubMed]
- Ponziani, F.R.; Gasbarrini, A. Sarcopenia in patients with advanced liver disease. Curr. Protein Pept. Sci. 2017. [Google Scholar] [CrossRef] [PubMed]
- Moctezuma-Velazquez, C.; Garcia-Juarez, I.; Soto-Solis, R.; Hernandez-Cortes, J.; Torre, A. Nutritional assessment and treatment of patients with liver cirrhosis. Nutrition 2013, 29, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Verney, J.; Metz, L.; Chaplais, E.; Cardenoux, C.; Pereira, B.; Thivel, D. Bioelectrical impedance is an accurate method to assess body composition in obese but not severely obese adolescents. Nutr. Res. 2016, 36, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.A.; de Mattos, A.A.; Tovo, C.V.; Marroni, C.A. Nutritional evaluation in cirrhosis: Emphasis on the phase angle. World J. Hepatol. 2016, 8, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Merchant, A.T. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr. J. 2008, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Walter-Kroker, A.; Kroker, A.; Mattiucci-Guehlke, M.; Glaab, T. A practical guide to bioelectrical impedance analysis using the example of chronic obstructive pulmonary disease. Nutr. J. 2011, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Kwon, O.; Shin, C.S.; Lee, S.M. Use of bioelectrical impedance analysis for the assessment of nutritional status in critically ill patients. Clin. Nutr. Res. 2015, 4, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Goodpaster, B.H.; Park, S.W.; Harris, T.B.; Kritchevsky, S.B.; Nevitt, M.; Schwartz, A.V.; Simonsick, E.M.; Tylavsky, F.A.; Visser, M.; Newman, A.B. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
- Flood, A.; Chung, A.; Parker, H.; Kearns, V.; O’Sullivan, T.A. The use of hand grip strength as a predictor of nutrition status in hospital patients. Clin. Nutr. 2014, 33, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Rauf, A.; Matin, A.; Agarwal, R.; Tyagi, P.; Arora, A. Handgrip strength as an important bed side tool to assess malnutrition in patient with liver disease. J. Clin. Exp. Hepatol. 2017, 7, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Crawford, P.B.; Obarzanek, E.; Morrison, J.; Sabry, Z.I. Comparative advantage of 3-day food records over 24-h recall and 5-day food frequency validated by observation of 9- and 10-year-old girls. J. Am. Diet. Assoc. 1994, 94, 626–630. [Google Scholar] [CrossRef]
- Yang, Y.J.; Kim, M.K.; Hwang, S.H.; Ahn, Y.; Shim, J.E.; Kim, D.H. Relative validities of 3-day food records and the food frequency questionnaire. Nutr. Res. Pract. 2010, 4, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Ortega, R.M.; Perez-Rodrigo, C.; Lopez-Sobaler, A.M. Dietary assessment methods: Dietary records. Nutr. Hosp. 2015, 31 (Suppl. 3), 38–45. [Google Scholar] [PubMed]
- Rojas-Loureiro, G.; Servin-Caamano, A.; Perez-Reyes, E.; Servin-Abad, L.; Higuera-de la Tijera, F. Malnutrition negatively impacts the quality of life of patients with cirrhosis: An observational study. World J. Hepatol. 2017, 9, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, C.F.; Lai, M. Nutrition interventions for chronic liver diseases and nonalcoholic fatty liver disease. Med. Clin. N. Am. 2016, 100, 1303–1327. [Google Scholar] [CrossRef] [PubMed]
- Kim, W. Treatment options in non-alcoholic fatty liver disease. Korean J. Gastroenterol. 2017, 69, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Chao, A.; Waitzberg, D.; de Jesus, R.P.; Bueno, A.A.; Kha, V.; Allen, K.; Kappus, M.; Medici, V. Malnutrition and nutritional support in alcoholic liver Disease: A review. Curr. Gastroenterol. Rep. 2016, 18, 65. [Google Scholar] [CrossRef] [PubMed]
- Putadechakum, S.; Klangjareonchai, T.; Soponsaritsuk, A.; Roongpisuthipong, C. Nutritional status assessment in cirrhotic patients after protein supplementation. ISRN Gastroenterol. 2012, 2012, 690402. [Google Scholar] [CrossRef] [PubMed]
- Hanai, T.; Shiraki, M.; Nishimura, K.; Ohnishi, S.; Imai, K.; Suetsugu, A.; Takai, K.; Shimizu, M.; Moriwaki, H. Sarcopenia impairs prognosis of patients with liver cirrhosis. Nutrition 2015, 31, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Anastácio, L.R.; Davisson Correia, M.I.T. Nutrition therapy: Integral part of liver transplant care. World J. Gastroenterol. 2016, 22, 1513–1522. [Google Scholar] [CrossRef] [PubMed]
- Thibault, R.; Chikhi, M.; Clerc, A.; Darmon, P.; Chopard, P.; Genton, L.; Kossovsky, M.P.; Pichard, C. Assessment of food intake in hospitalised patients: A 10-year comparative study of a prospective hospital survey. Clin. Nutr. 2011, 30, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Van Bokhorst-de van der Schueren, M.A.; Roosemalen, M.M.; Weijs, P.J.; Langius, J.A. High waste contributes to low food intake in hospitalized patients. Nutr. Clin. Pract. 2012, 27, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Navarro, D.A.; Boaz, M.; Krause, I.; Elis, A.; Chernov, K.; Giabra, M.; Levy, M.; Giboreau, A.; Kosak, S.; Mouhieddine, M.; et al. Improved meal presentation increases food intake and decreases readmission rate in hospitalized patients. Clin. Nutr. 2016, 35, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Holm, L.; Frost, M.B.; Kondrup, J. Food for patients at nutritional risk: A model of food sensory quality to promote intake. Clin. Nutr. 2012, 31, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Forde, C.G.; van Kuijk, N.; Thaler, T.; de Graaf, C.; Martin, N. Texture and savoury taste influences on food intake in a realistic hot lunch time meal. Appetite 2013, 60, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Lorefalt, B.; Wissing, U.; Unosson, M. Smaller but energy and protein-enriched meals improve energy and nutrient intakes in elderly patients. J. Nutr. Health Aging 2005, 9, 243–247. [Google Scholar] [PubMed]
- Poulsen, I.; Vendel Petersen, H.; Rahm Hallberg, I.; Schroll, M. Lack of nutritional and functional effects of nutritional supervision by nurses: A quasi-experimental study in geriatric patients. Scand. J. Food Nutr. 2007, 51, 6–12. [Google Scholar] [CrossRef]
- Campbell, K.L.; Webb, L.; Vivanti, A.; Varghese, P.; Ferguson, M. Comparison of three interventions in the treatment of malnutrition in hospitalised older adults: A clinical trial. Nutr. Diet. 2013, 70, 325–331. [Google Scholar] [CrossRef]
- Kozeniecki, M.; Fritzshall, R. Enteral nutrition for adults in the hospital setting. Nutr. Clin. Pract. 2015, 30, 634–651. [Google Scholar] [CrossRef] [PubMed]
| Nutritional Recommendations for Malnutrition in Cirrhosis | |
| Daily Calories | 35–40 kcal/kg/day |
| Proteins | 1.2–1.5 g/kg/day with increased BCAAs |
| Carbohydrates | 50–70% of daily calories with decreased simple sugars—especially fructose |
| Lipids | 10–20% of daily calories with increased MUFAs and PUFAs |
| Special Considerations | |
| Hepatic Encephalopathy | Maintain protein intake, increase BCAAs and decreased ammonia intake |
| Ascites | Low-sodium diet (≤2 g/day) and water restriction when necessary |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perumpail, B.J.; Li, A.A.; Cholankeril, G.; Kumari, R.; Ahmed, A. Optimizing the Nutritional Support of Adult Patients in the Setting of Cirrhosis. Nutrients 2017, 9, 1114. https://doi.org/10.3390/nu9101114
Perumpail BJ, Li AA, Cholankeril G, Kumari R, Ahmed A. Optimizing the Nutritional Support of Adult Patients in the Setting of Cirrhosis. Nutrients. 2017; 9(10):1114. https://doi.org/10.3390/nu9101114
Chicago/Turabian StylePerumpail, Brandon J., Andrew A. Li, George Cholankeril, Radhika Kumari, and Aijaz Ahmed. 2017. "Optimizing the Nutritional Support of Adult Patients in the Setting of Cirrhosis" Nutrients 9, no. 10: 1114. https://doi.org/10.3390/nu9101114





