Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
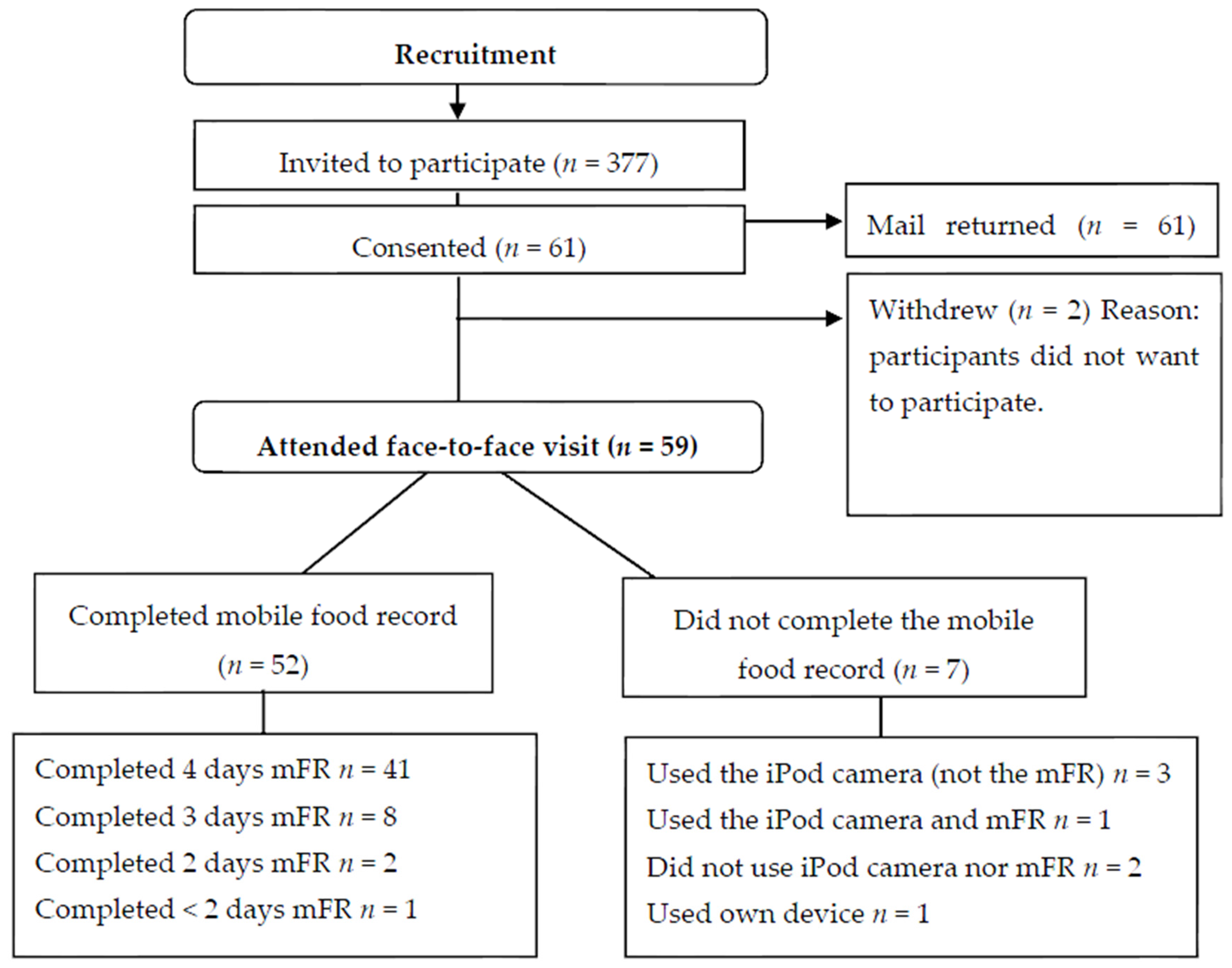
2.2. Participant Recruitment
2.2.1. PANDs Study
2.2.2. CHAT Study
2.3. Data Collection
2.3.1. PANDs Study
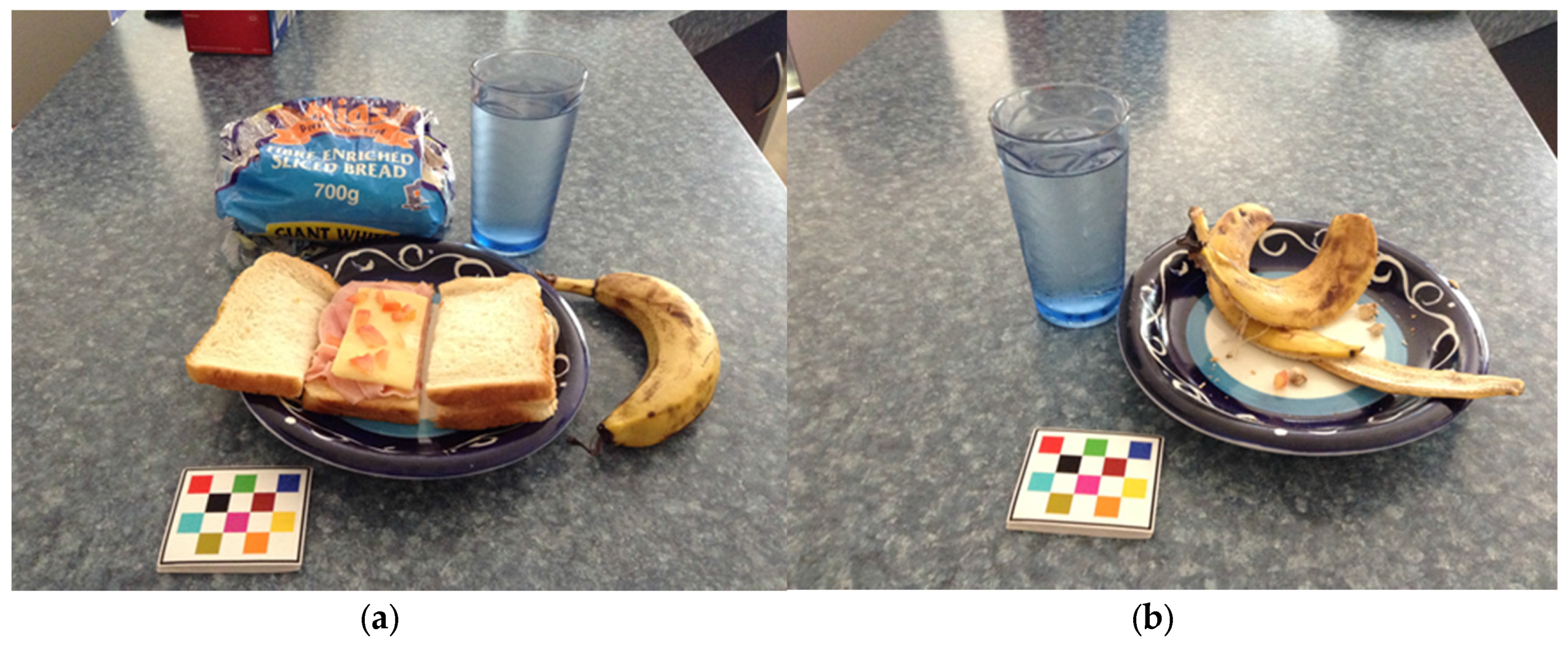
2.3.2. Image Analysis in the PANDs Study
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bourke, J.; de Klerk, N.; Smith, T.; Leonard, H. Population-based prevalence of intellectual disability and autism spectrum disorders in Western Australia: A comparison with previous estimates. Medicine 2016, 95, e3737. [Google Scholar] [CrossRef] [PubMed]
- Roizen, N.J.; Patterson, D. Down’s syndrome. Lancet 2003, 361, 1281–1289. [Google Scholar] [CrossRef]
- Glasson, E.J.; Jacques, A.; Wong, K.; Bourke, J.; Leonard, H. Improved survival in Down syndrome over the last 60 years and the impact of perinatal factors in recent decades. J. Pediatr. 2016, 169, 214–220.e1. [Google Scholar] [CrossRef] [PubMed]
- Humphries, K.; Traci, M.A.; Seekins, T. Nutrition and adults with intellectual or developmental disabilities: Systematic literature review results. Intellect. Dev. Disabil. 2009, 47, 163–185. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Profiles of Health, Australia, 2011–13, Cat. No. 4338.0; Australian Bureau of Statistics: Canberra, Australia, 2013.
- Hsieh, K.; Rimmer, J.H.; Heller, T. Obesity and associated factors in adults with intellectual disability. J. Intellect. Disabil. Res. 2014, 58, 851–863. [Google Scholar] [CrossRef] [PubMed]
- Krause, S.; Ware, R.; McPherson, L.; Lennox, N.; O’Callaghan, M. Obesity in adolescents with intellectual disability: Prevalence and associated characteristics. Obes. Res. Clin. Pract. 2016, 10, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Basil, J.S.; Santoro, S.L.; Martin, L.J.; Healy, K.W.; Chini, B.A.; Saal, H.M. Retrospective study of obesity in children with Down syndrome. J. Pediatr. 2016, 173, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Stancliffe, R.J.; Lakin, K.C.; Larson, S.; Engler, J.; Bershadsky, J.; Taub, S.; Fortune, J.; Ticha, R. Overweight and obesity among adults with intellectual disabilities who use intellectual disability/developmental disability services in 20 U.S. States. Am. J. Intellect. Dev. Disabil. 2011, 116, 401–418. [Google Scholar] [CrossRef] [PubMed]
- Pikora, T.J.; Bourke, J.; Bathgate, K.; Foley, K.R.; Lennox, N.; Leonard, H. Health conditions and their impact among adolescents and young adults with Down syndrome. PLoS ONE 2014, 9, e96868. [Google Scholar] [CrossRef] [PubMed]
- Ptomey, L.T.; Willis, E.A.; Goetz, J.R.; Lee, J.; Sullivan, D.K.; Donnelly, J.E. Digital photography improves estimates of dietary intake in adolescents with intellectual and developmental disabilities. Disabil. Health J. 2015, 8, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Ptomey, L.T.; Herrmann, S.D.; Lee, J.; Sullivan, D.K.; Rondon, M.F.; Donnelly, J.E. Photo-assisted recall increases estimates of energy and macronutrient intake in adults with intellectual and developmental disabilities. J. Acad. Nutr. Diet. 2013, 113, 1704–1709. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulou, M.G.; Manai, A.; Tsigga, M.; Tsiligiroglou-Fachantidou, A.; Galli-Tsinopoulou, A.; Zakas, A. Nutrient intake and anthropometry in children and adolescents with Down syndrome—A preliminary study. Dev. Neurorehabil. 2008, 11, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Fujiura, G.T.; Fitzsimons, N.; Marks, B.; Chicoine, B. Predictors of BMI among adults with Down syndrome: The social context of health promotion. Res. Dev. Disabil. 1997, 18, 261–274. [Google Scholar] [CrossRef]
- Nordstrom, M.; Paus, B.; Andersen, L.F.; Kolset, S.O. Dietary aspects related to health and obesity in Williams syndrome, Down syndrome, and Prader-Willi syndrome. Food Nutr. Res. 2015, 59, 25487. [Google Scholar] [CrossRef] [PubMed]
- Soler Marin, A.; Xandri Graupera, J.M. Nutritional status of intellectual disabled persons with Down syndrome. Nutr. Hosp. 2011, 26, 1059–1066. [Google Scholar] [PubMed]
- Tanis, E.S.; Palmer, S.; Wehmeyer, M.; Davies, D.K.; Stock, S.E.; Lobb, K.; Bishop, B. Self-report computer-based survey of technology use by people with intellectual and developmental disabilities. Intellect. Dev. Disabil. 2012, 50, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Bryen, D.N.; Carey, A.; Friedman, M. Cell phone use by adults with intellectual disabilities. Intellect. Dev. Disabil. 2007, 45, 1–9. [Google Scholar] [CrossRef]
- Stephenson, J.; Limbrick, L. A review of the use of touch-screen mobile devices by people with developmental disabilities. J. Autism Dev. Disord. 2015, 45, 3777–3791. [Google Scholar] [CrossRef] [PubMed]
- Ptomey, L.T.; Sullivan, D.K.; Lee, J.; Goetz, J.R.; Gibson, C.; Donnelly, J.E. The use of technology for delivering a weight loss program for adolescents with intellectual and developmental disabilities. J. Acad. Nutr. Diet. 2015, 115, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Kagohara, D.M.; van der Meer, L.; Ramdoss, S.; O’Reilly, M.F.; Lancioni, G.E.; Davis, T.N.; Rispoli, M.; Lang, R.; Marschik, P.B.; Sutherland, D.; et al. Using iPods(®) and iPads(®) in teaching programs for individuals with developmental disabilities: A systematic review. Res. Dev. Disabil. 2013, 34, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Spoden, M.; Zhu, F.M.; Delp, E.J.; Kerr, D.A. New mobile methods for dietary assessment: Review of image-assisted and image-based dietary assessment methods. Proc. Nutr. Soc. 2016. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Kerr, D.A.; Wright, J.; Lutes, K.D.; Ebert, D.S.; Delp, E.J. Use of technology in children’s dietary assessment. Eur. J. Clin. Nutr. 2009, 63, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- Bosch, M.; Zhu, F.; Khanna, N.; Boushey, C.J.; Delp, E.J. Combining global and local features for food identification in dietary assessment. IEEE Trans. Image Process. 2011, 2011, 1789–1792. [Google Scholar]
- Zhu, F.; Bosch, M.; Khanna, N.; Boushey, C.J.; Delp, E.J. Multiple hypotheses image segmentation and classification with application to dietary assessment. IEEE J. Biomed. Health Inform. 2015, 19, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Bosch, M.; Woo, I.; Kim, S.; Boushey, C.J.; Ebert, D.S.; Delp, E.J. The use of mobile devices in aiding dietary assessment and evaluation. IEEE J. Sel. Top. Signal Process. 2010, 4, 756–766. [Google Scholar] [PubMed]
- Ahmad, Z.; Bosch, M.; Khanna, N.; Kerr, D.A.; Boushey, C.J.; Zhu, F.; Delp, E.J. A mobile food record for integrated dietary assessment. In Proceedings of the 2nd International Workshop on Multimedia Assisted Dietary Management, Amsterdam, The Netherlands, 15–19 October 2016; ACM: Amsterdam, The Netherlands; pp. 53–62.
- Xu, C.; Zhu, F.; Khanna, N.; Boushey, C.J.; Delp, E.J. Image enhancement and quality measures for dietary assessment using mobile devices. Proc. SPIE Int. Soc. Opt. Eng. 2012. [Google Scholar] [CrossRef]
- Aflague, T.F.; Boushey, C.J.; Guerrero, R.T.; Ahmad, Z.; Kerr, D.A.; Delp, E.J. Feasibility and use of the mobile food record for capturing eating occasions among children ages 3–10 years in Guam. Nutrients 2015, 7, 4403–4415. [Google Scholar] [CrossRef] [PubMed]
- Schap, T.E.; Zhu, F.; Delp, E.J.; Boushey, C.J. Merging dietary assessment with the adolescent lifestyle. J. Hum. Nutr. Diet. 2014, 27 (Suppl. S1), 82–88. [Google Scholar] [CrossRef] [PubMed]
- Kerr, D.A.; Harray, A.J.; Pollard, C.M.; Dhaliwal, S.S.; Delp, E.J.; Howat, P.A.; Pickering, M.R.; Ahmad, Z.; Meng, X.; Pratt, I.S.; et al. The connecting health and technology study: A 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- Kerr, D.A.; Pollard, C.M.; Howat, P.; Delp, E.J.; Pickering, M.; Kerr, K.R.; Dhaliwal, S.S.; Pratt, I.S.; Wright, J.; Boushey, C.J. Connecting health and technology (CHAT): Protocol of a randomized controlled trial to improve nutrition behaviours using mobile devices and tailored text messaging in young adults. BMC Public Health 2012, 12, 477. [Google Scholar] [CrossRef] [PubMed]
- Foley, K.R.; Taffe, J.; Bourke, J.; Einfeld, S.L.; Tonge, B.J.; Trollor, J.; Leonard, H. Young people with intellectual disability transitioning to adulthood: Do behaviour trajectories differ in those with and without Down syndrome? PLoS ONE 2016, 11, e0157667. [Google Scholar] [CrossRef] [PubMed]
- Stewart, A.; Marfell-Jones, M.J.; Olds, T.S.; de Ridder, H. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Adelaide, Australia, 2011. [Google Scholar]
- National Health and Medical Research Council; Department of Health and Ageing. Eat for Health: Australian Dietary Guidelines; Providing the Scientific Evidence for Healthier Australian Diets; National Health and Medical Research Council: Canberra, Australia, 2013.
- Casperson, S.L.; Sieling, J.; Moon, J.; Johnson, L.; Roemmich, J.N.; Whigham, L. A mobile phone food record app to digitally capture dietary intake for adolescents in a free-living environment: Usability study. JMIR Mhealth Uhealth 2015, 3, e30. [Google Scholar] [CrossRef] [PubMed]
- Parra, P.; Costa, R.; de Asua, D.R.; Moldenhauer, F.; Suarez, C. Atherosclerotic surrogate markers in adults with Down syndrome: A case-control study. J. Clin. Hypertens. 2017, 19, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Real de Asua, D.; Parra, P.; Costa, R.; Moldenhauer, F.; Suarez, C. A cross-sectional study of the phenotypes of obesity and insulin resistance in adults with Down syndrome. Diabetes Metab. J. 2014, 38, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; Straker, L.M.; Kerr, D.A.; Smith, A.J. Overweight adolescents eat what? And when? Analysis of consumption patterns to guide dietary message development for intervention. J. Hum. Nutr. Diet. 2015, 28 (Suppl. S2), 80–93. [Google Scholar] [CrossRef] [PubMed]
- Leonard, S.; Bower, C.; Petterson, B.; Leonard, H. Survival of infants born with Down’s syndrome: 1980–1996. Paediatr. Perinat. Epidemiol. 2000, 14, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Boushey, C.J.; Harray, A.J.; Kerr, D.A.; Schap, T.E.; Paterson, S.; Aflague, T.; Bosch Ruiz, M.; Ahmad, Z.; Delp, E.J. How willing are adolescents to record their dietary intake? The mobile food record. JMIR Mhealth Uhealth 2015, 3, e47. [Google Scholar] [CrossRef] [PubMed]
- Daugherty, B.L.; Schap, T.E.; Ettienne-Gittens, R.; Zhu, F.M.; Bosch, M.; Delp, E.J.; Ebert, D.S.; Kerr, D.A.; Boushey, C.J. Novel technologies for assessing dietary intake: Evaluating the usability of a mobile telephone food record among adults and adolescents. JMIR 2012, 14, e58. [Google Scholar] [CrossRef] [PubMed]
- Labonte, M.E.; Kirkpatrick, S.I.; Bell, R.C.; Boucher, B.A.; Csizmadi, I.; Koushik, A.; L’Abbe, M.R.; Massarelli, I.; Robson, P.J.; Rondeau, I.; et al. Dietary assessment is a critical element of health research—Perspective from the partnership for advancing nutritional and dietary assessment in Canada. Appl. Physiol. Nutr. Metab. 2016, 41, 1096–1099. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Freedman, L.S.; Tooze, J.A.; Kirkpatrick, S.I.; Boushey, C.; Neuhouser, M.L.; Thompson, F.E.; Potischman, N.; Guenther, P.M.; Tarasuk, V.; et al. Addressing current criticism regarding the value of self-report dietary data. J. Nutr. 2015, 145, 2639–2645. [Google Scholar] [CrossRef] [PubMed]
- Hebert, J.R. Social desirability trait: Biaser or driver of self-reported dietary intake? J. Acad. Nutr. Diet. 2016, 116, 1895–1898. [Google Scholar] [CrossRef] [PubMed]
- Hammer, G.P.; du Prel, J.B.; Blettner, M. Avoiding bias in observational studies: Part 8 in a series of articles on evaluation of scientific publications. Dtsch. Arztebl. Int. 2009, 106, 664–668. [Google Scholar] [PubMed]
| PANDs Study | CHAT Study | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male n = 31 (53%) | Female n = 27 (47%) | Persons 2 n = 58 (100%) | Male n = 82 (34%) | Female n = 162 (66%) | Persons n = 244 (100%) | |||||||
| Characteristics | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Age (year) | 21.7 *** | 4.6 | 21.3 *** | 4.7 | 21.5 *** | 4.6 | 24.7 *** | 3.4 | 24.1 *** | 3.4 | 24.3 *** | 3.4 |
| Height (cm) | 158.0 *** | 6.3 | 145.8 *** | 6.8 | 152.3 *** | 9.0 | 178.3 *** | 7.3 | 165.0 *** | 6.8 | 169.5 *** | 9.4 |
| Weight (kg) | 65.9 *** | 12.7 | 61.3 | 15.5 | 63.8 ** | 14.2 | 78.7 *** | 15.3 | 65.6 | 15.6 | 70.0 ** | 16.7 |
| BMI | 26.4 | 4.7 | 28.6 *** | 6.5 | 27.4 *** | 5.7 | 24.7 | 4.4 | 24.1 *** | 5.8 | 24.3 *** | 5.4 |
| Food group serves | ||||||||||||
| Fruit daily serves (150 g) | 2.3 *** | 1.9 | 2.0 *** | 1.6 | 2.2 *** | 1.8 | 1.1 *** | 1.3 | 0.9 *** | 0.7 | 1.0 *** | 0.9 |
| Vegetable daily serves (75 g) | 2.4 * | 1.5 | 2.4 ** | 1.1 | 2.4 *** | 1.3 | 1.9 * | 1.0 | 1.9 ** | 1.0 | 1.9 *** | 1.0 |
| EDNP 3 daily serves (600 kJ) | 3.2 | 1.7 | 2.4 * | 1.2 | 2.8 | 1.5 | 3.3 | 2.0 | 3.1 * | 1.5 | 3.2 | 1.7 |
| SSB 4 daily serves (600 kJ) | 0.5 | 0.7 | 0.4 | 0.4 | 0.4 | 0.6 | 0.5 | 0.7 | 0.5 | 0.6 | 0.5 | 0.6 |
| PANDs Study (n = 51) | CHAT Study (n = 244) | |||
|---|---|---|---|---|
| N before Images (%) | N after Images (%) | N before Images (%) | N after Images (%) | |
| Fiducial marker present | 692 (90.3%) | 671 (88.9%) | 4768 (96.6%) | 4528 (91.8%) |
| Fiducial marker partially present | 23 (3.0%) | 24 (3.2%) | 12 (0.2%) | 17 (0.3%) |
| Fiducial marker missing | 51 (6.7%) | 58 (7.7%) | 105 (2.1%) | 110 (2.2%) |
| OOPS 1 | 0 | 2 (0.0%) | 50 (1.0%) | 280 (5.7%) |
| Total | 766 (100%) | 755 (100%) 2 | 4935 (100%) | 4935 (100%) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bathgate, K.E.; Sherriff, J.L.; Leonard, H.; Dhaliwal, S.S.; Delp, E.J.; Boushey, C.J.; Kerr, D.A. Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome. Nutrients 2017, 9, 273. https://doi.org/10.3390/nu9030273
Bathgate KE, Sherriff JL, Leonard H, Dhaliwal SS, Delp EJ, Boushey CJ, Kerr DA. Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome. Nutrients. 2017; 9(3):273. https://doi.org/10.3390/nu9030273
Chicago/Turabian StyleBathgate, Katherine E., Jill L. Sherriff, Helen Leonard, Satvinder S. Dhaliwal, Edward J. Delp, Carol J. Boushey, and Deborah A. Kerr. 2017. "Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome" Nutrients 9, no. 3: 273. https://doi.org/10.3390/nu9030273
APA StyleBathgate, K. E., Sherriff, J. L., Leonard, H., Dhaliwal, S. S., Delp, E. J., Boushey, C. J., & Kerr, D. A. (2017). Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome. Nutrients, 9(3), 273. https://doi.org/10.3390/nu9030273





