Analysis of Outcomes of the NRS 2002 in Patients Hospitalized in Nephrology Wards
Abstract
:1. Introduction
2. Materials and Methods
2.1. Nutritional Status
2.2. Statistical Analysis
3. Results
3.1. Nutritional Status
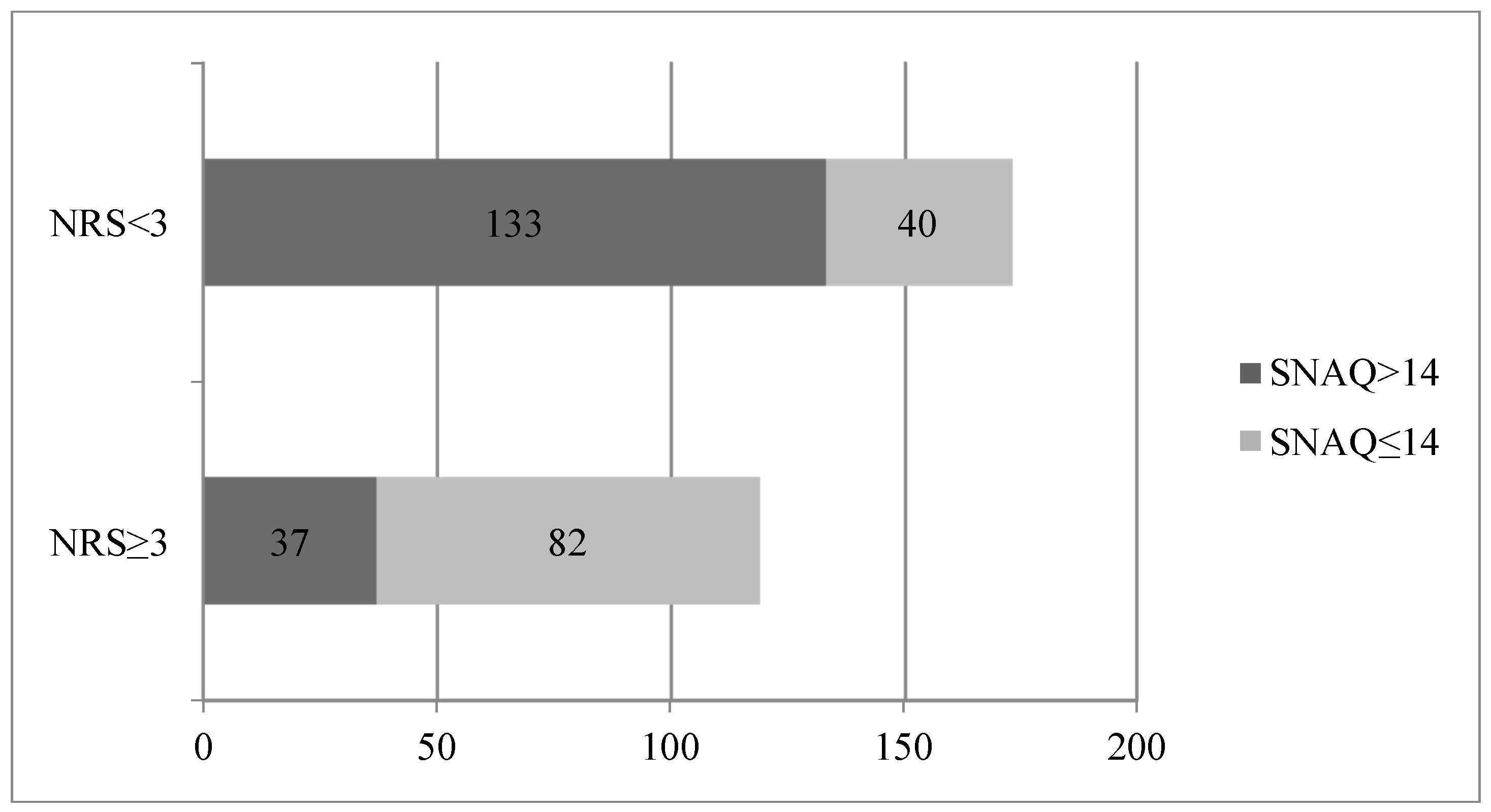
3.2. SNAQ
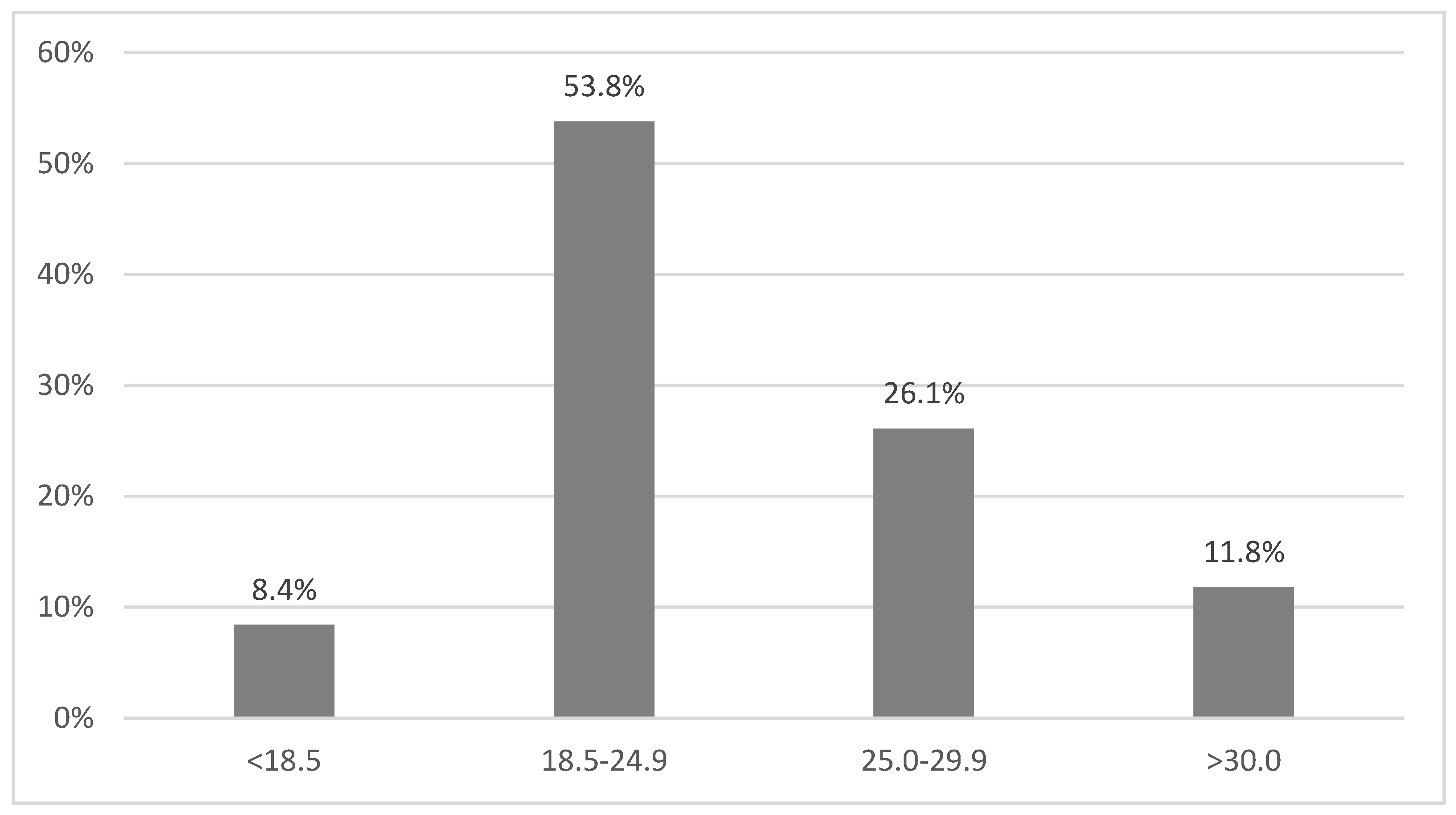
3.3. BMI
3.4. Chronic Kidney Disease (CKD)
4. Discussion
5. Conclusions/Summary
Author Contributions
Conflicts of Interest
References
- Mowe, M.; Bosaeus, I.; Rasmussen, H.H.; Kondrup, J.; Unosson, M.; Rothenberg, E.; Irtun, Ø.; Scandinavian Nutrition Group. Insufficient nutritional knowledge among health care workers? Clin. Nutr. 2008, 27, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, J.; Kondrup, J.; Prokopowicz, J.; Schiesser, M.; Krähenbühl, L.; Meier, R.; Liberda, M.; EuroOOPS Study Group. EuroOOPS: An international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin. Nutr. 2008, 27, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Kondrup, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z.; Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): A new method based on an analysis of controlled clinical trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- McCann, L. Using subjective global assessment to identify malnutrition in the ESRD patient. Nephrol. News Issues 1999, 13, 18–19. [Google Scholar] [PubMed]
- Wilson, M.M.; Thomas, D.R.; Rubenstein, L.Z.; Chibnall, J.T.; Anderson, S.; Baxi, A.; Diebold, M.R.; Morley, J.E. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr. 2005, 82, 1074–1081. [Google Scholar] [PubMed]
- Rasmussen, H.H.; Kondrup, J.; Staun, M.; Ladefoged, K.; Kristensen, H.; Wengler, A. Prevalence of patients at nutritional risk in Danish hospitals. Clin. Nutr. 2004, 23, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Fang, S.; Long, J.; Tan, R.; Lu, W.; Yan, F.; Peng, J. A multicentre assessment of malnutrition, nutritional risk, and application of nutritional support among hospitalized patients in Guangzhou hospitals. Asia Pac. J. Clin. Nutr. 2013, 22, 54–59. [Google Scholar] [PubMed]
- Tangvik, R.J.; Tell, G.S.; Guttormsen, A.B.; Eisman, J.A.; Henriksen, A.; Nilsen, R.M.; Ranhoff, A.H. Nutritional risk profile in a university hospital population. Clin. Nutr. 2015, 34, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Sobotka, L. Podstawy Żywienia Klinicznego; Wydawnictwo Lekarskie PZWL: Warszawa, Poland, 2007; pp. 25–256. [Google Scholar]
- Kondrup, J.; Johansen, N.; Plum, L.M.; Bak, L.; Larsen, I.H.; Martinsen, A.; Andersen, J.R.; Baernthsen, H.; Bunch, E.; Lauesen, N. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin. Nutr. 2002, 21, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Pilgrim, A.L.; Baylis, D.; Jameson, K.A.; Cooper, C.; Sayer, A.A.; Robinson, S.M.; Roberts, H.C. Measuring Appetite with the Simplified Nutritional Appetite Questionnaire Identifies Hospitalised Older People at Risk of Worse Health Outcomes. J. Nutr. Health Aging 2016, 20, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Leistra, E.; Langius, J.A.; Evers, A.M.; van Bokhorst-de van der Schueren, M.A.E.; Visser, M.; de Vet, H.C.; Kruizenga, H.M. Validity of nutritional screening with MUST and SNAQ in hospital outpatients. Eur. J. Clin. Nutr. 2013, 67, 738–742. [Google Scholar] [CrossRef] [PubMed]
- White, J.V.; Guenter, P.; Jensen, G.; Malone, A.; Schofield, M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J. Acad. Nutr. Diet 2012, 112, 730–738. [Google Scholar] [CrossRef] [PubMed]
- Keller, H.H.; Ostbye, T. Nutritional risk and time to death; predictive validity of SCREEN (Seniors in the Community Risk Evaluation for Eating and Nutrition). J. Nutr. Health Aging 2003, 7, 274–279. [Google Scholar] [PubMed]
- McWhirter, J.P.; Pennington, C.R. Incidence and recognition of malnutrition in hospital. BMJ 1994, 308, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Elia, M.; Stratton, R.J. How much undernutrition is there in hospitals? Br. J. Nutr. 2000, 84, 257–259. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Pichard, C.; Lochs, H.; Pirlich, M. Prognostic impact of disease-related malnutrition. Clin. Nutr. 2008, 27, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Waitzberg, D.L.; Caiaffa, W.T.; Correia, M.I. Hospital malnutrition: the Brazilian national survey (IBRANUTRI): A study of 4000 patients. Nutrition 2001, 17, 573–580. [Google Scholar] [CrossRef]
- Małgorzewicz, S.; Dębska-Slizień, A.; Czajka, B.; Rutkowski, B. Adipokines and nutritional status in kidney transplant recipients. Transplant Proc. 2014, 46, 2622–2626. [Google Scholar] [CrossRef] [PubMed]
- Jagielak, D.; Wernio, E.; Kozaryn, R.; Bramlage, P.; Gruchała-Niedoszytko, M.; Rogowski, J.; Małgorzewicz, S. The impact of nutritional status and appetite on the hospital length of stay, and postoperative complications in elderly patients with severe aortic stenosis before aortic valve replacement. Kardiochir. Torakochirurgia Pol. 2016, 13, 105–112. [Google Scholar] [CrossRef]
| Parameters | Total Sample Median (% or IQR or SD) | Nutritional Not at Risk Median (IQR) | At Risk for Malnutrition Median (IQR) |
|---|---|---|---|
| Subjects | 292 | 173 (59.2%) | 119 (40.8%) |
| Sex | |||
| Male | 157 (53.8%) | 93 (53.8%) | 64 (53.8%) |
| Female | 135 (46.2%) | 80 (46.2%) | 55 (46.2%) |
| Age (years) | 60 ± 17.8 | 54 (44–70) * | 73 (49–74) |
| Length of stay (days) | 12.7 (6.0–14.0) | 7 (6–14) * | 13 (8–17) |
| Body weight (kg) | 71.0 ± 18.3 | 75 (60–85) * | 65 (59–84) |
| Serum albumin level (g/L) | 29.4 (23.0–35.0) | 32.5 (25–36) * | 26 (22–33) |
| BMI (kg/m2) | 25.8 ± 5.8 | 25.6 (23–30) * | 23.4 (20–28) |
| Disease | |||
| Diabetes | 87 (30%) | 49 (28%) | 38 (31%) |
| Chronic pulmonary obstructive disease | 13 (4.4%) | 7 (4%) | 6 (5%) |
| Heart failure | 75 (25.7%) | 30 (17%) * | 45 (38%) |
| Coronary heart disease | 129 (44.2%) | 62 (35%) * | 67 (56%) |
| Cancer | 41 (14%) | 17 (10%) * | 24 (20%) |
| Hypertension | 198 (67.1%) | 112 (65%) | 86 (72%) |
| Regression Models | B | Standard Error | Beta | p-Value |
|---|---|---|---|---|
| Model 1 | ||||
| Constant | 9.05 | 0.92 | <0.001 | |
| NRS-2002 | 9.13 | 1.44 | 0.35 | <0.001 |
| Model 2 | ||||
| Constant | 12.7 | 2.87 | <0.001 | |
| NRS-2002 | 11.78 | 1.64 | 0.45 | <0.001 |
| Age | −0.18 | 0.05 | −0.25 | <0.001 |
| CVD | 4.91 | 1.57 | 0.19 | 0.002 |
| CKD | 4.75 | 1.74 | 0.15 | 0.006 |
| The Value of eGFR (mL/min) (4pMDRD) | The Percentage of Patients Diagnosed with Malnutrition |
|---|---|
| >60 | 20% |
| 30–59 | 29.2% |
| 15–29 | 43.3% |
| <15 or the treatment of dialysis | 52.2% |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borek, P.; Chmielewski, M.; Małgorzewicz, S.; Dębska Ślizień, A. Analysis of Outcomes of the NRS 2002 in Patients Hospitalized in Nephrology Wards. Nutrients 2017, 9, 287. https://doi.org/10.3390/nu9030287
Borek P, Chmielewski M, Małgorzewicz S, Dębska Ślizień A. Analysis of Outcomes of the NRS 2002 in Patients Hospitalized in Nephrology Wards. Nutrients. 2017; 9(3):287. https://doi.org/10.3390/nu9030287
Chicago/Turabian StyleBorek, Paulina, Michał Chmielewski, Sylwia Małgorzewicz, and Alicja Dębska Ślizień. 2017. "Analysis of Outcomes of the NRS 2002 in Patients Hospitalized in Nephrology Wards" Nutrients 9, no. 3: 287. https://doi.org/10.3390/nu9030287




