Oral Cyanocobalamin is Effective in the Treatment of Vitamin B12 Deficiency in Crohn’s Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Definition of Terminology
2.2. Study Population
2.3. Therapeutic Regimens
2.4. Statistical Analysis
3. Results
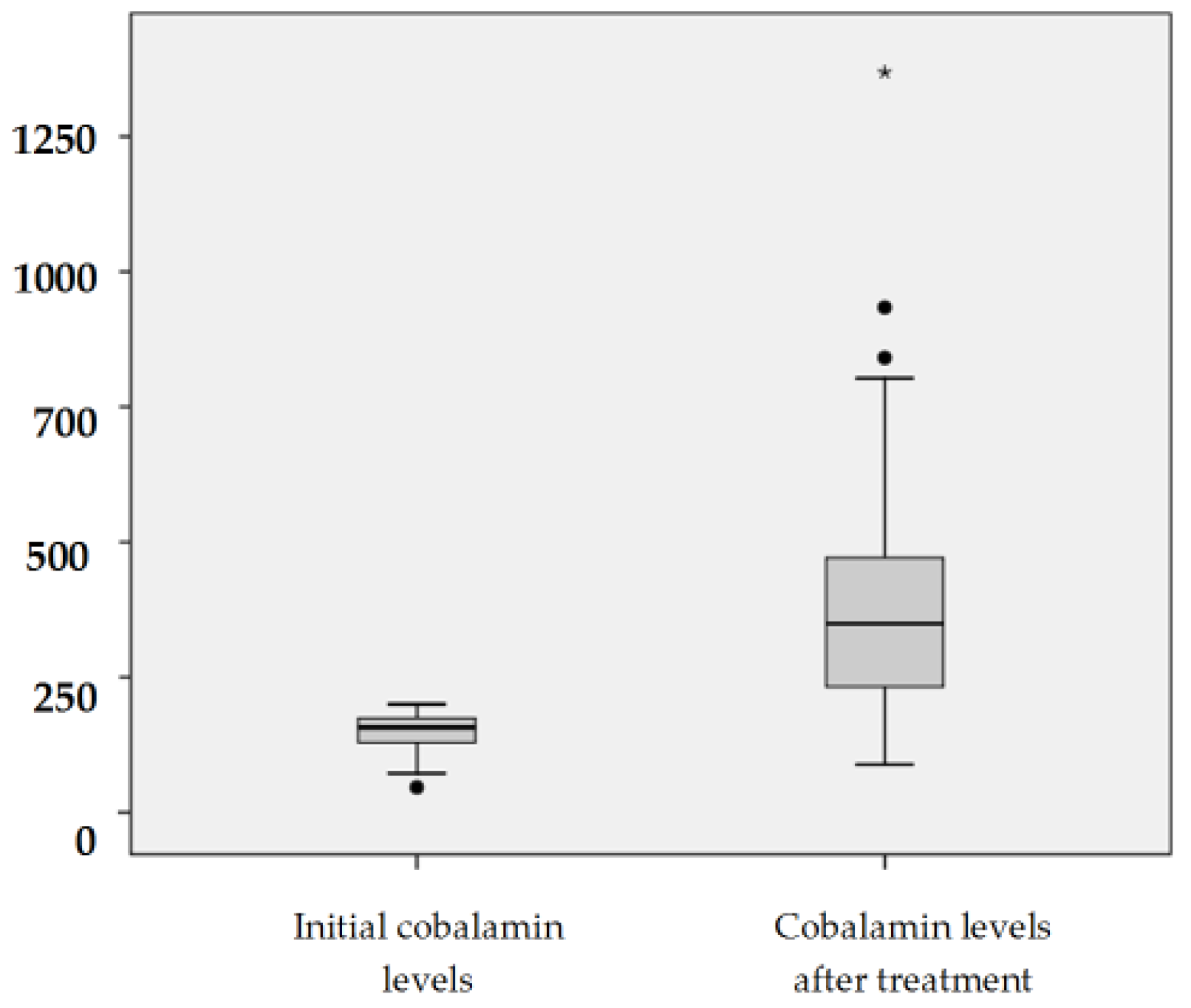
3.1. Effectiveness of Oral Treatment in Vitamin B12 Deficiency
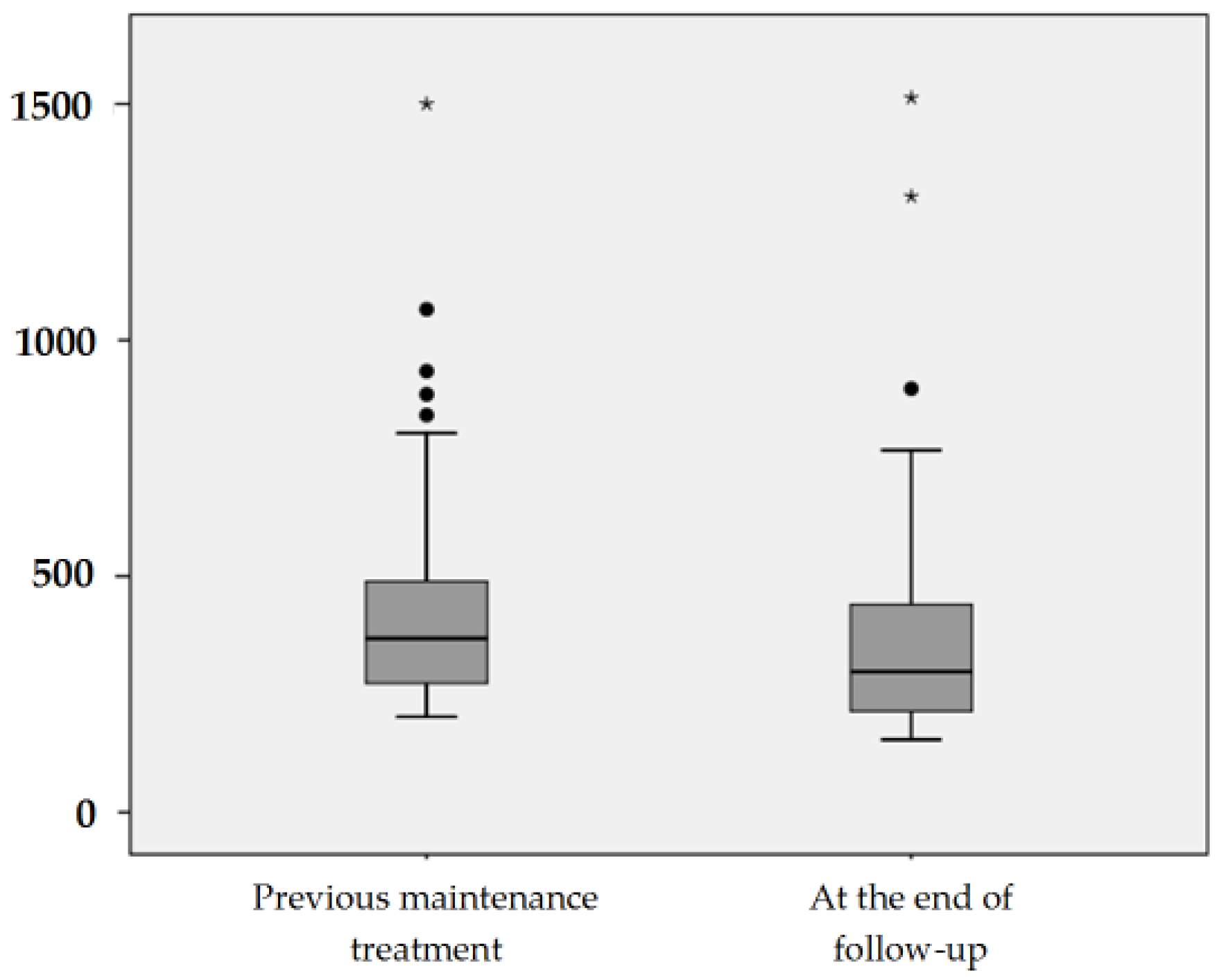
3.2. Effectiveness of Oral Route in Maintenance Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Stabler, S.P. Vitamin B12 deficiency. N. Engl. J. Med. 2013, 368, 2041–2042. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.J.; Rasmussen, M.R.; Andersen, C.B.; Nexø, E.; Moestrup, S.K. Vitamin B12 transport from food to the body’s cells—A sophisticated, multistep pathway. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Andrès, E. Oral cobalamin (vitamin B12) therapy in pernicious anemia. Autoimmun. Rev. 2014, 13, 778. [Google Scholar] [CrossRef] [PubMed]
- Kulnigg, S.; Gasche, C. Systematic review: Managing anaemia in Crohn’s disease. Aliment. Pharmacol. Ther. 2006, 24, 1507–1523. [Google Scholar] [CrossRef] [PubMed]
- Battat, R.; Kopylov, U.; Szilagyi, A.; Saxena, A.; Rosenblatt, D.S.; Warner, M.; Bessissow, T.; Seidman, E.; Bitton, A. Vitamin B12 deficiency in inflammatory bowel disease: Prevalence, risk factors, evaluation, and management. Inflamm. Bowel Dis. 2014, 20, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Headstrom, P.D.; Rulyak, S.J.; Lee, S.D. Prevalence of and risk factors for vitamin B12 deficiency in patients with Crohn’s disease. Inflamm. Bowel Dis. 2008, 14, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Yakut, M.; Ustün, Y.; Kabaçam, G.; Soykan, I. Serum vitamin B12 and folate status in patients with inflammatory bowel diseases. Eur. J. Intern. Med. 2010, 21, 320–323. [Google Scholar] [CrossRef] [PubMed]
- Lambert, D.; Benhayoun, S.; Adjalla, C.; Gelot, M.A.; Renkes, P.; Felden, F.; Gerard, P.; Belleville, F.; Gaucher, P.; Guéant, J.L.; et al. Crohn’s disease and vitamin B12 metabolism. Dig. Dis. Sci. 1996, 41, 1417–1422. [Google Scholar] [CrossRef] [PubMed]
- Dyer, N.H.; Dawson, A.M. Malnutrition and malabsorption in Crohn’s disease with reference to the effect of surgery. Br. J. Surg. 1973, 60, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Sinagra, E.; Tomasello, G.; Raimondo, D.; Rossi, F.; Facella, T.; Damiani, P.; Abruzzo, A.; Bruno, A.; Palumbo, V.D.; Cosentino, L.; et al. Nutrition, malnutrition and dietary interventions in inflammatory bowel disease. Prog. Nutr. 2014, 16, 79–89. [Google Scholar]
- Altomare, R.; Damiano, G.; Abruzzo, A.; Palumbo, V.D.; Tomasello, G.; Buscemi, S.; Lo Monte, A.I. Enteral nutrition support to treat malnutrition in inflammatory bowel disease. Nutrients 2015, 7, 2125–2133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berlin, H.; Berlin, R.; Brante, G. Oral treatment of pernicious anemia with high doses of vitamin B12 without intrinsic factor. Acta Med. Scand. 1968, 184, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Kuzminski, A.M.; del Giacco, E.J.; Allen, R.H.; Stabler, S.P.; Lindenbaum, J. Effective treatment of cobalamin deficiency with oral cobalamin. Blood 1998, 92, 1191–1198. [Google Scholar] [PubMed]
- Bolaman, Z.; Kadikoylu, G.; Yukselen, V.; Yavasoglu, I.; Barutca, S.; Senturk, T. Oral versus intramuscular cobalamin treatment in megaloblastic anemia: A single-center, prospective, randomized, open-label study. Clin. Ther. 2003, 25, 3124–3134. [Google Scholar] [CrossRef]
- Castelli, M.C.; Friedman, K.; Sherry, J.; Brazzillo, K.; Genoble, L.; Bhargava, P.; Riley, M.G. Comparing the efficacy and tolerability of a new daily oral vitamin B12 formulation and intermittent intramuscular vitamin B12 in normalizing low cobalamin levels: A randomized, open-label, parallel-group study. Clin. Ther. 2011, 33, 358–371. [Google Scholar] [CrossRef] [PubMed]
- Lennard-Jones, J.E. Classification of inflammatory bowel disease. Scand. J. Gastroenterol. Suppl. 1989, 170, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, M.S.; Satsangi, J.; Ahmad, T.; Arnott, I.D.; Bernstein, C.N.; Brant, S.R.; Caprilli, R.; Colombel, J.F.; Gasche, C.; Geboes, K.; et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can. J. Gastroenterol. 2005, 19, 5A–36A. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, M.D.; Motta, I. Anemia in Clinical Practice-Definition and Classification: Does Hemoglobin Change With Aging? Semin. Hematol. 2015, 52, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Alaball, J.; Butler, C.C.; Cannings-John, R.; Goringe, A.; Hood, K.; McCaddon, A.; McDowell, I.; Papaioannou, A. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst. Rev. 2005. [Google Scholar] [CrossRef]
- Plener, I.; Ferguson, C.; Kashkooli, S.; Saibil, F. Oral B12 replacement in Crohn’s disease—Is B12 by injection obsolete? Aliment. Pharmacol. Ther. 2014, 40, 1365–1366. [Google Scholar] [CrossRef] [PubMed]
- Mir, A.; Gracia, M.; García-Alvarado, M.; Lue, A.; Muñoz, F.; Garcia-Lopez, S.; Vicente, R.; Gomollon, F. Déficit de Vitamin B12 en la enfermedad de crohn: Tratamiento mediante suplementación oral. XVI Reunión Nacional de la Asociación Española de Gastroenterología. Madr. Spain Marzo 2013, 36, 165–170. [Google Scholar]
- Mir, A.; Gracia, M.; García-Alvarado, M.; Lue, A.; Muñoz, F.; Garcia-Lopez, S.; Vicente, R.; Gomollon, F. Efficacy of oral supplementation in B12 deficiency and maintenance in Crohn’s Disease. In Proceedings of the 8th Congress of ECCO (European Crohn’s and Colitis Organization), Viena, Austria, 14–16 February 2013.
- Nyholm, E.; Turpin, P.; Swain, D.; Cunningham, B.; Daly, S.; Nightingale, P.; Fegan, C. Oral vitamin B12 can change our practice. Postgrad. Med. J. 2003, 79, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.Q.; Low, L.L.; Lee, K.H. Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia. Front. Med. (Lausanne) 2016, 3, 38. [Google Scholar] [CrossRef] [PubMed]
- Kwong, J.C.; Carr, D.; Dhalla, I.A.; Tom-Kun, D.; Upshur, R.E. Oral vitamin B12 therapy in the primary care setting: A qualitative and quantitative study of patient perspectives. BMC Fam. Pract. 2005, 6, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Middleton, J.; Wells, W. Vitamin B12 injections: Considerable source of work for the district nurse. Br. Med. J. (Clin. Res. Ed.) 1985, 290, 1254–1255. [Google Scholar] [CrossRef]
- Van Walraven, C.; Austin, P.; Naylor, C.D. Vitamin B12 injections versus oral supplements. How much money could be saved by switching from injections to pills? Can. Fam. Physician 2001, 47, 79–86. [Google Scholar] [PubMed]
- Gomollón, F. Treatment adherence is always worse than we think: An unresolved problem in inflammatory bowel disease. Gastroenterol. Hepatol. 2016, 39, 14–19. [Google Scholar] [CrossRef]
- Eussen, S.J.; de Groot, L.C.; Clarke, R.; Schneede, J.; Ueland, P.M.; Hoefnagels, W.H.; van Staveren, W.A. Oral cyanocobalamin supplementation in older people with vitamin B12 deficiency: A dose-finding trial. Arch. Intern. Med. 2005, 165, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Lederle, F.A. Oral cobalamin for pernicious anemia. Medicine’s best kept secret? JAMA 1991, 265, 94–95. [Google Scholar] [CrossRef] [PubMed]
| Patients Demographics | Overall Study Population (94 Patients) n (%) | Cohort B12 Deficiency Treatment (76 Patients) n (%) | Cohort Maintenance Treatment (82 Patients) n (%) |
|---|---|---|---|
| Sex (male) | 52 (55.3) | 42 (55.3) | 45 (54.9) |
| Age (years) | |||
| Mean ± standard deviation | 45 ± 13 | 45 ± 13 | 44 ± 13 |
| Median, interquartile range | 43, 35–53 | 42, 35–54 | 44, 35–53 |
| Tobacco | |||
| Active smokers | 27 (28.7) | 21 (27.6) | 25 (30.5) |
| Non-active smokers | 67 (71.3) | 55 (72.4) | 57 (69.5) |
| Montreal Classification | |||
| A1 | 4 (4.3) | 2 (2.6) | 4 (4.9) |
| A2 | 65 (69.1) | 52 (68.4) | 56 (68.3) |
| A3 | 25 (26.6) | 22 (28.9) | 22 (26.8) |
| L1 | 45 (47.9) | 37 (48.7) | 40 (48.8) |
| L2 | 4 (4.2) | 4 (5.3) | 3 (3.7) |
| L3 | 45 (47.9) | 35 (46.0) | 39 (47.5) |
| B1 | 36 (38.3) | 29 (38.1) | 31 (37.8) |
| B2 | 41 (43.6) | 35 (46.1) | 35 (42.7) |
| B3 | 17 (18.1) | 12 (15.8) | 16 (19.5) |
| Perineal disease | 11 (11.7) | 2 (2.6) | 11 (13.4) |
| Upper gastrointestinal disease | 2 (1.88) | 1 (1.31) | 2 (2.43) |
| Ileal resection | 24 (25.5) | 21 (27.6) | 21 (25.6) |
| Brand Name | Qualitative and Quantitative Composition | Dosage | Patients n |
|---|---|---|---|
| BENEXOL© | B12 1 mg, B6 250 mg, B1 250 mg | 1 tablet/24 h | 38 |
| 1 tablet/12 h | 6 | ||
| 1 tablet/8 h | 3 | ||
| FOLIDOCE© | B12 0.002 mg, folic acid 0.4 mg | 1 tablet/12 h | 2 |
| HIDROXIL© | B12 0.5 mg, B6 250 mg, B1 250 mg | 1 tablet/24 h | 1 |
| NEURODAVUR© | B12 2.5 mg, B6 250 mg, B1 250 mg | 1 tablet/24 h | 3 |
| NEUROMADE© | B12 1 mg, B6 50 mg, B1 50 mg | 1 tablet/24 h | 6 |
| OPTOVITE© | B12 1 mg | 1 ampule/24 h | 9 |
| 2 ampule/7 days | 8 |
| Brand Name | Qualitative and Quantitative Composition | Dosage | Patients n |
|---|---|---|---|
| BENEXOL© | B12 1 mg, B6 250 mg, B1 250 mg | 1 tablet/24 h | 22 |
| 1 tablet/48 h | 1 | ||
| 2 tablet/7 days | 17 | ||
| FOLIDOCE© | B12 0.002 mg, folic acid 0.4 mg | 1 tablet/12 h | 2 |
| NEURODAVUR© | B12 2.5 mg, B6 250 mg, B1 250 mg | 1 tablet/24 h | 8 |
| NEUROMADE© | B12 1 mg, B6 50 mg, B1 50 mg | 1 tablet/24 h | 9 |
| OPTOVITE© | B12 1 mg | 2 ampule/7 days | 23 |
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 |
| Before | 46 | 72 | 79 | 86 | 90 | 104 | 104 | 105 | 111 | 116 | 117 | 118 | 119 | 119 | 119 | 121 | 128 | 128 | 129 | 135 | 136 | 137 | 137 | 139 | 139 | 139 | 141 | 142 | 151 | 152 | 153 | 153 | 155 | 156 | 156 | 156 | 157 | 157 |
| After | 177 | 229 | 554 | 333 | 464 | 488 | 273 | 232 | 202 | 230 | 202 | 1369 | 622 | 375 | 233 | 446 | 222 | 247 | 452 | 402 | 367 | 313 | 436 | 305 | 251 | 394 | 219 | 203 | 198 | 779 | 187 | 294 | 627 | 204 | 228 | 360 | 803 | 562 |
| Patient | 39 | 40 | 41 | 42 | 43 | 44 | 45 | 46 | 47 | 48 | 49 | 50 | 51 | 52 | 53 | 54 | 55 | 56 | 57 | 58 | 59 | 60 | 61 | 62 | 63 | 64 | 65 | 66 | 67 | 68 | 69 | 70 | 71 | 72 | 73 | 74 | 75 | 76 |
| Before | 157 | 159 | 159 | 161 | 163 | 164 | 165 | 166 | 168 | 169 | 170 | 170 | 170 | 171 | 173 | 173 | 173 | 174 | 174 | 175 | 175 | 176 | 177 | 181 | 184 | 186 | 192 | 193 | 196 | 199 | 200 | 200 | 200 | 200 | 200 | 200 | 200 | 200 |
| After | 216 | 321 | 223 | 350 | 360 | 391 | 934 | 296 | 471 | 294 | 349 | 841 | 402 | 478 | 497 | 182 | 286 | 623 | 478 | 761 | 246 | 507 | 252 | 238 | 218 | 296 | 359 | 380 | 337 | 411 | 380 | 259 | 660 | 744 | 430 | 373 | 287 | 647 |
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | 40 | 41 |
| Beginning | 202 | 202 | 202 | 204 | 214 | 216 | 218 | 222 | 223 | 228 | 229 | 230 | 232 | 238 | 244 | 246 | 247 | 251 | 252 | 259 | 273 | 286 | 287 | 294 | 294 | 296 | 296 | 304 | 305 | 305 | 313 | 321 | 337 | 338 | 349 | 350 | 359 | 360 | 360 | 364 | 367 |
| End | 168 | 255 | 155 | 271 | 214 | 422 | 211 | 295 | 310 | 193 | 201 | 224 | 289 | 491 | 288 | 209 | 413 | 263 | 176 | 174 | 303 | 279 | 287 | 294 | 194 | 463 | 372 | 359 | 233 | 166 | 186 | 176 | 283 | 316 | 454 | 293 | 359 | 468 | 270 | 364 | 215 |
| Patient | 42 | 43 | 44 | 45 | 46 | 47 | 48 | 49 | 50 | 51 | 52 | 53 | 54 | 55 | 56 | 57 | 58 | 59 | 60 | 61 | 62 | 63 | 65 | 66 | 67 | 68 | 69 | 70 | 71 | 72 | 73 | 74 | 75 | 76 | 77 | 78 | 79 | 80 | 81 | 82 | |
| Beginning | 369 | 371 | 373 | 375 | 380 | 380 | 389 | 391 | 394 | 402 | 411 | 430 | 432 | 436 | 446 | 452 | 464 | 471 | 478 | 488 | 489 | 497 | 532 | 554 | 560 | 587 | 622 | 623 | 645 | 647 | 660 | 695 | 744 | 761 | 803 | 841 | 885 | 934 | 1065 | 1500 | |
| End | 897 | 173 | 177 | 214 | 302 | 239 | 290 | 154 | 354 | 409 | 600 | 524 | 387 | 496 | 1304 | 177 | 239 | 229 | 365 | 709 | 398 | 460 | 167 | 535 | 496 | 413 | 416 | 391 | 494 | 729 | 440 | 522 | 328 | 351 | 1513 | 167 | 214 | 616 | 217 | 767 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomollón, F.; Gargallo, C.J.; Muñoz, J.F.; Vicente, R.; Lue, A.; Mir, A.; García-Alvarado, M.; Gracia, M.; García-López, S. Oral Cyanocobalamin is Effective in the Treatment of Vitamin B12 Deficiency in Crohn’s Disease. Nutrients 2017, 9, 308. https://doi.org/10.3390/nu9030308
Gomollón F, Gargallo CJ, Muñoz JF, Vicente R, Lue A, Mir A, García-Alvarado M, Gracia M, García-López S. Oral Cyanocobalamin is Effective in the Treatment of Vitamin B12 Deficiency in Crohn’s Disease. Nutrients. 2017; 9(3):308. https://doi.org/10.3390/nu9030308
Chicago/Turabian StyleGomollón, Fernando, Carla J. Gargallo, Jose Fernando Muñoz, Raquel Vicente, Alberto Lue, Alberto Mir, Marta García-Alvarado, Marta Gracia, and Santiago García-López. 2017. "Oral Cyanocobalamin is Effective in the Treatment of Vitamin B12 Deficiency in Crohn’s Disease" Nutrients 9, no. 3: 308. https://doi.org/10.3390/nu9030308





