Engineering Botulinum Toxins to Improve and Expand Targeting and SNARE Cleavage Activity
Abstract
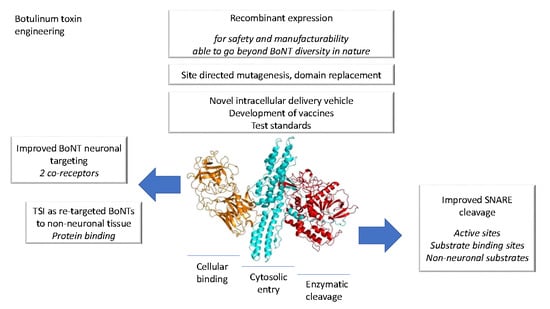
:1. Botulinum Toxin Background
2. Recombinant Production and Manufacture
3. BoNT Targeting
4. BoNT Re-Targeting
5. SNARE Cleavage Activity
6. Conclusions
Acknowledgments
Conflicts of Interest
References
- Dressler, D. Botulinum toxin drugs: Brief history and outlook. J. Neural Transm. 2016, 123, 277–279. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J. Botulinum toxin: State of the art. Mov. Disord. 2017, 32, 1131–1138. [Google Scholar] [CrossRef] [PubMed]
- Jabbari, B. History of botulinum toxin treatment in movement disorders. Tremor Other Hyperkinet. Mov. 2016, 6, 394. [Google Scholar]
- Grand View Research Inc. Botulinum Toxin Market Analysis by Type (Botulinum Toxin Type A; Botulinum Toxin Type B); by End Use (Therapeutic; Aesthetic); by Region (North America; Europe; Asia Pacific; Latin America; MEA); and Segment Forecasts; 2013–2025; Market Research Report 2017, Report ID GVR-1-68038-355-3; Grand View Research Inc.: San Francisco, CA, USA, 2017. [Google Scholar]
- Fonfria, E.; Maignel, J.; Lezmi, S.; Martin, V.; Splevins, A.; Shubber, S.; Kalinichev, M.; Foster, K.; Picaut, P.; Krupp, J. The expanding therapeutic utility of botulinum neurotoxins. Toxins 2018, 10, 208. [Google Scholar] [CrossRef] [PubMed]
- Dover, N.; Barash, J.R.; Hill, K.K.; Xie, G.; Arnon, S.S. Molecular characterization of a novel botulinum neurotoxin type h gene. J. Infect. Dis. 2014, 209, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Lebreton, F.; Mansfield, M.J.; Miyashita, S.I.; Zhang, J.; Schwartzman, J.A.; Tao, L.; Masuyer, G.; Martinez-Carranza, M.; Stenmark, P.; et al. Identification of a botulinum neurotoxin-like toxin in a commensal strain of enterococcus faecium. Cell Host Microbe 2018, 23, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A. The long journey of botulinum neurotoxins into the synapse. Toxicon 2015, 107, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.W.; Smith, T.J.; Anniballi, F.; Austin, J.W.; Bano, L.; Bradshaw, M.; Cuervo, P.; Cheng, L.W.; Derman, Y.; Dorner, B.G.; et al. Historical perspectives and guidelines for botulinum neurotoxin subtype nomenclature. Toxins 2017, 9, 38. [Google Scholar] [CrossRef] [PubMed]
- Kammerer, R.A.; Benoit, R.M. Botulinum neurotoxins: New questions arising from structural biology. Trends Biochem. Sci. 2014, 39, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Swaminathan, S. Neurotoxin structure. In Molecular Aspects of Botulinum Neurotoxin; Springer: Berlin, Germany, 2014; pp. 103–127. [Google Scholar]
- Montal, M. Botulinum neurotoxin: A marvel of protein design. Annu. Rev. Biochem. 2010, 79, 591–617. [Google Scholar] [CrossRef] [PubMed]
- Foster, K.A. Overview and history of botulinum neurotoxin clinical exploitation. In Clinical Applications of Botulinum Neurotoxin; Springer: Berlin, Germany, 2014; pp. 1–5. [Google Scholar]
- Fonfria, E. Botulinum neurotoxin: A multifunctional protein for the development of new therapeutics. In Neurotoxins; McDuffie, J.E., Ed.; InTechOpen: London, UK, 2018. [Google Scholar]
- Laing, T.; Laing, M.; O’Sullivan, S. Botulinum toxin for treatment of glandular hypersecretory disorders. J. Plast. Reconstr. Aesthet. Surg. 2008, 61, 1024–1028. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Dhaliwal, H.P.; Kukreja, R.V.; Singh, B.R. The Botulinum Toxin as a therapeutic agent: Molecular structure and mechanism of action in motor and sensory systems. In Seminars in Neurology; Thieme Medical Publishers: Stuttgart, Germany, 2016. [Google Scholar]
- Grando, S.; Zachary, C. The non-neuronal and non-muscular effects of botulinum toxin: A graceful opportunity for a deadly molecule to treat a human disease in the skin and beyond. Br. J. Dermatol. 2017, 178, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Weisemann, J.; Krez, N.; Fiebig, U.; Worbs, S.; Skiba, M.; Endermann, T.; Dorner, M.B.; Bergström, T.; Muñoz, A.; Zegers, I. Generation and characterization of six recombinant botulinum neurotoxins as reference material to serve in an international proficiency test. Toxins 2015, 7, 5035–5054. [Google Scholar] [CrossRef] [PubMed]
- Chaddock, J. Future developments: Engineering the neurotoxin. In Clinical Applications of Botulinum Neurotoxin; Springer: Berlin, Germany, 2014; pp. 177–192. [Google Scholar]
- Pickett, A. Botulinum toxin as a clinical product: Manufacture and pharmacology. In Clinical Applications of Botulinum Neurotoxin; Foster, K., Ed.; Springer: Berlin, Germany, 2014; pp. 7–49. [Google Scholar]
- Wortzman, M.S.; Pickett, A. The science and manufacturing behind botulinum neurotoxin type A-ABO in clinical use. Aesthet. Surg. J. 2009, 29, S34–S42. [Google Scholar] [CrossRef] [PubMed]
- Pirazzini, M.; Rossetto, O.; Eleopra, R.; Montecucco, C. Botulinum neurotoxins: Biology, pharmacology, and toxicology. Pharmacol. Rev. 2017, 69, 200–235. [Google Scholar] [CrossRef] [PubMed]
- Tobin, P.H.; Richards, D.H.; Callender, R.A.; Wilson, C.J. Protein engineering: A new frontier for biological therapeutics. Curr. Drug Metab. 2014, 15, 743–756. [Google Scholar] [CrossRef] [PubMed]
- Byrne, M.P.; Smith, T.J.; Montgomery, V.A.; Smith, L.A. Purification, potency, and efficacy of the botulinum neurotoxin type a binding domain from pichia pastoris as a recombinant vaccine candidate. Infect. Immun. 1998, 66, 4817–4822. [Google Scholar] [PubMed]
- O’Flaherty, S.; Klaenhammer, T.R. Multivalent chromosomal expression of the clostridium botulinum serotype a neurotoxin heavy-chain antigen and the bacillus anthracis protective antigen in lactobacillus acidophilus. Appl. Environ. Microbiol. 2016, 82, 6091–6101. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, M.; Tepp, W.H.; Whitemarsh, R.C.; Pellett, S.; Johnson, E.A. Holotoxin activity of botulinum neurotoxin subtype A4 originating from a nontoxigenic clostridium botulinum expression system. Appl. Environ. Microbiol. 2014, 80, 7415–7422. [Google Scholar] [CrossRef] [PubMed]
- Pellett, S.; Tepp, W.H.; Bradshaw, M.; Kalb, S.R.; Dykes, J.K.; Lin, G.; Nawrocki, E.M.; Pier, C.L.; Barr, J.R.; Maslanka, S.E.; et al. Purification and characterization of botulinum neurotoxin fa from a genetically modified clostridium botulinum strain. mSphere 2016, 1, e00100-15. [Google Scholar] [CrossRef] [PubMed]
- Blum, F.C.; Przedpelski, A.; Tepp, W.H.; Johnson, E.A.; Barbieri, J.T. Entry of a recombinant, full-length, atoxic tetanus neurotoxin into neuro-2a cells. Infect. Immun. 2014, 82, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, E.; Gu, C.; Niranjan, D.; Restani, L.; Rasetti-Escargueil, C.; Obara, I.; Geranton, S.M.; Arsenault, J.; Goetze, T.A.; Harper, C.B. Synthetic self-assembling clostridial chimera for modulation of sensory functions. Bioconjug. Chem. 2013, 24, 1750–1759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.; Masuyer, G.; Zhang, J.; Shen, Y.; Lundin, D.; Henriksson, L.; Miyashita, S.-I.; Martínez-Carranza, M.; Dong, M.; Stenmark, P. Identification and characterization of a novel botulinum neurotoxin. Nat. Commun. 2017, 8, 14130. [Google Scholar] [CrossRef] [PubMed]
- Nugent, M.; Wang, J.; Lawrence, G.; Zurawski, T.; Geoghegan, J.A.; Dolly, J.O. Conjugate of an IgG binding domain with botulinum neurotoxin a lacking the acceptor moiety targets its SNARE protease into TrkA-expressing cells when coupled to anti-TrkA IgG or Fc-βNGF. Bioconjug. Chem. 2017, 28, 1684–1692. [Google Scholar] [CrossRef] [PubMed]
- Mangione, A.S.; Obara, I.; Maiaru, M.; Geranton, S.M.; Tassorelli, C.; Ferrari, E.; Leese, C.; Davletov, B.; Hunt, S.P. Nonparalytic botulinum molecules for the control of pain. Pain 2016, 157, 1045–1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bade, S.; Rummel, A.; Reisinger, C.; Karnath, T.; Ahnert-Hilger, G.; Bigalke, H.; Binz, T. Botulinum neurotoxin type D enables cytosolic delivery of enzymatically active cargo proteins to neurones via unfolded translocation intermediates. J. Neurochem. 2004, 91, 1461–1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.; Casals-Diaz, L.; Zurawski, T.; Meng, J.; Moriarty, O.; Nealon, J.; Edupuganti, O.P.; Dolly, O. A novel therapeutic with two SNAP-25 inactivating proteases shows long-lasting anti-hyperalgesic activity in a rat model of neuropathic pain. Neuropharmacology 2017, 118, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Höltje, M.; Schulze, S.; Strotmeier, J.; Mahrhold, S.; Richter, K.; Binz, T.; Bigalke, H.; Ahnert-Hilger, G.; Rummel, A. Exchanging the minimal cell binding fragments of tetanus neurotoxin in botulinum neurotoxin A and B impacts their toxicity at the neuromuscular junction and central neurons. Toxicon 2013, 75, 108–121. [Google Scholar] [CrossRef] [PubMed]
- Meng, J.; Ovsepian, S.V.; Wang, J.; Pickering, M.; Sasse, A.; Aoki, K.R.; Lawrence, G.W.; Dolly, J.O. Activation of TRPV1 mediates calcitonin gene-related peptide release, which excites trigeminal sensory neurons and is attenuated by a retargeted botulinum toxin with anti-nociceptive potential. J. Neurosci. 2009, 29, 4981–4992. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zurawski, T.H.; Meng, J.; Lawrence, G.; Olango, W.M.; Finn, D.P.; Wheeler, L.; Dolly, J.O. A dileucine in the protease of botulinum toxin a underlies its long-lived neuroparalysis: Transfer of longevity to a novel potential therapeutic. J. Biol. Chem. 2011, 286, 6375–6385. [Google Scholar] [CrossRef] [PubMed]
- Rosano, G.L.; Ceccarelli, E.A. Recombinant protein expression in Escherichia coli: Advances and challenges. Front. Microbiol. 2014, 5, 172. [Google Scholar] [CrossRef] [PubMed]
- Somm, E.; Bonnet, N.; Martinez, A.; Marks, P.M.; Cadd, V.A.; Elliott, M.; Toulotte, A.; Ferrari, S.L.; Rizzoli, R.; Hüppi, P.S. A botulinum toxin–derived targeted secretion inhibitor downregulates the GH/IGF1 axis. J. Clin. Investig. 2012, 122, 3295–3306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webb, R.P.; Smith, L.A. What next for botulism vaccine development? Expert Rev. Vaccines 2013, 12, 481–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundeen, G.; Barbieri, J.T. Vaccines against botulism. Toxins 2017, 9, 268. [Google Scholar] [CrossRef] [PubMed]
- Doxey, A.C.; Mansfield, M.J.; Montecucco, C. Discovery of novel bacterial toxins by genomics and computational biology. Toxicon 2018, 147, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Moreira, G.; Cunha, C.; Salvarani, F.; Gonçalves, L.; Pires, P.; Conceição, F.; Lobato, F. Production of recombinant botulism antigens: A review of expression systems. Anaerobe 2014, 28, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Moreira, G.M.; Moreira, C., Jr.; da Cunha, C.E.; Mendonca, M.; Conceicao, F.R. Recombinant botulinum toxoids: A practical guide for production. Methods Mol. Biol. 2016, 1404, 621–632. [Google Scholar] [PubMed]
- Galloux, M.; Vitrac, H.; Montagner, C.; Raffestin, S.; Popoff, M.R.; Chenal, A.; Forge, V.; Gillet, D. Membrane interaction of botulinum neurotoxin a translocation (T) domain the belt region is a regulatory loop for membrane interaction. J. Biol. Chem. 2008, 283, 27668–27676. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Gu, S.; Jin, L.; Le, T.T.N.; Cheng, L.W.; Strotmeier, J.; Kruel, A.M.; Yao, G.; Perry, K.; Rummel, A. Structure of a bimodular botulinum neurotoxin complex provides insights into its oral toxicity. PLoS Pathog. 2013, 9, e1003690. [Google Scholar] [CrossRef] [PubMed]
- Montecucco, C. How do tetanus and botulinum toxins bind to neuronal membranes? Trends Biochem. Sci. 1986, 11, 314–317. [Google Scholar] [CrossRef]
- Binz, T.; Rummel, A. Cell entry strategy of clostridial neurotoxins. J. Neurochem. 2009, 109, 1584–1595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishiki, T.-I.; Kamata, Y.; Nemoto, Y.; Omori, A.; Ito, T.; Takahashi, M.; Kozaki, S. Identification of protein receptor for clostridium botulinum type B neurotoxin in rat brain synaptosomes. J. Biol. Chem. 1994, 269, 10498–10503. [Google Scholar] [PubMed]
- Dong, M.; Richards, D.A.; Goodnough, M.C.; Tepp, W.H.; Johnson, E.A.; Chapman, E.R. Synaptotagmins I and II mediate entry of botulinum neurotoxin B into cells. J. Cell Biol. 2003, 162, 1293–1303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berntsson, R.P.-A.; Peng, L.; Svensson, L.M.; Dong, M.; Stenmark, P. Crystal structures of botulinum neurotoxin DC in complex with its protein receptors synaptotagmin I and II. Structure 2013, 21, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, O.; Pirazzini, M.; Montecucco, C. Botulinum neurotoxins: Genetic, structural and mechanistic insights. Nat. Rev. Microbiol. 2014, 12, 535–549. [Google Scholar] [CrossRef] [PubMed]
- Karalewitz, A.P.-A.; Fu, Z.; Baldwin, M.R.; Kim, J.-J.P.; Barbieri, J.T. Botulinum neurotoxin serotype C associates with dual ganglioside receptors to facilitate cell entry. J. Biol. Chem. 2012, 287, 40806–40816. [Google Scholar] [CrossRef] [PubMed]
- Bercsenyi, K.; Schmieg, N.; Bryson, J.B.; Wallace, M.; Caccin, P.; Golding, M.; Zanotti, G.; Greensmith, L.; Nischt, R.; Schiavo, G. Nidogens are therapeutic targets for the prevention of tetanus. Science 2014, 346, 1118–1123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, L.; Tepp, W.H.; Johnson, E.A.; Dong, M. Botulinum neurotoxin d uses synaptic vesicle protein SV2 and gangliosides as receptors. PLoS Pathog. 2011, 7, e1002008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yowler, B.C.; Schengrund, C.-L. Botulinum neurotoxin a changes conformation upon binding to ganglioside GT1b. Biochemistry 2004, 43, 9725–9731. [Google Scholar] [CrossRef] [PubMed]
- Benson, M.A.; Fu, Z.; Kim, J.-J.P.; Baldwin, M.R. Unique ganglioside recognition strategies for clostridial neurotoxins. J. Biol. Chem. 2011, 286, 34015–34022. [Google Scholar] [CrossRef] [PubMed]
- Hamark, C.; Berntsson, R.P.-A.; Masuyer, G.; Henriksson, L.M.; Gustafsson, R.; Stenmark, P.l.; Widmalm, G.R. Glycans confer specificity to the recognition of ganglioside receptors by botulinum neurotoxin A. J. Am. Chem. Soc. 2016, 139, 218–230. [Google Scholar] [CrossRef] [PubMed]
- Weisemann, J.; Stern, D.; Mahrhold, S.; Dorner, B.G.; Rummel, A. Botulinum neurotoxin serotype a recognizes its protein receptor SV2 by a different mechanism than botulinum neurotoxin B synaptotagmin. Toxins 2016, 8, 154. [Google Scholar] [CrossRef] [PubMed]
- Yao, G.; Zhang, S.; Mahrhold, S.; Lam, K.-H.; Stern, D.; Bagramyan, K.; Perry, K.; Kalkum, M.; Rummel, A.; Dong, M. N-linked glycosylation of SV2 is required for binding and uptake of botulinum neurotoxin A. Nat. Struct. Mol. Biol. 2016, 23, 656. [Google Scholar] [CrossRef] [PubMed]
- Tao, L.; Peng, L.; Berntsson, R.P.-A.; Liu, S.M.; Park, S.; Yu, F.; Boone, C.; Palan, S.; Beard, M.; Chabrier, P.-E. Engineered botulinum neurotoxin B with improved efficacy for targeting human receptors. Nat. Commun. 2017, 8, 53. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.S.; Tse, C.K.; Dolly, J.O.; Hambleton, P.; Melling, J. Radioiodination of botulinum neurotoxin type a with retention of biological activity and its binding to brain synaptosomes. FEBS J. 1983, 131, 437–445. [Google Scholar] [CrossRef]
- Evans, D.M.; Williams, R.S.; Shone, C.C.; Hambleton, P.; Melling, J.; Dolly, J.O. Botulinum neurotoxin type B. FEBS J. 1986, 154, 409–416. [Google Scholar]
- Nishiki, T.-I.; Tokuyama, Y.; Kamata, Y.; Nemoto, Y.; Yoshida, A.; Sato, K.; Sekiguchi, M.; Takahashi, M.; Kozaki, S. The high-affinity binding of clostridium botulinum type B neurotoxin to synaptotagmin II associated with gangliosides GT1b/GD1a. FEBS Lett. 1996, 378, 253–257. [Google Scholar] [CrossRef]
- Desplantes, R.; Lévêque, C.; Muller, B.; Lotierzo, M.; Ferracci, G.; Popoff, M.; Seagar, M.; Mamoun, R.; El Far, O. Affinity biosensors using recombinant native membrane proteins displayed on exosomes: Application to botulinum neurotoxin B receptor. Sci. Rep. 2017, 7, 1032. [Google Scholar] [CrossRef] [PubMed]
- Stern, D.; Weisemann, J.; Le Blanc, A.; von Berg, L.; Mahrhold, S.; Piesker, J.; Laue, M.; Luppa, P.B.; Dorner, M.B.; Dorner, B.G. A lipid-binding loop of botulinum neurotoxin serotypes B, DC and G is an essential feature to confer their exquisite potency. PLoS Pathog. 2018, 14, e1007048. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A.; Bade, S.; Alves, J.; Bigalke, H.; Binz, T. Two carbohydrate binding sites in the HCC-domain of tetanus neurotoxin are required for toxicity. J. Mol. Biol. 2003, 326, 835–847. [Google Scholar] [CrossRef]
- Rummel, A.; Mahrhold, S.; Bigalke, H.; Binz, T. The HCC-domain of botulinum neurotoxins A and B exhibits a singular ganglioside binding site displaying serotype specific carbohydrate interaction. Mol. Microbiol. 2004, 51, 631–643. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Fu, Z.; Kim, J.-J.P.; Barbieri, J.T.; Baldwin, M.R. Gangliosides as high affinity receptors for tetanus neurotoxin. J. Biol. Chem. 2009, 284, 26569–26577. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.; Chen, C.; Barbieri, J.T.; Kim, J.-J.P.; Baldwin, M.R. Glycosylated SV2 and gangliosides as dual receptors for botulinum neurotoxin serotype F. Biochemistry 2009, 48, 5631–5641. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A.; Häfner, K.; Mahrhold, S.; Darashchonak, N.; Holt, M.; Jahn, R.; Beermann, S.; Karnath, T.; Bigalke, H.; Binz, T. Botulinum neurotoxins C, E and F bind gangliosides via a conserved binding site prior to stimulation-dependent uptake with botulinum neurotoxin F utilising the three isoforms of SV2 as second receptor. J. Neurochem. 2009, 110, 1942–1954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karalewitz, A.P.-A.; Kroken, A.R.; Fu, Z.; Baldwin, M.R.; Kim, J.-J.P.; Barbieri, J.T. Identification of a unique ganglioside binding loop within botulinum neurotoxins C and D-SA. Biochemistry 2010, 49, 8117–8126. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Buchko, G.W.; Qin, L.; Robinson, H.; Varnum, S.M. Structural analysis of the receptor binding domain of botulinum neurotoxin serotype D. Biochem. Biophys. Res. Commun. 2010, 401, 498–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strotmeier, J.; Gu, S.; Jutzi, S.; Mahrhold, S.; Zhou, J.; Pich, A.; Eichner, T.; Bigalke, H.; Rummel, A.; Jin, R. The biological activity of botulinum neurotoxin type C is dependent upon novel types of ganglioside binding sites. Mol. Microbiol. 2011, 81, 143–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strotmeier, J.; Lee, K.; Völker, A.K.; Mahrhold, S.; Zong, Y.; Zeiser, J.; Zhou, J.; Pich, A.; Bigalke, H.; Binz, T. Botulinum neurotoxin serotype D attacks neurons via two carbohydrate-binding sites in a ganglioside-dependent manner. Biochem. J. 2010, 431, 207–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, S.; Berntsson, R.P.; Tepp, W.H.; Tao, L.; Johnson, E.A.; Stenmark, P.; Dong, M. Structural basis for the unique ganglioside and cell membrane recognition mechanism of botulinum neurotoxin DC. Nat. Commun. 2017, 8, 1637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chai, Q.; Arndt, J.W.; Dong, M.; Tepp, W.H.; Johnson, E.A.; Chapman, E.R.; Stevens, R.C. Structural basis of cell surface receptor recognition by botulinum neurotoxin B. Nature 2006, 444, 1096. [Google Scholar] [CrossRef] [PubMed]
- Jin, R.; Rummel, A.; Binz, T.; Brunger, A.T. Botulinum neurotoxin B recognizes its protein receptor with high affinity and specificity. Nature 2006, 444, 1092. [Google Scholar] [CrossRef] [PubMed]
- Berntsson, R.P.; Peng, L.; Dong, M.; Stenmark, P. Structure of dual receptor binding to botulinum neurotoxin B. Nat. Commun. 2013, 4, 2058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, L.; Berntsson, R.P.-A.; Tepp, W.H.; Pitkin, R.M.; Johnson, E.A.; Stenmark, P.; Dong, M. Botulinum neurotoxin DC uses synaptotagmin I and II as receptors, and human synaptotagmin II is not an effective receptor for type B, DC and G toxins. J. Cell Sci. 2012, 125, 3233–3242. [Google Scholar] [CrossRef] [PubMed]
- Strotmeier, J.; Willjes, G.; Binz, T.; Rummel, A. Human synaptotagmin-II is not a high affinity receptor for botulinum neurotoxin B and G: Increased therapeutic dosage and immunogenicity. FEBS Lett. 2012, 586, 310–313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dressler, D. Clinical applications of botulinum toxin. Curr. Opin. Microbiol. 2012, 15, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Dong, M.; Liu, H.; Tepp, W.H.; Johnson, E.A.; Janz, R.; Chapman, E.R. Glycosylated SV2A and SV2B mediate the entry of botulinum neurotoxin e into neurons. Mol. Biol. Cell 2008, 19, 5226–5237. [Google Scholar] [CrossRef] [PubMed]
- Juzans, P.; Comella, J.X.; Molgo, J.; Faille, L.; Angaut-Petit, D. Nerve terminal sprouting in botulinum type-A treated mouse levator auris longus muscle. Neuromuscul. Disord. 1996, 6, 177–185. [Google Scholar] [CrossRef]
- Pang, Z.P.; Melicoff, E.; Padgett, D.; Liu, Y.; Teich, A.F.; Dickey, B.F.; Lin, W.; Adachi, R.; Südhof, T.C. Synaptotagmin-2 is essential for survival and contributes to Ca2+ triggering of neurotransmitter release in central and neuromuscular synapses. J. Neurosci. 2006, 26, 13493–13504. [Google Scholar] [CrossRef] [PubMed]
- Tejero, R.; Lopez-Manzaneda, M.; Arumugam, S.; Tabares, L. Synaptotagmin-2, and-1, linked to neurotransmission impairment and vulnerability in spinal muscular atrophy. Hum. Mol. Genet. 2016, 25, 4703–4716. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-Y.; Jahn, R.; Dahlström, A. Synaptotagmin I is present mainly in autonomic and sensory neurons of the rat peripheral nervous system. Neuroscience 1994, 63, 837–850. [Google Scholar] [CrossRef]
- Bartholome, O.; Van den Ackerveken, P.; Sánchez Gil, J.; de la Brassinne Bonardeaux, O.; Leprince, P.; Franzen, R.; Rogister, B. Puzzling out synaptic vesicle 2 family members functions. Front. Mol. Neurosci. 2017, 10, 148. [Google Scholar] [CrossRef] [PubMed]
- Yiangou, Y.; Anand, U.; Otto, W.R.; Sinisi, M.; Fox, M.; Birch, R.; Foster, K.A.; Mukerji, G.; Akbar, A.; Agarwal, S.K. Increased levels of SV2A botulinum neurotoxin receptor in clinical sensory disorders and functional effects of botulinum toxins A and E in cultured human sensory neurons. J. Pain Res. 2011, 4, 347. [Google Scholar] [PubMed]
- Robert K, Y.; Tsai, Y.-T.; Ariga, T.; Yanagisawa, M. Structures, biosynthesis, and functions of gangliosides-an overview. J. Oleo Sci. 2011, 60, 537–544. [Google Scholar]
- Schengrund, C.-L. Gangliosides: Glycosphingolipids essential for normal neural development and function. Trends Biochem. Sci. 2015, 40, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Willison, H.J.; Plomp, J.J. Anti-ganglioside antibodies and the presynaptic motor nerve terminal. Ann. N. Y. Acad. Sci. 2008, 1132, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Rummel, A. Transport Protein Which Is Used to Introduce Chemical Compounds into Nerve Cells. U.S. Patent 9,234,011, 12 January 2016. [Google Scholar]
- Shone, C.C.; Hambleton, P.; Melling, J. Inactivation of clostridium botulinum type a neurotoxin by trypsin and purification of two tryptic fragments. Proteolytic action near the COOH-terminus of the heavy subunit destroys toxin-binding activity. Eur. J. Biochem. 1985, 151, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Shone, C.C.; Hambleton, P.; Melling, J. A 50-kDa fragment from the NH2-terminus of the heavy subunit of clostridium botulinum type a neurotoxin forms channels in lipid vesicles. FEBS J. 1987, 167, 175–180. [Google Scholar] [CrossRef]
- Masuyer, G.; Thiyagarajan, N.; James, P.L.; Marks, P.M.; Chaddock, J.A.; Acharya, K.R. Crystal structure of a catalytically active, non-toxic endopeptidase derivative of clostridium botulinum toxin A. Biochem. Biophys. Res. Commun. 2009, 381, 50–53. [Google Scholar] [CrossRef] [PubMed]
- Chaddock, J.A.; Purkiss, J.R.; Duggan, M.J.; Quinn, C.P.; Shone, C.C.; Foster, K.A. A conjugate composed of nerve growth factor coupled to a non-toxic derivative of clostridium botulinum neurotoxin type A can inhibit neurotransmitter release in vitro. Growth Factors 2000, 18, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Chaddock, J.A.; Herbert, M.H.; Ling, R.J.; Alexander, F.C.; Fooks, S.J.; Revell, D.F.; Quinn, C.P.; Shone, C.C.; Foster, K.A. Expression and purification of catalytically active, non-toxic endopeptidase derivatives of clostridium botulinum toxin type A. Protein Express. Purif. 2002, 25, 219–228. [Google Scholar] [CrossRef]
- Foster, K.A.; Adams, E.J.; Durose, L.; Cruttwell, C.J.; Marks, E.; Shone, C.C.; Chaddock, J.A.; Cox, C.L.; Heaton, C.; Sutton, J.M.; et al. Re-engineering the target specificity of clostridial neurotoxins—A route to novel therapeutics. Neurotox. Res. 2006, 9, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Meng, J.; Wang, J.; Hearty, S.; Dolly, J.O.; O’Kennedy, R. Targeted delivery of a snare protease to sensory neurons using a single chain antibody (scFv) against the extracellular domain of P2X3 inhibits the release of a pain mediator. Biochem. J. 2014, 462, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Leggett, J.; Harper, E.; Waite, E.; Marks, P.; Martinez, A.; Lightman, S. Ghrh receptor-targeted botulinum neurotoxin selectively inhibits pulsatile GH secretion in male rats. Endocrinology 2013, 154, 3305–3318. [Google Scholar] [CrossRef] [PubMed]
- Darios, F.; Niranjan, D.; Ferrari, E.; Zhang, F.; Soloviev, M.; Rummel, A.; Bigalke, H.; Suckling, J.; Ushkaryov, Y.; Naumenko, N. Snare tagging allows stepwise assembly of a multimodular medicinal toxin. Proc. Natl. Acad. Sci. USA 2010, 107, 18197–18201. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, E.; Soloviev, M.; Niranjan, D.; Arsenault, J.; Gu, C.; Vallis, Y.; O’Brien, J.; Davletov, B. Assembly of protein building blocks using a short synthetic peptide. Bioconjug. Chem. 2012, 23, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Arsenault, J.; Ferrari, E.; Niranjan, D.; Cuijpers, S.A.; Gu, C.; Vallis, Y.; O’brien, J.; Davletov, B. Stapling of the botulinum type a protease to growth factors and neuropeptides allows selective targeting of neuroendocrine cells. J. Neurochem. 2013, 126, 223–233. [Google Scholar] [CrossRef] [PubMed]
- Fonfria, E.; Donald, S.; Cadd, V.A. Botulinum neurotoxin a and an engineered derivate targeted secretion inhibitor (TSI) a enter cells via different vesicular compartments. J. Recept. Signal Transduct. 2016, 36, 79–88. [Google Scholar]
- Jiang, W.; Bond, J.S. Families of metalloendopeptidases and their relationships. FEBS Lett. 1992, 312, 110–114. [Google Scholar] [CrossRef] [Green Version]
- Binz, T.; Sikorra, S.; Mahrhold, S. Clostridial neurotoxins: Mechanism of snare cleavage and outlook on potential substrate specificity reengineering. Toxins 2010, 2, 665–682. [Google Scholar] [CrossRef] [PubMed]
- Breidenbach, M.A.; Brunger, A.T. Substrate recognition strategy for botulinum neurotoxin serotype A. Nature 2004, 432, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Lacy, D.B.; Tepp, W.; Cohen, A.C.; DasGupta, B.R.; Stevens, R.C. Crystal structure of botulinum neurotoxin type a and implications for toxicity. Nat. Struct. Biol. 1998, 5, 898–902. [Google Scholar] [CrossRef] [PubMed]
- Guex, N.; Peitsch, M.C. SWISS-MODEL and the Swiss-Pdbviewer: An environment for comparative protein modeling. Electrophoresis 1997, 18, 2714–2723. [Google Scholar] [CrossRef] [PubMed]
- Sikorra, S.; Henke, T.; Galli, T.; Binz, T. Substrate recognition mechanism of VAMP/synaptobrevin-cleaving clostridial neurotoxins. J. Biol. Chem. 2008, 283, 21145–21152. [Google Scholar] [CrossRef] [PubMed]
- Shone, C.C.; Roberts, A.K. Peptide substrate specificity and properties of the zinc-endopeptidase activity of botulinum type B neurotoxin. FEBS J. 1994, 225, 263–270. [Google Scholar] [CrossRef]
- Sikorra, S.; Litschko, C.; Muller, C.; Thiel, N.; Galli, T.; Eichner, T.; Binz, T. Identification and characterization of botulinum neurotoxin a substrate binding pockets and their re-engineering for human SNAP-23. J. Mol. Biol. 2016, 428, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Kim, J.J.; Barbieri, J.T. Mechanism of substrate recognition by botulinum neurotoxin serotype A. J. Biol. Chem. 2007, 282, 9621–9627. [Google Scholar] [CrossRef] [PubMed]
- Kumaran, D.; Rawat, R.; Ahmed, S.A.; Swaminathan, S. Substrate binding mode and its implication on drug design for botulinum neurotoxin A. PLoS Pathog. 2008, 4, e1000165. [Google Scholar] [CrossRef] [PubMed]
- Ho, M.; Goh, C.H.; Brothers, M.C.; Wang, S.; Young, R.L.; Ou, Y.; Lui, J.N.; Kalafatis, M.; Lan, X.; Wolf, A.E.; et al. Glycine insertion at protease cleavage site of SNAP25 resists cleavage but enhances affinity for botulinum neurotoxin serotype A. Protein Sci. 2012, 21, 318–326. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schiavo, G.; Shone, C.C.; Bennett, M.K.; Scheller, R.H.; Montecucco, C. Botulinum neurotoxin type C cleaves a single Lys-Ala bond within the carboxyl-terminal region of syntaxins. J. Biol. Chem. 1995, 270, 10566–10570. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, V.V.; Yoshino, K.I.; Jahnz, M.; Dörries, C.; Bade, S.; Nauenburg, S.; Niemann, H.; Binz, T. Proteolysis of SNAP-25 isoforms by botulinum neurotoxin types A, C, and E. J. Neurochem. 1999, 72, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Jin, R.; Sikorra, S.; Stegmann, C.M.; Pich, A.; Binz, T.; Brunger, A.T. Structural and biochemical studies of botulinum neurotoxin serotype C1 light chain protease: Implications for dual substrate specificity. Biochemistry 2007, 46, 10685–10693. [Google Scholar] [CrossRef] [PubMed]
- Pellizzari, R.; Mason, S.; Shone, C.C.; Montecucco, C. The interaction of synaptic vesicle-associated membrane protein/synaptobrevin with botulinum neurotoxins D and F. FEBS Lett. 1997, 409, 339–342. [Google Scholar] [CrossRef] [Green Version]
- Pellizzari, R.; Rossetto, O.; Lozzi, L.; Johnson, E.; Shone, C.C.; Montecucco, C. Structural determinants of the specificity for synaptic vesicle-associated membrane protein/synaptobrevin of tetanus and botulinum type B and G neurotoxins. J. Biol. Chem. 1996, 271, 20353–20358. [Google Scholar] [CrossRef] [PubMed]
- Lam, K.-H.; Sikorra, S.; Weisemann, J.; Maatsch, H.; Perry, K.; Rummel, A.; Binz, T.; Jin, R. Structural and biochemical characterization of the protease domain of the mosaic botulinum neurotoxin type HA. Pathog. Dis. 2018, 76, fty044. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, S.; Binz, T.; Hayashi, T.; Szabo, E.; Yamasaki, N.; Eklund, M.; Jahn, R.; Niemann, H. Botulinum neurotoxin type G proteolyses the ALa81-ALa82 bond of rat synaptobrevin 2. Biochem. Biophys. Res. Commun. 1994, 200, 829–835. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.; Schmidt, J.J.; Stafford, R.G.; Swaminathan, S. Mode of VAMP substrate recognition and inhibition of clostridium botulinum neurotoxin F. Nat. Struct. Mol. Biol. 2009, 16, 789. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Chan, E.W.C.; Chen, S. Mechanism of substrate recognition by the novel botulinum neurotoxin subtype F5. Sci. Rep. 2016, 6, 19875. [Google Scholar] [CrossRef] [PubMed]
- Fasshauer, D.; Sutton, R.B.; Brunger, A.T.; Jahn, R. Conserved structural features of the synaptic fusion complex: SNARE proteins reclassified as Q- and R-SNAREs. Proc. Natl. Acad. Sci. USA 1998, 95, 15781–15786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masuyer, G.; Zhang, S.; Barkho, S.; Shen, Y.; Henriksson, L.; Kosenina, S.; Dong, M.; Stenmark, P. Structural characterisation of the catalytic domain of botulinum neurotoxin X—High activity and unique substrate specificity. Sci. Rep. 2018, 8, 4518. [Google Scholar] [CrossRef] [PubMed]
- Brunt, J.; Carter, A.T.; Stringer, S.C.; Peck, M.W. Identification of a novel botulinum neurotoxin gene cluster in enterococcus. FEBS Lett. 2018, 592, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Zornetta, I.; Azarnia Tehran, D.; Arrigoni, G.; Anniballi, F.; Bano, L.; Leka, O.; Zanotti, G.; Binz, T.; Montecucco, C. The first non clostridial botulinum-like toxin cleaves vamp within the juxtamembrane domain. Sci. Rep. 2016, 6, 30257. [Google Scholar] [CrossRef] [PubMed]
- Webb, R.P.; Smith, T.J.; Wright, P.; Brown, J.; Smith, L.A. Production of catalytically inactive BoNT/A1 holoprotein and comparison with BoNT/A1 subunit vaccines against toxin subtypes A1, A2, and A3. Vaccine 2009, 27, 4490–4497. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.J.; Bostian, K.A. Endoproteinase activity of type a botulinum neurotoxin: Substrate requirements and activation by serum albumin. J. Protein Chem. 1997, 16, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; de Paiva, A.; Liu, D.; Aoki, R.; Dolly, J.O. Expression and purification of the light chain of botulinum neurotoxin A: A single mutation abolishes its cleavage of SNAP-25 and neurotoxicity after reconstitution with the heavy chain. Biochemistry 1995, 34, 15175–15181. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, O.; Seveso, M.; Caccin, P.; Schiavo, G.; Montecucco, C. Tetanus and botulinum neurotoxins: Turning bad guys into good by research. Toxicon 2001, 39, 27–41. [Google Scholar] [CrossRef]
- Blasi, J.; Chapman, E.R.; Link, E.; Binz, T.; Yamasaki, S.; De Camilli, P.; Sudhof, T.C.; Niemann, H.; Jahn, R. Botulinum neurotoxin a selectively cleaves the synaptic protein SNAP-25. Nature 1993, 365, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Masuyer, G.; Stancombe, P.; Chaddock, J.A.; Acharya, K.R. Structures of engineered clostridium botulinum neurotoxin derivatives. Acta Crystallogr. Sect. F Struct. Biol. Cryst. Commun. 2011, 67, 1466–1472. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Zhang, Z.; Dong, M.; Sun, S.; Chapman, E.R.; Jackson, M.B. Syntaxin requirement for Ca2+-triggered exocytosis in neurons and endocrine cells demonstrated with an engineered neurotoxin. Biochemistry 2011, 50, 2711–2713. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.; Pan, X.; Zhao, Y.; Chen, S. Engineering clostridia neurotoxins with elevated catalytic activity. Toxicon 2013, 74, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Elliott, M.; Maignel, J.; Liu, S.M.; Favre-Guilmard, C.; Mir, I.; Farrow, P.; Hornby, F.; Marlin, S.; Palan, S.; Beard, M. Augmentation of vamp-catalytic activity of botulinum neurotoxin serotype B does not result in increased potency in physiological systems. PLoS ONE 2017, 12, e0185628. [Google Scholar] [CrossRef] [PubMed]
- Masuyer, G.; Chaddock, J.A.; Foster, K.A.; Acharya, K.R. Engineered botulinum neurotoxins as new therapeutics. Annu. Rev. Pharmacol. Toxicol. 2014, 54, 27–51. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Barbieri, J.T. Engineering botulinum neurotoxin to extend therapeutic intervention. Proc. Natl. Acad. Sci. USA 2009, 106, 9180–9184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, L.; Liu, H.; Ruan, H.; Tepp, W.H.; Stoothoff, W.H.; Brown, R.H.; Johnson, E.A.; Yao, W.D.; Zhang, S.C.; Dong, M. Cytotoxicity of botulinum neurotoxins reveals a direct role of syntaxin 1 and SNAP-25 in neuron survival. Nat. Commun. 2013, 4, 1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rust, A.; Leese, C.; Binz, T.; Davletov, B. Botulinum neurotoxin type C protease induces apoptosis in differentiated human neuroblastoma cells. Oncotarget 2016, 7, 33220–33228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williamson, L.C.; Neale, E.A. Syntaxin and 25-kDa synaptosomal-associated protein: Differential effects of botulinum neurotoxins C1 and A on neuronal survival. J. Neurosci. Res. 1998, 52, 569–583. [Google Scholar] [CrossRef]




© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonfria, E.; Elliott, M.; Beard, M.; Chaddock, J.A.; Krupp, J. Engineering Botulinum Toxins to Improve and Expand Targeting and SNARE Cleavage Activity. Toxins 2018, 10, 278. https://doi.org/10.3390/toxins10070278
Fonfria E, Elliott M, Beard M, Chaddock JA, Krupp J. Engineering Botulinum Toxins to Improve and Expand Targeting and SNARE Cleavage Activity. Toxins. 2018; 10(7):278. https://doi.org/10.3390/toxins10070278
Chicago/Turabian StyleFonfria, Elena, Mark Elliott, Matthew Beard, John A. Chaddock, and Johannes Krupp. 2018. "Engineering Botulinum Toxins to Improve and Expand Targeting and SNARE Cleavage Activity" Toxins 10, no. 7: 278. https://doi.org/10.3390/toxins10070278
APA StyleFonfria, E., Elliott, M., Beard, M., Chaddock, J. A., & Krupp, J. (2018). Engineering Botulinum Toxins to Improve and Expand Targeting and SNARE Cleavage Activity. Toxins, 10(7), 278. https://doi.org/10.3390/toxins10070278